Abstract
Background
HIV/AIDS has emerged as a nationwide epidemic and has taken the forefront position as the primary infectious killer of adults in China. The control and prevention of the disease have been hampered by a weak link in the form of heterosexual transmission. However, conventional intervention measures have demonstrated suboptimal efficacy in reducing the incidence of new HIV infections. In light of the current epidemiological characteristics, we have developed and executed an innovative intervention model known as the Joint Prevention and Control Mechanism of the ‘CDC-Public Security Bureau-NGO’. The purpose of this research is to assess the impact of this model on the AIDS awareness, HIV infection rates, sexual behavior, and associated factors among female sex workers and elderly clients. Through the provision of robust evidence of the efficacy of this innovative model, we seek to advocate for its implementation in future interventions.
Methods
The research design of this study incorporates both a serial cross-sectional study and time-series analysis from 2014 to 2021, including a 4-year traditional intervention (2014–2017) and the 4-year ‘CDC-Public Security Bureau-NGO’ innovative intervention (2018–2021), was conducted to evaluate the effects of the new intervention. The GM(1, 1) model was performed to predict the proportion of HIV infection without implementing the innovative intervention in 2018–2021; P and C values were used to evaluate the performance of the model. Mann-Kendall test and descriptive methods were used to analyzed the trend of traditional and innovative interventions models on HIV positive detection rate in FSWs and elderly clients.
Results
The condom usage rates during the last commercial sexual encounter for FSWs and elderly clients improved from 74.9% and 9.1%, respectively, to 96.9% and 28.1%. (P < 0.05), newly reported cases of HIV have decreased by 15.56% yearly and the HIV positive detection rate among middle-aged and elderly people has dropped by 14.47%. The innovative intervention model has significantly reduced the HIV infection rates.
Conclusions
The ‘CDC-Public Security Bureau-NGO’ innovative intervention has achieved beneficial effects on HIV/AIDS prevention and control and provides a good reference for Guangxi, China.
Similar content being viewed by others
Introduction
Acquired immune deficiency syndrome (AIDS) is a highly infectious disease caused by the human immunodeficiency virus (HIV). According to the 2019 data, 151,250 new cases of HIV infections were reported in China, with sexual transmission accounting for 97.1% of cases and heterosexual transmission accounting for 73.8% of cases [1,2,3]. Unprotected sex is the main cause of HIV transmission. In addition, the age of acquiring new HIV infections has shown an uneven distribution trend and the number of infections among young students and the elderly has increased significantly [4,5,6]. In 2019, the number of newly diagnosed HIV infections among elderly individuals in China rose to 28,763, which represents a 500% increase from 2010. This trend is more pronounced in Guangxi, which is the province with the third highest incidence rate of AIDS in China. Studies have found that the proportion of new HIV cases in the elderly population is closely linked to prostitution [7, 8]. Despite some successes achieved through traditional interventions, such as condom promotion programmes and public education campaigns, interventions targeting heterosexual transmission of AIDS still mainly employ conventional methods. Nevertheless, the proportion of new infections among elderly individuals continues to rise [9, 10]. The reason is that HIV prevention is a multi-faceted work and only the Centers for Disease Control and Prevention (CDC) is advancing unilaterally in traditional intervention, which is not ideal. Therefore, there is an urgent need to explore more effective strategies [11].
To decrease HIV transmission among female sex workers and the older population, we have devised a novel tripartite joint intervention policy. For departmental collaboration, we have taken into consideration that prostitution and solicitation are illegal activities. Therefore, we have included the Public Security Bureau to leverage its law enforcement powers in order to crack down on prostitution. The Public Security Bureau and the CDC will jointly participate in the detection and intervention of female sex workers and their clients in high-risk locations. For the general population, the CDC will collaborate with NGOs to increase the scope of HIV testing and conduct more targeted public education campaigns. Based on the principle of community-based interventions, an innovative municipal-level intervention that focuses on the city level, known as the ‘CDC-Public Security Bureau-NGO’ innovative intervention, was designed and implemented in Guigang city from July 2017.
