Abstract
Introduction
Identifying clinical factors that increase the risk of mortality in COVID-19 patients is crucial. This enables targeted screening, optimizing treatment, and prevention of severe complications, ultimately reducing death rates. This study aimed to develop prediction models for the death of patients (i.e., survival or death) during the COVID-19 pandemic in Shiraz, exploring the main influencing factors.
Method
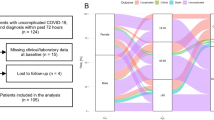
We conducted a retrospective cohort study using hospital-based records of 1030 individuals diagnosed with COVID-19, who were hospitalized for treatment between March 21, 2021, and March 21, 2022, in Shiraz, Iran. Variables related to the final outcome were selected based on criteria and univariate logistic regression. Hierarchical multiple logistic regression and classification and regression tree (CART) models were utilized to explore the relationships between potential influencing factors and the final outcome. Additionally, methods were employed to identify the high-risk population for increased mortality rates during COVID-19. Finally, accuracy was evaluated the performance of the models, with the area under the receiver operator characteristic curve(AUC), sensitivity, and specificity metrics.
Results
In this study, 558 (54.2%) individuals infected with COVID-19 died. The final model showed that the type of medicine antiviral (OR: 11.10, p = 0.038) than reference (antiviral and corticosteroid), and discharge oxygen saturation(O2) (OR: 1.10, p < 0.001) had a positive association with the chance of survival, but other variables were not considered as predictive variables. Predictive models for the final outcome(death) achieved accuracies ranging from 81 to 87% for hierarchical multiple logistic regression and from 87 to 94% for the CART model. Therefore, the CART model performed better than the hirerical multiple logistic regression model.
Conclusion
These findings firstly elucidate the incidence and associated factors of the outcome (death) among patients in Shiraz, Iran. Furthermore, we demonstrated that antiviral medication alone (without corticosteroids) and high O2 increase the survival chances of COVID patients.
Similar content being viewed by others
Introduction
The spread of coronavirus disease around the world is a great challenge affecting all aspects of people’s lives. Almost all people around the world are susceptible to SARS-CoV-2 infection [1]. Coronavirus disease 2019 (COVID-19), the disease of the new century, is an acute respiratory syndrome caused by coronavirus type 2 (SARS-COV2) [2]. This virus has the ability to infect humans, bats, and some mammals; it caused one of the most devastating epidemic in 2003 and 2003. Due to the complications and mortality caused by this disease, the World Health Organization declared this disease an epidemic on 11 March 2020 [3,4,5]. This disease has a broad spectrum of clinical manifestations, of which fever and cough are the most common ones [6]. In 30–60% of patients with COVID-19, there is shortness of breath, which occurs on average 5–8 days after the initial infection. In addition, in patients over 60 years of age, hypoxemia may also be observed [7]. Due to the spread of this virus variants and its different symptoms, predicting the course of the disease is complicated. Although COVID-19 is recognized as a respiratory disease, due to varying degrees of disease severity, a wide range of clinical manifestations from complete asymptomatic to severe pneumonia-related death have been reported. Following the aggravation of acute respiratory distress syndrome (ARDS) symptoms and cytokine storm, multi-organ failure occurs, which causes extensive changes in laboratory data and increases the mortality rate [8,9,10]. Although the ratio of the number of deaths to the number of recoveries is low, as reported 1.2% in the city of Shiraz (the capital of Fars province, which is located in the southwest of Iran), the rapid transmission of the virus leads to a high incidence rate and, as a result, a high mortality rate. The mortality rate of COVID-19 was 8119 people until the time of writing this article. Therefore, it is necessary to identify the factors related to the increased risk of death/mortality rate in COVID-19 patients. These factors include old age, male gender, comorbidities (diabetes, high blood pressure, reduced lung and kidney function, and other chronic diseases), racial/ethnic disparities, and some biomarkers [11, 12]. The connection between scientific and medical communities has led to the identification of reliable biomarkers related to COVID-19 and its progress [13]. Discerning effective biomarkers, in addition to having an important role in the screening of these patients, contributes to rapid diagnosis, appropriate management of treatment options, and prevention of