Abstract
Background
The weight-adjusted waist index (WWI) is a quantitative anthropometric index that can be applied to evaluate obesity. This study examined the relationship between adult United States (US) residents’ risk of diabetes mellitus type 2 (T2DM) and WWI.
Methods
The NHANES (National Health and Nutrition Examination Survey) 2001–2018 provided the data for this investigation. This study used multifactorial logistic regression analysis, smoothed curve fitting, subgroup analysis, and interaction tests to assess the association between WWI and T2DM. Additionally, threshold effects were calculated using a two-stage linear regression model. The receiver operating characteristic(ROC) curves evaluated the diagnostic ability of the WWI and commonly used obesity indicators.
Results
20,477 participants were enrolled in the analysis, and patients with greater levels of WWI had a higher prevalence of T2DM. WWI and T2DM have a non-linear relationship, with a positive association found on the left side of the breakpoint (WWI = 12.35) (OR = 1.82, 95%CI:1.64–2.02), whereas, on the right side, no such relationship was found (OR = 0.9, 95%CI:0.61–1.34). For every unit rise in WWI, the probability of having T2DM increased by 67% after controlling for all other variables (OR:1.67,95%CI:1.53–1.83). Based on subgroup analyses, individuals under 40 had a higher correlation between WWI and T2DM (P < 0.001).ROC analyses showed that WWI had the best discrimination and accuracy in predicting T2DM compared to other obesity indicators (WC, BMI, and Weight).
Conclusion
Higher WWI values had a higher prevalence of T2DM in US individuals, especially in adults under 40. WWI has the strongest ability to predict T2DM. Therefore, the importance of WWI in the early identification of T2DM in US adults should be emphasized.
Similar content being viewed by others
Introduction
T2DM is a chronic metabolic disease that often leads to damage to the cardiovascular system and is the most common cause of death in people with type 2 diabetes [1], and it has been estimated that about 6.7 million people will die from diabetes or diabetes complications in 2021 alone [2].T2DM is spreading and becoming more prevalent, making it a major global healthcare burden and public health problem [3]. The number of people with diabetes is projected to rise to 783 million by 2025 [4]. Healthcare expenditures for people with diabetes are three times higher than for the general non-diabetic population, with $673 billion spent on the treatment of diabetes and its associated complications alone in 2015 [4]. T2DM complications are difficult to reverse once they have occurred; however, clinical trials have demonstrated that people with T2DM can be prevented through a healthy diet and aerobic exercise [5,6,7]. Despite the availability of clinical guidelines for T2DM and its complications, the prevention and management of T2DM remains poor overall. Therefore, there is an urgent need to develop and implement new preventive and therapeutic strategies for the early detection to recognize T2DM.
Obesity has become an important global health problem [8]. Obesity, especially abdominal obesity, is strongly associated with the development of diabetes [9,10,11]. Previously, obesity was customarily assessed by body mass index (BMI) and waist circumference (WC), which are often used in combination for a more comprehensive assessment of central obesity risk, especially abdominal fat accumulation [12, 13]. However, BMI does not differentiate between body fat distribution [14] and WC does not differentiate between visceral and subcutaneous fat, a drawback found in previous studies, which showed that even people with low levels of both BMI and WC have visceral obesity and are at a similarly high risk of developing diabetes [15]. Therefore, a new obesity index called WWI (waist circumference divided by the square root of body weight) was proposed. WWI distinguishes between fat and muscle mass and explains centripetal obesity, which is not related to body weight [16,17,18]. In addition, WWI has the advantage of being proportional to age, reflecting changes in abdominal composition with age. It has been found that WWI can predict the changes that occur in fat and muscle composition associated with aging, and these changes can be used in a variety of populations [19, 20].
It has been found that increased WWI may be associated with the development of cardiovascular disease and non-alcoholic fatty liver [21,22,23]. It has been demonstrated that WWI was positively associated with T2DM [24]. Therefore, the present study further expanded the sample compared to previous studies by using NHANES data from 2001 to 2018 to investigate the relationship between WWI and T2DM in the US adult population, and to explore the predictive role of commonly used obesity indicators in the development of T2DM, and to find better indicators for early identification of the development of T2DM.
Methods
Survey description
This cross-sectional investigation included 91,348 participants, and all population data were isolated from the NHANES database. This database survey plays a critical role in providing comprehensive data that helps researchers and healthcare professionals understand health and nutrition trends. This survey uses a multistage, stratified, subgroup probability sampling investigation design. Every participant signed a written informed consent form, which was authorized by the NCHS Ethics Review Board [25, 26].