Guigang is located in the southeast of Guangxi, with frequent personnel exchanges, complex terrain and many villages and towns, which makes Guigang city a hot spot for commercial sex trade and HIV transmission. The current situation of the AIDS epidemic in Guangxi province is more representative in Guigang city [12, 13]. From the perspective of the composition of reported cases, the elderly population over 50 years old has increased rapidly since 2005, and by 2016 the percentage of middle-aged and elderly people with newly reported cases reached 59.02%. In terms of transmission routes, 98.88% of cases were transmitted through sexual behaviour, among which heterosexual transmission accounted for 95.5%, ranking second in the region. In terms of comprehensive transmission routes combined with gender, among the newly reported cases males dominated the commercial sexual behaviours, accounting for 86.54%. According to the characteristics of the target population, we designed and implemented an innovative intervention that centred on the joint multisectoral intervention of the CDC, the Public Security Department and NGOs from July 2017: namely, the Joint Prevention and Control Mechanism of the ‘CDC-Public Security Bureau-NGO’.
Our study conducted an 8-year survey and monitoring of two high-risk groups of female sex workers and elderly clients. Focus was on understanding the knowledge, attitude and behavioural changes of female sex workers (FSWs) and elderly clients in the high-risk groups, as well as changes in new HIV infection rates in Guigang city, and evaluating the effect of the innovative intervention, aiming to evaluate whether innovative and traditional interventions have different effects on reducing AIDS awareness, HIV infection rate, sexual behaviour and other effects in the two populations and to provide a scientific basis for the promotion of this strategy in the future.
Methods
Study design
With the support of the Guigang Municipal People’s Government, we designed and implemented the ‘CDC-Public Security Bureau-NGO’ innovative intervention from July 2017. The research design of this study incorporates both a serial cross-sectional study and time-series analysis from 2014 to 2021, population who received this intervention from 2018 to 2021 was defined as the innovation intervention group. The population who received the traditional intervention from 2014 to 2017 was defined as the traditional intervention group. By comparing indicators of awareness and high-risk behaviors, as well as comprehensively assessing the policy’s implementation effectiveness in terms of HIV positive detection rate.
The inclusion criteria for FSWs were: (1) a fixed geographical location in Guigang city; (2) complete demographic information available in the CDC database; and (3) engaged in sex trafficking services in Guigang city from 2014 to 2021, with at least one instance of commercial sexual behaviour during the survey period. The inclusion criteria for elderly clients were: (1) a fixed geographical location in Guigang city; (2) complete demographic information available in the CDC database; (3) age ≥ 50 years; and (4) at least one instance of commercial sexual activity in the past month.
Traditional intervention and ‘CDC-Public Security Bureau-NGO’ innovative intervention
In previous traditional intervention studies, the provincial, municipal and county CDC have undertaken all AIDS prevention and control work in their jurisdictions [14] and the number of staff is limited, so they can only provide limited intervention for the target population in some places on a short-term and regular basis through traditional AIDS education, condom promotion, voluntary HIV counselling, etc.
In the innovative intervention, the CDC has changed from the executor of all HIV prevention and control work to become part of the prevention and control work, playing the role of coordinating the overall situation, leading the way and supervising the prevention and control work (Fig. 1). In order to conduct full-coverage intervention testing for FSWs, it is necessary to screen out all potential sources of infection in the target population, with people in key high-risk places in Guigang city required to undergo HIV antibody testing every three months. The CDC will go to each high-risk site at least once a month to verify and test the key target groups. At the same time, the blood samples of HIV-positive FSWs and HIV-positive elderly clients in Guigang city were genotyped by means of molecular epidemiology; molecular network analysis was used to accurately locate the transmission cluster centre, locating and identifying key super-spreaders, to provide key information for subsequent control of the source of infection and to cut off the route of transmission.
In the innovative intervention, the Public Security Bureau plays a key role in ensuring the implementation of the intervention. In the stage of cutting off the transmission route, FSWs who tested positive will be required not to continue to engage in sex work in the jurisdiction and to cooperate with standardized follow-up management and treatment. If they refuse to obey, the Public Security Bureau will investigate and crack down. Through the method of finding and dealing with one case, the HIV-positive FSWs are precisely targeted and effectively controlled in order to cut off the spread of AIDS through the FSWs to the general population.