serious complications [14, 15]. Identification laboratory and cilinical information will be useful for predicting the disease progress, identifying prevention strategies, and thus reducing mortality. Given that so far the hierarchical logistic regression model has not been used to investigate the relationship between mortality and related factors in this pandemic. Additionally, decision trees can identifying the most influential factors for predicting an outcome and can discern and describe nonlinear relationships. Their results are presented in an intuitive flowchart format, facilitating interpretation, and they possess the ability to categorize individuals hierarchically based on various factors. Furthermore, decision trees can uncover multiple interactions without prior assumptions. While prevalence rates are typically compared across strata of only one or two independent variables, particularly in public health monitoring and reporting, classification trees enable more efficient utilization of available surveillance data by facilitating the simultaneous analysis of multiple independent variables. These attributes render decision tree methods advantageous compared to traditional regression techniques commonly used in the social and behavioral health sciences. Accordingly, use of classification trees may support a more precise identification of population groups that are heterogeneous in terms of Covid disease [16,17]. Same as hierarchical logistic regression model, small number of studies have used decision tree approaches to examine the factors associated with covid disease.
The present study used both hierarchical logistic regression and classification trees to develop a predictive model for final outcome among covid patients. Hierarchical multiple logistic regression and classification and regression tree (CART) models provide numerous advantages compared to conventional models such as logistic regression. These advantages include enhanced modeling complexity, greater flexibility in modeling, the ability to model interactions between variables, and the capability to detect and distinguish complex patterns. Utilizing hierarchical multiple logistic regression and CART models as alternatives to traditional logistic regression models can enhance the performance and accuracy of statistical analyses in research settings. At first, we used the two model to investigate the association between potential predictors with death of the patient (i.e., live and death) during the COVID-19 pandemic in Shiraz, Iran. Ultimately, the accuracy of the two models in predicting mortality is assessed and compared using appropriate metrics.
Method
In this descriptive-analytical retrospective cohort study, patients who had positive PCR and pneumonia according to physician’s diagnosis and Chest X-ray results were considered as COVID-19 patients. The study’s data collection involved hospital-based records of individuals diagnosed with COVID-19 who were hospitalized for treatment between March 21, 2021, and March 21, 2022. The data were gathered in accordance with the standard admission protocols of healthcare facilities referring to the intensive care units (ICUs) of four hospitals using a convenience sampling method. A total of 1030 COVID-19 patients admitted to the ICUs of these hospitals were identified, with 256 patients allocated to Ali Asghar Hospital, 153 patients to Nemazee Hospital, 480 patients to Shahid Faghihi Hospital, and 141 patients to Shahid Chamran Hospital, ensuring comprehensive data capture by clinical staff. There were no specific inclusion or exclusion criteria in this study; only individuals who tested positive for COVID-19 and were hospitalized at these four centers were eligible.
The method of univariate logistic regression and decision tree model assessed the association of every potential predictor (independent variable) individually with death of the patient (outcome variable).
Demographic particulars, encompassing age, gender, and education level were garnered through a questionnaire. Also, we extracted the patients’ information from the medical files manually in 2022. Clinical characteristics included underlying diseases, history of COVID-19, length of hospitalization, type of medication, category of underlying disease, Oxygen saturation (O2), White Blood Cells count (WBC), C-Reactive Protein (CRP), Serum Glutamic Oxaloacetic Transaminase (SGOT) or AST(Aspartate Aminotransferase), Serum Glutamic Pyruvic Transaminase (SGPT) or ALT(Alanine Aminotransferase), Total bilirubin, Direct bilirubin, and Partial Pressure of Oxygen (Po2), the type of medicine, history of COVID19 and category of underlying disease) were recorded in both hospitalization and discharge time. In this study, a specific questionnaire was designed based on the assumptions, research questions, and variables under investigation.