Study population
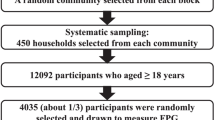
The NHANES database from 2001 to 2018 was used for this study. Initially, participants with T2DM and WWI data were integrated into our investigation. A total of 91,348 individuals were enlisted in the research, excluding patients with missing data on WWI (n = 15094), T2DM diagnosis (n = 49,132), age less than 20 years (n = 6032), and pregnant women (n = 622). For our final analysis, included in this study were 20,477 adults with complete data. (Fig. 1)
Exposure and outcome variables
The exposure variable WWI (cm/√kg) is an innovative anthropometric measurement of central obesity. The measurement is taken by a licensed healthcare professional who has received the necessary training. The subject’s abdomen is relaxed, and the waist circumference is measured horizontally around the abdomen to ensure data accuracy. The soft ruler is placed on the right midline of the axilla, which is the midpoint of the line connecting the upper edge of the iliac bone and the lower border of the 12th rib. Weight was recorded using a digital scale [27]. Subsequently, all participants were categorized into quartiles based on transforming the WWI continuous variable into a categorical variable. The outcome variable was T2DM, and participants in this study were identified as T2DM cases based on the relevant questionnaires and laboratory tests that met the following criteria: fasting blood glucose (FBG) ≥ 7 mmol/L; glycosylated hemoglobin (HbA1c%) ≥ 6.5%; 2-hour blood glucose ≥ 11.1 mmol/L at the time of the oral glucose tolerance test (OGTT); your doctor has told you that you have diabetes and you have been taking oral glucose-lowering medication or insulin injection [28, 29].
Covariates
The study included covariates that might confound the correlation between WWI and T2DM, the study categorized participants into different racial groups, including Mexican Americans, non-Hispanic Whites, non-Hispanic Blacks, and other races. Education levels were classified into three categories: less than high school, high school or general educational development (GED), and above high school. Household income was defined using the poverty-income ratio (PIR), with three categories: low income (PIR < 1.3), moderate income (1.3 ≤ PIR < 3.5), and high income (PIR ≥ 3.5) [30]. Smoking status was categorized as current, former, or never smokers. Alcohol intake was assessed with a “yes or no” question related to consuming at least 12 drinks per year. Physical activity was categorized into three groups: the inactive group, consisting of individuals not physically active in their leisure time, and the moderate and vigorous group, based on questions about weekly cycles of moderate-intensity and vigorous exercise. Total energy intake was obtained from dietary interviews and the NHANES database, with the dietary interviews conducted in part by the United States Department of Agriculture (USDA) and the United States Department of Health and Human Services (DHHS), with the National Center for Health Statistics (NCHS) being responsible for all aspects of the survey sample design and data collection, and with the USDA Food Surveys and Research Group (FSRG) being responsible for the dietary data collection methodology and for data review and processing. All NHANES participants were asked to conduct two 24-hour dietary recall interviews, with the first dietary interview conducted at a Mobile Examination Center (MEC) and the second interview conducted by telephone 3 to 10 days later. Total energy intake was obtained from the two 24-hour dietary recalls and averaged [31]. BMI was calculated using the formula weight (kg)/height (m²), and participants were categorized as normal weight (< 25 kg/m²), overweight (25–30 kg/m²), or obese (≥ 30 kg/m²). Hypertension was defined by self-reported high blood pressure, systolic blood pressure ≥ 140 mmHg, diastolic blood pressure ≥ 90 mmHg [32]. The complete measurement technique for these variables is easily accessible in the NHANES database.
Statistical analysis
This study utilized R (version 4.2) and Empower software (version 5.0) for statistical analyses, adhering to NHANES analysis guidelines and considering appropriate sample weights. Statistical significance was set at P < 0.05. Continuous variables were expressed as mean standard deviation and categorical variables as numbers and percentages. Continuous variables were tested for normality, and if they did not conform to normal distribution, the Kruskal-Wallis test was used for nonparametric tests, the U test was used for conformity to normal distribution, and the chi-square test was used for categorical variables. The association between WWI and diabetes mellitus was explored via multivariate logistic regression analysis. The models used for analysis were: Model 1: Unadjusted data. Model 2: Adjusted for age, sex, and race. Model 3: Adjusted for age, sex, race, education, BMI, poverty-to-income ratio, smoking status, alcohol intake, HDL, LDL, hypertension, physical activity, and total energy intake. Subgroup analyses were conducted to test interactions among variables like age, sex, BMI, and hypertension. Insignificant interaction p-values implied reliable results across populations; otherwise, specific populations might exhibit different outcomes. The study employed smoothed curve fitting to explore nonlinear correlations between WWI and T2DM. Upon detecting a nonlinear relationship, a recursive algorithm determined the significant inflection point of the WWI-T2DM relationship, followed by threshold effect analysis. This meticulous statistical approach allowed for a comprehensive exploration and understanding of the relationship between WWI and T2DM within the studied population.
