Abstract
Background
This study aimed to investigate the relationships between accelerometer-measured physical activity (PA) and sedentary behaviour (SB) with physical function (PF) among older Chinese women in the community.
Methods
The present study comprised 1,113 community-dwelling older females, with an average age of 65 ± 2 years. We employed a linear regression analysis to investigate the relationship between patterns of PA and SB with PF. PA variables consisted of total PA time, bouted PA time (a continuous PA that lasts equal to or more than 10 min), and sporadic PA time (a continuous PA that lasts less than 10 min). SB variables included total SB time, 30-min bout of SB (a continuous SB that lasts equal to or more than 30 min), and 60-min bout of SB (a continuous SB that lasts equal to or more than 60 min). PF variables comprised handgrip strength (HGS), one-legged stance test with eyes closed (OLSTEC), usual walking speed (UWS), maximum walking speed (MWS) and chair-stand time (CT). To explore the joint effects of moderate-to-vigorous-intensity PA (MVPA) and SB on PF, we divided the duration of SB and MVPA participation in older women into different combinations: low MVPA & high SB, low MVPA & low SB, high MVPA & high SB, high MVPA & low SB.
Results
The study revealed a significant association between 30-min bout of SB and CT, which remained after adjusting for total MVPA time (P = 0.021). Both total MVPA and bouted MVPA were found to be positively associated with better UWS, MWS, CT, and PF Z-score. When the combination of low MVPA & high SB was used as a reference, the regression coefficients for PF ascended by 1.32 (P < 0.001) in the high MVPA & high SB group and by 1.13 (P < 0.001) in the high MVPA & low SB group.
Conclusions
A significant association was observed between poorer lower limb function and prolonged, uninterrupted SB in older women, rather than with the total SB time. Concurrently, the insufficient engagement in MVPA may also be a crucial factor contributing to poorer PF in older women. Engaging in longer durations and higher intensity of PA, such as bouts of MVPA lasting a minimum of 10 min or longer, may contribute to better PF.
Similar content being viewed by others
Background
As individuals age, there is a tendency towards a reduction in physical activity (PA) and an increase in sedentary behaviour (SB) [1]. This trend is one of the key reasons for the decline in physical function (PF) [2, 3]. The decline in PF not only leads to a reduced quality of life in older adults [4, 5], but also rises the risk of falls and can lead to disability and loss of independence in severe cases [6, 7], placing a heavy burden on individuals, families and society. In contrast with men, the decrease in bone muscle mass, muscle strength, and PF is more pronounced in older women [8, 9]. Even more concerning is that older women are more susceptible to sarcopenia and related disease [10, 11]. In addition, older women have higher rates of disability [12], long-term care needs and medical expenses than men [13, 14]. These risks are strongly connected with PF, which means that identifying modifiable risk factors for preventing fall in PF is especially important for older females.
PA and SB are crucial factors affecting PF and the health status of elderly individuals [15, 16], and their relationship with PF in older women deserves further study. The relationships between PA and SB with PF are currently unclear, which impedes the design of effective interventions. Firstly, it is inconsistent among previous studies as to whether PA affects the association between SB and PF [17,18,19]. Secondly, the majority of research on the relationship between PA and PF has focused on the cumulative duration of moderate-to-vigorous-intensity PA (MVPA), with limited attention given to the cumulative patterns of MVPA. In 2020, the World Health Organization (WHO) revised its PA guidelines to omit the prior recommendation of at least 10 min of MVPA at a time. The update underscored that any volume of activity confers benefits relative to inactivity [20]. This revision serves to enhance the public’s comprehension of the potential advantages associated with various patterns of PA, including sporadic MVPA (duration < 10 min). Substantial research indicates that sporadic MVPA correlates with decreased instances of metabolic syndrome [21], fear of fall [22], frailty [23]and mortality [24]in older adults. Nevertheless, the relationship between sporadic MVPA and PF has only been explored in one study to date. Furthermore, the PF data in their study were obtained through self-reporting, which could introduce potential biases [25]. It has been observed that older adults tend to have a more negative view of their own health and functional abilities as they age [26]. This may result in lower levels of self-reported PF, which may in turn affect the accuracy of the results of studies based on self-reports [27]. Additionally, numerous studies have demonstrated that light intensity PA (LPA) can have a beneficial impact on the health of a larger population [28,29,30], yet few studies have incorporated LPA into PF research. A review of the literature reveals that there is no consensus on the relationship between LPA and PF in a few studies. Some studies have indicated that LPA is related to PF [31, 32], while others have suggested that LPA is not related to PF [33, 34]. For older individuals, it may be more feasible to engage in LPA than MVPA.
Consequently, in light of these gaps, this study aimed to explore the relationships between patterns of PA and SB with PF in older women to provide more accurate PA recommendations to improve PF in older females.
Methods
Participants
The cross-sectional data was sourced from the baseline surveys of the PA and Health in Older Women Study (PAHIOWS). PAHIOWS was a community-based study conducted in a coastal city in Shandong Province, China, aimed at exploring the relationship between PA and SB and the health status of older females. A total of 1,370 participants aged between 60 and 70 years were included in the PAHIOWS. These participants were able to communicate freely, were without cognitive impairment (Mini-Mental State Examination [35](MMSE) scores > 18), and had signed informed consent forms. This research was approved by the ethics committee of the School of Nursing and Rehabilitation, Shandong University, China (2020-R-067). All participants provided written informed consent.
Measurement of sedentary behaviour and physical activity variables
A triaxial accelerometer (ActiGraph wGT3X-BT, Pensacola, FL, USA) was employed to collect the participants’ PA and SB data [36]. The instructions were to wear the accelerometer on the subject’s hip for seven consecutive days, with the exception of periods of sleep, bathing, and swimming. While participants wore the accelerometer, they received two phone follow-ups to ensure compliance with the accelerometer-wearing protocol. Participants were included in the final analysis if they wore the accelerometer for a minimum of 10 h each day over at least four validation days [37].