Social organizations play a role in ensuring interventions for the entire target population [15]. In the stage of protecting vulnerable groups, social organizations carry out AIDS publicity and intervention activities that are more targeted and diverse than traditional models, strengthening AIDS health education for elderly people, especially rural elderly men over 50 years old, and at the same time increasing AIDS health education. The promotion of voluntary counselling and testing has enabled the elderly in rural areas to conduct HIV testing in a timely manner, with early detection and early treatment, to prevent the spread between husband and wife and to prolong life.
Data collection
The questionnaire designed by the CDC of China included three parts: sociodemographic characteristics, AIDS knowledge and sexual behaviour. Basic HIV/AIDS knowledge and awareness is measured by correctly answering eight questions about HIV/AIDS: (1) ‘Is AIDS an incurable serious infectious disease?’; (2) ‘Is sexual transmission a main mode of transmission of AIDS in our country?’; (3) ‘Can one judge whether a person is infected with AIDS by the appearance of the genitals?’; (4) ‘Will infection with other sexually transmitted diseases increase the risk of HIV infection’; (5) ‘Can insisting on correct use of condoms reduce the risk of HIV infection and transmission?’; (7) ‘After high-risk behaviour (needle sharing, drug use/unsafe sex, etc.), should you actively seek HIV testing and counselling?’; and (8) ‘Does the intentional transmission of AIDS require legal liability?’.
Our samples were collected from sentinel surveillance conducted by the Guigang Centers for Disease Control and Prevention. These sentinel surveillance sites are set up based on administrative regions, specifically targeting high-risk populations for sample collection. According to the Implementation Plan of China’s AIDS Sentinel Surveillance (2017), strict protocols were followed in high-risk service settings to ensure informed consent and anonymity. Professional staff conducted one-on-one monitoring of all high-risk groups. A total of 10,308 FSWs and elderly clients were included in this study, of which 3835 and 1220 received traditional interventions and 3467 and 1787 received innovative interventions, respectively. Among them, 98.6% of FSWs and 96.7% of elderly clients agreed to participate in this study and completed the questionnaire.
In addition, through the data system of the Guigang CDC, this project collected annual data on newly diagnosed HIV-positive cases among FSWs and elderly clients in Guigang city from 2014 to 2021 to assess the impact of comprehensive innovative intervention models.
Data analysis
Chi-square analysis or Fisher test, when appropriate, was used to assess whether the demographic variables, including age, ethnic group, household registry, education level, commercial trading place, and marital status, HIV/AIDS knowledge and high-risk behaviors were different or significantly changed before and after the innovative intervention implementation.
Due to the data imbalance between the traditional intervention and innovative intervention groups, we conducted separate 1:1 propensity score matching (PSM) for FSWs and elderly clients under traditional and innovative interventions. Subsequently, using the matched data, we carried out subsequent analyses to minimize bias introduced by demographic characteristics during different intervention periods as much as possible. Nearest neighbor matching was selected and matched controls were not replaced during matching. Using the propensity scores, innovative intervention groups were randomly matched to traditional intervention groups with 1:1 matching method, with a caliper value of 0.02. The matching criteria included age, education level, commercial trading place, and the presence of a regular sexual partner(s).
A GM(1, 1) prediction model was developed to predict the HIV positive detection rate using SPSSPRO software. Grey system theory was proposed by Deng and is often used for short-term forecasting of small datasets [16]. The principle is to build a dynamic model for a given time-series dataset, accumulate the original time series to generate a new cumulative series and then build a new model based on this. Finally, the results are simplified to generate new predicted values [17]. In this study, the HIV positive detection rate in 2018–2021 was predicted and the agreement with the actual value was assessed. Construction of the GM(1, 1) model was as follows: accumulate the original time-series data once, to weaken randomness and volatility and strengthen regularity, and obtain the accumulated time series Y(t); generate the mean series; and then construct the GM(1, 1) model using the following one-order linear differential equation:
where a is the development coefficient, which reflects the development trend of the original series, and b is the driving coefficient, which reflects the changes in the relationships between the system data.