Statistical analysis
Descriptive statistics, such as means, medians, standard deviations (SDs) and interquartile range (IQR) for continuous variables and frequencies and percentages for categorical variables, were used for all demographic variables. The method of univariate logistic regression assessed the association of every potential predictor individually with death of the patient (outcome variable). Following the univariate analyses, variables showing significant associations with the death were included in two models. The hierarchical logistic regression analyses (method: Enter) and decision tree model were then used to assess the association of each potential predictor with the patient’s death (outcome variable).
Hierarchical multiple logistic regression analyses
The method of Hierarchical multiple logistic regression analyses, In the first step, the death of the patient was assessed regarding their association with significant demographic characteristics. In the second step in the regression analyses, underlying disease, O2 saturation, WBC, type of medicine, history of COVID-19, and category of the underlying disease were entered by enter method in addition to the first step CRP in both hospitalization and discharge time, SGOT, and SGPT in discharge time were entered in the three step, as we aimed to investigate whether the inclusion of these variables increased the prediction accuracy by each block of variables entered in the dependent variable (death of the patient) after controlling for the previously entered variables. In this method, adjusted odds ratios (ORs) and corresponding 95% confidence intervals (CIs) were reported.
Classification and regression trees (or CART)
Based on the results of the univariate logistic regression, variables related to death were selected. CART analysis was performed to identify high-risk populations for increased mortality during COVID-19 and the factors that most deeply influenced the increase in death. The CART model constructs a binary classification system (tree) via recursive partitioning, effectively dividing the dataset into increasingly homogeneous subgroups. At each node, the CART algorithm identifies the explanatory variable and splitting value that optimize discrimination between two outcome classes. A complete CART algorithm continues adding nodes until they achieve homogeneity or contain only a small number of observations (≥ 5, as per standard practice). The challenge in developing a useful tree lies in determining appropriate criteria for pruning. The overarching principle of pruning is that the optimal tree size minimizes misclassification rates for individuals not present in the original dataset [18]. In decision trees, the the relationships between various nodes in the classification tree are logically established based on whether a respondent exhibits a specific characteristic at each node or not. Ultimately, we evaluated the performance of the CART model by computing sensitivity, specificity, and AUC (Area Under Curve) All analyses were performed using the IBM SPSS Statistics for Windows, version 22.0 (IBM Corp, Armonk, NY). The statistical significance level was set at less than 0.05.
Results
Sample characteristics
A total of 1030 patient were investigated between March 2021 and March 2022 in this study. 558 (54.2%) individuals infected with COVID-19 died, and the rest survived.
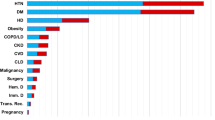
The gender of the patients with COVID-19 was almost equal. Most of the patient’s education was diploma and lower than diploma (668, 87.4%), and the rest had university education. (96, 12.6%( Most of the patients (756, 73.4%) had underlying diseases and had no history of COVID-19 infection (658, 89.9%). The mean age and length of hospitalization of the patients with COVID-19 were 59.66 years old [standard deviation (SD) = 17.10], ranging from 3 to 100 years and 12.32 days [SD = 11.11], with a range of 1- 122 days. Detailed patients’ demographic characteristics are presented in Table 1.
Characteristics of laboratory indicators
The patient’s comprehensive characteristics of laboratory indicators are represented in Table 2. A total of 1030 patients were selected; all patients from this survey were recognized as the COVID-19 cases.
Before exploring the relationship between variables and the binary patient outcome, we conduct a thorough investigation into the selection of relevant and influential variables for model inclusion. Certain variables are chosen based on established knowledge and expert insights extracted from hospital records. This methodology integrates prior knowledge with data-driven analysis to pinpoint crucial variables. Initially, each variable undergoes individual assessment via univariate logistic regression, with those exhibiting a probability value exceeding 0.2 being incorporated into the final model.