The data were recorded in 60-s epochs and analyzed using ActiLife software, version 6.13.4 (https://www.actigraphcorp.com/). Nonwear time was defined as 90 consecutive min or longer of zero-intensity counts, with no more than 2 min of counts between 0 and 100 [38]. In this study, SB was defined as < 100 count per minute (CPM), LPA was defined as 100–1951 CPM and MVPA was defined as > 1952 CPM. The cut-point of the MVPA corresponds approximately to the energy expenditure of a walking speed of 4 km/h [39]. The three cut-points were based on those developed by Freedson et al. [40] and have been validated in numerous studies of older women [41,42,43,44]. Meanwhile, the PA and SB variables were exported in order to identify specific patterns. The SB variables include: (i)Total SB time (Average daily sedentary time); (ii)30-min bout of SB (each time consisting of 30 consecutive minutes or more of SB); (iii)60-min bout of SB ( each time consisting of 60 consecutive minutes or more of SB). The PA variables include: (i)Total PA time (Average daily PA time); (ii)Bouted PA (each time consisting of 10 consecutive minutes or more of PA); (iii)Sporadic PA (any PA accumulated in < 10 min).
Measurement of physical function variables
This study employed a comprehensive assessment of PF in older women who met the inclusion criteria, utilising five validated performance tests [45]. The tests were administered one-on-one by trained staff at a fitness monitoring center. Before each test, participants were informed of about the specific requirements and asked if they were able to complete it. Individuals who self-reported an inability to perform the tests were excluded from the study. If participants confirmed their ability to undertake the tests, the staff closely monitored their condition, ready to provide assistance or discontinue the tests if necessary. The aforementioned tests encompass the following:
Handgrip strength (HGS)(ACMEWAY(Beijing) Health Technology, China): HGS testing is a validated and feasible bedside method that is currently the most commonly used method in clinical practice to measure upper-body strength [46, 47]. Participants were asked to stand with their arms parallel to the body and squeeze an electronic hand dynamometer (in kg) with their dominant hand as hard as possible on two occasions, with the highest value being recorded as the measurement.
One-legged stance test with eyes closed (OLSTEC) : The OLSTEC is a common method for assessing body balance and stability, and it is a predictor of fall risk in older adults [48, 49]. During the test, participants were instructed to close their eyes, maintain a parallel position of their arms to their bodies, elevate one foot off the ground and maintain balance. The timer starts when the foot is lifted, and the participant stands on one leg as long as possible (up to 120 s). In the event that the stationary foot is displaced, or the lifted foot contacts the ground, the timer is terminated. The dominant leg was subjected to two trials, with the most favourable outcome being selected for analysis.
5-m walk test: The 5-metre walk test has been demonstrated to be a reliable and valid indicator of mobility in older adults [49]. The participants were requested to complete two tests on a 7-metre track, one at their usual walking speed (UWS) and one at their maximum walking speed (MWS). The testers recorded the time taken by the participants to reach the 5-metre line on each occasion and subsequently analysed the measurements from both times.
Chair-standing time(CT): This test is used to assess lower limb functional strength [50, 51] and has been identified as a feasible, reliable, and effective measure for the prediction of falls in older adults in the community [52]. The participants were instructed to cross their hands in front of their chest, ascend from a stool without armrests to a fully standing position as quickly as possible, and then return to a seated position as soon as possible, which was repeated five times. The total time taken to complete the five repetitions was recorded by the testers using a stopwatch.
A standardised PF composite score (Z-score) was calculated by summing the individual Z-scores of the five tests [53]. Since a lower Z-score of CT, USW, and MWS indicates superior physical ability, the three Z-values were recorded as opposite numbers. The cumulative sum of these five Z-values served as the comprehensive continuous measurement for PF.
Measurements of other variables
Considering the effect of other factors on result, we collected data of potential confounding factors, which were shown to be associated with the variable of PF [54,55,56,57]. Sociodemographic characteristics including age, living alone (yes or no) were collected using face-to-face interview. Income (currency: CNY, unit: monthly/yuan; income options include ≤ 1000 yuan (approximately 137 dollars), 1001–2000 yuan, 2001–3000 yuan, 3001–4000 yuan, and > 4000 yuan) and the number of chronic diseases (assessed by self-reported history of medical diagnosis, consist of diabetes, heart disease, stroke, cancer, chronic lung, etc., defined as 0, 1, 2, 3 or more diseases) were measured. The Chinese version of the Athens Insomnia Scale (AIS) was used to assess sleep quality, with a total score ranging from 0 to 24 points, with higher scores representing more severe insomnia [58]. Nutritional status was measured using the Mini Nutritional Assessment Short Form (MNA) with a total score of 30, and lower scores indicate worse nutritional status [59]. Cognitive function was measured using the MMSE, with a total score ranging from 0 to 30, where lower scores were regarded as indicative of lower cognitive levels [35]. The body mass index (BMI) was derived by measuring the height and weight of subjects by a body composition analyzer (MC-180, TANITA, JAPAN) and then using the following formula: BMI = weight (kg)/height2 (m2).