The Mann-Kendall trend test was employed to evaluate the increase or decrease in the number of HIV positive detection rate during the study period using R 4.1.3 software. In the results, the Mann- Kendall-Tau (τ) < 0 indicated a downward trend for the time series, while the Mann- Kendall-Tau (τ) > 0 indicated an upward trend for the time series.
Results
Demographic characteristics
A total of 10,308 FSWs and elderly clients were included in this study, of which 3835 and 1220 received traditional interventions and 3467 and 1787 received innovative interventions, respectively. Among them, 98.6% of FSWs and 96.7% of elderly clients agreed to participate in this study and completed the questionnaire. The age of FSWs who received traditional and innovative interventions was 30.8 ± 8.6 and 35.0 ± 8.5 years, respectively. Over 75% of FSWs were Han Chinese. Most of the FSWs (89.4% and 95.1% for traditional and innovative intervention, respectively) have education levels below junior high school. Difference analysis of the two intervention modes revealed significant differences in age, household registration, education level, workplace level and the presence or absence of a permanent sexual partner(s) (Table 1).
Table 1 showed the demographic characteristics of the elderly clients in Guigang city. The number of Han elderly clients is much higher than the total number among other ethnic groups. Most of the elderly clients (88.8% and 98.2% for traditional and innovative intervention, respectively) have education levels below junior high school. During the implementation of innovative interventions from 2018 to 2021, the trend among elderly clients in their choice of commercial sexual transaction venues has gradually shifted from traditional high-end locations such as hotels and nightclubs towards lower-tier establishments. In both the traditional and innovative intervention groups, more than 75% of older clients had regular sexual partners. There were significant differences between both groups in age, education level and commercial sex trading venue (P < 0.05) but no difference in terms of race, household registration and presence of a regular sexual partner.
1:1 propensity score matching
To reduce the effect of possible selective bias, we performed a 1:1 propensity score matching(PSM) between the two groups of individuals under traditional and innovative intervention, After matching, there were no statistically significant differences in baseline characteristics between the traditional intervention group and the innovative intervention group (Table 2).
Analysis of basic knowledge and awareness of HIV/AIDS among FSWs and elderly clients during the two interventions periods after PSM
The elderly clients have a moderate awareness of HIV/AIDS knowledge under the traditional and innovative intervention models. Using the HIV knowledge questionnaire (HIVKO) designed by the CDC of China, in the context of the traditional intervention, 87.9% of elderly clients and 65.9% of FSWs reached the correct level of awareness, compared with 95.8% and 95.2% under the comprehensive innovative intervention, respectively. The difference is statistically significant (P < 0.05).
The changes of behavior of condom use and STD prevalence in FSWs between traditional and innovative interventions after PSM
As shown in Table 3, under traditional intervention, 8.2% of FSWs were afflicted with at least one sexually transmitted disease (STD), with 74.9% using condoms during their last commercial sexual encounter. During the innovative intervention period, there was an improvement, with the STD prevalence among FSWs decreasing to 6.0%, and condom usage during the last commercial sexual encounter increasing to 96.9%. Statistical analysis revealed a significant difference between the traditional and innovative intervention groups (P < 0.05).
Effects of traditional and innovative interventions models on condom use in elderly clients after PSM
When comparing the innovative intervention to the traditional intervention, the condom usage rate during the last commercial sexual encounter increased from 12 to 38.7%. The frequency of consistent condom use during monthly commercial sexual encounters rose from 2.3 to 9.7% (Table 4). For other high-risk behaviors, compared to the traditional intervention mode, both the condom use in last sex with spouse or cohabiting partner and condom use for all sex in the last month with spouse or cohabiting partner saw a significant impact on condom usage rates under the innovative intervention mode (P < 0.05).