Results
Baseline characteristics
The study included a sample of 20,477 adults aged 20 years or older, with 18.11% having Type 2 diabetes mellitus (T2DM). The average age was (50.15 ± 17.80) years with a roughly equal distribution of males (49.68%) and females (50.32%). The WWI was categorized into quartiles: Q1 (8.38–10.45), Q2 (10.45–11.02), Q3 (11.02–11.61), and Q4 (11.61–15.52). Variables such as age, gender, education, race, BMI, poverty-to-income ratio, smoking status, alcohol intake, HDL, LDL, hypertension, physical activity, and total energy intake exhibited statistically significant differences among the four WWI quartiles (all p < 0.05). Compared to those in the lowest WWI quartile, individuals in the highest WWI quartile were more likely to be female, elderly, non-Hispanic whites and Mexican Americans, less educated, inactive, smokers, and alcohol consumers. Additionally, a positive association was observed between higher WWI levels and hypertension, BMI, and LDL levels, while lower levels of total dietary energy, poverty-to-income ratio, and HDL were noted in the highest WWI quartile (Table 1). This detailed analysis provides a comprehensive overview of the demographic and health-related characteristics of the study participants across different WWI quartiles, shedding light on potential associations with T2DM.
Association of WWI with T2DM
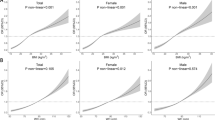
Table 2 investigates the relationship between WWI continuous and categorical variables and T2DM. A higher risk of developing T2DM appears to be linked to higher WWI, according to the current findings. In all multifactorial logistic regression models (Model 1: OR = 2.83, 95% CI: 2.69–2.97; Model 2: OR = 2.46, 95% CI: 2.32–2.60; Model3: OR = 1.67,95% CI:1.53–1.83), increased WWI was positively associated with a higher risk of developing T2DM. In model 3, after adjusting for potential confounding variables, there was a 42% increase in the chance of developing T2DM for every unit increase in WWI. Furthermore, this trend remained statistically significant after WWI was classified as a categorical variable, with the risk of developing T2DM in the higher WWI quartile being 1.96 times higher than in the lowest WWI quartile in all multivariate logistic regression models (OR = 2.96,95%CI:2.35–3.73). Smooth curve fitting revealed a nonlinear relationship between WWI and T2DM (Fig. 2). In the fully adjusted model, a nonlinear inverse L-shaped association was detected between WWI and T2DM, with a threshold effect analysis yielding a breakpoint point (K) of 12.35, and to the left of the breakpoint WWI was significantly and positively correlated with T2DM (OR = 1.82, 95% CI:1.64–2.02, P < 0.0001). On the right side of the breakpoint, however, there was no remarkable correlation between WWI and T2DM (OR = 0.90, 95% CI:0.61–1.34, P = 0.6106). The test P value for the log-likelihood ratio was 0.001(Table 3).
Subgroup analysis
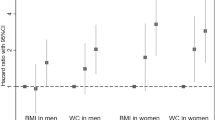
The associations between WWI and the risk of developing type 2 diabetes were found to be stable (all P < 0.05) in subgroup analyses and interaction tests stratified by age, sex, BMI, and hypertension. However, it was found that the most crucial interaction factor affecting the connection between WWI and T2DM was age, and subgroup analyses suggested a stronger association between WWI and T2DM among participants aged < 40 years (P < 0.001). In the population without hypertension, the relationship between WWI and T2DM was more substantial than in the hypertensive population (P < 0.05). The positive correlation between WWI and T2DM was comparable in populations with different gender and BMI status and may exert in different populations (Fig. 3).
ROC analysis
In this cross-sectional study, the area under the curve (AUC) values were calculated to compare the predictive accuracy of WWI with other obesity indicators (WC, BMI, and Weight) for T2DM (Fig. 4). We found that the AUC value of WWI was higher than the other 3 obesity indicators in predicting T2DM, T2DM: AUC (95% CI): 0.7332 (0.7249–0.7416). The difference in AUC values between WWI and the other obesity indicators was statistically significant (all P < 0.001) indicating that WWI was the most accurate predictor of T2DM compared to WC, BMI, and Weight, WWI was the best predictor of T2DM (Table 4).