Statistical analysis
Descriptive data were presented as means ± standard deviation (SD) for continuous variables and as frequency (percentages) for categorical variables. A linear regression analysis was employed to investigate the relationship of SB and PA with PF indicators and PF Z-score, respectively. In order to more precisely assess the effects of incremental changes in PA and SB on PF, new variables for SB and PA were developed. The variables represent the daily increments in time spent in SB, LPA, and MVPA. Specifically, the SB variable was configured to increase by 60 min per day in order to simulate an increase in SB. Concurrently, the LPA variable was adjusted to incorporate an additional 30 min per day to account for elevated levels of LPA, while the MVPA variable was set to incorporate an extra 10 min per day to signify increased MVPA [60, 61]. The following three models were used to adjust for confounding factors: Model 1 was adjusted for age and accelerometer daily wear time. Model 2 was additionally adjusted for Model 1 variables plus confounding factors including BMI, living alone, income, number of chronic diseases, AIS score, MNA score, and MMSE score. Model 3 additionally adjusted for corresponding accelerometer variables according to the specific independent variable. Model 3a was adjusted for total MVPA time to all SB variables and total LPA time, and Model 3b was adjusted for total SB time to total MVPA time. To investigate the independent associations between different PA patterns and PF, bouted PA and sporadic PA were adjusted for each other: Model 3c was adjusted for Model 2 variables plus total SB time, and additionally adjusted for bouted MVPA and sporadic MVPA to each other; Model 3d was adjusted for Model 2 variables plus total MVPA time, and additionally adjusted for bouted LPA and sporadic LPA to each other [60]. The variance inflation factor (VIF) for all variables were calculated to detect the presence of collinearity. In the fully adjusted Model 3, VIF below 3 which was considered acceptable [62].
To investigate the joint effects of MVPA and SB on PF, we divided the daily time spent in MVPA and SB among older women into tertiles. Based on the lowest and highest tertiles, participants’ activity combinations were categorized into four types: Low MVPA & High SB (MVPA < 23.2 min and SB ≥ 570.8 min); Low MVPA & Low SB (MVPA < 23.2 min and SB < 494.7 min); High MVPA & High SB (MVPA ≥ 38.4 min and SB ≥ 570.8 min) and High MVPA & Low SB (MVPA ≥ 38.4 min and SB < 494.7 min). Finally, linear regression analysis was performed using Models 1 and 2 described above. Regression coefficients and 95% confidence intervals (CI) represent all linear regression results. A value of P < 0.05 was considered significant, with P < 0.01 deemed highly significant. All computations were performed using Stata version 17.0.
Results
Participant characteristics
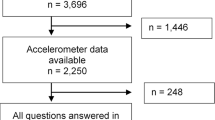
Of all 1370 older females, 148 women had insufficient accelerometer wear time, 97 women did not complete the questionnaire assessment, and 12 women did not finish PF assessment. The final analysis included data from 1,113 older females. The characteristics of the study population are presented in Table 1. The survey findings indicated that the average age of older women was 65 years old, 11.2% lived alone, 13.8% had three or more chronic diseases, and 50.9% earned between 3,001 and 4,000 yuan. In accordance with the established criteria for BMI classification (overweight defined as BMI > 25 kg·m− 2), the mean BMI of the study population was 25.4 kg·m− 2, indicating that the majority of participants were overweight.
Associations between patterns of physical activity, sedentary behaviour and physical function
Table 2 presents the final results (Model 3) of the associations between PA and SB with PF. Further details on Models 1 and 2 can be found in the supplementary material, Tables S1-S6. According to Table 2, among all SB variables, only 30-min bout of SB showed a significant association with CT (P = 0.021) after adjusting for total MVPA time. Regarding PA, both total MVPA time and Bouted MVPA were significantly associated with UWS, MWS, CT, and the PF Z-score. Specifically, for each increment of 10 min for total MVPA time, UWS decreased by 0.19 m/s (95% CI: -0.25, -0.14, P < 0.001), MWS decreased by 0.12 m/s (95% CI: -0.16, -0.75, P < 0.001), CT decreased by 0.44s(95% CI:-0.65,-0.23, P < 0.001) and the PF Z-score increased by 0.94 (95% CI: 0.63, 1.23, P < 0.001). Similarly, for each increment of 10 min for Bouted MVPA, UWS decreased by 0.07 m/s (95% CI: -0.10, -0.04, P < 0.001), MWS decreased by 0.03 m/s (95% CI: -0.05, 0.02, P < 0.001), CT decreased by 0.11s(95% CI:-0.20,-0.01, P = 0.024) and the PF Z-score increased by 0.25 (95% CI: 0.11, 0.39, P < 0.001). Moreover, there was no significant association between total LPA time, bouted LPA and sporadic LPA with PF in Model 3. Notably, HGS and OLSTEC had no association with any variables of SB and PA.
The joint associations of sedentary behaviour and moderate-to-vigorous-intensity physical activity categories with physical function measures
The analysis showed that MVPA levels moderated the relationship between SB and PF. The results of the combined effect of SB and MVPA on PF are shown in Table 3. In Model 2, we found that PF was significantly associated with both the high MVPA group compared to the Low MVPA & High SB combination. The regression coefficient of the High MVPA & High SB combination increased by 1.32 (95% CI: 0.83, 1.82, P < 0.001), and the regression coefficient of the High MVPA & Low SB combination increased by 1.13 (95% CI: 0.63, 1.63, P < 0.001). Notably, no association with PF was found for the Low MVPA & Low SB combination compared to the Low MVPA & High SB combination.
Discussion
Overall, our study in Model 3 demonstrates a significant association between 30-min bouts of SB and CT. In terms of PA, both total MVPA time and bouted MVPA were associated with better UWS, MWS, CT, and PF Z-score. However, all LPA variables show no significant association with any PF variables. Compared to the combination of low MVPA & high SB, high MVPA level combinations exhibit a significant improvement in PF Z-score regardless of the level of SB.