Univariate logistic regression models
Univariate logistic regression with the patients who died as a reference group revealed that gender, length of hospitalization, diploma category, all category of underlying disease, all Type of medicine, O2 saturation, WBC, CRP in both hospitalization and discharge time, SGOT and SGPT in discharge time were significantly associated with death characteristics status when analyzed as single predictors, while the other variables did not show a significant association. (Table 3).
Hierarchical multiple logistic regression analyses
The results of multiple hierarchical logistic regression analysis using patient death status as the dependent variable are shown in Table 4. This analysis was conducted in order to examine the contributions of variable blocks entered the prediction of patient death status simultaneously.
In the first step, age, education and length of hospitalization were assessed by inter method. In this block, gender variable made non-significant contributions to the patient’s death status, but age and educational level of the diploma compared to the reference and hospitalization period were significant predictors in this model. In the step 2, underlying diseases, history of COVID-19, type of medicines, O2 saturation, and WBC (in hospitalization and discharge time) were included in the model. In this block, age, educational level of the diploma compared to the reference and hospitalization period, type of medicine of the antiviral compared to the reference, O2 saturation and WBC in discharge were significant predictors in this model, but other variables were not. In the third step, CRP (in hospitalization and discharge time), SGOT, and SGPT (in discharge time) were added. Finally, this model predicted the risk of patients’ death with these variable by inter method.
Based on result, older age (OR = 0.95, p = 0.015) and higher length of hospitalization (OR = 0.96, p=0.019 0.) significantly decreased the chance of survival. Also, discharge WBC, discharge SGOT, and SGPT significantly decreased the chance of survival. Patients with a diploma level of education (OR = 0.1, p = 0.016) were more likely to report death than university graduates. The final model showed that the type of medicine antiviral (OR: 11.10, p = 0.038) than reference (antiviral and corticosteroid), and discharge O2 saturation (OR: 1.10, p < 0.001) had a positive association with the chance of survival, but other variables were not considered as predictive variables.
CART method
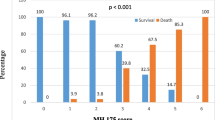
Figure 1 displays the optimal classification tree, segmented by the most influential predictive variable.
Table 5 shows the comparison of the predictive power of the different approaches in terms of the, sensitivity, specificity, and area under the ROC curve. Hierarchical logistic regression and CART models had similar performance. While in the regression model, at each step, adding variables and controlling for previous variables increases the prediction accuracy of the model. The classification model, albeit with a slight difference, has higher accuracy compared to the final regression model.
Predictive models for the final outcome(death) achieved accuracies ranging from 81 to 87% for hierarchical multiple logistic regression and from 87 to 94% for the CART model. Therefore, the CART model performed better than the hirerical multiple logistic regression model. Although the CART model showed higher accuracy, the differences in AUC are not statistically significant, and the results should be interpreted with caution.
Discussion
In this study, the relationship between the demographic, laboratory, and clinical information was investigated in patients with confirmed COVID-19. These patients were selected from those who were admitted in Ali Asghar, Nemazee, Shahid Faqihi and Shahid Chamran hospitals in Shiraz, the capital of Fars province in the south-western Iran. In the present study, no significant relationship was found between mortality and gender, which was inconsistent with the findings of the studies conducted in China and Italy, reporting that COVID-19 mortality rate was higher in men than in women [19, 20].
The Disease Control and Prevention Center in China reported a mortality rate of 2.8% and 1.7% in men and women, respectively [21].
There is also a lack of association between gender and COVID-19 mortality rate in Turkey, which may be related to the similarity of religion in this country and Iran [22, 23].
In addition, the current study showed that COVID-19 mortality rate was higher in the elderly patients, which may be due to the fact that COVID-19 mortality rate is generally higher in patients aged > 55 years [24].
