Abstract
Introduction
Long COVID (LC) is a multisystem disease with symptoms lasting weeks or months beyond the acute COVID-19 infection. Several manifestations are reported by people with LC, including effects on mental health, with varying degrees of psychological distress and disturbances to daily activities. Research conducted to identify effective interventions to support mental health among people with LC has been limited by the breadth and scope of studies.
Aim
This review aims to identify interventions being tested to support mental health of people with LC.
Methods
A scoping review was conducted by searching five databases for articles published between January 2020 and early October 2022 to identify research evaluating interventions focused on improving mental health symptoms associated with LC. Results from all sources were checked for eligibility by two reviewers, and agreements were resolved by discussion. Gray literature and reference list of included studies and relevant reviews were scrutinised to identify any additional studies. Data extraction was conducted by one reviewer and checked by another reviewer for accuracy.
Results
Of the 940 studies identified, 17 were included, the design of which varied but included mainly case studies (n = 6) and clinical trials (n = 5). Several interventions were described, ranging from single interventions (e.g., pharmacologic) to more holistic, comprehensive suites of services (pharmacologic and non-pharmacologic). Several mental health outcomes were measured, mostly anxiety and depression. All included studies were reported to be associated with improvements in participants’ mental health outcomes.
Conclusion
This scoping review identified studies reporting on a variety of interventions to support mental health among people with LC. Although positive changes were reported by all studies, some were case studies and thus their findings must be interpreted with caution. There is a need for more research to be conducted to identify the impact of interventions on mental health of people with LC.
Similar content being viewed by others
Introduction
The COVID-19 pandemic began in China in December 2019 [1], and as of December 2022, it had claimed the lives of more than six million people and infected more than 640 million around the world [2]. Most attention has focused on the acute COVID-19 infection [3], with comparatively little devoted to the longer term and ongoing symptoms experienced and reported by many people [4]. These people, who often felt their symptoms were neglected or disbelieved, formed support groups on social media, drawing global attention to this ongoing condition, which was named ‘long COVID’ (LC) [5]. This condition has been described by several other labels, including post-COVID, long haulers, post-acute COVID, and post-SARS-COV-2 [6,7,8]. It has also several definitions [9]. For example, in the UK, according to the National Institute for Health and Care Excellence (NICE), LC represents “signs and symptoms that develop during or after an infection consistent with COVID-19, continue for more than 12 weeks and are not explained by an alternative diagnosis… It includes both ongoing symptomatic COVID-19 (from 4 to 12 weeks) and post-COVID-19 syndrome (12 weeks or more)” [10]. Similarly, the World Health Organisation (WHO) defines LC as follows: “Post-COVID-19 condition occurs in individuals with a history of probable or confirmed SARS-CoV-2 infection, usually 3 months from the onset of COVID-19 with symptoms that last for at least 2 months and cannot be explained by an alternative diagnosis.” [11].
Research on LC shows that following the acute viral infection, damage can occur in different organs in the body including the brain [12]. There are multiple potential symptomatic sequelae including musculoskeletal problems, cognitive impairment, fatigue, and psychological distress [13,14,15,16].
Chronic illness and disability caused by LC represents a major emerging health challenge [4], LC can affect all aspects of an individual’s daily life, including quality of life (QoL), social functioning, and ability to participate in normal activities [17, 18]. In addition, mental health problems appear common in LC [19,20,21,22].
The precise proportion of people who contract COVID-19 and have LC has not been firmly established [23,24,25], though it is estimated that, globally, around 43% of people experience some degree of long-term symptoms following the acute infection [26]. In the UK it has been estimated that more than 1.8 million people have LC [27], though this will likely increase as COVID-19 continues to circulate [3]. Those at most risk of LC are women, elderly people, smokers, obese or overweight people, and those living in socio-economically challenged areas [4, 28].
The impact of LC on mental health has been examined. Studies report that more than 87% of people with LC have mental health symptoms, including anxiety, depression, and cognitive problems [29,30,31,32,33,34,35,36]. As LC is a relatively new illness, it is surrounded by a great deal of uncertainty: it can manifest differently from one person to another, with more than 200 associated symptoms [31] and presentations that do not necessarily fit into established clinical categories [4]. Indeed, some consider LC to be a form of post-viral syndrome [37], which provides some evidence base for treatment and management. However, in the face of uncertainty, patients can be at risk of being either over-investigated and over-treated, or under-investigated and under-treated [4]. As such, no evidence-based treatment options are yet available [38,39,40,41]. Usual care currently provided to people with LC is through LC clinics and services, and general medical practices [42, 43].