The subjects of this study were older women residing in the community. Their average sedentary time was 9.1 h per day, less than the 9.4 h previously reported for most older adults [63]. This may be attributed to the fact that in our community, residents engage in social interactions with their neighbours on occasion, which may contribute to a reduction in sedentary time. Previous studies have shown that total SB time and 60-min bout of SB in older adults were associated with poor performance on OLSTEC and CT [64]. Nevertheless, our findings do not fully corroborate the previously proposed association. Specifically, our results indicate that in older women, 30-min bout of SB was associated with worse CT manifestations, while other SB variables had no significant association with PF indicators and Z-score. This suggests that total SB time may not be the main influencing factor, but longer continuous sedentary bout patterns could pose a risk to specific PF indicators, especially lower limb function. It is likely that gender is a significant factor in this divergent outcome. Previous studies have revealed significant differences in PF between men and women [65,66,67]. For example, Gennuso et al. [67]. discovered that there was no significant association between 20, 40, and 60-min bout of SB and short physical performance battery score in the female sample. However, a significant association was observed in the male sample. This indicates that gender may play a moderating role in the relationship between SB and PF. Meanwhile, their study also reported that total SB time was not associated with PF in both male and female samples, consistent with our findings. Additionally, the participants in our study exhibited fewer instances of SB lasting 60 min or more, which represented only 14% of the total daily sedentary time on average. Approximately half of the older female participants engaged in less than one bout of SB lasting 60 min or more per day. In contrast, 30-min bout of SB was significantly more prevalent, accounting for 31.5% of the total sedentary time, nearly twice as much as the 60-min bout of SB. Notwithstanding the absence of a significant association between 60-min bout of SB and PF observed in our study, it cannot be ruled out that such prolonged periods of SB may adversely affect the PF of older women. In summary, our study indicates that it was the prolonged, uninterrupted patterns of SB, rather than the total SB time, that were more strongly linked to the decline in lower-extremity function among older adults. Subsequent research should take into account potential gender differences and further investigate the beneficial effects of reducing continuous SB on improving PF in older adults.
The analysis of MVPA and PF revealed a significant positive association between total MVPA time and PF enhancement, which was consistent with the results of both male and female samples [19, 68, 69]. Furthermore, our study highlights the benefits of bouted MVPA. More specifically, the PF regression coefficient increased by 0.25 for every 10 min/day increase in bouted MVPA. The results of this study are consistent with those of a previous investigation which demonstrated that both total time spent in MVPA and bouts of at least 10 min in duration were associated with improved PF in older women [70]. Sporadic MVPA was an important component of the total MVPA time. However, our study did not find an association between sporadic MVPA and PF. The reason why no association between sporadic MVPA and PF was found may be that our study sample had relatively healthier PF levels and that sporadic MVPA was not sufficient to improve PF. Thus, the effect of sporadic MVPA on PF needs to be applied to more people in the future to verify whether sporadic MVPA can improve lower PF levels. Based on our findings, we currently recommend that healthy older women should participate in MVPA lasting 10 min or more at a time to gain health benefits on PF. Moreover, a comprehensive examination of the data revealed a noteworthy phenomenon: a substantial proportion of the participants (70%) demonstrated compliance with the WHO recommendation of engaging in at least 150 min per week of MVPA. The high compliance rate may be attributed to the pervasive participation of older women in community square dancing activities across China. Square dancing is a popular group activity characterised by an upbeat rhythm and easily learned choreography. The dissemination of new steps and choreographic patterns is expedited by the guidance provided by lead dancers, which subsequently encourages greater participation among older adults. An interventional study has demonstrated that regular participation in square dancing can significantly improve cognitive function, reduce symptoms of depression, and enhance the quality of life in elderly individuals with mild cognitive impairment [71]. The results of our investigation indicate that community-based square dancing may play a significant role in enabling elderly Chinese women to achieve or even exceed the PA levels recommended by the WHO.
Although LPA was more likely to be involved relative to MVPA, all LPA variables were not associated with PF in this study. This result is consistent with the results of several previously published studies on total LPA time and PF [18, 33, 70, 72]. In a study by Izawa et al. [14], an association was identified between LPA and MWS among 181 older adults with a mean age of 73.4 ± 4.8 years. The finding indicate that LPA may enhance mobility in seniors who are unlikely to withstand high-intensity activities. The authors point out, however, that the limited size of the sample limits the generalizability of their findings. The results of our current research indicate that LPA was unlikely to be an effective intervention for maintaining or improving PF in healthy older adults. Furthermore, our analyses did not reveal any significant associations between the PA variables measured and either HGS or OLSTEC. It is likely that this finding can be attributed to the fact that individuals participating in this study demonstrated superior levels of PF on both tests. In accordance with the 2019 Asian Sarcopenia Working Group Consensus, a female handgrip strength under 18 kg signifies low HGS, whereas 18 kg and above is considered normal HGS [73]. It is crucial to highlight that the average HGS among the group of older women participating in this study was 24 kg, which is significantly higher than the threshold for normal HGS as defined by the aforementioned consensus from the 2019 Asian Sarcopenia Working Group. Furthermore, a meta-analysis that consolidated of data from 18 studies demonstrated that the OLSTEC test yielded an average duration of 8.29s for individuals aged 60 to 64, and 7.15s for those aged 65 to 69, among which the average performance of Chinese elderly samples was 8.05s [74]. In contrast to the aforementioned groups, the older women in our study achieved a mean duration of 9.73s on the balance test, which was significantly superior to the performances of all the referenced comparison groups. Consequently, the pronounced enhancements in handgrip strength and balance abilities observed among our sample of older women indicate that they may have attained a level of PF that sufficiently masks the potential benefits typically associated with structured PA.
In order to explore the joint effect of PA and SB on PF, participants’ activity combinations were divided into four categories: low MVPA & high SB, low MVPA & low SB, high MVPA & high SB, and high MVPA & low SB. The results of the analysis indicated that combination of high MVPA & high SB and high MVPA&low SB were independently associated with the improvement of PF in older females, indicating that regardless of the level of SB, higher levels of MVPA were related to the advancement of PF. A previous study that included male samples demonstrated that high SB & low MVPA and low SB & low MVPA were associated with poorer PF [75]. Their study further supported the notion that the detrimental impact on PF was primarily due to insufficient MVPA. Therefore, even for individuals who accumulate a high amount of sedentary time, maintaining an adequate level of MVPA can still confer health benefits, particularly in relation to PF. This insight was of value to older women who may be required to sit for extended periods due to occupational or lifestyle factors. It highlighted the significance of regular engagement in MVPA as a key factor in maintaining their functional health.
