Abstract
Background
There are many factors effective on occurrence of post-partum anxiety and depression. COVID-19 pandemic, as a major health crisis, affected many countries and had undesirable mental health outcomes, especially for the vulnerable population. The aim of this study was to evaluate the prevalence of post-partum anxiety and depression and their related factors during COVID-19 pandemic.
Methods
The present descriptive cross-sectional study was conducted on 360 mothers who delivered their child during COVID-19 pandemic and had referred to the comprehensive urban health canter of Lenjan city two months after their delivery (from November 10th, 2021, until March 19th, 2022). Data were gathered using 3 questionnaires including demographic characteristics, Edinburgh Postnatal Depression Scale (EPDS), and Beck Anxiety Inventory (BAI). Data were analyzed using SPSS software version 24 and the level of significance was set at p < 0.05.
Results
The prevalence of anxiety and post-partum depression was 27% and 20%, respectively. None of the demographic characteristics had a significant relationship with anxiety and depression. Related factors to post-partum anxiety included desired pregnancy, premenstrual syndrome, marital conflicts, history of mother’s hospitalization due to COVID-19, compliance rate with preventive health measures for COVID-19, stressful events, and social support.
Conclusion
It is suggested to screen mothers to detect significant related factors of post-partum anxiety and depression in other future pandemics or epidemics to support them.
Similar content being viewed by others
Introduction
Post-partum blues is common among mothers and if it lasts more than 10 days, it would be called post-partum depression. Post-partum depression is a common but treatable problem with widespread effects on mothers and their families which is associated with feeling of sadness, inability to have pleasure, irritability, anger, and decreased self-confidence. Symptoms of this disorder are mood swings, changes in appetite, fear of getting hurt, serious concerns about the baby, extreme sorrow and crying, hesitation, concentration problem, becoming uninterested in daily activities, sleep disorder and death and suicidal thoughts [1]. This disorder would also lead to decrease the level of healthy relationship and attachment between mother and the infant, infant’s growth disorder, decreased level of mother’s health, permanent depression of mother and marital conflicts [2]. The risk of depression relapse following delivery has been reported as 40% [3]. The prevalence of this disabling disorder in the world has been reported from 5 to 60.8% [1]. According to the results of previous studies, the prevalence of post-partum depression varies in the world, in a way that, up to 2017, it was about 9.5% in high-income countries, 20.8% in average-income countries, and 25.8% in low-income countries [4, 5]. In 2020, in Asian countries, the prevalence of post-partum depression was reported from 7 to 33% [6]. Considering its high prevalence and harmful outcomes, post-partum depression has been recognized as one of the most severe global health problems during the past decade [3].
Evidence has shown that, following extensive prevalence of infectious diseases, psychological disorders would also appear. Psychological reactions to pandemics include inconsistent behaviors, emotional distress and defensive responses such as anxiety, fear, disappointment, anger, boredom, depression, stress, and avoidance behaviors [7]. COVID-19 pandemic was also a major health crisis; therefore, it could be expected that it would be associated with undesirable psychological outcomes especially in the vulnerable groups such as pregnant women [8]. The review articles by Usmani (2021) in Turkey showed that the prevalence of post-partum depression during COVID-19 pandemic was from 7 to 80.8% [9]. Also, in Romania, during the COVID-19 pandemic in 2020, this prevalence was 18.8% [10].
Anxiety is also an undesirable and vague feeling which usually appears in the form of concern and is defined as a sense of hesitation towards an unknown factor. This undesirable feeling could be associated with many physiologic, emotional and mental symptoms and be expressed in the form of a severe emotional feeling. Post-partum anxiety and anxiety disorders are common among women [1, 11]. According to a review article by Rujcumar (2020) in India, the prevalence of anxiety and depression among general population was 16–28% during COVID-19 pandemic, and were among the most common psychological problems [12].
Studies have that various factors have been related to anxiety and post-partum depression. For example, based on the systematic review by Usmani (2021), the risk factors for post-partum depression during COVID-19 pandemic were divided into 6 categories: social-demographic, psychological, previously existed psychological disorders, metabolic factors, abortion, and incorrect information from media [9]. Study by Xiong (2020) on post-partum mothers in China showed that the probability of anxiety and depression among mothers who were students, had background diseases, and had poor health conditions, was higher [13]. Gurudatt (2014) in their study reported higher prevalence of depression among working mothers during the first months following delivery in comparison to non-working mothers [14]. Probably, there were some other effective factors during COVID-19 pandemic.