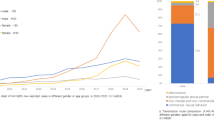
Evaluate the prevalence trends of HIV among FSWs and elderly clients under the innovative intervention model using GM(1, 1) and the exponential smoothing model after PSM
The GM(1, 1) model and the exponential smoothing model are often used for short-term prediction of time series, especially for datasets with a small sample size. This study used GM(1, 1) and the exponential smoothing model to fit the 2014–2017 HIV positive detection rate of FSWs and elderly clients to predict the epidemic trend of 2018–2021. Since the innovative intervention was implemented in 2018, the intervention effect of the innovative mode can be found by comparing the predicted values of the model for 2018–2021 with the true positive detection rate of HIV. As shown in Supplementary Table 1, the RMSE values of the GM(1, 1) model in the FSWs and elderly client datasets were both 0.0042, which are lower than the exponential smoothing model, thus indicating better performance. Therefore, we used the GM(1, 1) model to predict the possible positive detection rate of HIV from 2018 to 2021 based on the data of the traditional intervention. The C values of the model in the FSWs and elderly client datasets were 0.0420 and 0.0086, respectively, indicating that the model has good accuracy (Supplementary Table 1). The error probability P values were both 1.000, indicating that the model was qualified (Supplementary Table 3). From 2018 to 2021, the positive detection rates of HIV were 17.2%, 20.4%, 24.2% and 28.8%, respectively, in FSWs and 39.1%, 45.9%, 53.9% and 63.2% in elderly clients (Fig. 2). Subsequently, we employed Mann-Kendall trend analysis to assess the trends in HIV-positive detection rates among FSWs and elderly clients during the periods of traditional intervention from 2014 to 2017 and innovative intervention from 2018 to 2021. The results, based on GM(1,1) model predictions, indicate that during the period of traditional intervention from 2018 to 2021, the HIV-positive detection rates for FSWs (τ = 0.67) and elderly clients (τ = 1.00) continued to maintain an upward trend. However, in the practical implementation of the innovative intervention from 2018 to 2021, both FSWs (τ=-1.00) and elderly clients (τ=-1.00) experienced a reduction in HIV-positive detection rates, demonstrating a consistent declining trend.
Discussion
In this study we designed an innovative intervention model, the ‘CDC-Public Security Bureau-NGO’. The implementation effect of this model was evaluated and shown to effectively reduce the positive detection rate of HIV/AIDS among elderly clients and FSWs, also reduce the risky behaviours of them.
There were significant differences in some demographic characteristics between traditional and innovative interventions (Table 1). To reduce the effect of possible selective bias, we performed a 1:1 propensity score matching(PSM) between the two groups of individuals under traditional and innovative intervention, the matching criteria included age, education level, commercial trading place, and the presence of a regular sexual partner(s). After matching, there were no significant differences in demographic characteristics between the two intervention modes. Based on this matching, our analysis revealed that the innovative intervention still to ameliorate risky behaviors among both FSWs and elderly clients.
The results indicate that under the traditional intervention mode, the HIV/AIDS knowledge awareness rate among elderly clients exceeds 85%, whereas among FSWs, it stands at only 65.9%. This suggests that the traditional intervention has a certain impact, but its effectiveness in improving HIV/AIDS knowledge awareness among FSWs is suboptimal. The underlying reason for this may be the relative clandestine nature of the FSWs, which may result in limited access to HIV/AIDS education. However, the rate of condom use during nearly one month of commercial sex by elderly clients remains low and most (95.1%) choose to abandon condom use with each other, indicating that ‘separation of knowledge and action’ is a serious issue in the elderly population; and the proportion of voluntary condom use is still low considering the high awareness rate. The above contradictions expose the limitations of traditional intervention models. While elderly clients exhibit a higher level of HIV/AIDS knowledge compared to the FSWs population, the utilization of condoms during their last commercial sexual encounter is significantly lower than that of FSWs. This discrepancy underscores the potential divergence in sexual education and information access pathways between FSWs and elderly clients. FSWs may have easier access to sexual health education information, which could lead to a preference for condom use even if their knowledge of HIV/AIDS is relatively limited. Additionally, the hesitancy towards condom usage and the potential difficulty in obtaining condoms among elderly clients may contribute to their higher HIV/AIDS knowledge but poorer condom usage. Overall, although elderly clients have a high level of AIDS knowledge, they still abandon the use of condoms during commercial sex due to the influence of economy, concept and educational level, etc [18], which inevitably leads to the high positive detection rate of HIV/AIDS among the elderly clients. In addition, because the clients have been dominant in commercial sexual relationships, FSWs are likely to agree to give up condom use for material gain, which also increases the burden of HIV transmission. This situation is more serious among middle-aged and elderly clients. Some studies have shown that 6% of the middle-aged and elderly population lack knowledge of condom use, do not know how to obtain condoms, do not believe condoms can prevent HIV and cannot afford condoms [11]. FSWs, on the other hand, have lower socioeconomic status and suffer from long-term social isolation and stigma. They are often reluctant to argue with clients when they ask not to use condoms during commercial sex [19]. An FSW usually receives many clients every day, and once infected HIV is likely to spread widely among clients [20].
