Abstract
Introduction
Cardiovascular disease (CVD) is a major health concern worldwide, particularly in low- and middle-income countries. The COVID-19 pandemic that emerged in late 2019 may have had an impact on the trend of CVD mortality. This study aimed to investigate the trend and changes in CVD mortality rates in Malaysia, using age-standardized mortality rates (ASMR) from 2010 to 2021.
Methods
The Malaysian population and mortality data from 2010 to 2021 were obtained from the Department of Statistics Malaysia (DOSM). ASMRs from CVD per 100,000 population were calculated based on the World Health Organization (2000–2025) standard population using the direct method. The ASMRs were computed based on sex, age groups (including premature mortality age, 30–69 years), and CVD types. The annual percent change (APC) and average annual percent change (AAPC) of the ASMR with corresponding 95% confidence intervals (95% CI) were estimated from joinpoint regression model using the Joinpoint Regression Program, Version 4.9.1.0.
Results
Throughout the study period (2010–2021), ASMRs for CVD exhibited an increase from 93.1 to 147.0 per 100,000, with an AAPC of 3.6% (95% CI: 2.1 to 5.2). The substantial increase was observed between 2015 and 2018 (APC 12.6%, 95% CI: 5.4%, 20.3%), with significant changes in both sexes, and age groups 50–69, 70 years and over, and 30–69 (premature mortality age). Notably, the ASMR trend remained consistently high in the premature mortality age group across other age groups, with males experiencing higher rates than females. No significant changes were detected before or after the COVID-19 pandemic (between 2019 and 2021), except for females who died from IHD (10.3% increase) and those aged 0–4 (25.2% decrease).
Conclusion
Overall, our analysis highlights the persistently high burden of CVD mortality in Malaysia, particularly among the premature mortality age group. These findings underscore the importance of continued efforts to address CVD risk factors and implement effective prevention and management strategies. Further research is needed to fully understand the impact of the COVID-19 pandemic on CVD mortality rates and to inform targeted interventions to reduce the burden of CVD in Malaysia.
Similar content being viewed by others
Background
Cardiovascular disease (CVD) is the leading cause of death worldwide, responsible for approximately one-third of all deaths globally [1, 2]. Low- and middle-income countries (LMICs) bear a disproportionate burden of CVD, accounting for 32% of all CVD deaths [3]. Despite declining age-standardized mortality rates (ASMR) in high-income regions, most LMICs have not experienced similar reductions [4, 5]. Instead, there has been an increase in premature mortality (deaths that occur at a younger age than expected) from CVD in LMICs [6]. Recognizing this alarming trend, there is a global commitment to reducing premature CVDs by 25% by the year 2025 [7]. While significant progress has been made in preventing and treating CVD, there are notable disparities among different subpopulations, and the trend for CVD mortality has been inconsistent globally [5, 8,9,10,11,12]. Malaysia, classified as an LMIC, also faces a significant burden of CVD, particularly ischemic heart disease (IHD) and stroke [13].
Changes in CVD mortality trends can be attributed to several factors. Adverse conditions or behaviours related to modifiable risk factors such as diabetes, obesity, lack of physical activity, hypertension, an unhealthy diet, smoking, and excessive alcohol consumption are associated with an increase in CVD mortality trends [4, 14,15,16]. Without reducing these risk factors, it is predicted that almost 23.6 million people will die from CVDs by 2030 [17]. Other factors, including an aging population [18], environmental factors [19], and changes in healthcare access and quality [15], may contribute to these disparities in the trend for CVD mortality.
In addition to these factors, the COVID-19 pandemic, which began in late December 2019 [20] has had a significant impact on the healthcare system and may have affected the trend for CVD mortality. For example, the pandemic resulted in excess all-cause mortality in the USA [21] and in a multi-country study using data from 74 countries worldwide [22]. In Poland, in-hospital mortality for acute heart failure increased [23], whereas in Sweden, CVD mortality, particularly from IHD and myocardial infarction, decreased substantially during 2020 [24]. Several countries reported a decrease in hospitalizations and percutaneous coronary interventions during the COVID-19 pandemic, likely leading to a reduction in recorded mortality from cardiac events [25,26,27]. Lockdowns and prioritization of COVID-19 care may have indirectly affected diseases like CVDs that require a functional healthcare system [28, 29]. Thus, analysing mortality trends allows for understanding the indirect impacts of the pandemic on health outcomes, identifying gaps in healthcare delivery, and developing strategies to mitigate these impacts.
Joinpoint analysis is a statistical method that is commonly used to detect changes in trends or patterns in data over time, and it has been used in many previous studies to investigate the burden of various diseases, including CVD [30,31,32,33]. Investigating the trend for CVD mortality within a country is crucial, particularly in LMICs like Malaysia. However, to date, the trend and any change in trend of ASMR from CVD in Malaysia have not been investigated over the past decade, including the impact of COVID-19 on CVD mortality rates. Using joinpoint analysis to analyse Malaysian data will provide valuable insights into the temporal patterns of CVD mortality occurrence in Malaysia and help inform policy and intervention strategies to reduce the burden of CVD in the country. Moreover, it will contribute to the literature on CVD mortality trends and change point analysis, particularly in LMICs, and provide a basis for future studies on CVD mortality in the region. Therefore, this study aims to explore the change in trend of ASMR from CVD in Malaysia from 2010 to 2021. Specifically, we aim to identify any changes in trends according to sex, major CVD types, and age group, including premature mortality. Furthermore, we aim to assess any changes in the CVD mortality trend within each subgroup before and after the COVID-19 pandemic.