Aim and objectives
Since, very few studies have been conducted in Iran about the prevalence of and related factors to anxiety and post-partum depression during COVID-19 pandemic and the effect of these disorders on the health of mothers and infants, such studies could lead to development of beneficial interventions during future pandemics/epidemies. Therefore, this study was conducted to evaluate the prevalence of and related factors to post-partum anxiety and depression during COVID-19 pandemic in Lenjan city of Isfahan Province, Iran in 2021.
Methods
Study design
This study was a descriptive cross-sectional study conducted on all mothers who had delivered during COVID-19 pandemic in 2021 and had referred to the comprehensive urban health center of Lenjan two months after delivery for the vaccination of their infants. Sampling was conducted from November 10th 2021 until March 19th 2022. This study was conducted after the start of vaccination of pregnant women (August 12th 2021) against COVID-19 in Iran.
Study sample
Since the number of births during 2020 in Lenjan was 3020 infants, the number of participants was calculated to be 360 individuals; using the following formula with a 30% expected prevalence and 5% error probability:
Study recruitment
Inclusion criteria |
mother’s willingness to participate in the study |
having Iranian nationality |
having no history of mental diseases |
no consumption of antidepressant and antianxiety drugs according to mother’s statements and information from SIB website |
having no history of drug addiction |
no abnormalities in the last infant |
having no history of infertility related to the last pregnancy |
Exclusion criteria |
not responding to more than 5% of the questions |
Data collection
In this study, the mothers were selected using random cluster multistage sampling method from comprehensive urban health centers of Lenjan city, Iran. It must be noted that there are 12 comprehensive health centers, 11 health bases, 21 health houses and 22 dependent villages in Lenjan city. From all the health houses and dependent villages which were 43 centers, 10 were randomly selected and from each health house, 4 to 5 participants were randomly selected and completed the questionnaires. Also, from a total of 23 health center and health base, 14 were randomly selected and from each, 16–28 mothers completed the questionnaires, based on the number of mothers who had delivered their infants there. So, mothers who have given birth and had two-month-old infants were enrolled in the study. For this matter, name of the mothers who had two-month-old infants or their infants would become two-month-old in the future was listed and a number was assigned to each of them. By dividing the number of mothers by the number of needed samples, the space between the samples was calculated. Then, by selecting a number from the calculated space from the list of the names and adding it to the calculated space between the samples, the number of the mothers who were intended for the study was achieved. When their infants reached the age of two months, mothers were invited for completing the questionnaires.
Instruments
Data were gathered using 4 questionnaires that were completed by the mothers in the presence of the researcher.
Demographic questionnaire
Demographic questionnaire included 7 items: age, education level, occupation, parity, husband’s education level, family income, and husband’s occupation.
Questionnaires of dependent variables (depression and anxiety)
Edinburgh Postnatal Depression Scale (EPDS) was applied to assess mothers’ depression. It has been used in various studies and its validity and reliability have been approved. This scale contains 10 multiple-choice questions which are scored from 0 to 3 based on a 4-point Likert scale, with a total number of 0 to 30. Higher total scores indicate higher level of depression and the threshold for depression is the score of 10. Scores of 10 to 16 indicate mild depression, 17 to 23 indicate moderate depression and 24 to 30 indicate severe depression [13, 15, 16]. Cronbach’s α for Edinburgh Scale was calculated through a validation study in Iran to be more than 0.7 and its reliability along with Beck Scale was 0.44 [17].
Beck Anxiety Inventory (BAI) was applied to assess mothers’ anxiety. It evaluates specifically the severity of symptoms of clinical anxiety in patients with 21 questions scored from 0 to 3 based on a 4-point Likert scale. The total score ranges from 0 to 63. The threshold for anxiety is the score of 8. Scores from 0 to 7 indicate no or low anxiety, scores from 8 to 15 indicate mild anxiety, scores from 16 to 25 indicate moderate anxiety and scores from 26 to 63 indicate severe anxiety [18]. Its Cronbach’s α was calculated to be 0.87 to 0.92, its validity was calculated as 0.75 using test-retest method after one week and the correlation of its items varied from 0.30 to 0.76. In present study, the data analyzer hade to concatenate the levels of depression and anxiety and reported tables included two rows (yes or no). In the rows related to anxiety and depression, “Yes” means that participant has mild, moderate, or sever status.