A recent systematic review showed that while some research is currently being conducted to examine interventions to support the mental health of people with LC, the breadth and scope of this research is limited [35]. This systematic review was focused on ongoing trials that were conducted between January 2020 to May 2022. In this context, this scoping review aims to more broadly identify what interventions have been examined to support the mental health of people with LC.
Methods
Database search
This scoping review was conducted following Arksey and O’Malley framework [44] and is reported following PRISMA-ScR (Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews) guidelines [45]. No priori protocol to this scoping review was published or registered. A systematic search was conducted on 3 October 2022 to identify relevant studies using MEDLINE, EMBASE, Web of Science, CINAHL, and PsycInfo databases from January 2020 to early October 2022. Searches were limited to journal articles. Records were exported initially into the reference manager Endnote, where duplicates were identified and removed, and then to Covidence software for data management [46].
Search terms
Between 16 September and 3 October 2022, preliminary searches were initially conducted using the databases mentioned to identify appropriate keywords to use in this review. Search terms were selected based on the target population and the target intervention, and terms were grouped under three headings related to LC, intervention, and mental health problems associated with LC. The search keywords are detailed in Table 1, (see Additional file 1 for an example of the search strategy). Moreover, reference lists of included studies and related reviews were also examined to identify additional potentially eligible studies. Grey literature was also checked to identify any additional relevant studies, using the following resources: Social Care Institute for Excellence (SCIE), Canadian Agency for Drug and Technologies in Health (CADTH), King’s Fund, Open Grey, and the Health Foundation. The search strategy was adapted appropriately when searching the different databases.
Study inclusion criteria
As is conventional with scoping reviews [47, 48], our inclusion criteria were deliberately broad, namely:
-
1.
Research focused on LC and mental health
-
2.
Research that introduces/discusses an intervention/treatment/support for mental health issues associated with LC
-
3.
Research where assessment of mental health is the primary outcome (since mental health is commonly affected by LC and is also impacted by physical symptoms of LC).
-
4.
Patient population is aged 18 years and above
-
5.
Publications from 2020 to 2022
-
6.
Original research (article/journal article) (including qualitative, quantitative, or mixed research methods, case reports or other study designs that reports an original research).
Studies that did not meet one or more of the above criteria or that met any of the following exclusion criteria were excluded from the review. Research that is focused on:
-
1.
COVID-19 acute infection and/or its treatment
-
2.
Treatment of mental health issues not related to/ induced by LC
-
3.
Treating issues caused by LC but not related to mental health (e.g., respiratory, or cardiovascular problems).
Study selection
Title and abstracts, then full text screening were independently carried out by two reviewers (HA and LDH), to assess article eligibility against the inclusion and exclusion criteria. Any arising disagreements were resolved by discussion between the two reviewers, and if necessary, by consulting with a third reviewer (CFS).
For studies not written in the English language but were found relevant at title and abstract screening, corresponding authors were contacted to request relevant information; when additional information was not provided by the authors, Yandex website (https://translate.yandex.com/doc) was used to translate these studies to confirm eligibility and extract relevant data. Additionally, where full texts of included studies were not retained even after contacting corresponding authors, their abstracts were included and used for data extraction.
Data extraction
A data extraction template was designed using Microsoft Excel to extract the following items-where available- from each study:
-
1.
Author(s) and publication year
-
2.
Study design
-
3.
Study setting and country
-
4.
Participant information (recruited participants, age, gender, and ethnicity)
-
5.
Practitioners involved in delivering the intervention/treatment
-
6.
Description of the intervention
-
7.
Description of the outcome measures and study findings.
Data extraction was carried out by HA and was reviewed and verified by LDH, AC, MS, DC, DRT and CFS to ensure accuracy and completeness. Disagreements were resolved by discussion or through consultation with a third reviewer (CFS).
Data synthesis
A narrative approach was used to synthesize and describe the data extracted from included studies [49].
Dealing with missing data
Corresponding authors were contacted by email to collect any missing data. When no response was received, studies were still included in the review with missing data designated as ‘not reported’.
Results
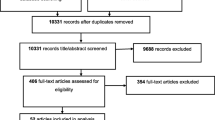
A total of 940 unique records were identified through the database search. No additional studies were identified from the grey literature or from the reference lists of included studies. After the complete screening and selection process, the final review encompassed 17 studies. The findings of the search process are presented in the PRISMA flow diagram (Fig. 1).
General description of included studies
Table 2 provides an overview of included studies. Of all included studies, one study was retained based on a relevant abstract in the absence of a full text despite multiple attempts to obtain it [50]. All studies were written in the English language except for three, written in Russian [50,51,52]. The included studies were conducted in nine countries, with more than half conducted in Europe (n = 11, 64.7%), five of which were from the UK.
