Abstract
Introduction
Child undernutrition is a major public health problem in sub-Saharan Africa. Children who eat animal-based foods have higher intakes of various nutrients that are important for optimal linear growth. However, the prevalence of animal-source food consumption was low across many countries. Therefore, this study aimed to determine the prevalence of good consumption of animal-source foods and its determinants among children aged 6 to 23 months in sub-Saharan African countries.
Methods
A cross-sectional pooled dataset using recent demographic and health surveys from 19 sub-Saharan African countries was employed. A total weighted sample of 65,742 children aged 6 to 23 months was included in the study. Data extracted from the recent DHS data sets were cleaned, recorded, and analyzed using STATA/SE version 14.0 statistical software. Descriptive analysis was carried out to present both individual and community-level variables using frequencies and percentages. A multilevel mixed-effects logistic regression was used to determine the factors associated with the outcome variable. Finally, variables with a p-value less than 0.05 and an adjusted odds ratio with a 95% confidence interval were declared statistically significant.
Results
In this study, 43.1% (95% CI: 42.7–43.5%) of children aged 6 to 23 months consumed animal-source foods. Factors like maternal education [AOR = 1.36; 95% CI (1.28, 1.44)], maternal occupation [AOR = 1.24; 95% CI (1.18, 1.31)], exposure to media [AOR = 1.30; 95% CI (1.24, 1.36)], wealth index [AOR = 1.16; 95% CI (1.10, 1.23)] & [AOR = 1.28; 95% CI (1.21, 1.36)], owned a mobile telephone [AOR = 1.23; 95% CI (1.17, 1.29)], ANC visits [AOR = 1.20; 95% CI (1.15, 1.25)], place of delivery [AOR = 1.09; 95% CI (1.04, 1.14)], PNC checkup [AOR = 1.34; 95% CI (1.28, 1.39)], the current age of the child [AOR = 1.99; 95% CI (1.85, 2.14)], [AOR = 3.34; 95% CI (3.14, 3.56)], & [AOR = 4.3; 95% CI (4.10, 4.66)], birth interval [AOR = 0.92; 95% CI (0.87, 0.97)], residence [AOR = 1.43; 95% CI (1.35, 1.50)], community illiteracy [AOR = 0.91; 95% CI (0.86, 0.96)], and community poverty [AOR = 1.07; 95% CI (1.01, 1.14)] were significantly associated with consumption of animal-source foods.
Conclusion
Less than half of children aged 6 to 23 months consumed any type of animal-source foods in sub-Saharan African countries. Higher educational level, non-agricultural work, exposure to media, high economic status, having a mobile telephone, attending 4 + ANC visits, health facility delivery, PNC checkups, older children, a birth interval of 24 months, urban residency, community literacy, and low community poverty were determinates of good consumption of animal source foods. Women empowerment, dissemination of nutrition-related information through mass media, promotion of health facility delivery, and improving utilization of maternal health services are recommended to improve infant and child feeding practices.
Similar content being viewed by others
Introduction
Child undernutrition is a major public health problem in sub-Saharan Africa [1]. It is one of the main determinants of child mortality aged under 59 months, in which 14.7% and 14.4% of deaths are attributed to stunting and underweight, respectively [2]. More than half of preschool-aged children in the world have micronutrient deficiencies [3]. Micronutrient deficiency impairs the cognitive function of children and harms the economic growth of a nation [4].
Deficiencies in micronutrients among children lead to an increased risk of acquiring infections, visual impairment, decreased academic performance and productivity, growth retardation, and death [5, 6]. Increasing the intake of micronutrients is associated with a reduced burden of child morbidity, mortality, and neurocognitive impairment [7]. Both micronutrients and macronutrients in proper amounts and balance are essential for children to maintain optimal growth and development [8].
Children who consume animal-source foods (ASFs) have higher intakes of various nutrients important for optimal linear growth [9]. Consuming ASFs is associated with increased intakes of energy, protein, essential fatty acids, vitamin B12, vitamin D, phosphorus and selenium, protein, and zinc [10]. According to the WHO, breastfed and non-breastfed children should eat ASFs daily, or as often as possible [11, 12]. Evidence shows that children who consume ASFs are less likely to be stunted [13].