Discussion
Assessing the relationship between the adult US population between WWI and T2DM was the aim of this study. In this cross-sectional study that recruited 20,477 participants, there was a nonlinear relationship between the chance of getting T2DM and WWI, with WWI to the left of the breakpoint being significantly and positively associated with T2DM prevalence (WW I = 12.35). WWI to the left of the breakpoint was positively associated with T2DM prevalence, whereas the association to the right was not statistically significant. Tests of interactions and subgroup analysis supported the strength of this positive correlation across BMI and gender, especially in the adult population aged < 40 years, where there was a stronger association between WWI and T2DM (interaction P < 0.001). According to these findings, < 40 years of young adults’ development of type 2 diabetes may be independently correlated with elevated WWI.
Obesity is increasingly becoming a health problem worldwide, and it has a substantial correlation with the emergence of numerous illnesses. In particular, it targets the recognized harmful intra-abdominal cellulite. An extraordinary association between the occurrence of T2DM and abdominal obesity has been demonstrated by earlier research [33]. Although T2DM has been linked to traditional obesity-related indices like waist-to-hip ratio (WHR), WC, and BMI, there is still an obesity paradox. BMI has several limitations. The fact that it cannot discriminate between muscle and fat mass is one of its primary disadvantages. Because people with significant muscle mass tend to have higher BMIs, BMI may not be a reliable indicator of how body fat is distributed. In addition, racial disparities, gender, and age all have an impact on the validity of BMI. In elderly adults, changes may occur in muscle mass and fat distribution. Therefore, Weight gain resulting from high lean body mass and high-fat body mass cannot be distinguished by BMI [34, 35]. There are also non-traditional obesity indicators that, despite widespread interest, are difficult to quantify and have extremely limited practical clinical application. There are also indicators with highly centralized mean values and slight variance, which make it impossible to determine a clinical threshold, leading to limited clinical practice [36].
The WWI is a new obesity index that combines the advantages of WC with lessening its impacts, making it a more accurate and thorough measure for assessing abdominal obesity. WWI is applicable to various racial and demographic groups, and the outcomes could be more dependable and consistent when presented in multicenter or cross-racial research [37]. Park et al. found that a new and reliable obesity index, WWI, was developed by a considerable cohort study in South Korea by investigating and calculating waist circumference and body weight data of 465,629 subjects, suggesting that WWI may be independent of BMI in predicting T2DM in subjects with average and high body mass index [38]. In their study, Kim et al. stated that WWI had a positive correlation with fat mass and a negative correlation with bone and muscle mass [39]. Yu et al. conducted a prospective study in which they discovered a substantial and positive correlation between the incidence of new-onset T2DM and an increase in WWI among 9205 non-diabetic rural adult patients from northeastern China [40]. Sun et al. revealed that in the Japanese population, WWI had a positive and linear relationship with new-onset T2DM, which can be used as an indicator of weight control in managing patients with T2DM [41]. The above studies demonstrated the reliability and promising application of WWI. The initial study is the one that examined the connection between WWI and T2DM prevalence. In adult Americans. Additionally, a cross-sectional analysis was carried out by the researchers to look into this relationship. According to the current data, there appears to be a positive correlation between increased WWI and T2DM. That correlation is powerful in individuals under 40, which could be explained by the different distribution of body fat between younger and older adults [42]. The above investigations in different racial populations similarly demonstrated the stability of the WWI index in different racial populations. In summary, the WWI index is simple to calculate, has stability in predicting T2DM, and can predict the occurrence of T2DM early, thus potentially reducing the incidence of T2DM.
Obesity is associated with the development and progression of T2DM. However, the underlying mechanistically, leptin, lipocalin, and other adipokines, as well as a variety of bioactive proteins like tumor necrosis factor and interleukin 6 (IL-6), can be continuously secreted by visceral adipose tissue, which promotes the body to experience hypoxic stress and inflammatory response and impair pancreatic β-cell function [43, 44]. On the other hand, obesity is closely related to dysregulation of lipid and glucose metabolism [45]. Metabolic disorders are closely associated with lipocalin, cellular oxidative stress [13], and the renin-angiotensin-aldosterone system [14], it eventually results in the loss of pancreatic islet β-cells and insulin resistance, which in turn causes diabetes mellitus [46,47,48,49]. In addition, during visceral adipose tissue accumulation, pro-inflammatory macrophages in adipose further contribute to the immuno-permeability of the organs [47]. Specific isoforms of adipose-derived ceramidase can reduce insulin activity and lead to insulin resistance [48]. Age-related changes to body composition include the reorganization of fat mass, which increases the likelihood of ectopic fat deposition in the liver and skeletal muscle as well as visceral fat deposition in the abdomen. Research has indicated that beyond the age of 20, there is a 2–3% decrease in the rate of resting energy expenditure per decade [49]. Our study further emphasizes and validates that controlling abdominal obesity is crucial in reducing the risk of T2DM.