Of the 17 included studies, six were case studies [53, 56, 59, 62,63,64] and five were clinical trials [50,51,52, 60, 61], two of the latter were randomised controlled trials (RCTs) [60, 61]. Other designs encompassed four single arm pre-post studies [55, 57, 65, 66], one qualitative study [54] and a single service evaluation study [58]. Several settings were described by included studies including primary and secondary healthcare settings, a university setting in collaboration with a local GP collaboration group, outpatient subspeciality clinic, and hospital outpatient care. Three studies did not clearly report their setting [51, 56, 63].
Eight studies did not report the method used in recruiting participants [50,51,52, 56, 57, 59, 63, 64]. Described recruitment approaches included social media, referral from LC clinics, medical doctors, or a local community network. One study recruited staff with LC opportunistically from specific settings [55].
A total of 940 participants were recruited across all included studies, with individual study numbers ranging from one [56, 59, 62,63,64] to 219 [55]. All case studies (n = 6) recruited only one or two participants [53, 56, 59, 62,63,64]. Participants were recruited at different stages of their LC journey (i.e., at different time points since having the acute COVID-19 infection). This was reported by 13 studies [50, 51, 54,55,56,57, 59,60,61,62,63,64,65], ranging from one month post-acute COVID-19 [57] to over a year post infection [64, 65].
The gender of included participants was reported by all studies except one [50], but in two further studies, gender was reported as a missing variable for some participants [55, 58]. Most recruited participants were women (total n = 353, range 1–121) [51,52,53,54, 56,57,58,59,60,61,62,63,64,65,66, 63]. One study reported the gender of participants pre and post assessment [55].
Age of included participants was reported by all studies, either as a precise age (n = 5) [53, 56, 59, 62, 64], or as an average (mean, median) of all participants (n = 2) [57, 61], or as an average age of groups of participants allocated at different treatment groups or at different assessment time points (n = 4) [50, 52, 55, 60], or as a range (n = 6) [51, 54, 58, 63, 65, 66]. Across all studies, age ranged from a 15–24 age group to 92 years [58].
Ethnicity or cultural background of participants was reported for only nine studies, with half of these including only people identifying as white or Asian and the rest reporting a variety of ethnicities/cultural backgrounds.
Description of study intervention/treatment
Table 3 describes the various interventions tested by the included studies, ranging from a single intervention (e.g., using a pharmacological product, sessions of electromagnetic field, modifications to diet) (n = 7) [50, 51, 59, 61,62,63, 65], to integrated programmes covering diverse elements of health (n = 10) [52,53,54,55,56,57,58, 60, 64, 66]. Healthcare components included rehabilitation programmes, lifestyle interventions, stress management, sleep hygiene, breathing techniques, optimising diet, energy conservation, psychoeducation, maintaining social contacts with close networks, reading, relaxation techniques and cognitive behavioural therapy (CBT). Some interventions were focused on testing the effects of certain pharmacological products or nutritional changes on enhancing outcomes.
Practitioners involved in delivering the intervention were reported by 12 studies, five of which engaged practitioners of a particular speciality, (e.g., medical doctors or clinical psychologists) [53, 60, 62, 64, 65]; one was being supervised by a cardiopulmonary specialist [64]. A multidisciplinary team approach was adopted in the other six studies, including physicians, occupational therapists, psychologists, physiotherapists, dieticians, speech and language therapists, sport medicine specialists and CBT therapists [54,55,56,57,58, 61]. The remaining six studies did not report who was involved in delivering the intervention [50,51,52, 59, 63, 66].
The duration of intervention delivery was reported by all studies except one [66], and ranged from a single dose [62] to 20 weeks [66]. Frequency of intervention delivery was not clearly described by two studies [64, 66], however, it varied widely between the remaining studies from daily [50,51,52, 63], once a week [53,54,55, 58, 61], twice a week [56, 59], or multiple times a week [57, 60, 65].
Some studies used a virtual approach to deliver the intervention (using online platforms for example to deliver sessions or a virtual clinic) [54, 55, 60, 61, 64, 66]. One study used an artificial intelligence-based intervention to deliver a personalised care approach [60].
Description of study outcomes
Outcome measures are described in Table 4. Mental health outcomes included anxiety, depression, stress, sleep, neuropsychological functioning, and wellbeing. The timing of outcome measures was reported by all studies except one. Most studies used pre- and post-intervention measures, with additional follow-ups.
The most commonly reported questionnaires for anxiety and depression were the Hospital Anxiety and Depression Scale (n = 3), the Generalized Anxiety Disorder-7 (n = 2) and the Patient Health Questionnaire-9 (n = 3). The Short-Form-36 questionnaire was mostly reported for measuring health-related QoL (n = 4). Other studies used a wide array of scales and measures, as detailed in Table 4.