Methods
Source of data
Data on CVD mortality and Malaysian population (census and inter-census years) were obtained from the Department of Statistics Malaysia (DOSM) for the period 2010–2021. Malaysian law mandates that all deaths be registered with the National Registration Department (NRD), which issues death certificates [34]. Deaths in Malaysia are categorized into medically certified deaths, which occur in health facilities and are determined by medical officers based on symptoms and examination, and non-medically certified deaths, which occur outside health facilities. While death registration quality is an issue in many countries [35]. Malaysia stands out as one of the few Asian countries with a functioning vital registration system. Analysing trends from 1995 to 2010, medically certified deaths increased over time, while non-medically certified deaths remained stable [36]. In 1995, non-medically certified deaths were 55%, surpassing medically certified deaths at 45% [36]. In 2021, DOSM reported an improvement, with medically certified deaths at 70.0% and non-medically certified deaths at 30.0% [37]. In Malaysia, death certificates document a clear sequence of events leading to death. The cause of death listed on the lowermost line of the sequence, which initiated the train of events leading to death, is defined as the underlying cause of death. All other causes listed on the lines between the underlying cause (on the lowermost line) and the immediate cause (on the topmost line) are referred to as antecedent causes of death [38]. DOSM is responsible for cleaning and classifying cause-of-death information for all medically certified deaths obtained from the NRD, coding them based on the 10th International Classification of Diseases (ICD-10) [39]. This process is carried out by specialized coders at DOSM. To ensure the study’s quality and enhance the accuracy of cause-of-death information, only medically certified deaths for CVD as indicated by ICD-10 (code I01-I99) were used for this analysis. The unknown cause of death and missing information on age and sex were excluded.
Statistical analysis
We estimated ASMRs per 100,000 population for all medically certified deaths from CVD. The World (WHO 2000–2025) Standard population [40] was used as the reference population to calculate ASMR, based on the direct method of age-standardization. The use of a standard population is important to enable comparability between relevant years and rates from other countries. To calculate the ASMR using direct standardization, we first aggregated the number of CVD deaths into 5-year age intervals (0–4, 5–9, 10–14, 15–19, 20–24, 25–29, 30–34, 35–39, 40–44, 45–49, 50–54, 55–59, 60–64, 65–69, 70–74, 75–79 and 80+) for each year of study. Next, we calculated the age-specific mortality rates by dividing the number of deaths in a specific age group by the number of people in that age group and then multiplying the result by 100,000. Finally, the ASMR was calculated by multiplying the age-specific death rate by the weight of that age group in the standard population [40]. This direct standardization method was applied to calculate the overall ASMR, and stratified by gender (male and female), CVD type (IHD and stroke), and selected specific age ranges (e.g., 0–1, 30–49, 50–59 years). To explore the trend for premature CVD mortality, we also selected a specific age group of 30–69 years, in accordance with the WHO definition of premature mortality [41]. The descriptive statistics of ASMR and trend plots were analysed using R software.
Joinpoint regression analysis was utilized to detect the significant changes in annual ASMR for CVD mortality from 2010 to 2021 according to sex, age groups and CVD types. A joinpoint regression model was employed to estimate the magnitude of change in the trend of CVD mortality rates over time. This model allows us to identify points in time, where significant changes occur in the trend. Additionally, the model provides a confidence measure around these estimated changes. We used the Joinpoint Regression Program, Version 4.9.1.0 for this analysis [42]. The Joinpoint program fits a series of straight lines to the ASMRs on a log scale and detects the best fitting points, called ‘joinpoints’ [43]. This program selects the final model using two methods; the Monte Carlo permutation tests and the Bayesian Information Criterion (BIC) [43]. The analysis starts with the minimum number of joinpoints (e.g., zero joinpoints, which is a straight line), and tests whether one or more joinpoints are significant and must be added to the model. Based on the recommendation of the Joinpoint program, a maximum of two joinpoints can be selected for the given 12 data points [42]. Permutation tests determine the number of joinpoints by comparing different hypotheses until the final number is reached. Starting with ka = minimum number of joinpoint and kb = maximum number of joinpoint, each test compares the null hypothesis H0: number of joinpoints = ka against the alternative Ha: number of joinpoints = kb, where ka < kb. If the null hypothesis is rejected, ka is increased by 1; otherwise, kb is decreased by 1. This process continues until ka = kb, and the final value is the selected number of joinpoints. Then, models with this number of joinpoints are compared using BIC, and the model with the minimum BIC value is selected as the optimal model [44].
To describe changes in CVD mortality rates, the annual percent change (APC) of the ASMR between the trend-change point and the average annual percent change (AAPC) in the whole period studied was calculated with corresponding 95% confidence intervals (95% CI). We applied the log transformation to calculate the APC. This approach assumes that CVD mortality rates change at a constant percentage relative to the rate of the previous year, and the log transformation allows for linear changes on a logarithmic scale. To derive the APC for a given data series, the following regression model is employed [45];
where \(\text{log}\left({R}_{y}\right)\) is the natural log of the rate in year \(y\). \({b}_{0}\)is the intercept, representing the value of the natural log of the rate when \(y=0,\) and \({b}_{1}\) is the slope, indicating the rate of change in the natural log of the rate per year.