Consumption of ASFs was also positively associated with psychosocial functioning, including orientation toward success, expectations for future economic conditions, and self-perceived health [14]. However, the prevalence of ASF consumption was low across many countries [15]. In low- and middle-income countries (LMICs), ASF consumption by young children is limited, with only 49% of children aged 6 to 23 months consuming at least 1 ASF on the day before the survey [16]. Affordability, accessibility, a child’s age, perceived nutritional value, taste preferences, food prohibitions, preferential food allocation, and child feeding styles are some of the factors that influence the consumption of ASFs by young children in LMICs [17, 18].
Two studies conducted in Ethiopia using the 2016 and 2019 mini demographic and health survey (DHS) data showed that the consumption of ASFs among children aged 6–23 months ranges from 22.7 to 46.5% [19, 20]. Factors like religion, child age, number of household assets, number of livestock owned by a household, ownership of land usable for agriculture, place of delivery, wealth index, educational level of mothers, multiple-risk pregnancy, and residence were significant determinants of ASF consumption [19, 20].
Though studies demonstrated lower rates of stunting in children that consumed ASFs than children that only consumed plant-based diets [21, 22], there has not been a continent-wide analysis that determines ASF consumption status and its determinants among children aged 6 to 23 months in sub-Saharan Africa. Therefore, this study aimed to determine the prevalence of good consumption of ASFs and its determinants among children aged 6–23 months in sub-Saharan African countries using recent DHS data. The findings of this study will help with effective nutritional interventions and assist non-governmental organizations working on child health, health professionals, and health policymakers to design intervention approaches to improve the consumption of ASFs for the most susceptible group to malnutrition.
Methods and materials
Data source, study design, and sampling
A cross-sectional pooled dataset using recent DHS from 19 sub-Saharan African countries, which was conducted between 2015 and 2020, was employed. Demographic and health surveys from 19 sub-Saharan African countries, including Angola, Benin, Burundi, Cameron, Ethiopia, Gambia, Guinea, Liberia, Mali, Malawi, Nigeria, Rwanda, Serra Leone, Senegal, Tanzania, Uganda, South Africa, Zambia, and Zimbabwe, were used. These countries were selected depending on the availability of the most recent DHS dataset and outcome variable. The data were appended to figure out the prevalence of good consumption of ASFs and its determinants among children aged 6–23 months in sub-Saharan African countries. Different datasets, including those for children, males, women, births, and households, are included in the survey for each country. The current study used the kid’s record (KR) file. The DHS is a nationwide survey, mostly collected every five years across LMICs. It makes cross-country comparison possible as it uses standard procedures for sampling, questionnaires, data collection, cleaning, coding, and analysis [23].
A total weighted sample of 65,742 children aged 6 to 23 months was included in the study (Table 1). The DHS employs a stratified, two-stage sampling technique [24]. The first stage involves the development of a sampling frame, consisting of a list of primary sampling units (PSUs) or enumeration areas (EAs), which covers the entire country and is usually developed from the latest available national census. The second stage is the systematic sampling of households listed in each cluster, or EA. Further information on the survey sampling strategies is available in the DHS guideline [25].
Study variables
Outcome variable
ASF consumption (“1”: consumed ASFs, “0”: do not consume ASFs).
ASF consumption is defined as a percentage of children 6–23 months of age who consumed food groups 5 (flesh foods) and 6 (eggs) described in indicators of minimum dietary diversity during the previous day [26]. If either food group has been consumed, children are counted as “consumed ASF,” otherwise they are counted as “not consumed ASF” [27].
Independent variables
Both individual and community-level variables were considered.
Individual-level variables
Child-related factors (age of the child (6–8 months, 9–11 months, 12–17 months, 18–23 months), sex of child (male, female), preceding birth interval (< 24 months, >=24 months)); socioeconomic factors (maternal age (15–24 years, 25 - -34 years, 35–49 years), maternal education (no education, primary, secondary and above), current marital status of the mother (married, unmarried), maternal occupation (not working, agricultural works, and nonagricultural works), exposure to media (yes, no), wealth index (poor, middle, rich), owns a mobile telephone (yes, no)); health service related factors: place of delivery (home, health facility), attended 4 + ANC visits (yes, no), PNC checkup (yes, no).