The questionnaire of independent variables
The questionnaire of independent variables included 12 variables nonrelated to COVID-19 pandemic (Table 1) and 12 variables related to COVID-19 pandemic (Tables 2 and 3). Out of first 12 variables, social support and stressful events of life were assessed by previously developed questionnaires. Social support questionnaire developed by Phillips et al. consists of 43 items scored from 1 to 4 (completely disagree- completely disagree) based on a 4-point Likert. The items of 3, 10, 13, 21, and 22 score reversely. Higher scores show more social support. Its reliability was confirmed in a study in Iran (Cronbach’s α 0.74) [19]. Also, stressful events of life were assessed by questionnaire of stressful events developed by Thomas Holms and Richard Rahe in 1976. This questionnaire includes 43 items scored from 1 to 4 (very mild- sever) based on a 4-point Likert. The scores 0-149, 150–199, 200–299, and 300 or more indicate very mild, mild, moderate, and sever stress respectively. It has a satisfying reliability (Cronbach’s α 0.79) as well as face and content validity. In Iran, its reliability was confirmed by calculating Cronbach’s α (0.72) and split – half method (0.64) in a study [20].
The variables related to COVID-19 pandemic (n = 12) were achieved based on review of literature and the opinions of academic members of midwifery and obstetrics/gynecology including: history of mother’s definite infection with COVID-19 based on PCR test, history of definite infection with COVID-19 among close relatives of mothers based on PCR test, history of mother’s hospitalization due to COVID-19, history of hospitalization due to COVID-19 among mother’s family members and intimate friends/relatives, history of mortality due to COVID-19 among mother’s family members and intimate friends/relatives, history of mortality due to COVID-19 among mother’s non-intimate friends and relatives, following COVID-19 news by the mother, compliance with preventive health measures for COVID-19, being in contact with someone without compliance with preventive health measures COVID-19, vaccination of mother’s family members and intimate friends/ relatives with close contacts, mother’s vaccination against Covid-19, and the reason for mother’s lack of vaccination against Covid-19. One of above mentioned variables was “compliance rate with preventive health measures for COVID-19 by participants”. To assess this variable, a 16-item questionnaire was developed by the research team and its validity was assessed through calculating the Content Validity Ratio and Content Validity Index based on the opinions of 10 faculty members of Health and Nursing/Midwifery Faculties of the university. After modifications, the 14-item questionnaire was achieved with satisfactory Cronbach’s alpha (0.87) (Table 4). The questions score from 1 to 4 based on a 4-point Likert scale, with a total number of 14 to 56. Higher total scores indicate higher compliance rate and 14–34 indicates “yes” and 35–56 indicates “no” compliance.
Statistical analyses
Data analysis was conducted using descriptive statistics (mean and standard deviation) and chi square test. P values less than 0.05 were considered statistically significant and data analysis was conducted by SPSS software version 24. In this study, the data analyzer hade to concatenate the levels and reported tables included two rows (yes or no) because the numbers in some rows were less than 6.
Results
Demographic characteristics
The mean age of the participants was 31.05 ± 5.37 years (16–43 years). Most of them had diploma (45%) and were housewife (89.41%), and multiparous (60.83%). Most of the husbands were self-employed (37.67%). Most of them had a moderate family’s income (51.5%).
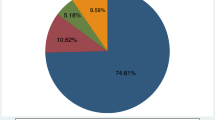
Results of this study showed that most of the mothers did not have post-partum anxiety (73%) and distribution of anxiety severity was as follows: 18.7% of mothers had mild anxiety, 4.5% had moderate anxiety, and 3.9% severe anxiety (27% in total). The mean score of mothers’ anxiety was at the no anxiety level (5.60 ± 7.8). Also, results indicated that most of the mothers did not have depression (80%) and distribution of depression was as follows: 15.30% had mild depression, 3.60% hah moderate depression and 1.10% had severe depression (20% in total). The mean score of mothers’ depression was at the no depression level (5.34 ± 5.38).
Also, results showed that post-partum anxiety in mothers had no significant relationship with demographic variables including age, educational level, occupation, parity, husband’s occupation, and family’s income.