The APC from year \(y\) to year \(y\) + 1 is derived from this formula
The formula is further transformed to represent an annual percent change;.
The AAPC was calculated to summarize the trend over a specific fixed interval (2010–2021), allowing for the use of a single number to describe the APCs over multiple years. The AAPC is computed by taking a weighted average of the APCs from the joinpoint model, with the weights determined by the length of each APC interval. The AAPC over any fixed interval is calculated by taking a weighted average of the slope coefficients of the underlying joinpoint regression model, where the weights correspond to the length of each segment within the interval [46].
APCi = {exp(bi) − 1} x 100.
where bi is the slope coefficient for the ith segment (within the desired range of years).
In the calculation, the weighted average of slope coefficients is further transformed to represent an average annual percent change [46];
where wi is the length of each segment within that range.
The Joinpoint Regression Program performs a series of hypothesis tests. These tests compare the null hypothesis (the assumption of no trend or no joinpoints) against alternative hypotheses with different numbers of joinpoints. A small p-value indicates strong evidence against the null hypothesis, suggesting significant trends or joinpoints. The trend was considered to be significantly increasing (positive change) or decreasing (negative change) when the p-value was below 0.05 (p < 0.05).
Results
Table 1 shows the demographic structure of the Malaysian population and the age standardized mortality rate from CVD. The Malaysian population is systematically increasing for the period 2010–2021 from 28.6 million to 32.6 million [47]. During the observed period, 1.9 million deaths (from all causes) were recorded in Malaysia, of which 318,268 deaths (16.6%) were caused by CVD.
Age standardised mortality rate
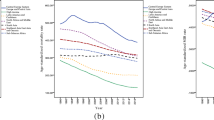
The ASMR ranged from 88.1 to 147.0 per 100,000 population (Table 1). The overall ASMR showed an increase trend from 93.1 to 147.0 deaths per 100,000 population from 2010 to 2021, but with small variation between years. During the study period, the rates were almost twice as high in men as in women. The trend shown increases in both sexes and the main CVD types (IHD and stroke). Although all of the rates increased over the period of study, the pattern of increase varied across age groups. Figure 1 shows that the ASMR trend in males was highest among those aged 30–69 years (defined as premature mortality), whereas in females, the highest rate was observed in those over 70 years of age. We detected that the trend for both sexes was rising and peaking in 2018, particularly among the premature mortality age group and those over 50. Meanwhile, the mortality trend among adolescents and children below the age of 15 for both sexes has almost plateaued over the years.
Joinpoint regression model
Table 2 shows the joinpoint regression analysis of ASMR for total CVD and the model for both sexes stratified by age group and CVD type. The jointpoint model demonstrated a statistically significant increase in ASMR for CVD, with an AAPC of 3.6% (95% CI: 2.1, 5.2) during the entire study period (2010 to 2021). However, when we looked at a specific segment, the trend was slightly decreasing between 2010 and 2015, with an APC of -2.2% (95% CI: -3.6, -0.7), and a substantial increase between 2015 and 2018, with an APC of 12.6% (95% CI: 5.4, 20.3). Between 2018 and 2021, the rate increased slightly (APC: 5.0%, 95% CI: 1.6%, 8.6%), and no significant changes were detected before or after the COVID-19 pandemic (2019–2021). These changes in ASMRs exhibited similar patterns in both men and women, with large increments occurring between 2015 and 2018.
The analysis of trends by age strata (Table 2) demonstrated the large increase between 2015 and 2018 was contributed by the age groups 50–59, ≥ 70 years, and premature mortality group, with APCs of 9.5%, 16.7%, and 9.3%, respectively. Meanwhile, the reduction in trend between 2010 and 2015 was notable among females aged 50–69 (reduced by -2.3%) and both male and female aged ≥ 70 age groups (reduced by -3.6% in females and − 3.9% in males). Interestingly, among premature CVD mortality (age 30–69), the trend was systematically increasing throughout the study period, where the reduction slopes between 2010 and 2015 were not statistically significant. In addition, the AAPC during the observed study (2010–2021) only significantly increased among the aged group over 30 years. Meanwhile, the mortality rate in the age group below 30 years was nearly constant, and the trend in this subgroup was not statistically significant, except for those aged 0–4 years, who showed a significant decline in trend (reduced by 25.5%) from 2019 to 2021. Figures 2 and 3 present the joinpoint model plots illustrating the overall ASMR trend from CVD, as well as the trends by sex and age group.
In terms of CVD subtype, both IHD and stroke showed an upward trend between 2010 and 2021, with AAPC rates of 3.9% and 3.4%, respectively (Table 2). Although females reported lower ASMR from IHD and stroke than males, females had a greater increase in trend for IHD and stroke. Specifically, the AAPC for females was 4.5% for IHD and 3.6% for stroke, whereas for males it was 3.8% for IHD and 3.3% for stroke.
During the period from 2019 to 2021, which encompasses the pre- and post-COVID-19 pandemic eras, our joinpoint analysis revealed significant changes in CVD mortality rates among females. Specifically, there was a notable increase in the mortality rate due to IHD among females, with an APC of 10.3%. Additionally, there was a significant decrease in mortality among female children aged 0–4, with an APC of -25.2%. However, it’s important to note that significant changes among males were detected between 2018 and 2021, which falls outside the defined pre- and post-COVID-19 pandemic period of 2019–2021.