Community-level variables
Place of residence (urban, rural), community poverty level (low, high), community illiteracy (low, high), community media exposure (low, high).
Data management and analysis
Data extracted from the recent DHS data sets were cleaned, recoded, and analyzed using STATA/SE version 14.0 statistical software. Sample weight was employed to manage sampling errors and non-responses. Continuous variables were categorized, and categorical variables were further re-categorized. Descriptive analysis was carried out to present the data in frequencies and percentages. Both the individual and community-level variables were presented using descriptive statistics. The DHS data’s variables were organized in clusters; 65,742 children are nested within households, and households were nested within 1400 clusters. Due to clustering, the traditional logistic regression model could not be used because of non-independent observations and unequal variance across clusters. This is an indication that using a sophisticated model to take into account between-cluster factors is necessary. As a result, multilevel mixed-effects logistic regression was used to determine the factors associated with ASF consumption. Multilevel mixed effect logistic regression follows four models: the null model (outcome variable only), model I (only individual-level variables), model II (only community-level variables), and model III (both individual and community-level variables). The model without independent variables (the null model) was used to check the variability of ASF consumption across the cluster. The association of individual-level variables with the outcome variable (Model I) and the association of community-level variables with the outcome variable (Model II) were assessed. In the final model (Model III), the association of both individual and community-level variables was fitted simultaneously with the outcome variable (ASF consumption).
The magnitude of the clustering effect and the degree to which community-level factors explain the unexplained variance of the null model were quantified by checking the intra-class correlation coefficient (ICC) and proportional change in variance (PCV). A model with the lowest deviance was selected as the best-fitted model. As indicated in Table 2, the deviance for models I, II, and III was 59,185.638, 87,790.142, and 58,957.696, respectively. Hence, model III was considered the best-fitted model. Finally, variables with a p-value less than 0.05 and an adjusted odds ratio (AOR) with a 95% confidence interval (CI) were described as statistically significant variables associated with consumption ASFs. The presence of multi-collinearity between covariates was checked by using a variance inflation factor (VIF) falling within acceptable limits of 1–10 with a mean VIF of 1.43, indicating the absence of significant collinearity across independent variables (supplementary file 1).
Random effects
Random effects or measures of variation of the outcome variable were estimated using the median odds ratio (MOR), ICC, and PCV. The variation between clusters was measured by the ICC and PCV. Taking clusters as a random variable, the ICC reveals the variation of animal source food consumption between clusters is computed as: ICC = VC/(VC + 3.29)×100%. The MOR is the median value of the odds ratio between the area of the highest risk and the area of the lowest risk for animal source food consumption when two clusters are randomly selected, using clusters as a random variable; MOR = 𝑒0.95√VC. In addition, the PCV demonstrates the variation in the prevalence of animal source food consumption explained by factors and computed as: PCV = (Vnull-VC)/Vnull×100%, where Vnull = variance of the null model and VC = cluster level variance [28]. The association between the likelihood of animal-source food consumption and individual and community-level independent variables was estimated by the fixed effects.
Results
Individual- and community-level characteristics of study subjects
A total of 65,742 children aged 6 to 23 months were included in this study. The mean age of mothers was 27.92 ± 0.03 years, and 45.51% of them fall in the age range of 25–34 years. More than one-third (34.60%) of the mothers completed primary education, and 70.25% of them were currently married. Nearly 38% of mothers had non-agricultural work, and 63.13% of them had exposure to the media. More than half (54.83%) of mothers in SSA owned a mobile telephone, and 46.85% of them had poor socioeconomic status. Home delivery was reported by 28.29% of mothers in SSA countries, and only 36.73% of them had PNC checkups. More than half (58.39%) of mothers attended 4 + ANC visits during pregnancy. The mean age of children was 14.26 ± 0.02 months, and 35% of them fall in the age range of 12–17 months. More than half (51%) of the children were male, and the preceding birth interval was ≥ 24 months for the majority (84%) of children aged 6–23 months. Only 31% of the study subjects were from urban areas, and 51% had low media exposure. More than half (53%) and (51%) of mothers of children aged 6 to 23 months had low community poverty and community illiteracy, respectively (Table 3).