Out of independent variables nonrelated to COVID-19 pandemic, intention status of recent pregnancy (p < 0.001), history of premenstrual syndrome (p < 0.001), marital conflict (p < 0.001), stressful events (p < 0.001), and social support (p = 0.014) showed significant relationships with anxiety. Also, out of them, the history of premenstrual syndrome (p < 0.001), history of chronic diseases of the mother (p = 0.014), marital conflict (p < 0.001), stressful events (p < 0.001), and social support (p < 0.001) showed significant relationships with depression. (Table 1)
Out of independent variables related to COVID-19 pandemic, history of hospitalization due to COVID-19 among mother’s family members, intimate friends/relatives (p = 0.021) and compliance with preventive health measures showed significant relationships with anxiety (p = 0.008). (Table 2) Also, out of them, the history of mother’s hospitalization due to COVID-19 (p = 0.038) and compliance with preventive health measures showed significant relationships with depression (p < 0.001). (Table 3)
Discussion
The results of the present descriptive cross-sectional study showed that the level of anxiety among studied mothers two months after delivery was 27%. In a study that was conducted in Kashan on pregnant women during COVID-19 pandemic, the level of anxiety was 18.71% and in another study in Ahwaz conducted from March 20th to April 10th 2020, the level of anxiety was 22.3% [21, 22]. The above-mentioned studies were conducted while vaccination has not yet been started for general population and pregnant mothers but this study was conducted after vaccination was started; however, results showed that the prevalence of anxiety was higher in this study which might have been due to the differences between the study environments.
In this study the level of depression was 20%. Also, the results of another study in Singapore during COVID-19 pandemic in 2021 showed that the rate of depression was 17% [23]. In the systematic review by Rajkumar in India (2020) the level of depression was from 16 to 28% [13] and in the systematic review by Usmani (2021) from Turkey, that was titled evaluation of risk factors for post-partum depression during COVID-19 pandemic, the rate of post-partum depression during the pandemic was reported from 7 to 80.8% [9]. The reason for difference in the results of studies might be due to the different time of sampling (disease outbreaks or the gap between outbreaks), study environment, cultural, economic, and social difference as well as different intervals between delivery and sampling.
The results of this study showed no significant relationship between anxiety and depression and mother’s occupation which were in line with the results of two studies conducted on pregnant women during COVID-19 pandemic, one by Saadati in Ahwaz (2020) and another by Karimi (2021) in Tehran [22, 24]. On the contrary, Guvenc et al. (2021) in a study that was conducted on post-partum anxiety and depression during COVID-19 pandemic in Turkey revealed that working pregnant women were more prone to post-partum depression [25]. The reason for this difference might be due to the difference between the participants of the studies. In this study most of participants were housewife and even though the study was conducted during the COVID-19 pandemic, but it was after the vaccination was started and individual’s concerns were reduced, and therefore, working women were less concerned about getting out of the house; but the study by Guvenc et al. (2021) was conducted during the time that people were more willing to stay in the house to prevent infection with COVID-19 and therefore, working women were more likely to develop depression.
The results of this study showed that post-partum anxiety had a significant relationship with the pregnancy being wanted or unwanted; but it was in contrast with the results of the study by Karimi (2021) in Iran during the COVID-19 pandemic which showed no significant relationship between wanted or unwanted pregnancies and mother’s anxiety [24]. It seems that mothers who were not willing to get pregnant during the COVID-19 pandemic were concerned about the problems of raising a child during pandemic, and therefore, unwanted pregnancies were associated with more anxiety in mothers.
On the other hand, the reason for different results might be due to cultural differences, social support and number of participants. Also, this study was conducted on women after delivery and the above-mentioned study was conducted on pregnant women.
According to the results of this study, post-partum depression and anxiety had a significant relationship with premenstrual syndrome; meaning that the prevalence of premenstrual; syndrome was higher among anxious and depressed mothers than mothers with low levels of anxiety and depression. Results of this study were in line with the study by Alimoradi (2019) which indicated a significant relationship between the history of premenstrual syndrome and post-partum depression [26].