Discussion
In this study, we conducted joinpoint analysis to identify and measure temporal patterns of ASMR on CVD mortality in Malaysia from 2010 to 2021. These analytical methods proved useful in understanding the underlying drivers of the observed trends and their implications for policies and interventions. Our findings indicated an overall increase in ASMR from CVD over the study period (AAPC of 3.6%) with a large increment occurring between 2015 and 2018 (APC of 12.6%). Interestingly, we detected a slight decrease in the trend between 2010 and 2015 (APC of -2.2%). This descending trend in CVD mortality aligns with other reports worldwide. For example, the findings from the GBD Study 2017 reported that nearly all countries, including developing countries and regions like Southeast Asia, experienced a significant declining trend in age-standardized CVD mortality rates from 1990 to 2017 [48]. A study by Khan et al. revealed that the global mortality trend of IHD decreased slowly but progressively from 1990 to 2017 [49]. They suggested that this reduction may be partly due to increasing global awareness of lifestyle factors. Another study showed that the ASMR of stroke decreased sharply by 33.4% over the same period [50].
However, several epidemiological studies have reported a global trend of age-standardized CVD mortality rates either slightly declining or increasing in most LMICs, while high-income regions have experienced a significant reduction [4, 18]. For example, a study in Central Asia (comprising LMICs) found that CVD mortality trends have risen over the past two decades [51]. The researchers attributed this rise to factors such as inadequate preventive care, low awareness of disease signs and symptoms, reduced physical activity, elevated blood pressure, and insufficient utilization of healthcare services.
Although a slight reduction occurred before 2015, our joinpoint model suggests that the ASMR for CVD in Malaysia increased throughout the study period (2010–2021). The observed increase in ASMR from CVD in this country may be attributed to a combination of factors, including urbanization, changes in lifestyle and dietary habits, and a shift towards more sedentary lifestyles [52,53,54]. These factors have contributed to unhealthy, high-calorie diets, leading to the development of metabolic disorders like obesity and diabetes, which are well-known risk factors for CVD. Over the past decade, Malaysia has experienced a significant increase in the prevalence of several metabolic disorders, including obesity, diabetes, hypertension, and hypercholesterolemia. According to the National Health and Morbidity Survey (NHMS), the prevalence of obesity among adults in Malaysia has risen from 14.0% in 2006 [55] to 17.7% in 2019 [56], while the prevalence of diabetes has increased from 11.6% in 2006 [55] to 18.3% in 2019 [56]. The survey also showed that the prevalence of hypertension and hypercholesterolemia among adults in Malaysia has been increasing from 32.2% and 20.6% in 2006 [55] to 43.5% and 47.7% in 2019 [56], respectively. These trends are concerning, as these metabolic disorders are significant risk factors for CVD, which could contribute to the observed increase in ASMR from CVD in Malaysia. Additionally, Malaysia is experiencing a demographic transition due to an increasing aged population ≥ 60 years and increased life expectancy [57]. Population aging is becoming the most important driver of the CVD epidemic [58]. On the other hand, increased access to healthcare and better medical treatment for CVD [59, 60] may have also led to higher reported CVD mortality rates. Firstly, increased access to healthcare can lead to better detection and diagnosis of CVD cases, including previously undiagnosed or asymptomatic cases. As a result, more individuals with CVD are identified and included in mortality statistics, thus contributing to higher reported mortality rates. Secondly, better medical treatment for CVD can prolong the lives of individuals with the condition. While this is beneficial for improving individual health outcomes, it can also increase the pool of individuals living with CVD, who are at risk of dying from CVD-related complications in the long term. This, in turn, can lead to higher reported mortality rates.
While there has been an overall upward trend in CVD mortality rates, our joinpoint regression analysis only identified significant changes pre- and post-COVID-19 outbreak (2019–2021) among females who died from IHD and females aged 0–4 years, with no significant changes detected in other subgroups during this period (2019–2021). It is important to note that the impact of COVID-19 on CVD mortality rates during the early phases of the pandemic is inconsistent, with some countries reporting a decrease in CVD mortality [61,62,63] and others having observed an increase or excess mortality [64,65,66]. While our data is limited to one-year post-COVID-19 pandemic (2021), the study by Jayaraj et al. [67] on all-cause mortalities in Malaysia between January 2016 and September 2021 also utilized similar post-COVID data points up to 2021. Their results show a reduction in all-cause mortality in 2020, especially during the first Movement Control Order, followed by a significant increase between July and September 2021. This pattern supports our findings and might explain why the APC did not show significant changes between 2019–2021 in our study, despite an overall significant increase in the APC between 2018–2021. Additionally, the use of monthly data points with all causes of death in their study might have allowed for more precise detection of changes in trends during the COVID-19 pandemic compared to our study, which used yearly data points with specific causes of death.
On the other hand, our study highlights the persistent burden of premature CVD mortality (age 30–69) in Malaysia, which is in line with the trend of increasing global premature CVD mortality observed in LMICs [1]. Furthermore, there are notable sex disparities, with higher rates of premature CVD mortality among males compared to females. This finding is consistent with the results of Zhang et al. (2021) [68], who reported a 35.6% higher overall premature CVD mortality rate among men than women, based on global data from the WHO Global Health Estimates (GHE). Other studies [69,70,71] have also highlighted sex disparities related to premature CVD mortality.