Animal source food consumption
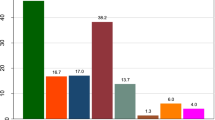
In the current study, 43.1% (95% CI: 42.7–43.5%) of children aged 6 to 23 months consumed ASFs (either flesh foods or eggs) during the day preceding the interview (Fig. 1). About 14.5% and 37.8% of children aged 6 to 23 months in SSA countries consumed eggs and flesh foods, respectively (Fig. 2). The result showed that consumption of ASFs improves with increasing household wealth status, with the proportion of children who consumed ASFs being lowest among children from poor household families (35.23%) and highest among rich household families (53.70%) (Fig. 3).
Random effects (measures of variation) and model fitness
A null model was used to determine whether the data supported the decision to assess randomness at the community level. Findings from the null model showed that there were significant differences in ASF consumption between communities, with a variance of 0.0925833 and a P value of < 0.001. The variance within clusters contributed 72.63% of the variation in ASF consumption, while the variance across clusters was responsible for 27.37% of the variation. In the null model, the odds of ASF consumption differed between higher and lower-risk clusters by a factor of 1.34 times. The intra-class correlation value for Model I indicated that 19.55% of the variation in ASF consumption accounts for the disparities between communities. Then, with the null model, we used community-level variables to generate Model II. According to the ICC value from Model II, cluster variations were the basis for 25.39% of the differences in ASF consumption. In the final model (model III), which attributed approximately 21% of the variation in the likelihood of ASF consumption to both individual and community-level variables, the likelihood of ASF consumption varied by 1.29 times across low and high ASF consumption (Table 2).
Individual and community-level factors associated with ASF consumption
In the final fitted model (model III) of multivariable multilevel logistic regression, maternal educational level, maternal occupation, exposure to media, wealth index, ownership of a mobile telephone, ANC visits attended during pregnancy, place of delivery, PNC checkup, the current age of the child, preceding birth interval, residence, community illiteracy, and community poverty were significantly associated with consumption of ASFs among children aged 6–23 months.
The odds of ASF consumption were 1.36 times higher among mothers who completed secondary and higher education compared with mothers who had no formal education [AOR = 1.36; 95% CI (1.28, 1.44)]. Children of mothers with non-agricultural jobs were 1.24 times more likely to have good consumption of ASF than those who were not working [AOR = 1.24; 95% CI (1.18, 1.31)]. Similarly, children of mothers who had exposure to media were 1.30 times more likely to have good consumption of ASF compared with their counterparts [AOR = 1.30; 95% CI (1.24, 1.36)]. The odds of ASF consumption were 1.16 and 1.28 times higher among mothers with middle and rich economic status compared with those with poor economic status, respectively [AOR = 1.16; 95% CI (1.10, 1.23)] and [AOR = 1.28; 95% CI (1.21, 1.36)].
Children of mothers who owned a mobile telephone were 1.23 times more likely to have good consumption of ASF compared with their counterparts [AOR = 1.23; 95% CI (1.17, 1.29)]. Place of delivery was also a determinant of ASF consumption, in which mothers who delivered at a health facility were 1.09 times more likely to give their child ASF compared with mothers who delivered at home [AOR = 1.09; 95% CI (1.04, 1.14)]. Mothers who attended 4 + ANC visits during recent pregnancy were 1.20 times more likely to give their child ASF compared with mothers who didn’t [AOR = 1.20; 95% CI (1.15, 1.25)]. The odds of ASF consumption were 1.34 times higher among mothers who had PNC checkups than mothers who hadn’t [AOR = 1.34; 95% CI (1.28, 1.39)].
The age of the child was another factor significantly associated with ASF consumption. Children aged 9–11, 12–17, and 18–23 months were 1.99, 3.34, and 4.37 times more likely to have good consumption of ASF compared with children aged 6–8 months, respectively [AOR = 1.99; 95% CI (1.85, 2.14)], [AOR = 3.34; 95% CI (3.14, 3.56)], and [AOR = 4.3; 95% CI (4.10, 4.66)]. Children with a preceding birth interval of < 24 months were 8% times less likely to have good consumption of ASF compared with children with a birth interval of ≥ 24 months [AOR = 0.92; 95% CI (0.87, 0.97)]. Mothers from urban areas were 1.43 times more likely to give their children ASF compared with mothers from rural areas [AOR = 1.43; 95% CI (1.35, 1.50)]. Children from low community poverty were 1.07 times more likely to have good consumption of ASF compared with children from high community poverty [AOR = 1.07; 95% CI (1.01, 1.14)]. Children from high community illiteracy were 9% less likely to have good consumption of ASF compared with children from low community illiteracy [AOR = 0.91; 95% CI (0.86, 0.96)] (Table 4).