This study found that people in the highest quartile of WWI were more likely to be female, elderly, and inactive compared to those in the lowest quartile of WWI, while total dietary energy was relatively low, previous studies have found that overweight/obesity occurs when energy intake chronically exceeds energy expenditure [50]. However, with aging and declining physical activity, even when energy intake from food decreases and body weight decreases, waist circumference may also increase and is considered to be related to decreased growth hormone secretion, delayed hypogonadism, changes in thyroid and adrenal function, insulin, and changes in appetite-related peptides (leptin, ghrelin) [51]. It has been found that high-protein diets are effective in weight loss and that high protein can help control weight by increasing satiety and thermogenesis and maintaining/increasing fat-free mass, but increasing protein intake at the expense of fat or carbohydrates and decreasing starch intake by increasing other macronutrients may bring about weight loss while increasing waist circumference [52, 53]. Human nutritional intake includes sugar protein fat catabolism, only total energy intake was analyzed in this study, and future studies will be conducted to investigate the effects of different nutrient intakes on WWI in adults to find a healthier diet to combat abdominal obesity.
Comparison with previous studies
This study has various advantages. Unlike previous studies on WWI and T2DM [24], this paper adjusted various confounders in the model as much as possible, increasing factors such as energy intake. Hence, we used more comprehensive and representative data from the NHANES database in the study and obtained more reliable results by adjusting the model to exclude the influence of confounders to the greatest extent. Second, this article studies the prediction of WWI, weight, WC, and BMI on the prediction of T2DM in adults, and finds for the first time that WWI may be a better predictor of T2DM than weight, WC, and BMI, which provides a direction for us to prevent and reduce the risk of T2DM in adults through the measurement of WWI.
Limitations
This research is imperative to acknowledge the limitations. First, due to the cross-sectional study design of this study, the authors could not obtain a clear causal relationship to distinguish the association between WWI and diagnosed or newly occurring diabetes. Despite using a nationally representative dataset, the authors’ results are based on information from 2001 to 2018, with the most recent data coming from 5 years ago, subject to data bias. Second, the influence of additional potential confounders could not be totally ruled out by the authors, even after some potential covariates were taken into account.
Conclusion
In summary, this investigation discovered an obvious correlation between the incidence of T2DM and WWI. This implies WWI could be a biomarker for T2DM in American adults under 40, potentially aiding in the management and prevention of T2DM in the adult population. However, future confirmation of this will require numerous prospective studies.
Data availability
Data is provided within the manuscript or supplementary information files.The database used for this study can be found in online repositories. For more information, visit https://www.cdc.gov/nchs/nhanes/index.htm.
References
Raev DC. Which left ventricular function is impaired earlier in the evolution of diabetic cardiomyopathy? An echocardiographic study of young type I diabetic patients. Diabetes Care. 1994;177:633–9. https://doi.org/10.2337/diacare.17.7.633.
Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the International Diabetes Federation Diabetes Atlas, 9(th) edition. Diabetes Res Clin Pract. 2019;157:107843. https://doi.org/10.1016/j.diabres.2019.107843.
Cloete L. Diabetes mellitus: an overview of the types, symptoms, complications and management. Nurs Stand. 2022;371:61–6. https://doi.org/10.7748/ns.2021.e11709.
Boyle JP, Thompson TJ, Gregg EW, Barker LE, Williamson DF. Projection of the year 2050 burden of diabetes in the US adult population: dynamic modeling of incidence, mortality, and prediabetes prevalence. Popul Health Metr. 2010;8:29. https://doi.org/10.1186/1478-7954-8-29.
Park KS. The search for genetic risk factors of type 2 diabetes mellitus. Diabetes Metab J. 2011;351:12–22. https://doi.org/10.4093/dmj.2011.35.1.12.
Weisman A, Fazli GS, Johns A, Booth GL. Evolving trends in the epidemiology, risk factors, and Prevention of type 2 diabetes: a review. Can J Cardiol. 2018;345:552–64. https://doi.org/10.1016/j.cjca.2018.03.002.
Shubrook JH, Chen W, Lim A. Evidence for the Prevention of type 2 diabetes Mellitus. J Am Osteopath Assoc. 2018;11811:730–7. https://doi.org/10.7556/jaoa.2018.158.
Fang H, Berg E, Cheng X, Shen W. How to best assess abdominal obesity. Curr Opin Clin Nutr Metab Care. 2018;215:360–5. https://doi.org/10.1097/MCO.0000000000000485.