Innovations and limitations
In the present study, accelerometers were worn at the hip to assess PA and SB among elderly women aged between 60 and 70 years. The hip has been validated as the optimal single placement for an accelerometer for the measurement of PA intensity. This methodology effectively minimized the burden on participants and enhanced the feasibility of the study. Consequently, the implementation of this methodology led to a notable enhancement in the precision of data collection, accompanied by a reduction in the potential for subjective bias. This, in turn, served to reinforce the reliability and accuracy of the study’s findings. Moreover, our research investigated the associations between diverse intensities and patterns of PA with PF in elderly women, as well as conducted a thorough analysis of the joint effects of PA and SB on PF. This provided a comprehensive perspective on how different intensities and patterns of PA independently or collectively affect PF. Notably, our study revealed for the first time the association between bouted LPA, sporadic LPA, and PF, contributing novel insights to the field of LPA research.
Despite these strengths, it is important to acknowledge several limitations. Firstly, the efficacy of the accelerometer in discerning body postures (i.e., standing, sitting, lying) may be constrained. Secondly, the cross-sectional design of the study precluded the establishment of causal relationships. Furthermore, the sample was drawn from a single city in China, which may not be sufficiently representative of the broader population of Chinese elderly individuals, limiting the generalisability of the findings. Finally, it is possible that the participants in this study were relatively healthy and more physically capable, which may have resulted in a selection bias towards individuals with better health statuses. In light of these limitations, future research should consider employing a longitudinal study design to explore more deeply the causal relationships between PA and SB patterns and PF in elderly women. Furthermore, it would be beneficial to expand the sample scope to encompass a more diverse population, while aiming for more precise measurement of SB and PA, in order to ensure the broad applicability of the study results.
Conclusions
A significant association was observed between poorer lower limb function and prolonged, uninterrupted SB in older women, rather than with the total SB time. Concurrently, the insufficient engagement in MVPA may also be a crucial factor contributing to poorer PF in older women. Engaging in longer durations and higher intensity of PA, such as bouts of MVPA lasting a minimum of 10 min or longer, may contribute to better PF.
Data availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- PA:
-
Physical Activity
- SB:
-
Sedentary Behaviour
- PF:
-
Physical Function
- MVPA:
-
Moderate-to-Vigorous-intensity Physical Activity
- WHO:
-
World Health Organization
- LPA:
-
Light intensity Physical Activity
- PAHIOWS:
-
Physical Activity and Health in Older Women Study
- OLSTEC:
-
One-legged Stance Test with Eyes Closed
- UWS:
-
Usual walking speed
- MWS:
-
Maximum walking speed
- CT:
-
Chair-standing Time
- CPM:
-
Counts Per Minute
- AIS:
-
Athens Insomnia Scale
- MNA:
-
Mini Nutritional Assessment Short Form
- MMSE:
-
Mini-Mental State Examination
- BMI:
-
Body Mass Index
- CI:
-
Confidence intervals
- VIF:
-
Variance Inflation Factor
References
Eckstrom E, Neukam S, Kalin L, Wright J. Physical activity and healthy aging. CLIN GERIATR MED. 2020;36(4):671–83.
Ortlieb S, Gorzelniak L, Nowak D, Strobl R, Grill E, Thorand B, Peters A, Kuhn KA, Karrasch S, Horsch A, et al. Associations between multiple accelerometry-assessed physical activity parameters and selected health outcomes in elderly people–results from the KORA-age study. PLoS ONE. 2014;9(11):e111206.
Ramsey KA, Rojer A, D’Andrea L, Otten R, Heymans MW, Trappenburg MC, Verlaan S, Whittaker AC, Meskers C, Maier AB. The association of objectively measured physical activity and sedentary behavior with skeletal muscle strength and muscle power in older adults: a systematic review and meta-analysis. AGEING RES REV. 2021;67:101266.
Reid N, Healy GN, Gianoudis J, Formica M, Gardiner PA, Eakin EE, Nowson CA, Daly RM. Association of sitting time and breaks in sitting with muscle mass, strength, function, and inflammation in community-dwelling older adults. Osteoporos INT. 2018;29(6):1341–50.
Yorston LC, Kolt GS, Rosenkranz RR. Physical activity and physical function in older adults: the 45 and up study. J AM GERIATR SOC. 2012;60(4):719–25.
Miller ME, Rejeski WJ, Reboussin BA, Ten HT, Ettinger WH. Physical activity, functional limitations, and disability in older adults. J AM GERIATR SOC. 2000;48(10):1264–72.
Visser M, Simonsick EM, Colbert LH, Brach J, Rubin SM, Kritchevsky SB, Newman AB, Harris TB. Type and intensity of activity and risk of mobility limitation: the mediating role of muscle parameters. J AM GERIATR SOC. 2005;53(5):762–70.
Suetta C, Haddock B, Alcazar J, Noerst T, Hansen OM, Ludvig H, Kamper RS, Schnohr P, Prescott E, Andersen LL, et al. The Copenhagen Sarcopenia Study: lean mass, strength, power, and physical function in a Danish cohort aged 20–93 years. J CACHEXIA SARCOPENI. 2019;10(6):1316–29.
Ward-Ritacco CL, Greaney ML, Clark PG, Riebe D. The Longitudinal Association between Physical Activity and physical function in Older Women. FRONT SPORTS ACT LIV. 2022;4:879025.
Kassiano W, Costa B, Nunes JP, Cyrino LT, Nascimento MA, Tomeleri C, Antunes M, Gobbo LA, Ribeiro AS, Coelho-E-Silva MJ, et al. Muscular strength and skeletal muscle mass in 511 physically independent older women aged 60–88 years. EXP GERONTOL. 2022;166:111867.