The aforementioned analytical results indicate that traditional interventions have had some impact on HIV/AIDS knowledge levels. The elderly clients in Guangxi have relatively high levels of HIV knowledge. However, due to the separation of knowledge and behavior, as well as the influence of economic, cultural, biological, and legal factors, they often adopt a passive position when it comes to decisions about condom use during commercial sex, and further contributing to HIV infections among FSWs (Fig. 2). However, in the innovative intervention, We expanded HIV testing among high-risk populations, incorporated law enforcement efforts from the Public Security Bureau, and conducted targeted awareness and educational campaigns, the separation of knowledge and action has been significantly improved. More elderly clients and FSWs have used condoms during commercial sex in the previous month and the positive detection rate of HIV has also been decreasing annually. Therefore, we establish this innovative HIV prevention and control system is of importance to correct the behaviour pattern of clients and FSWs in order to limit the transmission of HIV.
The intervention of FSWs has always been a difficult issue for HIV/AIDS prevention and control work in Guangxi Zhuang Autonomous Region, mainly due to the mobility and concealment of FSWs. Elderly clients and FSWs have the same conditions of intervention because of their close interrelationships. In the analysis of elderly clients, we found that implementation of the innovative intervention model can effectively control the spread of HIV/AIDS by precisely targeting HIV-positive FSWs. In Guigang there is a high proportion of the elderly among clients of FSWs and the transmission of HIV is mainly through sexual contact. FSWs who know they are HIV positive usually migrate to other areas to continue their commercial sex work, which results in a much higher HIV-positive detection rate among elderly clients than that of the FSW population. Therefore, the innovative intervention mode for epidemic control is thorough because it fits the above characteristics of HIV in Guigang city. Traditional intervention strategies mainly focus on behavioral intervention and education. Behavioral intervention includes providing free condoms and other protective equipment in high-risk areas, encouraging the use of condoms during commercial sex to reduce the risk of infection, and providing voluntary HIV testing and treatment services for FSWs at high-risk locations. Education involves distributing pamphlets and conducting related activities such as lectures and distributing leaflets at high-risk locations to increase awareness and knowledge of sexual health among elderly clients and FSWs. However, traditional intervention strategies have significant limitations. Firstly, sex workers are often hidden and mobile, making them difficult to locate and intervene, and they often provide services in concealed locations, making intervention work challenging. Secondly, although commercial sex is illegal, the CDC in China has no law enforcement powers or relevant supervision mechanisms, making it difficult to manage and regulate comprehensively. The essence of the innovative intervention model is that the Public Security Bureau and the CDC conduct comprehensive screening for potential infection sources throughout Guigang city, enforce mandatory control of those who are screened as HIV positive and reduce high-risk behaviours by distributing condoms. Furthermore, joint public security departments, procuratorates, courts and social forces are used to detect and combat prostitution to protect vulnerable populations. These combined interventions can effectively compensate for the shortcomings of traditional intervention strategies. In addition, joint interventions by the CDC, public security agencies, and social organizations have the following advantages over traditional intervention strategies. Firstly, it can integrate comprehensive resources. The CDC is responsible for providing HIV prevention knowledge, testing, and treatment services; public security agencies can regulate and crack down on illegal activities; and social organizations can undertake education and rehabilitation work, thus constructing an integrated intervention network. Secondly, it can efficiently provide intervention measures. Through institutional cooperation, relevant information and data, including the activities, risk assessment, and control strategies of elderly clients and FSWs, can be shared. The involvement of public security agencies makes the information collection by the CDC and social organizations more efficient, which is critical for more comprehensive intervention of key populations. Finally, multi-agency interventions can consider the needs of prevention, testing, treatment, and rehabilitation, thus forming a comprehensive strategy for prevention and control to effectively control HIV transmission.