Sahakyan KR, Somers VK, Rodriguez-Escudero JP, Hodge DO, Carter RE, Sochor O, et al. Normal-weight central obesity: implications for Total and Cardiovascular Mortality. Ann Intern Med. 2015;16311:827–35. https://doi.org/10.7326/M14-2525.
Kivimaki M, Kuosma E, Ferrie JE, Luukkonen R, Nyberg ST, Alfredsson L, et al. Overweight, obesity, and risk of cardiometabolic multimorbidity: pooled analysis of individual-level data for 120 813 adults from 16 cohort studies from the USA and Europe. Lancet Public Health. 2017;26:e277–85. https://doi.org/10.1016/S2468-2667(17)30074-9.
Ahn N, Baumeister SE, Amann U, Rathmann W, Peters A, Huth C, et al. Visceral adiposity index (VAI), lipid accumulation product (LAP), and product of triglycerides and glucose (TyG) to discriminate prediabetes and diabetes. Sci Rep. 2019;91:9693. https://doi.org/10.1038/s41598-019-46187-8.
Pinho CPS, Diniz ADS, De Arruda IKG, Leite A, Petribu MMV, Rodrigues IG. Predictive models for estimating visceral fat: the contribution from anthropometric parameters. PLoS ONE. 2017;127:e0178958. https://doi.org/10.1371/journal.pone.0178958.
Wu L, Zhu W, Qiao Q, Huang L, Li Y, Chen L. Novel and traditional anthropometric indices for identifying metabolic syndrome in non-overweight/obese adults. Nutr Metab (Lond). 2021;181:3. https://doi.org/10.1186/s12986-020-00536-x.
Elagizi A, Kachur S, Lavie CJ, Carbone S, Pandey A, Ortega FB, et al. An overview and update on obesity and the obesity Paradox in Cardiovascular diseases. Prog Cardiovasc Dis. 2018;612:142–50. https://doi.org/10.1016/j.pcad.2018.07.003.
Gulati S, Misra A. Abdominal obesity and type 2 diabetes in Asian indians: dietary strategies including edible oils, cooking practices and sugar intake. Eur J Clin Nutr. 2017;717:850–7. https://doi.org/10.1038/ejcn.2017.92.
Park Y, Kim NH, Kwon TY, Kim SG. A novel adiposity index as an integrated predictor of cardiometabolic disease morbidity and mortality. Sci Rep. 2018;81:16753. https://doi.org/10.1038/s41598-018-35073-4.
Li X, Wang L, Zhou H, Xu H. Association between weight-adjusted-waist index and chronic kidney disease: a cross-sectional study. BMC Nephrol. 2023;241:266. https://doi.org/10.1186/s12882-023-03316-w.
Kim NH, Park Y, Kim NH, Kim SG. Weight-adjusted waist index reflects fat and muscle mass in the opposite direction in older adults. Age Ageing. 2021;503:780–6. https://doi.org/10.1093/ageing/afaa208.
Kim JY, Choi J, Vella CA, Criqui MH, Allison MA, Kim NH. Associations between Weight-Adjusted Waist Index and Abdominal Fat and muscle Mass: multi-ethnic study of atherosclerosis. Diabetes Metab J. 2022;465:747–55. https://doi.org/10.4093/dmj.2021.0294.
Tao J, Zhang Y, Tan C, Tan W. Associations between weight-adjusted waist index and fractures: a population-based study. J Orthop Surg Res. 2023;181:290. https://doi.org/10.1186/s13018-023-03776-8.
Hu Q, Han K, Shen J, Sun W, Gao L, Gao Y. Association of weight-adjusted-waist index with non-alcoholic fatty liver disease and liver fibrosis: a cross-sectional study based on NHANES. Eur J Med Res. 2023;281:263. https://doi.org/10.1186/s40001-023-01205-4.
Li H, Fang G, Huang C, An W, Bai X, Huang Y. Association between the weight-adjusted Waist Index and serum uric acid: a cross-sectional study. Int J Clin Pract. 2023;2023(8215866). https://doi.org/10.1155/2023/8215866.
Fang H, Xie F, Li K, Li M, Wu Y. Association between weight-adjusted-waist index and risk of cardiovascular diseases in United States adults: a cross-sectional study. BMC Cardiovasc Disord. 2023;231:435. https://doi.org/10.1186/s12872-023-03452-z.
Zheng D, Zhao S, Luo D, Lu F, Ruan Z, Dong X, et al. Association between the weight-adjusted waist index and the odds of type 2 diabetes mellitus in United States adults: a cross-sectional study. Front Endocrinol (Lausanne). 2023;14:1325454. https://doi.org/10.3389/fendo.2023.1325454.