In our study, the duration of hospitalization was 12 days on average, which was close to that in COVID-19 patients admitted to Ghana hospital (10–11 days). However, it was different from the length of hospitalization in patients admitted to Vietnam and China hospitals, which was 19 to 21 days on average [25, 26].
This difference in the length of hospitalization might be due to the difference in the quality of health care systems and the implemented strategies for prevention and control of COVID-19 in different countries. In our study, the patients’ WBC count during hospitalization and discharge, especially at the time of discharge, had a significant relationship with the mortality rate. In general, increased WBC count was associated with increased mortality in our study. The results of our study and that carried out in Uttar Pradesh, India, suggest that absolute neutrophil count and WBC count, which are part of the innate immune system, increased along with the severity of COVID-19 symptoms. When the neutrophil count increases, reactive oxygen species, which can damage the normal and foreign cells, are released and reduce the lymphocyte count needed to fight against infectious diseases. This factor is suitable for measuring and predicting the probability of death due to COVID-19 [27, 28].
In our study, patients with lower education level (high school diploma or lower) had a much lower chance of survival than those who had university education. This finding is probably due to the fact that patients with a lower level of education have less information about the ways to prevent disease transmission and infection, such as how to properly wash hands, strengthen the immune system, wear face mask, and adhere to quarantine principles [29].
In line with a study conducted in Turkey, we also found that patients whose SGOT, SGPT, and CRP levels were uncontrolled and higher at the time of discharge had a lower chance of survival [22].
A significant increase of SGOT, SGPT, and CRP levels can be an indicator of liver failure.
The level of these two enzymes, as an early warning sign of the disease, can help to classify the COVID-19 and pneumonia into mild, moderate, and severe categories and to decide about admission or non-admission of patients in the ICU. In the present study, with the increase of blood O2 saturation rate during hospitalization and discharge, the chances of survival of patients increased, which was in line with the findings of a study done by Oliveira et al. [30].
On the other hand, in our study, the patients who only used antiviral medications had a much better recovery than those who simultaneously took antivirals and corticosteroids. Chang et al., (2022) reported that treatment with corticosteroids was responsive to ARDS diseases other than COVID-19 [31].
Due to their anti-inflammatory and immunosuppressive properties, corticosteroids are used to relieve the symptoms induced by COVID-19.
One of our study limitations included the incompleteness of some of the patients’ medical file. An appropriate sample size (n = 1030) and inclusion of all COVID-19 patients in Shiraz can be the strengths of this study. Future studies are suggested to investigate the problems which occur after being infected with COVID-19.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- WBC:
-
White Blood Cells
- CRP:
-
C-Reactive Protein
- SGOT:
-
Serum Glutamic-Oxaloacetic Transaminase OR AST: Aspartate Aminotransferase
- SGPT:
-
Serum Glutamic Pyruvic Transaminase OR ALT: Alanine Aminotransferase
- po2:
-
Partial Pressure of Oxygen
- CART:
-
Classification And Regression Tree
- AUC:
-
Area under ROC Curve
References
Sahin A-R, Erdogan A, Agaoglu PM, Dineri Y, Cakirci A-Y, Senel M-E, et al. 2019 novel coronavirus (COVID-19) outbreak: a review of the current literature. EJMO. 2020;4(1):1–7.
Suter F, Consolaro E, Pedroni S, Moroni C, Pastò E, Paganini MV et al. A simple, home-therapy algorithm to prevent hospitalisation for COVID-19 patients: a retrospective observational matched-cohort study. EClinicalMedicine. 2021:100941.
Ghebreyesus T. May. World Health Organization. WHO Director-General’s opening remarks at the media briefing on COVID-19-25 2020.
Hsieh Y-H, Lee J-Y, Chang H-L. SARS epidemiology modeling. Emerg Infect Dis. 2004;10(6):1165.