There are some limitations in this study. Firstly, the innovative intervention and the traditional intervention are not conducted in the same period, and there are certain differences in the demographic characteristics. We attempted to eliminate known confounding factors as much as possible through 1:1 propensity score matching, but we still cannot guarantee that all variables, apart from the intervention mode, remained consistent between the two intervention periods. While the matched results have shown satisfactory outcomes, however, we must acknowledge that this still remains one of the limitations of our study. Due to the large time scale, the analysis of intervention effects may be influenced by economic, social and cultural circumstances, which may lead to bias. Secondly, sexual transmission is the main route of HIV infection among FSWs and middle-aged and elderly clients. The innovative intervention model is highly targeted and may not be suitable for the control of all high-risk groups. Thirdly, evaluating the effects of innovative interventions requires long-term observations. Since the launch of the innovative intervention model at the end of 2017, the cognition and behaviour of FSWs and elderly clients have been significantly improved and the HIV positive detection rate has shown a downward yearly trend, but whether these effects can be maintained for a long time in the future remains to be further investigated.
Conclusion
In conclusion, this innovative tripartite intervention model (Joint Prevention and Control Mechanism of the ‘CDC-Public Security Bureau-NGO’) can effectively reduce HIV/AIDS-related risk among FSWs and elderly clients. This innovative intervention model not only provides a favourable environment for reducing the positive detection rate of HIV/AIDS but also precisely combats the behaviour of intentional transmission of the virus. At the same time, the level of HIV/AIDS-related knowledge has been further improved among high-risk groups. This innovative intervention model can be extended to other regions where heterosexual transmission is the main mode, which provides a reference for the prevention and treatment of HIV/AIDS in China.
Data availability
The data are obtained through the database of Guigang Center for Disease Control and Prevention, the datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Abbreviations
- AIDS:
-
Acquired immune deficiency syndrome
- HIV:
-
Human immunodeficiency virus
- CDC:
-
Centers for Disease Control and Prevention
- FSWs:
-
Female sex workers
- HIVKO:
-
HIV knowledge questionnaire
- STDs:
-
Sexually transmitted diseases
- OR:
-
The odds ratio
- PSM:
-
Propensity score matching
References
Liu G, Zhang H, Zhu WB, et al. HIV prevalence among 338,432 infertile individuals in Hunan, China, 2012–2018: a cross-sectional study. PLoS ONE. 2020;15:e0238564.
Cassim N, Coetzee LM, Stevens WS, et al. Addressing antiretroviral therapy-related diagnostic coverage gaps across South Africa using a programmatic approach. Afr J Lab Med. 2018;7:681.
Zhao B, Zhang Z, Li X. Numerical study of the transport of droplets or particles generated by respiratory system indoors. Build Environ. 2005;40:1032–9.
Fourcade L, Sabourin-Poirier C, Perraud V, et al. Natural immunity to HIV is associated with low BLyS/BAFF levels and low frequencies of innate marginal zone like CD1c + B-cells in the genital tract. PLoS Pathog. 2019;15:e1007840.
Manea E, Jipa R, Niculescu I, et al. Co-infections and co-morbidities among injecting drug users versus sexually infected patients in Bucharest. J Int AIDS Soc. 2014;17:19665.
Fraietta JA, Mueller YM, Lozenski KL, et al. Abasic phosphorothioate oligomers inhibit HIV-1 reverse transcription and block virus transmission across polarized ectocervical organ cultures. Antimicrob Agents Chemother. 2014;58:7056–71.
Chen X, Qin C, Chen R, et al. Epidemiological profile and molecular genetic characterization of HIV-1 among female sex workers and elderly male clients in Guangxi, China. Emerg Microbes Infect. 2021;10:384–95.
Heaton B, Gondal N. Health-based homophily in public housing developments. BMC Public Health. 2023;23:238.
Schmid D, Allerberger F, Huhulescu S, et al. Whole genome sequencing as a tool to investigate a cluster of seven cases of listeriosis in Austria and Germany, 2011–2013. Clin Microbiol Infect. 2014;20:431–6.