Wang H, Lv Y, Ti G, Ren G. Association of low-carbohydrate-diet score and cognitive performance in older adults: National Health and Nutrition Examination Survey (NHANES). BMC Geriatr. 2022;221:983. https://doi.org/10.1186/s12877-022-03607-1.
Huang D, Zhong S, Yan H, Lai S, Lam M, Jia Y. Association between serum zinc levels and suicidal ideation in US adults: a population-based cross-sectional study. J Affect Disord. 2023;329:359–68. https://doi.org/10.1016/j.jad.2023.02.039.
Guo F, Wang M, Guo X, Pu L, Sun M, Li S, et al. The association between fatty acid intake and breast cancer based on the NHANES and mendelian randomization study. Cancer Epidemiol. 2021;73:101966. https://doi.org/10.1016/j.canep.2021.101966.
Huang W, Ma X, Liang H, Li H, Chen J, Fang L, et al. Dietary Magnesium Intake Affects the Association between Serum Vitamin D and type 2 diabetes: a cross-sectional study. Front Nutr. 2021;8:763076. https://doi.org/10.3389/fnut.2021.763076.
Li B, Chen L, Hu X, Tan T, Yang J, Bao W, et al. Association of serum uric acid with all-cause and Cardiovascular Mortality in Diabetes. Diabetes Care. 2023;462:425–33. https://doi.org/10.2337/dc22-1339.
Mazidi M, Katsiki N, Mikhailidis DP, Sattar N, Banach M. Lower carbohydrate diets and all-cause and cause-specific mortality: a population-based cohort study and pooling of prospective studies. Eur Heart J. 2019;4034:2870–9. https://doi.org/10.1093/eurheartj/ehz174.
Johnson CL, Paulose-Ram R, Ogden CL, Carroll MD, Kruszon-Moran D, Dohrmann SM, et al. National health and nutrition examination survey: analytic guidelines, 1999–2010. Vital Health Stat. 2013;2:161: 1–24. https://www.ncbi.nlm.nih.gov/pubmed/25090154.
Piche ME, Tchernof A, Despres JP. Obesity phenotypes, diabetes, and Cardiovascular diseases. Circ Res. 2020;12611:1477–500. https://doi.org/10.1161/CIRCRESAHA.120.316101.
Kim NH, Lee J, Kim TJ, Kim NH, Choi KM, Baik SH, et al. Body Mass Index and Mortality in the General Population and in subjects with chronic disease in Korea: a Nationwide Cohort Study (2002–2010). PLoS ONE. 2015;1010:e0139924. https://doi.org/10.1371/journal.pone.0139924.
Fenger-Gron M, Overvad K, Tjonneland A, Frost L. Lean body Mass is the predominant anthropometric risk factor for Atrial Fibrillation. J Am Coll Cardiol. 2017;6920:2488–97. https://doi.org/10.1016/j.jacc.2017.03.558.
Ji M, Zhang S, An R. Effectiveness of a body shape index (ABSI) in predicting chronic diseases and mortality: a systematic review and meta-analysis. Obes Rev. 2018;195:737–59. https://doi.org/10.1111/obr.12666.
Kim KJ, Son S, Kim KJ, Kim SG, Kim NH. Weight-adjusted waist as an integrated index for fat, muscle and bone health in adults. J Cachexia Sarcopenia Muscle. 2023. https://doi.org/10.1002/jcsm.13302.
Yu S, Wang B, Guo X, Li G, Yang H, Sun Y. Weight-adjusted-Waist Index predicts newly diagnosed diabetes in Chinese rural adults. J Clin Med. 2023;124. https://doi.org/10.3390/jcm12041620.
Sun H, Li Y, Shi J, Li K, Zhao Y, Shang L, et al. Weight-adjusted waist index is not superior to conventional anthropometric indices for predicting type 2 diabetes: a secondary analysis of a retrospective cohort study. Fam Pract. 2023. https://doi.org/10.1093/fampra/cmad047.
Szulc P, Duboeuf F, Chapurlat R. Age-related changes in Fat Mass and distribution in men-the cross-sectional STRAMBO study. J Clin Densitom. 2017;204:472–9. https://doi.org/10.1016/j.jocd.2016.08.003.
Tagi VM, Chiarelli F. Obesity and insulin resistance in children. Curr Opin Pediatr. 2020;324:582–8. https://doi.org/10.1097/MOP.0000000000000913.