Rahman PNSN, Zaki R, Tan Z, Bibi S, Baghbanzadeh M, Aghamohammadi N, Zhang W, Haque U. Int J Epidemiol. 2020;49:717–26.
Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–62.
Xie J, Covassin N, Fan Z, Singh P, Gao W, Li G, et al. editors. Association between hypoxemia and mortality in patients with COVID-19. Mayo Clinic Proceedings; 2020: Elsevier.
Adhikari SP, Meng S, Wu Y-J, Mao Y-P, Ye R-X, Wang Q-Z, et al. Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of coronavirus disease (COVID-19) during the early outbreak period: a scoping review. Infect Dis Poverty. 2020;9(1):1–12.
Hafeez A, Ahmad S, Siddqui SA, Ahmad M, Mishra S. A review of COVID-19 (coronavirus Disease-2019) diagnosis, treatments and prevention. Ejmo. 2020;4(2):116–25.
Javanmardi F, Keshavarzi A, Akbari A, Emami A, Pirbonyeh N. Prevalence of underlying diseases in died cases of COVID-19: a systematic review and meta-analysis. PLoS ONE. 2020;15(10):e0241265.
Albitar O, Ballouze R, Ooi JP, Ghadzi SMS. Risk factors for mortality among COVID-19 patients. Diabetes Res Clin Pract. 2020;166:108293.
Tazerji SS, Shahabinejad F, Tokasi M, Rad MA, Khan MS, Safdar M et al. Global data analysis and risk factors associated with morbidity and mortality of COVID-19. Gene Rep. 2022:101505.
Emami A, Javanmardi F, Akbari A, Yeganeh BS, Rezaei T, Bakhtiari H, et al. Liver biomarkers assay in COVID-19 cases: a comparison study between alive and dead patients. Iran J Public Health. 2022;51(1):172.
Tjendra Y, Al Mana AF, Espejo AP, Akgun Y, Millan NC, Gomez-Fernandez C, et al. Predicting disease severity and outcome in COVID-19 patients: a review of multiple biomarkers. Arch Pathol Lab Med. 2020;144(12):1465–74.
Malik P, Patel U, Mehta D, Patel N, Kelkar R, Akrmah M, et al. Biomarkers and outcomes of COVID-19 hospitalisations: systematic review and meta-analysis. BMJ evidence-based Med. 2021;26(3):107–8.
Mubayi A. Computational modeling approaches linking health and social sciences: sensitivity of social determinants on the patterns of health risk behaviors and diseases. Handbook of statistics. Elsevier; 2017. pp. 249–304.
Biswas A, et al. Identifying the sociodemographic and work-related factors related to workers’ daily physical activity using a decision tree approach. BMC Public Health. 2023;23(1):1853.
Loh W-Y. Fifty years of classification and regression trees. Int Stat Rev. 2014;82(3):329–48.
Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, Qiu Y, Wang J, Liu Y, Wei Y, Yu T. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–13.
Wenham C, Smith J, Morgan R. COVID-19: the gendered impacts of the outbreak. Lancet. 2020;395(10227):846–8.
Team E. The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19)—China, 2020. China CDC Wkly. 2020;2(8):113.
Ergenc Z, Ergenc H, Araç S, Tör IH, Usanmaz M, Alkılınç E, Karacaer C, Kaya T, Nalbant A, Görgün S, Öztürk A, Yıldırım I. Predictors of disease severity, clinical course, and therapeutic outcome in COVID-19 patients: our experience with 1,700 patients. Eur Rev Med Pharmacol Sci. 2022;26(21):8180–8187. https://doi.org/10.26355/eurrev_202211_30171. PMID: 36394767.
Delanghe JR, Speeckaert MM, De Buyzere ML. COVID-19 related mortality and religious denomination vs. genetics. Clin Chem Lab Med. 2022;60(7):e157-e158. https://doi.org/10.1515/cclm-2022-0393. PMID: 35488443.