Discussion
Animal-source food consumption is positively associated with adequate protein and micronutrient intakes, including vitamin A, calcium, and zinc, which are important for child growth and development [29]. This study was conducted to determine ASF consumption and its determinants among children aged 6 to 23 months in sub-Saharan African countries using the most recent DHS data.
In the present study, the consumption of ASFs among children aged 6 to 23 months in sub-Saharan African countries was 43.1% (95% CI: 42.7–43.5%). This finding was higher than a study conducted in Ethiopia using pooled data from the 2016/19 Ethiopia Demographic and Health Surveys (22.7%) [20]. This difference might be explained by variations in study settings, in which the previous study was conducted only in a single country, while the current study uses data from 19 SSA countries. Sociocultural differences between Ethiopia and other SSA countries might also be the reason for the lower consumption of ASFs in the previous study. On the other hand, the findings of this study were lower than those of studies conducted in Ethiopia (46.5%, 50.9%) [18, 19] and Timor-Leste (52.8%) [30]. The possible justification for this difference might be differences in sample size and the criteria used to measure the outcome variable. The large sample size used in the current study might underestimate the proportion of children who consumed ASFs. Dairy consumption was not considered in this study to define ASF consumption.
Only 14.52% (95% CI: 14.25%, 14.79%) of children aged 6 to 23 months consumed eggs during the previous day of the interview. This finding was lower than studies conducted in Ethiopia (17.0%, 27.4%, and 17.5%) [18,19,20] and Timor-Leste (22.5%) [30]. This might be due to the use of pooled data from different countries in the current study, unlike the previous studies, which were conducted in a single area with the same socioeconomic and sociocultural factors. The current study also reported that flesh foods were consumed by 37.77% (95% CI: 37.40%, 38.14%) of the study subjects. This finding was higher than studies conducted in Ethiopia (8.7%) [20] and Timor-Leste (24.3%) [30]. This difference could be due to the difference in study period, as the current study uses the 2021 WHO indicators for infant and young children’s feeding practices.
This study also identified different factors significantly associated with the consumption of ASFs. The odds of ASF consumption were higher among mothers who completed secondary and higher education compared with mothers who had no formal education. This finding was consistent with a study conducted in Ethiopia [20]. This might be because mothers with higher educational status have a better understanding of nutrition-related education than mothers who have no formal education. In addition, educated mothers might have a better chance of exposure to information about the importance of giving ASFs to their children through mass media and might read leaflets, magazines, and books. Children of mothers with non-agricultural jobs were more likely to have good consumption of ASFs than those who were not working. Evidence supported this finding in that maternal employment was associated with improved diet quality and meal frequency among children across 50 LMICs [31].
Children of mothers who had exposure to media were more likely to have good consumption of ASFs compared with their counterparts. This finding is in agreement with studies conducted in Ethiopia [20]. This might be due to the significant role of media in raising attentiveness and affecting mothers’ infant and young children’s feeding practices. Mothers who had media exposure (listening to radio, watching television, and reading magazines) were also more likely to be exposed to infant and young children’s feeding education provided through those media. The odds of ASF consumption were higher among mothers with middle and rich economic status compared with those with poor economic status. A similar finding was reported by studies conducted in Ethiopia [20, 32] and Indonesia [33]. This could be attributed to the high price of ASFs and considering their consumption as a luxury. Mothers with low economic status might also sell livestock and their products to generate income to cover school, food, and other expenses rather than giving ASFs to their children.