Han W, Yang S, Xiao H, Wang M, Ye J, Cao L, et al. Role of Adiponectin in Cardiovascular diseases related to glucose and lipid metabolism disorders. Int J Mol Sci. 2022;2324. https://doi.org/10.3390/ijms232415627.
Magliano DJ, Sacre JW, Harding JL, Gregg EW, Zimmet PZ, Shaw JE. Young-onset type 2 diabetes mellitus - implications for morbidity and mortality. Nat Rev Endocrinol. 2020;166:321–31. https://doi.org/10.1038/s41574-020-0334-z.
Kumar P, Liu C, Suliburk J, Hsu JW, Muthupillai R, Jahoor F, et al. Supplementing Glycine and N-Acetylcysteine (GlyNAC) in older adults improves glutathione Deficiency, oxidative stress, mitochondrial dysfunction, inflammation, physical function, and Aging Hallmarks: a Randomized Clinical Trial. J Gerontol Biol Sci Med Sci. 2023;781:75–89. https://doi.org/10.1093/gerona/glac135.
Kalupahana NS, Moustaid-Moussa N. The renin-angiotensin system: a link between obesity, inflammation and insulin resistance. Obes Rev. 2012;132:136–49. https://doi.org/10.1111/j.1467-789X.2011.00942.x.
Sramek J, Nemcova-Furstova V, Kovar J. Molecular mechanisms of apoptosis induction and its regulation by fatty acids in pancreatic beta-cells. Int J Mol Sci. 2021;228. https://doi.org/10.3390/ijms22084285.
Yao D, Gangyi Y, Qinan W. Autophagic dysfunction of beta cell dysfunction in type 2 diabetes, a double-edged sword. Genes Dis. 2021;84:438–47. https://doi.org/10.1016/j.gendis.2020.03.003.
Bijnen M, Josefs T, Cuijpers I, Maalsen CJ, Van De Gaar J, Vroomen M, et al. Adipose tissue macrophages induce hepatic neutrophil recruitment and macrophage accumulation in mice. Gut. 2018;677:1317–27. https://doi.org/10.1136/gutjnl-2016-313654.
Ghaben AL, Scherer PE. Adipogenesis and metabolic health. Nat Rev Mol Cell Biol. 2019;204:242–58. https://doi.org/10.1038/s41580-018-0093-z.
Ahmed B, Sultana R, Greene MW. Adipose tissue and insulin resistance in obese. Biomed Pharmacother. 2021;137. https://doi.org/10.1016/j.biopha.2021.111315.
Blackburn GL, Wollner S, Heymsfield SB. Lifestyle interventions for the treatment of class III obesity: a primary target for nutrition medicine in the obesity epidemic. Am J Clin Nutr. 2010;911:S289–92. https://doi.org/10.3945/ajcn.2009.28473D.
Michalakis K, Goulis DG, Vazaiou A, Mintziori G, Polymeris A, Abrahamian-Michalakis A. Obesity in the ageing man. Metabolism. 2013;6210:1341–9. https://doi.org/10.1016/j.metabol.2013.05.019.
Westerterp-Plantenga MS, Lemmens SG, Westerterp KR. Dietary protein - its role in satiety, energetics, weight loss and health. Br J Nutr. 2012;108(Suppl 2):S105–12. https://doi.org/10.1017/S0007114512002589.
Agnoli C, Sieri S, Ricceri F, Macciotta A, Masala G, Bendinelli B, et al. Macronutrient composition of the diet and long-term changes in weight and waist circumference in the EPIC-Italy cohort. Nutr Metab Cardiovasc Dis. 2021;311:67–75. https://doi.org/10.1016/j.numecd.2020.08.007.
Acknowledgements
DeclarationsEthics approval and consent to participateThe study was approved by the National Centre for Health Statistics Research Ethics Review Board, and every participant signed informed consent.Availability of data and materialsThe database used for this study can be found in online repositories. For more information, visit https://www.cdc.gov/nchs/nhanes/index.htm.Competing interestsThe authors declare no competing interests.FundingNot applicable. Authors’ contributionsXinMeng Li: conceptualization, statistical analysis, manuscript writing, and editing. Hongkun Wang: methodology, reviewing and editing. Dan Zhao: statistical analysis. The author(s) read and approved the final manuscript.
Funding
Not applicable.
Ethics declarations
Ethics approval and consent to participate
The study was approved by the National Centre for Health Statistics Research Ethics Review Board, and every participant signed informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it.The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Li, X., Zhao, D. & Wang, H. Association between weight-adjusted waist index and risk of diabetes mellitus type 2 in United States adults and the predictive value of obesity indicators. BMC Public Health 24, 2025 (2024). https://doi.org/10.1186/s12889-024-19576-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-19576-6