The results of this study showed a significant relationship between anxiety and depression and having marital conflicts. Results of this study were in line with the study by Effati Daryani (2020) in Tabriz, which reported marital conflicts as a predictor of anxiety in pregnant women during the COVID-19 pandemic [27]. The study of Seymour (2015) which was conducted in Australia to evaluate the risk factors for anxiety and parenting during the first year of child’s birth, revealed that low quality of marital relationship and having marital conflicts were significantly associated with higher levels of mother’s anxiety. These results were in line with the results of this study [28].
This study also indicated a significant relationship between anxiety and the history of COVID-19 related hospitalization of mother’s relatives. The study of Abedzadeh in Kashan (2021), also showed that history of infection of family members with COVID-19 and concerns about infection of herself and her infant were predictors of anxiety score of pregnant women during the COVID-19 pandemic. These results were in line with the results of this study [21].
This study showed that anxiety and depression had significant relationships with observing preventive health measures by the mother during the pandemic; meaning that, mothers who did not observe preventive health measures had higher levels of anxiety and depression. Results of the study by Xiong (2020) which was titled evaluation of prevalence of and related factors to post-partum depression during the COVID-19 pandemic in women, in Guangzhou of China, indicated that observing preventive health measures had a positive psychological effect. It was in line with the results of this study [13]. Also, the study of Zanardo (2020) in Italy on mothers after their delivery during the COVID-19 pandemic showed that being concerned about getting infected with COVID-19 along with conducted quarantine measures during the pandemic had a negative effect on mothers’ thoughts and emotions after delivery and worsened the symptoms of depression; but, in contrast, in this study, not observing preventive health measures by mothers were associated with higher levels of depression [29]. The reason for this difference might be due to the differences in the time and place of sampling and also differences in the living environments of the mothers.
This study revealed that mothers’ post-partum anxiety and depression had a significant relationship with stressful events of life; in a way that mothers who had experienced more stressful events had higher levels of anxiety. In the study of Abedzadeh (2021), during the COVID-19 pandemic, perceived stress was one of the predictors of anxiety score in pregnant mothers [21]. This result was in line with the result of our study.
Also, this study indicated a significant relationship between post-partum anxiety and depression and perceived social support; in a way that, the prevalence of anxiety was higher among mothers who had received less social support. In this regard, the study of Pandey (2020) from Ethiopia about related factors to general anxiety among mothers receiving prenatal services revealed that poor social support had a significant relationship with general anxiety disorder [30]. Also, the study of Abuhammad (2024) in Jordan aimed to compare the levels of post-partum depression between Arab women residing in Jordan and the United States and the effect of social support on post-partum depression during the COVID-19 pandemic, showed a significant correlation between depression and social support; meaning that, increased social support was associated with decreased depression. The above mentioned results were in line with the results of this study [31]. No published studies are available that showed contrasting results.
Moreover, this study revealed a significant relationship between mother’s post-partum depression and history of having chronic diseases; meaning that, mothers with chronic diseases had higher levels of depression. It seems that suffering from chronic diseases and obligation to consume drugs for a long period of time and receiving constant medical care would lower the mental health and increase the chance of depression in some women. Results of the study by Suarez-Rico (2021), which was conducted on Mexican women after delivery during the COVID-19 pandemic, were in contrast with the results of this study [32]. In the above-mentioned study, having chronic hypertension and pregestational diabetes were evaluated.
Furthermore, results of this study indicated a significant relationship between mother’s post-partum depression and her hospitalization while infected with Covid-19; meaning that, mothers who were hospitalized due to COVID-19 infection had higher levels of depression. Since mothers who were severely infected with COVID-19 had to be hospitalized and, in these cases, the possibility of mortality was higher, it was expected that the level of depression would be higher among them. No other published study has examined this correlation.
Strengths and limitations
The strength point of this study was evaluation of the relationship between post-partum depression and anxiety with variables that have not been noticed in other studies (such as the place of care for mothers infected with COVID-19 and history of hospitalization of mother’s relatives due to COVID-19). One of the limitations of this study was that its environment was limited to a small town and its related villages which could affect the generalization of the results; furthermore, this study was conducted after vaccination was started which might have reduced the concerns in general population and mothers and have reduced the level of depression and anxiety in them.
Conclusions
Results of this study showed that most of the mothers had no anxiety and depression and the prevalence of post-partum anxiety and depression were 27% and 20%, respectively. Also, the mean scores of anxiety and depression were in the level of no anxiety and depression.