Similarly, children of mothers who owned a mobile telephone were more likely to have good consumption of ASFs compared with their counterparts. This might be due to the fact that mothers may obtain nutrition education from health professionals, including dietary diversity and appointment reminders through text messaging. Mobile phone short message service is effective in improving knowledge of appropriate infant feeding practices for mothers [34]. Mothers who delivered at a health facility, who attended 4 + ANC visits during their recent pregnancy, and who had PNC checkups were more likely to give their child ASFs compared with their counterparts. This finding was supported by studies conducted in Ethiopia [20] and Indonesia [33]. Mothers who deliver in health facilities can get direct counseling from health professionals about appropriate child-feeding practices. In addition, mothers who have attended 4 + ANC visits may be more informed, have greater access to services, and thus be more likely to be able to provide animal-sourced foods to their children. The advice provided to mothers during post-natal checkups could also contribute to increased consumption of ASFs. This implies that improving access and utilization of maternal health services and promoting health facility delivery should be stressed to achieve optimal feeding practices for infants and young children.
From child-related factors, the age of the child and birth interval were significantly associated with ASF consumption. The odds of ASF consumption were higher among children in higher age groups. Similar findings were reported by studies conducted in Ethiopia [18,19,20]. This could be attributed to social norms and beliefs. Respondents to a qualitative study reported that avoiding meat for children aged below two years is common in their localities, and children have no teeth to chew meat [32]. The other possible justification could be a lack of nutrition-related knowledge and food taboos about ASF consumption in children aged 6 to 23 months. Interventions are needed to improve the mothers’ nutritional knowledge and bring about behavioral change to improve infant and young children’s feeding practices. Children with a preceding birth interval of < 24 months were less likely to have good consumption of ASFs. This might be due to the short birth interval; birth might cause sharing problems among living children, and parents can’t feed their children a variety of foods, including ASFs.
Community-level variables like residence, community poverty, and community illiteracy were also determinants of ASF consumption. Mothers from urban areas were more likely to give their children ASFs compared with mothers from rural areas. A similar finding was reported by a previous study [20]. The possible reason could be that mothers who live in urban areas might have better access to health care services where they can take advantage of appropriate counseling about child feeding practices. Mothers residing in urban areas might also have higher exposure to and access to health services and nutrition-related information through various media than in rural areas. Children from low-community poverty were more likely to have good consumption of ASFs compared with children from high-community poverty. This finding was in agreement with a study conducted in Ethiopia [20]. This might be due to household food insecurity, as community poverty is the composite effect of individual economic status, which impacts nutrition by limiting the amount and quality of food consumed by all the members of a household. Furthermore, children with high community illiteracy were less likely to have good consumption of ASFs. This could be associated with an educated community that might have proper resource management, better health-promoting activities, and better children’s feeding practices. Hence, improving the literacy of the community and increasing awareness about optimal infant and young child feeding practices will help to improve children’s consumption of ASFs.
The main strength of this study was the use of a multilevel mixed-effects model that resolved the problem of the hierarchical nature of the DHS data. Next, the revised WHO indicators were used to determine the prevalence of good consumption of ASFs in sub-Saharan Africa. The study also used the most recent ((2015–2020) DHS and region-wide survey data to help the concerned authorities in this region set appropriate strategies towards optimal infant and child feeding practices. Finally, the study uses a larger sample size, which is important to maintain the internal validity of the study as it provides precise findings and makes generalizability possible.
This study also has some limitations. First, as the consumption of animal-source foods was measured based on mothers’ self-report, there might be an introduction of recall and social desirability bias. In addition, the study did not provide information on the quantity and frequency of ASF consumption due to the secondary nature of the data.
Conclusion
Less than half of children aged 6 to 23 months consumed any type of ASF in sub-Saharan African countries. Higher educational level, non-agricultural work, exposure to media, high economic status, having a mobile telephone, attending 4 + ANC visits, health facility delivery, PNC checkups, older children, a birth interval of 24 months, urban residency, community literacy, and low community poverty were determinates of good consumption of ASFs. Women empowerment, dissemination of nutrition-related information through mass media, promoting health facility delivery, improving utilization of maternal health services, and behavioral change communication are recommended to improve infant and child feeding practices. Further research using primary data is needed to determine the quantity and frequency of ASF consumption and focus on interventions to improve the feeding practices of mothers of children in sub-Saharan Africa. Health policymakers can use this information to design intervention approaches to improve the consumption of animal-source foods for the most susceptible group to malnutrition by investing in policy execution and appraisal as well as engaging with stakeholders in child health.
Data availability
The most recent data from the Demographic and Health Survey is publicly available online at https://www.dhsprogram.com.