Description of study findings
Table 5 provides a description of study findings. Positive findings were reported by all studies. Nine studies reported significant improvements in different outcomes following the intervention [50,51,52, 55, 57, 60, 61, 63, 65], of which five are trials [50,51,52, 60, 61].
Some of the interventions used by these studies included using drug products i.e., Cholytilin and MexiB 6 for anxiety and depression, Intravenous Cytoflavin in combination with a standard rehabilitation program for depression, Anvifen for anxiety, depression, health-related QoL and sleep. Significant improvements were reported on these outcomes. Other studies examined wellbeing services or rehabilitation programs, such as Multidisciplinary Rehabilitation (MDR) for anxiety, depression and health-related QoL, and Primary Care Wellbeing Service (PCWBS) for general health and health-related QoL, with both showing significant improvement in these outcomes. Neuropsychological programmes included cognitive treatment, together with other respiratory and physiotherapy, for anxiety and depression, that were significantly improved. An English National Opera (ENO) programme that was delivered online and was focused on breathing re-training through singing techniques and utilising lullabies, was used to assess health-related QoL with significant improvement only reported to the mental health composite score. Another intervention included using a high-fibre formula examined anxiety that was reported to be significantly improved. Lastly, a neurofeedback (NFB) program that included locating electrodes on the right and left temporal lobes to examine anxiety and depression, with significant improvements reported. (See Tables 3, 4 and 5 for more details).
Discussion
Summary of main results
To the best of our knowledge, this is the first scoping review focused on interventions tested for their impact on mental health issues associated with LC. Seventeen studies were identified, with a wide range of recruitment methods, number of participants recruited, intervention tested, duration of the intervention, practitioners involved in delivering the intervention, outcome measures, and post intervention follow up. Various tools were employed to measure a wide range of outcomes. Results were generally positive, with all included studies reporting improvements in mental health outcomes. However, as most studies were case reports, which are known to be of low-quality evidence compared to RCTs and cohort studies [67], the findings of these studies should be interpreted with caution.
Recruitment and participants
All participants recruited into the included studies were reported to have LC. However, it was not clear in some studies how long participants had been suffering from LC or when they had their acute COVID-19 infection. These participants may have varied with regard to their LC diagnosis, and the duration of time since they had acute COVID-19 infection. The lack of a consistent definition of LC resulted in a heterogeneous sample of participants joining research at different stages of their illness. This might have implications on the impact of the interventions, and the number of symptoms and symptom severity. Therefore, future research needs to take this into consideration and also interrogating whether interventions have different impacts at the different stages of the LC journey.
The over-representation of women and older participants reflects the literature indicating that these are risk factors for LC [26, 28, 68]. However, some studies indicate that people from minority ethnic backgrounds are more likely to acquire a COVID-19 infection compared to the general population [69,70,71].
Thus, the lack of ethnic diversity in studies in this review leaves a knowledge gap and suggests particular attention be given to ethnic and cultural diversity in future studies.
Outcomes and outcome measures
Mental health was assessed in multiple ways, mostly focusing on anxiety and depression, with a number of studies also considering QoL. This reflects the broad nature of mental health and that it encompasses multiple aspects of people’s physical, social and psychological life [72]. A wide range of measures were adopted, making cross-study comparison difficult. Researchers might consider using a standardised core outcome set to enhance the comparability of outcomes in future research, as suggested in a recent Delphi consensus study [73]. Additionally, from a patient and public engagement standpoint [74], people with LC could support future trials throughout the research process, including in selecting the best questionnaires to use for the targeted outcome in manners that resonate with their lived experience. Almost all studies assessed targeted outcomes before and after the intervention, with few studies conducting further follow-up measurements to follow progress over time. The addition of follow-up assessments in future research is of high importance, as this would allow researchers to identify the longer-term impact of their intervention [75].
Interventions and findings
Although this review included only interventions targeting the mental health of patients with long COVID, a wide range of interventions was described. Some interventions were of specific pharmacologic products or looked at dietary change. However, the majority of studies used an integrated approach to try to address the different elements of participants’ mental health and QoL. Most integrated treatments were delivered by a multidisciplinary team and patients needed to take active roles in implementing agreed therapeutic strategies.
Given the heterogeneity of interventions described, no specific ‘standard’ treatment can be delineated. However, our review suggests that a wide variety of interventions have the potential to support mental health of individuals with LC. and a variety of integrated care models have been examined.
