Abstract
Background
Cardiovascular disease (CVD) is a major health concern for middle-aged and older adults, with lifestyle and metabolic risk factors well-studied. However, the role of psychosocial factors in CVD remains underexplored.
Objective
This study aims to delve into the connection between psychosocial factors and the occurrence of CVD.
Methods
We utilized data from the UK Biobank, a large-scale study covering adults aged 38 to 73 recruited from various centers across the UK between 2006 and 2010. We employed Cox proportional hazards models to analyze the relationship between social isolation, loneliness, and incident CVD. CVD diagnoses were confirmed through hospital records and death-register data. Additionally, we conducted mediation analyses to assess the impact of low-grade inflammation.
Results
The study encompassed 427,942 participants free from CVD, 55.8% of whom are women. High levels of social isolation and loneliness were linked to a higher risk of CVD (HRs 1.11, 95% CI 1.06–1.16; HRs 1.17, 95% CI 1.11–1.23). Depression also emerged as a predictor of CVD onset (HRs 1.25, 95% CI 1.19–1.31), with each psychosocial factor independently contributing to increased CVD risk. Mediation analyses pinpointed inflammation as a crucial mediator, especially for loneliness (indirect effect proportion: 4.7%).
Conclusions
This study underscores the significance of psychosocial factors in relation to CVD. Integrating assessments for social isolation, loneliness, and depression into routine healthcare could potentially aid in CVD prevention among middle-aged and elderly individuals.
Lay summary
This study underscores the significance of psychosocial factors in relation to CVD, emphasizing the association between social isolation or loneliness and the heightened risk of CVD.
Graphical abstract

Similar content being viewed by others
Introduction
Cardiovascular disease (CVD) stands as a paramount global health challenge, profoundly impacting individuals aged 40 and above. Despite substantial therapeutic advancements, CVD claimed 17.9 million lives in 2019, representing a 25.1% increase since 2000 [1]. The projection anticipates around 24 million death by 2030 [2], with a notable rise in the age-standardized rate of CVD in middle-aged and older adults, reflecting the normative physiological changes associated with aging—over 70% of adults develop CVD by 70 years of age [3,4].
Traditionally, CVD has been recognized as a Metabolic and lifestyle related disease, with extensive attention paid to factors like body weight, diet habits, physical activity, smoking, blood pressure, and cholesterol level [5,6,7,8,9]. However recent studies have shown a significant link between mental health and personality traits and CVD [10,11,12]. For instance, Kang et al. (2023) discussed the mental health of CHD patients using data from the UK Household Longitudinal Study [13], and another study by Kang (2024) explored the associations between the big five personality traits and clinical diagnosis of angina [14]. Social isolation and loneliness, often marginalized in discussions on chronic diseases, emerges as compelling yet underexplored variables. Acknowledging this, the World Health Organization (WHO) recently instituted a Commission on Social Connection, emphasizing social isolation as a pressing health threat. The WHO contends that the absence of social connection carries a risk equivalent to, or even greater than, other well-known risk factors [15]. Middle-aged and older adults, often grappling with altered diet, limited physical activity and diminished social contact, face an increased risk of social isolation or loneliness, with one-third projected to experience varying degrees of social isolation or loneliness later in life [16].
This comprehensive perspective is vital for a more precise understanding of cardiovascular risk factors and their association with the risk of CVD. Nevertheless, the intricate association between social isolation, depression and CVD remain inadequately understood, creating a critical gap in knowledge. This study aims to bridge these gaps, focusing on unraveling novel dimensions of the connection between older adults, social isolation, loneliness, and CVD. By positioning social isolation and loneliness, as focal points, we seek to provide insights into the role of social and emotional elements in shaping disease outcomes. This study is motivated by the recognition that an individual’s psychosocial well-being may contribute significantly to the complex trajectory of CVD within middle-aged and older adults.