Huang X, Wei F, Hu L, Wen L, Chen K. Epidemiology and clinical characteristics of COVID-19. Arch Iran Med. 2020;23(4):268–71. https://doi.org/10.34172/aim.2020.09.
Ashinyo ME, Duti V, Dubik SD, Amegah KE, Kutsoati S, Oduro-Mensah E, Puplampu P, Gyansa-Lutterodt M, Darko DM, Buabeng KO, Ashinyo A. Clinical characteristics, treatment regimen and duration of hospitalization among COVID-19 patients in Ghana: a retrospective cohort study. The Pan African Medical Journal. 2020;37(Suppl 1).
Thai PQ, et al. Factors associated with the duration of hospitalisation among COVID-19 patients in Vietnam: a survival analysis. Epidemiol Infect. 2020;148:1–7. https://doi.org/10.1017/S0950268820001259.
Awale RB, Singh A, Mishra P, Bais PS, Vansh K, Shamim R, et al. Routine hematology parameters in COVID-19: a predictor of disease severity and mortality. J Family Med Prim Care. 2022;11:3423–9.
Yang AP, Liu JP, Tao WQ, Li HM. The diagnostic and predictive role of NLR, d-NLR and PLR in COVID-19 patients. Int Immunopharmacol. 2020;84:106504. https://doi.org/10.1016/j.intimp.2020.106504. Epub 2020 Apr 13. PMID: 32304994; PMCID: PMC7152924.
Guimarães RA, Pinheiro RS, Paula H, Araújo LAd, Gonçalves IAdJ, Pedroso CF, Guilarde AO, Oliveira GAd, Batista K. d.A. Mortality Risk factors for coronavirus infection in hospitalized adults in Brazil: a retrospective cohort study. Int J Environ Res Public Health. 2022;19:14074. https://doi.org/10.3390/ijerph192114074.
Oliveira RMAF, Gorzoni ML, Rosa RF. Mortality predictors in a cohort of patients with COVID-19 admitted to a large tertiary hospital in the city of São Paulo, Brazil: a retrospective study. Sao Paulo Med J. 2022 Sep 12:S1516-31802022005023208. doi: 10.1590/1516-3180.2021.0914.R2.13062022. Epub ahead of print. PMID: 36102455.
Chang X, Li S, Fu Y, et al. Safety and efficacy of corticosteroids in ARDS patients: a systematic review and meta-analysis of RCT data. Respir Res. 2022;23:301. https://doi.org/10.1186/s12931-022-02186-4.
Acknowledgements
The researchers would like to thank Miss Borna for data gathering. The authors would also like to thank Shiraz University of Medical Sciences, Shiraz, Iran and also Center for Development of Clinical Research of Nemazee Hospital and Dr. Nasrin Shokrpour for editorial assistance.
Funding
This research was financially supported by Shiraz University of medical science of Shiraz, Iran. The funding source had no role in the design of the study, data collection, analysis, interpretation of results, or writing of the manuscript.
Author information
Authors and Affiliations
Contributions
PGH and ZM aided in the conceptualization, design, and critical revision of the final manuscript, ZM, MR, PGH, MMR, SG and BKH, aided in design, preparation of manuscript and critical revision of the final manuscript. ZM, PGH aided in data analysis and critical revision of the final manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
I hereby confirm that all experimental protocols conducted in this study were approved by the Shiraz University of Medical Sciences, Iran, based on a proposal with grant number 21032 and the Ethics code number IR.SUMS.NUMIMG.REC.1401.011 issued on 18.10.1401. In addition, informed consent was obtained from all subjects or their legal guardian(s) prior to their participation in the research.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mohebbi, Z., Ghaemmaghami, P., Rajaei, M. et al. The association between potential predictors and death of patients during the COVID-19 pandemic in Shiraz: a hierarchical multiple regression analysis. BMC Public Health 24, 1975 (2024). https://doi.org/10.1186/s12889-024-19372-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-19372-2