In addition, our study revealed that while males had a higher overall ASMR than females, the magnitude of increase during the entire study period (2010–2021) was greater among females (AAPC 3.8% in females versus 3.5% in males). Notably, females aged over 70 years exhibited the highest ASMR over time compared to other age groups. These findings are consistent with the observations of Roth et al. [1], who reported a rapid increase in the proportion of CVD-related deaths among women after the age of 70, surpassing that among men. However, Roth et al. found that this trend is driven predominantly by stroke mortality, whereas our findings show that IHD had a higher increment among Malaysian females. These findings highlight the importance of targeted interventions and policies to address sex-specific CVD types and age-related disparities in ASMR from CVD mortality in Malaysia.
Study limitations
The study had some limitations that should be taken into consideration when interpreting the results. Firstly, the use of yearly data points and the lack of post-COVID-19 outbreak observation may have contributed to the insignificant findings of changes in the overall CVD mortality trend and most of the subgroup during the pre- and post-COVID-19 outbreak period (2019–2021). Therefore, the true burden of the effect of COVID-19 on CVD deaths should be interpreted with caution. Despite this limitation, our intention to examine the potential impact of the early COVID-19 pandemic on CVD mortality remains relevant, as evidenced by the significant APC detected during the pre- and post-COVID-19 period (2019–2021) in certain groups (e.g., females with IHD). Additionally, the study was limited by the variables available in the death registry, which did not include information on other modifiable risk factors such as diabetes, hypertension, and alcohol use, as well as important sociodemographic factors such as ethnic group, regional area, income level, and employment status. These variables may have been important to adjust or stratify in the joinpoint regression analysis. Furthermore, the study may not have represented the total CVD deaths in Malaysia, as it relied only on medically certified deaths. However, the use of the most complete and accurate data on CVD death, with ICD-10 coding conducted by specialist coders from DOSM and validated by independently certified coders, is a strength of the study.
Conclusion
In conclusion, this study highlights the increasing trend in ASMR from CVD in Malaysia, with a substantial increase observed between 2015 and 2018. The findings also underscore the ongoing burden of premature CVD mortality in the country, particularly among males. Efforts to address CVD risk factors and implement effective prevention and management strategies should be continued, including public health campaigns to raise awareness about healthy lifestyle behaviours, enhancing access to affordable and quality healthcare services, strengthening primary healthcare systems, investing in community-based interventions, and promoting multi-sectoral collaboration. Further research is warranted to explore the specific impact of the COVID-19 pandemic on CVD mortality rates in Malaysia and to guide the development of targeted interventions to mitigate its effects.
Data availability
The mortality data used in this study were obtained from a restricted source (Department of Statistics Malaysia). The population structure in Malaysia is available online (https://pqi.stats.gov.my). We confirm that all methods were carried out in accordance with the relevant guidelines and regulations.
Abbreviations
- AAPC:
-
the average annual percent change.
- APC:
-
the annual percent change.
- IHD:
-
Ischemic heart disease (ICD-10 code: I20-I25).
- Stroke:
-
including all cerebrovascular disease.
References
Roth GA, Huffman MD, Moran AE, Feigin V, Mensah GA, Naghavi M, et al. Global and regional patterns in cardiovascular mortality from 1990 to 2013. Circulation. 2015;132:1667–78.
Vos T, Lim SS, Abbafati C, Abbas KM, Abbasi M, Abbasifard M, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of Disease Study 2019. Lancet. 2020;396:1204–22.
WHO. Cardiovascular diseases (CVDs): Key Facts. In: Word Health Organization (WHO) [Internet]. 2021 [cited 9 Oct 2022]. Available: https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds).
Jagannathan R, Patel SA, Ali MK, Narayan KMV. Global updates on Cardiovascular Disease Mortality trends and Attribution of traditional risk factors. Curr Diab Rep. 2019;19:44. https://doi.org/10.1007/s11892-019-1161-2
Levi F, Lucchini F, Negri E, La Vecchia C. Trends in mortality from cardiovascular and cerebrovascular diseases in Europe and other areas of the world. Heart. 2002;88:119–24.
Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study. J Am Coll Cardiol. 2020;76:2982–3021.
WHO. Global action plan for the prevention and control of noncommunicable diseases 2013–2020. World Health Organization (WHO); 2013.
Wang H, Naghavi M, Allen C, Barber R, Bhutta M. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the global burden of Disease Study 2015. Lancet. 2016;388:1459–544. https://doi.org/10.1016/S0140-6736(16)31012-1
Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the global burden of Disease Study 2010. Lancet. 2012;380:2095–128. https://doi.org/10.1016/S0140-6736(12)61728-0
Global regional. National age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the global burden of Disease Study 2013. Lancet. 2015;385:117–71. https://doi.org/10.1016/S0140-6736(14)61682-2
Moran AE, Forouzanfar MH, Roth GA, Mensah GA, Ezzati M, Murray CJL, et al. Temporal trends in ischemic heart disease mortality in 21 world regions, 1980 to 2010: the global burden of Disease 2010 study. Circulation. 2014;129:1483–92.
Hartley A, Marshall DC, Salciccioli JD, Sikkel MB, Maruthappu M, Shalhoub J. Trends in mortality from ischemic heart disease and cerebrovascular disease in Europe: 1980 to 2009. Circulation. 2016;133:1916–26.