Stanghelle B, Bentzen H, Giangregorio L, Pripp AH, Skelton DA, Bergland A. Effects of a resistance and balance exercise programme on physical fitness, health-related quality of life and fear of falling in older women with osteoporosis and vertebral fracture: a randomized controlled trial. Osteoporos INT. 2020;31(6):1069–78.
Crimmins EM, Beltrán-Sánchez H. Mortality and morbidity trends: is there compression of morbidity? J GERONTOL B-PSYCHOL. 2011;66(1):75–86.
Harris-Kojetin L, Sengupta M, Park-Lee E, Valverde R, Caffrey C, Rome V, Lendon J. Long-term care providers and services users in the United States: data from the National Study of Long-Term Care providers, 2013–2014. Vital Health Stat. 2016;3(38):1–105.
Vara MJ. Long-term care for elder women in Spain: advances and limitations. J AGING SOC POLICY. 2014;26(4):347–69.
Nelson ME, Rejeski WJ, Blair SN, Duncan PW, Judge JO, King AC, Macera CA, Castaneda-Sceppa C. Physical activity and public health in older adults: recommendation from the American College of Sports Medicine and the American Heart Association. MED SCI SPORT EXER. 2007;39(8):1435–45.
Reuter C, Bellettiere J, Liles S, Di C, Sears DD, LaMonte MJ, Stefanick ML, LaCroix AZ, Natarajan L. Diurnal patterns of sedentary behavior and changes in physical function over time among older women: a prospective cohort study. INT J BEHAV NUTR PHY. 2020;17(1):88.
Rosenberg DE, Bellettiere J, Gardiner PA, Villarreal VN, Crist K, Kerr J. Independent associations between sedentary behaviors and Mental, Cognitive, Physical, and Functional Health among older adults in Retirement communities. J GERONTOL A-BIOL. 2016;71(1):78–83.
Walker RL, Greenwood-Hickman MA, Bellettiere J, LaCroix AZ, Wing D, Higgins M, Richmire K, Larson EB, Crane PK, Rosenberg DE. Associations between physical function and device-based measures of physical activity and sedentary behavior patterns in older adults: moving beyond moderate-to-vigorous intensity physical activity. BMC GERIATR. 2021;21(1):216.
Spartano NL, Lyass A, Larson MG, Tran T, Andersson C, Blease SJ, Esliger DW, Vasan RS, Murabito JM. Objective physical activity and physical performance in middle-aged and older adults. EXP GERONTOL. 2019;119:203–11.
World Health Organization. Phycial Activity|*2023*2023.; 2022.
Clarke J, Janssen I. Sporadic and bouted physical activity and the metabolic syndrome in adults. MED SCI SPORT EXER. 2014;46(1):76–83.
Du L, Zhang X, Wang W, He Q, Li T, Chen S, Pan Y. Associations between objectively measured pattern of physical activity, sedentary behavior and fear of falling in Chinese community-dwelling older women. GERIATR NURS. 2022;46:80–5.
Kehler DS, Clara I, Hiebert B, Stammers AN, Hay JL, Schultz A, Arora RC, Tangri N, Duhamel TA. The association between bouts of moderate to vigorous physical activity and patterns of sedentary behavior with frailty. EXP GERONTOL. 2018;104:28–34.
Saint-Maurice PF, Troiano RP, Matthews CE, Kraus WE. Moderate-to-vigorous physical activity and all-cause mortality: do bouts Matter? J AM HEART ASSOC 2018, 7(6).
Hrubeniuk TJ, Sénéchal M, Mayo A, Bouchard DR. Association between physical function and various patterns of physical activity in older adults: a cross-sectional analysis. AGING CLIN EXP RES. 2020;32(6):1017–24.
Jerez-Roig J, Souza DL, Andrade FL, Lima BF, Medeiros RJ, Oliveira NP, Cabral SN, Lima KC. Self-perceived health in institutionalized elderly. CIENC SAUDE COLETIVA. 2016;21(11):3367–75.
Roshanravan B, Patel KV. Assessment of physical functioning in the clinical care of the patient with advanced kidney disease. SEMIN DIALYSIS. 2019;32(4):351–60.
Sardinha LB, Ekelund U, Dos SL, Cyrino ES, Silva AM, Santos DA. Breaking-up sedentary time is associated with impairment in activities of daily living. EXP GERONTOL. 2015;72:57–62.
LaCroix AZ, Bellettiere J, Rillamas-Sun E, Di C, Evenson KR, Lewis CE, Buchner DM, Stefanick ML, Lee IM, Rosenberg DE, et al. Association of Light Physical Activity measured by Accelerometry and incidence of Coronary Heart Disease and Cardiovascular Disease in Older Women. JAMA NETW OPEN. 2019;2(3):e190419.
Gomez-Bruton A, Navarrete-Villanueva D, Pérez-Gómez J, Vila-Maldonado S, Gesteiro E, Gusi N, Villa-Vicente JG, Espino L, Gonzalez-Gross M, Casajus JA et al. The effects of Age, Organized Physical Activity and Sedentarism on Fitness in older adults: an 8-Year longitudinal study. INT J ENV RES PUB HE 2020, 17(12).
Savikangas T, Tirkkonen A, Alen M, Rantanen T, Fielding RA, Rantalainen T, Sipilä S. Associations of physical activity in detailed intensity ranges with body composition and physical function. A cross-sectional study among sedentary older adults. EUR REV AGING PHYS A. 2020;17:4.
Foong YC, Chherawala N, Aitken D, Scott D, Winzenberg T, Jones G. Accelerometer-determined physical activity, muscle mass, and leg strength in community-dwelling older adults. J CACHEXIA SARCOPENI. 2016;7(3):275–83.