Related factors to post-partum anxiety in this study were desirability of pregnancy, history of premenstrual disorder, marital conflicts, history of hospitalization of mother’s relatives due to COVID-19, compliance rate with preventive health measures for COVID-19 by the mother during the COVID-19 pandemic, stressful events, and family support.
Related factors to post-partum depression in this study were history of premenstrual syndrome, having chronic diseases, marital conflicts, and history of mother’s hospitalization when infected with COVID-19, compliance rate with preventive health measures for COVID-19 by the mother during the COVID-19 pandemic, stressful events, and family support.
Data availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request. “The questionnaire of the compliance rate with preventive health measures for COVID-19”, developed by the research team, was written in the text.
References
Ghaedrahmati M, Kazemi A, Kheirabadi G, Ebrahimi A, Bahrami M. Postpartum depression risk factors: a narrative review. J Educ Health Promotion. 2017;6.
Habibzadeh A, Habibzadeh Z. Evaluation of effective factors and its prevalence on postpartum depression among women in the city of Qom, Iran. Int J Women’s Health Reproduc Sci. 2016;4(1):23–8.
Wan Mohamed Radzi CWJB, Salarzadeh Jenatabadi H, Samsudin N. Postpartum depression symptoms in survey-based research: a structural equation analysis. BMC Public Health. 2021;21:1–12.
Chen Q, Li W, Xiong J, Zheng X. Prevalence and risk factors associated with postpartum depression during the COVID-19 pandemic: a literature review and meta-analysis. Int J Environ Res Public Health. 2022;19(4):2219.
Didi-Huberman G, Miller C. Critical image/Imaging critique. Oxf Art J. 2017;40(2):249–61.
Patabendige M, Gamage MM, Weerasinghe M, Jayawardane A. Psychological impact of the COVID-19 pandemic among pregnant women in Sri Lanka. Int J Gynecol Obstet. 2020;151(1):150–3.
Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–20.
Bao Y, Sun Y, Meng S, Shi J, Lu L. 2019-nCoV epidemic: address mental health care to empower society. Lancet. 2020;395(10224):e37–8.
Usmani S, Greca E, Javed S, Sharath M, Sarfraz Z, Sarfraz A, et al. Risk factors for Postpartum Depression during COVID-19 pandemic: a systematic literature review. J Prim Care Community Health. 2021;12:21501327211059348.
Citu C, Gorun F, Motoc A, Sas I, Burlea B, Citu IM, et al. Prevalence and risk factors of postpartum depression in Romanian women during two periods of COVID-19 pandemic. J Clin Med. 2022;11(6):1628.
Ashford MT, Ayers S, Olander EK. Supporting women with postpartum anxiety: exploring views and experiences of specialist community public health nurses in the UK. Health Soc Care Commun. 2017;25(3):1257–64.
Rajkumar RP. COVID-19 and mental health: a review of the existing literature. Asian J Psychiatry. 2020;52:102066.
Xiong R, Liu Y, Liang P, Wang Y, Shi S. Prevalence and factors Associated with Postpartum Depression during the Covid-19 pandemic among women in Guangzhou, China: a cross-sectional study. 2020;10(11)
Gurudatt N. Postpartum depression in working and non-working women. International Proceedings of Economics Development and Research. 2014;78(69).
Rahimi M, Karimi N, Sedighi M, Mousavi S. Postpartum depression and sleep disorders among working women with social support, referring to Health Centers in Shiraz, Iran. J Occup Health Epidemiol. 2019;8(3):141–7.
Afshari P, Tadayon M, Abedi P, Yazdizadeh S. Prevalence and related factors of postpartum depression among reproductive aged women in Ahvaz. Iran Health care Women Int. 2020;41(3):255–65.
Ahmadi kani Golzar A, GoliZadeh Z. Validation of Edinburgh Postpartum Depression Scale (EPDS) for screening postpartum depression in Iran. Iran J Psychiatric Nurs. 2015;3(3):1–10.
Beck AT, Steer RA, Epstein N, Brown G. Beck self-concept test. Psychol Assessment: J Consulting Clin Psychol. 1990;2(2):191.
Khabaz M, Behjati Z, Naseri M. Relationship between social support and coping styles and resiliency in adolescents. 2012:108–23.
Heydari A, Namjoo Z. Comparison of Alexithymia, attachment styles and stress in men and women employees in Ahvaz. 2011:21–40.