Global Burden of Disease. The Global Burden of Disease Study 2010 (GBD 2010): GBD profile Malaysia. 2010 p. 131.
Zhang Y-B, Pan X-F, Chen J, Cao A, Xia L, Zhang Y, et al. Combined lifestyle factors, all-cause mortality and cardiovascular disease: a systematic review and meta-analysis of prospective cohort studies. J Epidemiol Community Health. 2021;75:92–9.
Ezzati M, Obermeyer Z, Tzoulaki I, Mayosi BM, Elliott P, Leon DA. Contributions of risk factors and medical care to cardiovascular mortality trends. Nat Rev Cardiol. 2015;12:508–30.
Yusuf S, Hawken S, Ôunpuu S, Dans T, Avezum A, Lanas F, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364:937–52. https://doi.org/10.1016/S0140-6736(04)17018-9
Mathers CD, Loncar D. Projections of global mortality and Burden of Disease from 2002 to 2030. PLoS Med. 2006;3:e442. https://doi.org/10.1371/journal.pmed.0030442
Roth GA, Forouzanfar MH, Moran AE, Barber R, Nguyen G, Feigin VL, et al. Demographic and epidemiologic drivers of global cardiovascular mortality. N Engl J Med. 2015;372:1333–41.
Cosselman KE, Navas-Acien A, Kaufman JD. Environmental factors in cardiovascular disease. Nat Rev Cardiol. 2015;12:627–42.
WHO. WHO announces COVID-. 19 outbreak a pandemic – WHO Director- General’s opening remarks at the media briefing on COVID- 19. In: World Health Organization (WHO) [Internet]. 2020 [cited 26 Mar 2022]. Available: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020
Woolf SH, Chapman DA, Sabo RT, Weinberger DM, Hill L. Excess deaths from COVID-19 and other causes, March-April 2020. JAMA. 2020;324:510. https://doi.org/10.1001/jama.2020.11787
Wang H, Paulson KR, Pease SA, Watson S, Comfort H, Zheng P, et al. Estimating excess mortality due to the COVID-19 pandemic: a systematic analysis of COVID-19-related mortality, 2020–21. Lancet. 2022. https://doi.org/10.1016/S0140-6736(21)02796-3
Kubica J, Ostrowska M, Stolarek W, Kasprzak M, Grzelakowska K, Kryś J, et al. Impact of COVID-19 pandemic on acute heart failure admissions and mortality: a multicentre study (COV‐HF‐SIRIO 6 study). ESC Heart Fail. 2022;9:721–8. https://doi.org/10.1002/ehf2.13680
Axenhus M, Schedin-Weiss S, Winblad B, Wimo A. Changes in mortality trends amongst common diseases during the COVID-19 pandemic in Sweden. Scand J Public Health. 2021;140349482110646. https://doi.org/10.1177/14034948211064656
Solomon MD, McNulty EJ, Rana JS, Leong TK, Lee C, Sung S-H, et al. The Covid-19 pandemic and the incidence of acute myocardial infarction. N Engl J Med. 2020;383:691–3.
De Filippo O, D’Ascenzo F, Angelini F, Bocchino PP, Conrotto F, Saglietto A, et al. Reduced rate of hospital admissions for ACS during Covid-19 outbreak in Northern Italy. N Engl J Med. 2020;383:88–9.
Garcia S, Albaghdadi MS, Meraj PM, Schmidt C, Garberich R, Jaffer FA, et al. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020;75:2871–2.
Driggin E, Madhavan MV, Bikdeli B, Chuich T, Laracy J, Biondi-Zoccai G, et al. Cardiovascular considerations for patients, Health Care Workers, and Health systems during the COVID-19 pandemic. J Am Coll Cardiol. 2020;75:2352–71. https://doi.org/10.1016/j.jacc.2020.03.031
Doupis J, Avramidis K. Managing diabetes during the COVID-19 pandemic. Eur Endocrinol. 2020;16:85. https://doi.org/10.17925/EE.2020.16.2.85
Qiu D, Katanoda K, Marugame T, Sobue T. A joinpoint regression analysis of long-term trends in cancer mortality in Japan (1958–2004). Int J Cancer. 2009;124:443–8.
Wong MCS, Fung FDH, Leung C, Cheung WWL, Goggins WB, Ng CF. The global epidemiology of bladder cancer: a joinpoint regression analysis of its incidence and mortality trends and projection. Sci Rep. 2018;8:1129.
Wilson L, Bhatnagar P, Townsend N. Comparing trends in mortality from cardiovascular disease and cancer in the United Kingdom, 1983–2013: joinpoint regression analysis. Popul Health Metr. 2017;15:23. https://doi.org/10.1186/s12963-017-0141-5
Gawryszewski VP, de Souza M. FM de. Mortality due to cardiovascular diseases in the Americas by region, 2000–2009. Sao Paulo Medical Journal. 2014;132: 105–110.
Malaysian Legislation. Births and Deaths Registration Act 1957 (Revised 1983). In: Commissioner of Law Revision, Malaysia under the authority of the Revision of Laws Act 1968 in collaboration with Percetakan Nasional Malaysia Bhd [Internet]. 2006 [cited 21 Aug 2023]. Available: http://www.commonlii.org/my/legis/consol_act/badra19571983376/
Mathers CD, Ma Fat D, Inoue M, Rao C, Lopez AD. Counting the dead and what they died from: an assessment of the global status of cause of death data. Bull World Health Organ. 2005;83:171–c177.