Edholm P, Nilsson A, Kadi F. Physical function in older adults: impacts of past and present physical activity behaviors. SCAND J MED SCI SPOR. 2019;29(3):415–21.
Yatsugi H, Chen T, Chen S, Liu X, Kishimoto H. The associations between objectively measured physical activity and physical function in Community-Dwelling Older Japanese men and women. Int J Environ Res Public Health 2022, 19(1).
Katzman R, Zhang MY, Ouang-Ya-Qu, Wang ZY, Liu WT, Yu E, Wong SC, Salmon DP, Grant I. A Chinese version of the Mini-mental State examination; impact of illiteracy in a Shanghai dementia survey. J CLIN EPIDEMIOL. 1988;41(10):971–8.
Migueles JH, Cadenas-Sanchez C, Ekelund U, Delisle NC, Mora-Gonzalez J, Löf M, Labayen I, Ruiz JR, Ortega FB. Accelerometer Data Collection and Processing Criteria to assess physical activity and other outcomes: a systematic review and practical considerations. SPORTS MED. 2017;47(9):1821–45.
Ballin M, Nordström P, Niklasson J, Nordström A. Associations of objectively measured physical activity and sedentary time with the risk of stroke, myocardial infarction or all-cause mortality in 70-Year-old men and women: a prospective cohort study. SPORTS MED. 2021;51(2):339–49.
Choi L, Liu Z, Matthews CE, Buchowski MS. Validation of accelerometer wear and nonwear time classification algorithm. MED SCI SPORT EXER. 2011;43(2):357–64.
Qiu J, Yang J, Lu M, Chen Y, Yang Y, Cao W, Meng K, Chen Y, Zhang J, Xu C, et al. Compilation of physical activities of healthy Chinese adults: reference values for Energy Expenditure. Chin J Sports Med. 2022;41(5):335–49.
Freedson PS, Melanson E, Sirard J. Calibration of the Computer Science and Applications, Inc. accelerometer. MED SCI SPORT EXER. 1998;30(5):777–81.
Shiroma EJ, Freedson PS, Trost SG, Lee IM. Patterns of accelerometer-assessed sedentary behavior in older women. JAMA-J AM MED ASSOC. 2013;310(23):2562–3.
Bellettiere J, LaMonte MJ, Evenson KR, Rillamas-Sun E, Kerr J, Lee IM, Di C, Rosenberg DE, Stefanick M, Buchner DM, et al. Sedentary behavior and cardiovascular disease in older women: the Objective Physical Activity and Cardiovascular Health (OPACH) Study. Circulation. 2019;139(8):1036–46.
Evenson KR, Wen F, Herring AH, Di C, LaMonte MJ, Tinker LF, Lee IM, Rillamas-Sun E, LaCroix AZ, Buchner DM. Calibrating physical activity intensity for hip-worn accelerometry in women age 60 to 91 years: the women’s Health Initiative OPACH Calibration Study. PREV MED REP. 2015;2:750–6.
Gorman E, Hanson HM, Yang PH, Khan KM, Liu-Ambrose T, Ashe MC. Accelerometry analysis of physical activity and sedentary behavior in older adults: a systematic review and data analysis. EUR REV AGING PHYS A. 2014;11(1):35–49.
Cooper R, Kuh D, Hardy R. Objectively measured physical capability levels and mortality: systematic review and meta-analysis. BMJ-BRIT MED J. 2010;341:c4467.
Norman K, Stobäus N, Gonzalez MC, Schulzke JD, Pirlich M. Hand grip strength: outcome predictor and marker of nutritional status. CLIN NUTR. 2011;30(2):135–42.
Taekema DG, Gussekloo J, Maier AB, Westendorp RG, de Craen AJ. Handgrip strength as a predictor of functional, psychological and social health. A prospective population-based study among the oldest old. AGE AGEING. 2010;39(3):331–7.
Hinman MR, O’Connell JK, Dorr M, Hardin R, Tumlinson AB, Varner B. Functional predictors of stair-climbing speed in older adults. J GERIATR PHYS THER. 2014;37(1):1–6.
Shinkai S, Watanabe S, Kumagai S, Fujiwara Y, Amano H, Yoshida H, Ishizaki T, Yukawa H, Suzuki T, Shibata H. Walking speed as a good predictor for the onset of functional dependence in a Japanese rural community population. AGE AGEING. 2000;29(5):441–6.
Muñoz-Bermejo L, Adsuar JC, Mendoza-Muñoz M, Barrios-Fernández S, Garcia-Gordillo MA, Pérez-Gómez J, Carlos-Vivas J. Test-Retest Reliability of Five Times sit to stand test (FTSST) in adults: a systematic review and Meta-analysis. BIOLOGY-BASEL 2021, 10(6).
Buatois S, Miljkovic D, Manckoundia P, Gueguen R, Miget P, Vançon G, Perrin P, Benetos A. Five times sit to stand test is a predictor of recurrent falls in healthy community-living subjects aged 65 and older. J AM GERIATR SOC. 2008;56(8):1575–7.
Tiedemann A, Shimada H, Sherrington C, Murray S, Lord S. The comparative ability of eight functional mobility tests for predicting falls in community-dwelling older people. AGE AGEING. 2008;37(4):430–5.
Júdice PB, Silva AM, Berria J, Petroski EL, Ekelund U, Sardinha LB. Sedentary patterns, physical activity and health-related physical fitness in youth: a cross-sectional study. INT J BEHAV NUTR PHY. 2017;14(1):25.
Parry SM, Huang M, Needham DM. Evaluating physical functioning in critical care: considerations for clinical practice and research. CRIT CARE. 2017;21(1):249.
Shen Y, Shi Q, Nong K, Li S, Yue J, Huang J, Dong B, Beauchamp M, Hao Q. Exercise for Sarcopenia in older people: a systematic review and network meta-analysis. J CACHEXIA SARCOPENI. 2023;14(3):1199–211.