Abbreviations
- ANC:
-
Antenatal Care
- AOR:
-
Adjusted Odds Ratio
- ASFs:
-
Animal Source Foods
- CI:
-
Confidence Interval
- DHS:
-
Demographic and Health Survey
- ICC:
-
Intra-class Correlation Coefficient
- LMICs:
-
Low- and middle-income countries
- MOR:
-
Median Odds Ratio
- PCV:
-
Proportional Change in Variance
- PNC:
-
Postnatal Care
- SSA:
-
Sub-Saharan Africa
- VIF:
-
Variance Inflation Factor
- WHO:
-
World Health Organization
References
Ricci C, Asare H, Carboo J, Conradie C, Dolman RC, Lombard M. Determinants of undernutrition prevalence in children aged 0–59 months in sub-saharan Africa between 2000 and 2015. A report from the World Bank database. Public Health Nutr. 2019;22(9):1597–605.
Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, De Onis M, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet. 2013;382(9890):427–51.
Stevens GA, Beal T, Mbuya MN, Luo H, Neufeld LM, Addo OY, et al. Micronutrient deficiencies among preschool-aged children and women of reproductive age worldwide: a pooled analysis of individual-level data from population-representative surveys. Lancet Global Health. 2022;10(11):e1590–9.
Githanga D, Awiti A, Were F, Ngwiri T, Nyarko M, Shellack N. A consensus on malnutrition in Africa: a report from the micronutrient deficiency awareness forum (Nairobi 2017). Afr J Food Agric Nutr Dev. 2019;19(2):14277–90.
Petry N, Olofin I, Hurrell RF, Boy E, Wirth JP, Moursi M, et al. The proportion of anemia associated with iron deficiency in low, medium, and high human development index countries: a systematic analysis of national surveys. Nutrients. 2016;8(11):693.
Roth DE, Abrams SA, Aloia J, Bergeron G, Bourassa MW, Brown KH, et al. Global prevalence and disease burden of vitamin D deficiency: a roadmap for action in low-and middle‐income countries. Wiley Online Library; 2018. pp. 0077–8923. Report No.
Keats EC, Das JK, Salam RA, Lassi ZS, Imdad A, Black RE, et al. Effective interventions to address maternal and child malnutrition: an update of the evidence. Lancet Child Adolesc Health. 2021;5(5):367–84.
Savarino G, Corsello A, Corsello G. Macronutrient balance and micronutrient amounts through growth and development. Ital J Pediatr. 2021;47(1):1–14.
Papanikolaou Y, Fulgoni VL III. Egg consumption in infants is associated with longer recumbent length and greater intake of several nutrients essential in growth and development. Nutrients. 2018;10(6):719.
Tang M, Krebs NF. High protein intake from meat as complementary food increases growth but not adiposity in breastfed infants: a randomized trial. Am J Clin Nutr. 2014;100(5):1322–8.
WHO. Guiding principles for complementary feeding of the breastfed child, 2003.
WHO. Guiding principles for feeding non-breastfed children 6–24 months of age. World Health Organization; 2005.
Umwali N, Kunyanga CN, Kaindi DWM. Determinants of stunting in children aged between 6–23 months in Musanze region, Rwanda. Front Nutr. 2022;9:1044350.
Masa R, Chowa G. Correlates of animal source food consumption and its association with psychosocial functioning of adults in rural Western Uganda. Food Secur. 2019;11(3):665–77.
White JM, Bégin F, Kumapley R, Murray C, Krasevec J. Complementary feeding practices: current global and regional estimates. Matern Child Nutr. 2017;13:e12505.
Headey D, Hirvonen K, Hoddinott J. Animal sourced foods and child stunting. Wiley Online Library; 2018.
Cornelsen L, Alarcon P, Häsler B, Amendah DD, Ferguson E, Fèvre EM, et al. A cross-sectional study of drivers of animal-source food consumption in low-income urban areas of Nairobi, Kenya. BMC Nutr. 2016;2:1–13.
Potts KS, Mulugeta A, Bazzano AN. Animal source food consumption in young children from four regions of Ethiopia: Association with religion, livelihood, and participation in the productive safety net program. Nutrients. 2019;11(2):354.
Gebretsadik GG, Adhanu AK, Mulugeta A. Magnitude and determinants of animal source food consumption among children aged 6–23 months in Ethiopia: secondary analysis of the 2016 Ethiopian demographic and health survey. BMC Public Health. 2022;22(1):453.