Adnan TH, Bujang MA, Supramaniam P, Mustaâ N, Lazim SSMAT, Haniff J et al. Trend Analysis of medically certified death in Malaysia, 1995–2010. J Health Inf Dev Ctries. 2012;6.
DOSM. Statistics on Cause of Death, Malaysia, 2022. In: Copyright ©2023 Department of Statistics Malaysia (DOSM) [Internet]. 2023 [cited 21 Aug 2023]. Available: https://www.dosm.gov.my/site/downloadrelease?id=statistics-on-causes-of-death-malaysia-2022&=English
Malaysia DCDM. of H. Manual for Cause of Death Assignment: Verification of Non-Medically Certified Death Data. Ministry of Health Malaysia, Malaysia; Available: https://www.moh.gov.my/moh/resources/Penerbitan/Rujukan/NCD/Kanser/Manual_for_Cause_of_Death_Assignment.pdf
National Center for Health Statistics. International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM). In: National Center for Health Statistics, CDC [Internet]. 2022 [cited 26 Mar 2022]. Available: https://www.cdc.gov/nchs/icd/icd10cm.htm
Ahmad OB, Boschi-Pinto C, Lopez AD, Murray CJL, Lozano R, Inoue M et al. Age standardization of rates: a new WHO standard. Geneva: World Health Organization. 2001;9: 1–14.
WHO. Indicator Metadata Registry List. Premature mortality from noncommunicable disease. In: World Health Organization (WHO) [Internet]. 2023 [cited 30 Mar 2023]. Available: https://www.who.int/data/gho/indicator-metadata-registry/imr-details/3411
National Cancer Institute. Joinpoint Regression Program, Version 4.0. 4. Statistical methodology and Applications Branch. Surveillance Research; 2013.
Kim H-J, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19:335–51.
Zhang NR, Siegmund DO. A modified Bayes Information Criterion with Applications to the Analysis of Comparative Genomic Hybridization Data. Biometrics. 2007;63:22–32. https://doi.org/10.1111/j.1541-0420.2006.00662.x
National Cancer Institute. Joinpoint Regression Program: Annual Percent Change (APC) and Confidence Interval. 2013. Available: https://surveillance.cancer.gov/help/joinpoint/setting-parameters/method-and-parameters-tab/apc-aapc-tau-confidence-intervals/estimate-average-percent-change-apc-and-confidence-interval
National Cancer Institute. Joinpoint Regression Program: Average Annual Percent Change (AAPC) and Confidence Interval. 2013. Available: https://surveillance.cancer.gov/help/joinpoint/setting-parameters/method-and-parameters-tab/apc-aapc-tau-confidence-intervals/average-annual-percent-change-aapc
DOSM. Population Projection (Revised), Malaysia, 2010–2040. In: Department of Statistics Malaysia (DOSM) [Internet]. 2022 [cited 30 Mar 2023]. Available: https://www.dosm.gov.my/v1/index.php?r=column/ctheme&menu_id=L0pheU43NWJwRWVSZklWdzQ4TlhUUT09&bul_id=Y3kwU2tSNVFDOWp1YmtZYnhUeVBEdz09
Amini M, Zayeri F, Salehi M. Trend analysis of cardiovascular disease mortality, incidence, and mortality-to-incidence ratio: results from global burden of disease study 2017. BMC Public Health. 2021;21:1–12.
Khan MAB, Hashim MJ, Mustafa H, Baniyas MY, Al Suwaidi SKBM, AlKatheeri R et al. Global epidemiology of ischemic heart disease: results from the global burden of disease study. Cureus. 2020;12.
Avan A, Digaleh H, Di Napoli M, Stranges S, Behrouz R, Shojaeianbabaei G, et al. Socioeconomic status and stroke incidence, prevalence, mortality, and worldwide burden: an ecological analysis from the global burden of Disease Study 2017. BMC Med. 2019;17:1–30.
Altyn, Aringazina Tleuberdi, Kuandikov Viktor, Arkhipov. Burden of the cardiovascular diseases in central Asia Central Asian J Global Health. 2018;7(1). https://doi.org/10.5195/cajgh.2018.321
Goh E, Von, Azam-Ali S, McCullough F, Roy Mitra S. The nutrition transition in Malaysia; key drivers and recommendations for improved health outcomes. BMC Nutr. 2020;6:1–14.
Hawkes C, Chopra M, Friel S. Globalization, trade, and the nutrition transition. Globalization and health. Routledge; 2009. pp. 257–284.
Popkin BM, Adair LS, Ng SW. Global nutrition transition and the pandemic of obesity in developing countries. Nutr Rev. 2012;70:3–21.
Institute for Public Health. The Third National Health and Morbidity Survey (NHMS III). 2006: General Findings. 2008. Available: https://iku.gov.my/images/IKU/Document/REPORT/2006/GeneralFindings.pdf
Institute for Public Health. National Health and Morbidity Survey (NHMS). 2019: Vol. I: NCDs–Non-Communicable Diseases: Risk Factors and Other Health Problems. Ministry of Health Malaysia Setia Alam, Malaysia; 2020.
Jacob R. Aging and current trends in Malaysia. Int J Social Work Hum Serv Pract. 2016;4:57–61.