All interventions used by studies in this review were associated with positive outcomes. However, considering study designs of most included studies, the findings should be interpreted cautiously. More large-scale, high-quality trials are needed to define effective intervention strategies for LC. As LC presentation varies between individuals, interventions addressing a wide range of symptoms including mental health and QoL could be promising in building the evidence base.
Strengths and limitations
The findings of this scoping review contribute to the body of knowledge on LC. Strengths of the review include: 1) Adherence to the PRISMA-ScR (Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews) guidelines [45], including the widest available evidence through a combination of complementary keywords to search all related databases and was also covering grey literature and the reference lists of all included studies and related reviews; 2) no language restrictions - all retrieved studies in different languages were examined, translated, and included; and 3). Selection bias was minimised by having two independent reviewers conducting the title, abstract and full text screening, with a sample of data extraction being reviewed by a third person.
However, some limitations were encountered with this review. There was missing data from some included studies despite attempts to contact corresponding authors, which precluded rigorous comparisons being made. Another limitation was related to the search strategy, which was limited to studies where mental health was the primary outcome. This may have led to missing some important interventions that may have had positive impacts on mental health as a secondary outcome.
Conclusions
A wide range of interventions designed to support mental health in patients with long COVID has been examined. Overall, these interventions reported positive effects on mental health outcomes, though more research is needed to confirm this. Considering the ongoing nature of LC and treatment recommendations to date, it is important to address patients’ care needs holistically, ideally through using an integrated care approach.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
Abbreviations
- BDI-II:
-
Beck Depression Inventory-II
- BAI:
-
Beck Anxiety Inventory
- BRS:
-
Brief Resilience Scale
- CADTH:
-
Canadian Agency for Drug and Technologies in Health
- CBT:
-
Cognitive Behavioural Therapy
- DASS-21:
-
Depression, Anxiety and Stress Scale-21
- EQ-5D-5L:
-
Euro-Qol 5 dimensions 5 levels
- GAD-7:
-
Generalized Anxiety Disorder-7
- FAS:
-
Fatigue Assessment Scale
- HADS:
-
Hospital Anxiety and Depression Scale
- HDRS:
-
Hamilton Depression Rating Scale
- LC:
-
Long COVID
- NICE:
-
National Institute for Health and Care Excellence
- NR:
-
Not reported
- PHQ-9:
-
Patient Health Questionnaire 9 items
- PRISMA-ScR:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews
- PSS-10:
-
Perceived Stress Scale-10
- RCT:
-
Randomised Controlled Trial
- SCIE:
-
Social Care Institute for Excellence
- SF-12:
-
12-Item Short Form Survey
- SF-36:
-
36-Item Short Form Survey
- WAM:
-
Wellbeing, Activity and Mood questionnaire
- WHHQ-18:
-
Warwick Holistic Health Questionnaire
- WHO:
-
World Health Organisation
- Zung SRDS:
-
Self-Rating Depression Scale
- Zung SRAS:
-
Self-Rating Anxiety Scale
- QoL:
-
Quality of life
References
Kong WH, Li Y, Peng MW, Kong DG, Yang XB, Wang L, et al. SARS-CoV-2 detection in patients with influenza-like illness. Nat Microbiol. 2020;5(5):675–8.
WHO. WHO Coronavirus (COVID-19) Dashboard. 2021. Available from: https://covid19.who.int/.
CIPD. Working with long COVID: research evidence to inform support. London: Chartered Institute of Personnel and Development; 2022.
NIHR. Researching long COVID: addressing a new global health challenge: NIHR; 2022. Available from: https://doi.org/10.3310/nihrevidence_50331.
Callard F, Perego E. How and why patients made Long Covid. Soc Sci Med. 2021;268:113426.
Stengel A, Malek N, Zipfel S, Goepel S. Long Haulers—What is the evidence for post-COVID fatigue? Front Psychiatry. 2021;12:677934.
Lopez-Leon S, Wegman-Ostrosky T, Perelman C, Sepulveda R, Rebolledo PA, Cuapio A, et al. More than 50 long-term effects of COVID-19: a systematic review and meta-analysis. Sci Rep. 2021;11:16144.
Raveendran AV, Jayadevan R, Sashidharan S. Long COVID: an overview. Diabetes Metab Syndr. 2021;15(3):869–75.
Munblit D, O’Hara ME, Akrami A, Perego E, Olliaro P, Needham DM. Long COVID: aiming for a consensus. Lancet Respir Med. 2022;10:632–4.
NICE 2021. COVID-19 rapid guideline: managing the long-term effects of COVID-19. COVID-19 rapid guideline: managing the long-term effects of COVID-19. National Institute for Health and Care Excellence (NICE), Scottish Intercollegiate Guidelines Network (SIGN) and Royal College of General Practitioners (RCGP). NICE guideline [NG191]. Available from: https://nice.org.uk/ng188.