Liang S, Shen Z, Yan J, et al. Low Virologic failure and drug resistance among HIV-Infected patients receiving hospital-based ART while Care and Outreach through Community in Guangxi, China. Front Public Health. 2015;3:244.
Platt L, Grenfell P, Meiksin R, et al. Associations between sex work laws and sex workers’ health: a systematic review and meta-analysis of quantitative and qualitative studies. PLoS Med. 2018;15:e1002680.
Li L, Sun G, Liang S, et al. Different distribution of HIV-1 subtype and drug resistance were found among treatment naïve individuals in Henan, Guangxi, and Yunnan Province of China. PLoS ONE. 2013;8:e75777.
Lai J, Qin C, Nehl EJ, et al. HIV prevalence among female sex workers in Guigang City, Guangxi, China: an 8-year consecutive cross-sectional study. BMC Public Health. 2018;18:450.
Jin H, Qian X. How the Chinese government has done with Public Health from the perspective of the evaluation and comparison about Public-Health expenditure. Int J Environ Res Public Health 2020;17.
Chandra Y, Jiang LC, Wang CJ. Mining social entrepreneurship strategies using topic modeling. PLoS ONE. 2016;11:e0151342.
Yan J, Li Y, Zhou P. Impact of COVID-19 pandemic on the epidemiology of STDs in China: based on the GM (1,1) model. BMC Infect Dis. 2022;22:519.
Yu J, Zhang Y, Jiang J, et al. Implementation of a County-Township-Village Allied HIV Prevention and Control Intervention in Rural China. AIDS Patient Care STDS. 2017;31:384–93.
Ge XM, Yang WM, Zhu QY, et al. [Epidemiological characteristics of HIV/AIDS in Guangxi Zhuang Autonomous Region, 2010–2017]. Zhonghua Liu Xing Bing Xue Za Zhi. 2019;40:315–21.
Wamoyi J, Wight D, Plummer M, et al. Transactional sex amongst young people in rural northern Tanzania: an ethnography of young women’s motivations and negotiation. Reprod Health. 2010;7:2.
Cuadros DF, Awad SF, Abu-Raddad LJ. Mapping HIV clustering: a strategy for identifying populations at high risk of HIV infection in sub-saharan Africa. Int J Health Geogr. 2013;12:28.
Acknowledgements
The work was supported by the Guangxi Medical University Training Program for Distinguished Young Scholars [to Junjun Jiang], Guangxi Medical University Training Program for Young Leading Talents(to Junjun Jiang) and Guangxi Science and Technology Base and Talent Project [AD21220013]. The authors would like to acknowledge the Guigang Center for Disease Control and Prevention (Guangxi, China) for their help. Thanks to everyone who participated or contributed to this project.
Funding
The work was supported by the Guangxi Medical University Training Program for Distinguished Young Scholars [to Junjun Jiang]; Guangxi Science and Technology Base and Talent Project [GUIKE AD21220013]; Guangxi Medical University Training Program for Young Leading Talents(to Junjun Jiang).
Author information
Authors and Affiliations
Contributions
Junjun Jiang, Fashuang Wei, Hao Liang, Li Ye conceived and designed the study. Xing Tao, Yunxuan Huang, Pingzuo Zheng conducted the data analysis and literature review and drafted the article. Gang Wang, Yuexiang Xu, Yongfeng Chen and Benben Deng were involved in the study supervision, data collection, and interpretation of the data. Xiu Chen, Tongxue Qin, Yinlu Liao, Minjuan Shi, Beibei Lu, Yuting Wu and Jinmiao Li assisted with data management and data analysis. All authors contributed to the revision of the article and approved the fifinal version.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
We confirmed that informed consent was obtained from all subjects and/or their legal guardian(s), and all methods were carried out in accordance with relevant guidelines and regulations. Ethics approval was granted by Guangxi medical University Medical Ethics Committee (approval number: 2019-SB-102).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Tao, X., Huang, Y., Zheng, P. et al. Application of ‘CDC- Public Security Bureau-NGO’ Joint Prevention and Control Mechanism Allied AIDS prevention and control in Guigang, Guangxi. BMC Public Health 24, 2416 (2024). https://doi.org/10.1186/s12889-024-19873-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-19873-0