Buchmann N, Spira D, Norman K, Demuth I, Eckardt R, Steinhagen-Thiessen E. Sleep, muscle Mass and muscle function in older people. DTSCH ARZTEBL INT. 2016;113(15):253–60.
You KS, Lee H. The physical, mental, and emotional health of older people who are living alone or with relatives. ARCH PSYCHIAT NURS. 2006;20(4):193–201.
Soldatos CR, Dikeos DG, Paparrigopoulos TJ. Athens Insomnia Scale: validation of an instrument based on ICD-10 criteria. J PSYCHOSOM RES. 2000;48(6):555–60.
Rubenstein LZ, Harker JO, Salvà A, Guigoz Y, Vellas B. Screening for undernutrition in geriatric practice: developing the short-form mini-nutritional assessment (MNA-SF). J GERONTOL A-BIOL. 2001;56(6):M366–72.
Chen S, Chen T, Kishimoto H, Yatsugi H, Kumagai S. Associations of objectively measured patterns of sedentary behavior and physical activity with Frailty Status screened by the Frail Scale in Japanese Community-Dwelling older adults. J SPORT SCI MED. 2020;19(1):166–74.
Zhang X, Yang Z, Du L, Xiong C, Wang Z, Pan Y, He Q, Chen S, Cui L. Associations of accelerometer-measured physical activity, sedentary behavior with self-reported insomnia in older women: does pattern matter? SLEEP MED. 2023;104:58–63.
Sofer T, Zheng X, Laurie CA, Gogarten SM, Brody JA, Conomos MP, Bis JC, Thornton TA, Szpiro A, O’Connell JR, et al. Variant-specific inflation factors for assessing population stratification at the phenotypic variance level. NAT COMMUN. 2021;12(1):3506.
Harvey JA, Chastin SF, Skelton DA. How sedentary are older people? A systematic review of the amount of sedentary behavior. J AGING PHYS ACTIV. 2015;23(3):471–87.
Wilson JJ, McMullan I, Blackburn NE, Skjødt M, Caserotti P, Giné-Garriga M, Farche A, Klenk J, Dallmeier D, Deidda M, et al. Associations of sedentary behavior bouts with community-dwelling older adults’ physical function. SCAND J MED SCI SPOR. 2021;31(1):153–62.
Yatsugi H, Chen T, Chen S, Liu X, Kishimoto H. The associations between objectively measured physical activity and physical function in Community-Dwelling Older Japanese men and women. INT J ENV RES PUB HE 2021, 19(1).
Liao Y, Hsu HH, Shibata A, Ishii K, Koohsari MJ, Oka K. Associations of total amount and patterns of objectively measured sedentary behavior with performance-based physical function. PREV MED REP. 2018;12:128–34.
Gennuso KP, Thraen-Borowski KM, Gangnon RE, Colbert LH. Patterns of sedentary behavior and physical function in older adults. AGING CLIN EXP RES. 2016;28(5):943–50.
Lai TF, Liao Y, Lin CY, Huang WC, Hsueh MC, Chan DC. Moderate-to-vigorous physical activity duration is more important than timing for physical function in older adults. SCI REP-UK. 2020;10(1):21344.
Cooper AJ, Simmons RK, Kuh D, Brage S, Cooper R. Physical activity, sedentary time and physical capability in early old age: British birth cohort study. PLoS ONE. 2015;10(5):e126465.
Hsueh MC, Rutherford R, Chou CC, Park JH, Park HT, Liao Y. Objectively assessed physical activity patterns and physical function in community-dwelling older adults: a cross-sectional study in Taiwan. BMJ OPEN. 2020;10(8):e34645.
Wang S, Yin H, Meng X, Shang B, Meng Q, Zheng L, Wang L, Chen L. Effects of Chinese square dancing on older adults with mild cognitive impairment. GERIATR NURS. 2020;41(3):290–6.
Petrica MSF, Serrano J, Paulo J, Ramalho R, Lucas A, Ferreira D, Duarte-Mendes JP. P: The Sedentary Time and Physical Activity Levels on Physical Fitness in the Elderly: A Comparative Cross Sectional Study. INT J ENV RES PUB HE 2019, 16(19).
Chen LK, Woo J, Assantachai P, Auyeung TW, Chou MY, Iijima K, Jang HC, Kang L, Kim M, Kim S, et al. Asian Working Group for Sarcopenia: 2019 Consensus Update on Sarcopenia diagnosis and treatment. J AM MED DIR ASSOC. 2020;21(3):300–7.
Pin ZHANG, Zi-Xuan ZOU, Ting-Ting ZOU. Meta-analysis of evaluation of standing on one foot with closed eyes in healthy elderly. Chin J Gerontol. 2023;43(10):2401–6.
Gilchrist SC, Bennett A, Judd SE, Akinyemiju T, Howard VJ, Hooker SP, Cushman M, Diaz KM. Sedentary behavior and physical functioning in Middle-Age and older adults living in the United States: the reasons for Geographic and racial differences in Stroke Study. MED SCI SPORT EXER. 2022;54(11):1897–903.
Acknowledgements
The authors would like to acknowledge the National Health Monitoring Center of Yantai City, who contributed test site and subjects’ recruitment for support to the study and the participants of this study as well as our research volunteers for their time and commitment.
Funding
This work was supported by the Ministry of Education of Humanities and Social Science Project of China under Grant 19YJCZH255.
Author information
Authors and Affiliations
Contributions
XLZ, DLT, QH, SC and YP helped YYL modify the revised manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board of the School of Nursing and Rehabilitation, Shandong University (2020-R-067). Informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lu, Y., Li, Q., Wang, W. et al. Associations between accelerometer-measured physical activity and sedentary behaviour with physical function among older women: a cross-sectional study. BMC Public Health 24, 1754 (2024). https://doi.org/10.1186/s12889-024-19270-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-19270-7