Additionally, we aim to explore the mechanism underpinning the incidence of CVD. Most individuals develop inflamm-aging, a condition characterized by elevated levels of blood inflammatory markers, heightening susceptibility to chronic morbidity, disability, frailty, and premature death [17]— a critical factor in the development of CVD and atherosclerosis [18]. This subclinical condition, characterized by elevated levels of inflammatory biomarkers without obvious clinical symptoms [17], potentially serves a pathophysiological process linking older subjects at high risk to an increased risk of CVD [Fig. 1].
Therefore, based on the literature and the framework outlined above, our study proposes the following hypotheses: primary hypothesis——increased social isolation and loneliness will be associated with a higher incidence of CVD among middle-aged and older adults, independent of traditional risk factors; secondary hypothesis——the mediation analysis will reveal that inflammation partially mediates the relationship between social isolation, loneliness, and CVD risk. In this study, we investigated the prospective associations of the social isolation and loneliness with CVD risk in participants, particularly comparing their relative importance to traditional risk factors (e.g. lifestyle factors and metabolic risk factors) in CVD risk. Moreover, we evaluate the mediation role of inflammation in relation to CVD risk.
Methods
Study design and participants
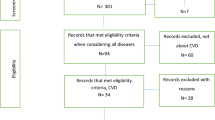
Our study leverages the expansive and diverse UK Biobank, a resource established between 2006 and 2010, featuring a cohort exceeding 500,000 participants aged 38 to 73 [19]. Recruitment efforts extends across a 35-mile radius, encompassing 22 assessment centers in England, Scotland, and Wales, and this radius aimed to ensure accessibility for participants residing within these areas to the assessment centers. Baseline assessments were thorough, gathering both questionnaire responses and biological data. The UK Biobank’ questionnaire was developed by a research team consisting of several people. The intention was to create a composite questionnaire out of previously existing and validated measures, taking into account participant acceptability, scope for collaborations with international studies through making results comparable, and the need to balance depth and breadth of phenotyping. Ethical approval for this study was secured from the UK North West Multi-Centre Research Ethics Committee (reference number 11/NW/0382), ensuring adherence to rigorous ethical standards. Under application number 95,180, our research, unfolds prospectively, focusing on individuals without pre-existing CVD at baseline. To uphold transparency and reliability in reporting, we strictly adhere to STROBE guidelines [20]. In this investigation, we restricted to UK Biobank participants who manifested no signs of CVD at baseline (n = 427,942). Exclusions comprised 151 participants without CVD diagnosis time, 7,589 participants with prior CVD diagnoses and 66,682 participants with missing confounder data [see Additional file 1 Figure S1].
Exposure and outcome
Data on social isolation and loneliness were gathered through a touchscreen questionnaire developed and administered by the UK Biobank. To provide transparency and facilitate further investigation, we have included a direct link to the questionnaire on the UK Biobank website in the Data Availability section for readers’ access. The evaluation of social isolation incorporated three social isolation factors: household size, social activities involvement, and frequency of friends or family visits. Household size was collected via a self-report question: “Including yourself, how many people are living together in your household?”, social activities involvement was collected via a self-report question: “Which of the following leisure/social activities do you engage in once a week or more often?”, and frequency of friends or family visits was collected via a self-report question: “How often do you visit friends or family or have them visit you?” High-risk social isolation factors were defined as follows: living alone, never engaging in leisure or social activities, never or less than once per month receiving friends’ visits [21,22,23]. Participants meeting two or more of these criteria were classified as experiencing high-risk social isolation. To evaluate loneliness, two primary factors were considered: self-reported feelings of loneliness, and the frequency of confiding in others. Loneliness was collected via a self-report question: “Do you often feel lonely?”, and the frequency of confiding in others was collected via a self-report question: “How often are you able to confide in someone close to you?” High-risk loneliness factors were defined as follows: persistent experiences of loneliness and infrequent confiding in a close friend (less than once per month) [21,22,23].
We utilized pre-identified outcomes for CVD. These outcomes were derived through algorithmic combinations of coded information from linkage of three primary data sources: the baseline assessment data collection of the UK Biobank (which encompassed self-reported medical conditions, operations, and medications), linked data from hospital admissions (encompassing diagnoses and procedures), and information from death registries.