Dominguez LJ, Galioto A, Ferlisi A, Pineo A, Putignano E, Belvedere M, et al. Ageing, lifestyle modifications, and cardiovascular disease in developing countries. J Nutr Health Aging. 2006;10:143.
Merican I, bin Yon R. Health care reform and changes: the Malaysian experience. Asia Pac J Public Health. 2002;14:17–22.
Thomas S, Beh L, Nordin R, Bin. Health care delivery in Malaysia: changes, challenges and champions. J Public Health Afr. 2011;2.
Banerjee A, Chen S, Pasea L, Lai AG, Katsoulis M, Denaxas S, et al. Excess deaths in people with cardiovascular diseases during the COVID-19 pandemic. Eur J Prev Cardiol. 2021;28:1599–609.
Normando PG, Araujo-Filho J, de Fonseca A, de Rodrigues G, Oliveira REF, Hajjar VA. LA, Reduction in hospitalization and increase in mortality due to cardiovascular diseases during the COVID-19 pandemic in Brazil. Arq Bras Cardiol. 2021.
Santos AM dos, de Souza BF, de Carvalho CA, Campos MAG, de Oliveira BLCA, Diniz EM et al. Excess deaths from all causes and by COVID-19 in Brazil in 2020. Rev Saude Publica. 2021;55.
Roth GA, Emmons-Bell S, Alger HM, Bradley SM, Das SR, De Lemos JA, et al. Trends in patient characteristics and COVID-19 in-hospital mortality in the United States during the COVID-19 pandemic. JAMA Netw Open. 2021;4:e218828–218828.
Zhu D, Ozaki A, Virani SS. Disease-specific excess mortality during the COVID-19 pandemic: an analysis of weekly US death data for 2020. Am J Public Health. 2021;111:1518–22.
Gobiņa I, Avotinš A, Kojalo U, Strele I, Pildava S, Villeruša A, et al. Excess mortality associated with the COVID-19 pandemic in Latvia: a population-level analysis of all-cause and noncommunicable disease deaths in 2020. BMC Public Health. 2022;22:1–12.
Jayaraj VJ, Chong DW-Q, Wan K-S, Hairi NN, Bhoo-Pathy N, Rampal S, et al. Estimating excess mortalities due to the COVID-19 pandemic in Malaysia between January 2020 and September 2021. Sci Rep. 2023;13:86.
Zhang J, Jin Y, Jia P, Li N, Zheng Z-J. Global gender disparities in premature death from Cardiovascular Disease, and their associations with Country Capacity for Noncommunicable Disease Prevention and Control. Int J Environ Res Public Health. 2021;18. https://doi.org/10.3390/ijerph181910389
Connelly PJ, Azizi Z, Alipour P, Delles C, Pilote L, Raparelli V. The importance of gender to understand sex differences in cardiovascular disease. Can J Cardiol. 2021;37:699–710.
Humphries KH, Izadnegahdar M, Sedlak T, Saw J, Johnston N, Schenck-Gustafsson K, et al. Sex differences in cardiovascular disease–impact on care and outcomes. Front Neuroendocrinol. 2017;46:46–70.
Kontis V, Mathers CD, Bonita R, Stevens GA, Rehm J, Shield KD, et al. Regional contributions of six preventable risk factors to achieving the 25$\times$ 25 non-communicable disease mortality reduction target: a modelling study. Lancet Glob Health. 2015;3:e746–57.
Acknowledgements
We thank the Department of Statistics Malaysia (DOSM) for providing the mortality data with ICD-10 codes for cause of death and population structure.
Funding
No funding was obtained for this study.
Author information
Authors and Affiliations
Contributions
Conceptualization: Wan Shakira Rodzlan Hasani, Kamarul Imran Musa, Kueh Yee Cheng, Sarat Chandra Dass. Data curation: Wan Shakira Rodzlan Hasani, Kamarul Imran Musa. Formal analysis: Wan Shakira Rodzlan Hasani. Investigation: Wan Shakira Rodzlan Hasani, Kamarul Imran Musa, Kueh Yee Cheng. Methodology: Wan Shakira Rodzlan Hasani, Kamarul Imran Musa, Sarat Chandra Dass. Project administration: Wan Shakira Rodzlan Hasani. Resources: Wan Shakira Rodzlan Hasani, Kamarul Imran Musa. Software: Wan Shakira Rodzlan Hasani. Writing – original draft: Wan Shakira Rodzlan Hasani. Writing – review & editing: Wan Shakira Rodzlan Hasani, Kamarul Imran Musa, Kueh Yee Cheng, Sarat Chandra Dass. All authors read the manuscript and approved the submission.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was conducted in accordance with the Declaration of Helsinki and ethical approval was obtained from the Medical Research and Ethics Committee (MREC), Ministry of Health Malaysia and the Human Research Ethics Committee of USM (USM/JEPeM/22,030,181). Mortality data was obtained with approval from the Department of Statistics Malaysia (DOSM). All data was anonymized prior to use in this study. Due to the using of DOSM database (vital registration data), the requirement for informed consent was waived.
Consent for publication
Not applicable.
Competing interests
All authors declare that they have no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Hasani, W.S.R., Musa, K.I., Cheng, K.Y. et al. Exploring the trend of age-standardized mortality rates from cardiovascular disease in Malaysia: a joinpoint analysis (2010–2021). BMC Public Health 24, 2519 (2024). https://doi.org/10.1186/s12889-024-19103-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-19103-7