WHO. A clinical case definition of post COVID-19 condition by a Delphi consensus, 6 October 2021. World Health Organization; 2021.
Wu Y, Xu X, Chen Z, Duan J, Hashimoto K, Yang L, et al. Nervous system involvement after infection with COVID-19 and other coronaviruses. Brain Behav Immun. 2020;87:18–22.
Disser NP, De Micheli AJ, Schonk MM, Konnaris MA, Piacentini AN, Edon DL, et al. Musculoskeletal consequences of COVID-19. J Bone Joint Surg Am. 2020;102(14):1197.
Ellul MA, Benjamin L, Singh B, Lant S, Michael BD, Easton A, et al. Neurological associations of COVID-19. Lancet Neurol. 2020;19(9):767–83.
Komaroff AL, Bateman L. Will COVID-19 lead to myalgic encephalomyelitis/chronic fatigue syndrome? Front Med. 2021;7:606824.
Wostyn P. COVID-19 and chronic fatigue syndrome: Is the worst yet to come? Med Hypotheses. 2021;146:110469.
Kingstone T, Taylor AK, O’Donnell CA, Atherton H, Blane DN, Chew-Graham CA. Finding the ‘right’ GP: a qualitative study of the experiences of people with long-COVID. BJGP Open. 2020;4(5):bjgpopen20X101143.
Ladds E, Rushforth A, Wieringa S, Taylor S, Rayner C, Husain L, et al. Developing services for long COVID: lessons from a study of wounded healers. Clin Med. 2021;21(1):59.
Chandu VC, Marella Y, Panga GS, Pachava S, Vadapalli V. Measuring the impact of COViD-19 on mental health: a scoping review of the existing scales. Indian J Psychol Med. 2020;42(5):421–7.
Lei L, Huang X, Zhang S, Yang J, Yang L, Xu M. Comparison of prevalence and associated factors of anxiety and depression among people affected by versus people unaffected by quarantine during the COVID-19 epidemic in Southwestern China. Med Sci Monit. 2020;26:e924609–11.
Tang W, Hu T, Hu B, Jin C, Wang G, Xie C, et al. Prevalence and correlates of PTSD and depressive symptoms one month after the outbreak of the COVID-19 epidemic in a sample of home-quarantined Chinese university students. J Affect Disord. 2020;274:1–7.
Wang C, Pan R, Wan X, Tan Y, Xu L, McIntyre RS, et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav Immun. 2020;87:40–8.
Aiyegbusi OL, Hughes SE, Turner G, Rivera SC, McMullan C, Chandan JS, et al. Symptoms, complications and management of long COVID: a review. J R Soc Med. 2021;114(9):428–42.
Michelen M, Cheng V, Manoharan L, Elkheir N, Dagens D, Hastie C, et al. What are the long-term symptoms and complications of COVID-19: a protocol for a living systematic review. F1000Res. 2020;9:1455.
Tenforde MW, Kim SS, Lindsell CJ, Rose EB, Shapiro NI, Files DC, et al. Symptom duration and risk factors for delayed return to usual health among outpatients with COVID-19 in a multistate health care systems network—United States, March–June 2020. MMWR. 2020;69(30):993.
Chen C, Haupert SR, Zimmermann L, Shi X, Fritsche LG, Mukherjee B. Global prevalence of post-COVID 19 condition or long COVID: a meta-analysis and systematic review. J Infect Dis. 2022;226:1593–607.
Stewart C. Long COVID in the United Kingdom (UK) - statistics & facts: Statista; 2022. Available from: https://www.statista.com/topics/8340/long-covid-in-the-uk/#dossierKeyfigures.
Nabavi N. Long covid: How to define it and how to manage it. BMJ. 2020;370:m3489.
Ladds E, Rushforth A, Wieringa S, Taylor S, Rayner C, Husain L, et al. Persistent symptoms after Covid-19: qualitative study of 114 “long Covid” patients and draft quality principles for services. BMC Health Serv Res. 2020;20(1):1–13.
Aucott JN, Rebman AW. Long-haul COVID: heed the lessons from other infection-triggered illnesses. Lancet. 2021;397(10278):967–8.
Davis HE, Assaf GS, McCorkell L, Wei H, Low RJ, Re’em Y, et al. Characterizing long COVID in an international cohort: 7 months of symptoms and their impact. EClinMed. 2021;38:101019.
Huang C, Huang L, Wang Y, Li X, Ren L, Gu X, et al. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet. 2021;397(10270):220–32.