Hamza HA, Oumer A, Kabthymer RH, Ali Y, Ahmed Mohammed A, Shaka MF, et al. Individual and community-level factors associated with animal source food consumption among children aged 6–23 months in Ethiopia: multilevel mixed effects logistic regression model. PLoS ONE. 2022;17(4):e0265899.
Darapheak C, Takano T, Kizuki M, Nakamura K, Seino K. Consumption of animal source foods and dietary diversity reduce stunting in children in Cambodia. Int Archives Med. 2013;6(1):1–11.
Dror DK, Allen LH. The importance of milk and other animal-source foods for children in low-income countries. FoodNutr Bull. 2011;32(3):227–43.
Corsi DJ, Neuman M, Finlay JE, Subramanian S. Demographic and health surveys: a profile. Int J Epidemiol. 2012;41(6):1602–13.
Aliaga A, Ruilin R, editors. Cluster optimal sample size for demographic and health surveys. 7th International Conference on Teaching Statistics–ICOTS; 2006.
Croft T, Marshall AM, Allen CK, Arnold F, Assaf S, Balian S, et al. Guide to DHS statistics: DHS-7 (version 2). Rockville, MD: ICF; 2020.
WHO. Indicators for assessing infant and young child feeding practices: definitions and measurement methods. 2021.
Heidkamp RA, Kang Y, Chimanya K, Garg A, Matji J, Nyawo M, et al. Implications of updating the minimum dietary diversity for children indicator for tracking progress in the eastern and southern Africa region. Curr Developments Nutr. 2020;4(9):nzaa141.
Sommet N, Morselli D. Keep calm and learn multilevel logistic modeling: a simplified three-step procedure using Stata, R, mplus, and SPSS. Int Rev Social Psychol. 2017;30:203–18.
Muslimatun S, Wiradnyani LAA. Dietary diversity, animal source food consumption and linear growth among children aged 1–5 years in Bandung, Indonesia: a longitudinal observational study. Br J Nutr. 2016;116(S1):S27–35.
Wong JT, Bagnol B, Grieve H, da Costa Jong JB, Li M, Alders RG. Factors influencing animal-source food consumption in Timor-Leste. Food Secur. 2018;10:741–62.
Oddo VM, Ickes SB. Maternal employment in low-and middle-income countries is associated with improved infant and young child feeding. Am J Clin Nutr. 2018;107(3):335–44.
Haileselassie M, Redae G, Berhe G, Henry CJ, Nickerson MT, Tyler B, et al. Why are animal source foods rarely consumed by 6–23 months old children in rural communities of Northern Ethiopia? A qualitative study. PLoS ONE. 2020;15(1):e0225707.
Sebayang SK, Dibley MJ, Astutik E, Efendi F, Kelly PJ, Li M. Determinants of age-appropriate breastfeeding, dietary diversity, and consumption of animal source foods among Indonesian children. Matern Child Nutr. 2020;16(1):e12889.
Jiang H, Li M, Wen LM, Hu Q, Yang D, He G, et al. Effect of short message service on infant feeding practice: findings from a community-based study in Shanghai, China. JAMA Pediatr. 2014;168(5):471–8.
Acknowledgements
I am grateful to the DHS program for letting me use the relevant DHS data in this study.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
Activities like designing the study, data extraction, data analysis, interpretation, reporting, and manuscript writing were done by E.G.M.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval and consent to participate
Permission was granted to download and use the data from http://www.dhs.program.com before conducting the study. Ethical clearance was obtained from the Institution Review Board of the DHS Program, ICF International. The procedures for DHS public-use data sets were approved by the Institution Review Board. Identifiers for respondents, households, or sample communities were not allowed in any way, and the names of individuals or household addresses were not included in the data files. The number for each EA in the data file does not have labels to show their names or locations. There were no patients or members of the public involved since this study used a publicly available data set.
Consent for publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it.The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Mekonen, E.G. Animal source food consumption and its determinants among children aged 6 to 23 months in sub-Saharan African countries: a multilevel analysis of demographic and health survey. BMC Public Health 24, 2060 (2024). https://doi.org/10.1186/s12889-024-19628-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-19628-x