Abedzadeh-Kalahroudi M, Karimian Z, Nasiri S, Khorshidifard MS. Anxiety and perceived stress of pregnant women towards Covid-19 disease and its related factors in Kashan (2020). Iran J Obstet Gynecol Infertility. 2021;24(5):8–18.
Saadati N, Afshari P, Boostani H, Beheshtinasab M, Abedi P, Maraghi E. Health anxiety of pregnant women and its related factors during the pandemic of Corona Virus. 2021; 21: 95.
Shorey SY, Ng ED, Chee CY. Anxiety and depressive symptoms of women in the perinatal period during the COVID-19 pandemic: a systematic review and meta-analysis. Scand J Public Health. 2021;49(7):730–40.
Karimi L, Makvandi S, Mahdavian M, Khalili R. Relationship between social support and anxiety caused by COVID-19 in pregnant women. Iran J Obstet Gynecol Infertility. 2021;23(10):9–17.
Guvenc G, Yesilcinar İ, Ozkececi F, Öksüz E, Ozkececi CF, Konukbay D et al. Anxiety, depression, and knowledge level in postpartum women during the COVID-19 pandemic. Perspect Psychiatr Care. 2021;57(3).
Alimoradi B, Nejat H. Brain behavioral systems, early maladaptive Schema, and Premenstrual in Mothers with Postpartum Depression Disorder. Iran J Rehabilitation Res. 2019;6(2):56–65.
Effati-Daryani F, Zarei S, Mohammadi A, Hemmati E, Ghasemi Yngyknd S, Mirghafourvand M. Depression, stress, anxiety and their predictors in Iranian pregnant women during the outbreak of COVID-19. BMC Psychol. 2020;8:1–10.
Seymour M, Giallo R, Cooklin A, Dunning M. Maternal anxiety, risk factors and parenting in the first post-natal year. Child Care Health Dev. 2015;41(2):314–23.
Zanardo V, Manghina V, Giliberti L, Vettore M, Severino L, Straface G. Psychological impact of COVID-19 quarantine measures in northeastern Italy on mothers in the immediate postpartum period. Int J Gynecol Obstet. 2020;150(2):184–8.
Pandey D. The prevalence of general anxiety disorder and its associated factors among women attending the perinatal service of Dilla University referral hospital, Ethiopia during the COVID-19 pandemic. Heliyon. 2020;6(11):e05593.
Abuhammad S, Abu Al-Rub S, Al-Delaimy W. Postnatal depression and social support during the COVID-19 pandemic among arab women in Jordan and the United States: a comparative study. Electron J Gen Med. 2024;21(1):em557.
Suárez-Rico BV, Estrada-Gutierrez G, Sánchez-Martínez M, Perichart-Perera O, Rodríguez-Hernández C, González-Leyva C, et al. Prevalence of depression, anxiety, and perceived stress in postpartum Mexican women during the COVID-19 lockdown. Int J Environ Res Public Health. 2021;18(9):4627.
Acknowledgements
We thank all mothers that participated in the study as well as all staffs of the health centers and health houses involved in the study and Research Deputy of Isfahan University of Medical Sciences.
Funding
This study was approved (approval number: 3400547) and financially supported by the Research Deputy of Isfahan University of Medical Sciences.
Author information
Authors and Affiliations
Contributions
Tahmineh Dadkhahtehrani, Mohammad Javad Tarrahi, and Masoume Salimiyan contributed to the study conception and design. Masoume Salimiyan was responsible for the recruitment. Data analysis was performed by Mohammad Javad Tarrahi. The first draft of the manuscript was written by Tahmineh Dadkhahtehrani, Masoume Salimiyan, and Masoume Pirhadi. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the ethics committee of Isfahan University of Medical Sciences (IR.MUI.RESEARCH.REC.1400.325). In accordance with the Declaration of Helsinki written informed consent was obtained from all the participants, questionnaires were anonymous and confidentiality of the data was considered. Health considerations were observed for mothers and infants at the time of completing the questionnaires.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Salimian, M., Tarrahi, M.J., Dadkhahtehrani, T. et al. The prevalence and related factors of post-partum anxiety and depression among mothers during COVID-19 pandemic in 2021. BMC Public Health 24, 2394 (2024). https://doi.org/10.1186/s12889-024-19843-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-19843-6