Logue JK, Franko NM, McCulloch DJ, McDonald D, Magedson A, Wolf CR, et al. Sequelae in adults at 6 months after COVID-19 infection. JAMA Netw Open. 2021;4(2):e210830-e.
Penninx BWJH. Psychiatric symptoms and cognitive impairment in “Long COVID”: the relevance of immunopsychiatry. World Psychiatry. 2021;20(3):357.
Hawke LD, Nguyen ATP, Ski CF, Thompson DR, Ma C, Castle D. Interventions for mental health, cognition, and psychological wellbeing in long COVID: a systematic review of registered trials. Psychol Med. 2022;52(13):2426–40.
Houben-Wilke S, Goërtz YMJ, Delbressine JM, Vaes AW, Meys R, Machado FVC, et al. The impact of long COVID-19 on mental health: observational 6-month follow-up study. JMIR Mental Health. 2022;9(2):e33704.
Chandan JS, Brown KR, Simms-Williams N, Bashir NZ, Camaradou J, Heining D, et al. Non-pharmacological therapies for post-viral syndromes, including Long COVID: a systematic review. Int J Environ Res Public Health. 2023;20(4):3477.
Alwan NA. The road to addressing Long Covid. Science. 2021;373(6554):491–3.
Taribagil P, Creer D, Tahir H. ‘Long COVID’ syndrome. BMJ Case Rep. 2021;14(4):e241485.
Blomberg B, Cox RJ, Langeland N. Long COVID: a growing problem in need of intervention. Cell Rep Med. 2022;3(3):100552.
Brown K, Yahyouche A, Haroon S, Camaradou J, Turner G. Long COVID and self-management. Lancet. 2022;399(10322):355.
NHS England. Post-COVID syndrome (long COVID). 2021. Available from https://www.england.nhs.uk/coronavirus/post-covid-syndrome-long-covid/.
PULSE. Management of long Covid in primary care: PULSE; 2022. Available from: https://www.pulsetoday.co.uk/covid-19-primary-care-resources/guides/testing-trials-and-research/management-of-long-covid-in-primary-care/.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73.
Covidence systematic review software. Better systematic review management Melbourne, Australia: Veritas Health Innovation; 2022. Available from: www.covidence.org.
Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18(1):1–7.
Pollock D, Davies EL, Peters MDJ, Tricco AC, Alexander L, McInerney P, et al. Undertaking a scoping review: a practical guide for nursing and midwifery students, clinicians, researchers, and academics. J Adv Nurs. 2021;77(4):2102–13.
Coyle A, Lyons E. Analysing qualitative data in psychology. London: Sage; 2021. ISBN 9781412907828.
Esin RG, Khayrullin IK, Esin OR, Malova LA, Alimbekova LR. Effectiveness of the anxiolytic Anvifen in the treatment of post-COVID brain fog. Zh Nevrol Psikhiatr Im S S Korsakova. 2022;122(8):101–5.
Bogolepova AN, Osinovskaya NA, Kovalenko EA, Makhnovich EV. Fatigue and cognitive impairment in post-COVID syndrome: possible treatment approaches. [Russian]. Nevrol Neiropsikhiatr Psikhosomatika. 2021;13(4):88–93.
Tereshin AE, Kiryanova VV, Reshetnik DA. Correction of mitochondrial dysfunction in the complex rehabilitation of COVID-19. Zh Nevrol Psikhiatr Im S S Korsakova. 2021;121(8):25–9.
Brodsky M. Post-COVID-19 long hauler clinical program: change in health-related quality-of-life. Glob Adv Health Med. 2021;10:21649561211059080.
Fowler-Davis S, Young R, Maden-Wilkinson T, Hameed W, Dracas E, Hurrell E, et al. Assessing the acceptability of a co-produced long COVID intervention in an underserved community in the UK. Int J Environ Res Public Health. 2021;18(24):14.
Harenwall S, Heywood-Everett S, Henderson R, Godsell S, Jordan S, Moore A, et al. Post-Covid-19 syndrome: improvements in health-related quality of life following psychology-led interdisciplinary virtual rehabilitation. J Prim Care Community Health. 2021;12:21501319211067670.
Łuckoś M, Cielebak K, Kaminski P. EEG neurofeedback in the treatment of cognitive dysfunctions after the infection of SARS-COV-2 and long COVID-19. Acta Neuropsychologica. 2021;19(3):361–72.
Compagno S, Palermi S, Pescatore V, Brugin E, Sarto M, Marin R, et al. Physical and psychological reconditioning in long COVID syndrome: results of an out-of-hospital exercise and psychological - based rehabilitation program. IJC Heart Vasc. 2022;41:101080.
Brough DN, Abel S, Priddle L. A service evaluation of a community project combining psychoeducation and mind-body complementary approaches to support those with long covid in the UK. Eur J Integr Med. 2022;55:102182.
Wagner B, Steiner M, Markovic L, Crevenna R. Successful application of pulsed electromagnetic fields in a patient with post-COVID-19 fatigue: a case report. Wien Med Wochenschr. 2022;172(9–10):227–32.
Garcia-Molina A, Garcia-Carmona S, Espina-Bou M, Rodriguez-Rajo P, Sanchez-Carrion R, Ensenat-Cantallops A. Neuropsychological rehabilitation for post-COVID-19 syndrome: results of a clinical program and six-month follow up. Neurologia. 2022:S2173-5808(22)00094-3.
Philip KEJ, Owles H, McVey S, Pagnuco T, Bruce K, Brunjes H, et al. An online breathing and wellbeing programme (ENO Breathe) for people with persistent symptoms following COVID-19: a parallel-group, single-blind, randomised controlled trial. Lancet Respir Med. 2022;10(9):851–62.
Tobinick E, Spengler RN, Ignatowski TA, Wassel M, Laborde S. Rapid improvement in severe long COVID following perispinal etanercept. Curr Med Res Opin. 2022;38:2013–20.
Wang Y, Wu G, Zhao L, Wang W. Nutritional modulation of gut microbiota alleviates severe gastrointestinal symptoms in a patient with post-acute COVID-19 syndrome. mBio. 2022;13(2):e0380121.
Skilbeck L. Patient-led integrated cognitive behavioural therapy for management of long COVID with comorbid depression and anxiety in primary care - a case study. Chronic Illn. 2022;18(3):691–701.
Orendáčová M, Kvasnak E, Vranova J. Effect of neurofeedback therapy on neurological post-COVID-19 complications (A pilot study). PLoS One. 2022;17(7):e0271350.
Koliadenko NV, Zhyvago KS, Bursa AI. Provision of medical-psychological and psychiatric care to patients with post-covid syndrome in telemedicine conditions. Bangladesh J Med Sci. 2022;21(4):719–30.
Medical College of Wisconsin. Evidence-based practice: study designs & evidence levels. Milwaukee: MCW Libraries; 2023.
Cabrera Martimbianco AL, Pacheco RL, Bagattini ÂM, Riera R. Frequency, signs and symptoms, and criteria adopted for long COVID: a systematic review. Int J Clin Pract. 2021;75:e14357.
Kirby T. Evidence mounts on the disproportionate effect of COVID-19 on ethnic minorities. Lancet Respir Med. 2020;8(6):547–8.
NHS Digital. Ethnicity and outcomes of coronavirus (COVID-19) patients in England. 2020. Available from: https://digital.nhs.uk/coronavirus/coronavirus-data-services-updates/ethnicity-and-outcomes-of-covid-19-patients-in-england.
Tai DBG, Shah A, Doubeni CA, Sia IG, Wieland ML. The disproportionate impact of COVID-19 on racial and ethnic minorities in the United States. Clin Infect Dis. 2021;72(4):703–6.
Galderisi S, Heinz A, Kastrup M, Beezhold J, Sartorius N. Toward a new definition of mental health. World Psychiatry. 2015;14(2):231.
Munblit D, Nicholson T, Akrami A, Apfelbacher C, Chen J, De Groote W, et al. A core outcome set for post-COVID-19 condition in adults for use in clinical practice and research: an international Delphi consensus study. Lancet Respir Med. 2022;10:715–24.
NHS Health Research Authority. Public involvement. NHS Health Research Authority; 2022.
Ssekamatte D, Okello SM. Using baseline studies as a basis for monitoring and evaluation: a review of the literature. Uganda J Manag Public Policy Stud. 2016;11:1.
Acknowledgements
The authors thank Jennifer Coe, a member of the Long COVID Patient and Public advisory group, for reviewing this paper and offering helpful comments.
Funding
This study was funded by the NHS Norfolk and Waveney Integrated Care Board.
Author information
Authors and Affiliations
Contributions
HA, LDH and CFS contributed to the design of the review. HA and LDH participated in the methodology and analysis. HA drafted the manuscript. All authors were all involved in data extraction. All authors critically reviewed the manuscript and agreed on the final version before submission and take responsibility for its content.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable
Consent for publication
Not applicable
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Example of search strategy using Medline.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Al-Jabr, H., Hawke, L.D., Thompson, D.R. et al. Interventions to support mental health in people with long COVID: a scoping review. BMC Public Health 23, 1186 (2023). https://doi.org/10.1186/s12889-023-16079-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-023-16079-8