Confounders
Our analytical framework included a comprehensive array of confounders, guided by insights from prior research on the risk factors of CVD [1,6,7,8,22,24], taking into account the possession of variable data in the UK Biobank database to finalize the confounders included in our study. This approach ensured that our analysis included relevant and comprehensive confounders. The selected confounders encompass a wide range of participant demographics and health-related factors at baseline, including age, sex, ethnicity, educational background, deprivation index, and body mass index (BMI). Mental health status was thoroughly considered, encompassing variables such as depression, loneliness, and social isolation. Health behaviors were also factored in, including smoking status, alcohol use, physical activity, sleep duration, dietary habits, and salt use. Additionally, the presence of specific diseases at baseline, such as family history of stroke, family history of heart disease, diabetes, hypertension, as well as the use of medications for diabetes, hypertension, and hyperlipidemia, were taken into account. To address potential variations related to seasonal influences on self-reported measures of social connection, the month of assessment was incorporated as a covariate in the statistical analysis [25,26]. A detailed description of the collection and definitions of these confounders is provided in the appendix [see Additional file 1 Table S1].
Measuring low-grade inflammation
In evaluating the magnitude of low-grade inflammation, we employed the Low-Grade Inflammation Score (INFLA-score), a composite index tailored explicitly to measure the intensity of low-grade inflammation [27]. This score incorporates four well-established inflammatory biomarkers: C-reactive protein (CRP), white blood cell count, platelet count, and the neutrophil-to-lymphocyte ratio (NLR). The computation of the INFLA-score involves assigning each of these four components a value within the range of -4 to 4, reflecting their respective deciles. Subsequently, the individual scores of these components are summated, yielding a cumulative score that spans from − 16 to 16 (refer to Supplementary Table 3 for details). A heightened INFLA-score indicates an increased level of low-grade inflammation.
Statistical analysis
Our analytical endeavor commenced with an exploration of the baseline characteristics within the study population. For categorical variables, proportions were presented, while means along with standard deviations were reported for continuous variables. Our primary objective was to investigate the association between social isolation or loneliness and the risk of CVD. This exploration spanned the entire study population, utilizing Cox proportional hazards regression models to estimate hazard ratios (HRs) and 95% confidence intervals (CI) for the relationship between social isolation, loneliness, and the risk of CVD.
The validation of the proportional hazard assumption was conducted through log cumulative hazard plots [see Additional file 1 Figure S9-14], which revealed parallel hazard curves for groups with and without social isolation or loneliness, affirming the assumption’s validity. Follow-up time was defined from the recruitment date to the endpoint, encompassing CVD diagnosis, death, loss to follow-up, or the conclusion of follow-up on the latest available hospital admission and mortality data (19 December 2022), whichever transpired first.
To estimate the effect size of social isolation and loneliness on CVD risk, a systematic step-by-step approach for confounders adjustment was adopted, progressively including variables to address potential confounders. All variables were adjusted in their original form without categorization. This approach was applied to continuous variables such as BMI and age, as well as categorical variables like ethnicity, smoking status, and alcohol intake. Our fully adjusted Model 4 comprehensively considered various confounders, including age, sex, ethnicity background, education, deprivation index, BMI, month of assessment, depression, smoking status, alcohol drink frequency, physical activity, sleep duration, diet, salt consumption, family history of stroke, family history of heart disease, diabetes, hypertension, diabetes medication use, hypertension medication use, and hyperlipidemia medication use.
Furthermore, to ensure consistency in our analysis, we used the same form of variables across both the forest plot and Cox regression analyses. The forest plot visually represents the hazard ratios and confidence intervals for each covariate, providing a clear summary of the effects of social isolation and loneliness on CVD risk.
Additionally, we explored the potential mediation effect of low-grade inflammation on the association between social isolation or loneliness and CVD risk. The mediation analysis followed a regression-based approach [28] to estimate the indirect effect of social isolation or loneliness on CVD through low-grade inflammation. Specifically, we applied the widely empolyed mediation formula method [28,29,30], adjusting for a comprehensive set of confounders identified from the literature as potential confounders. This method involved:
-
a)
Estimating the total effect of social isolation or loneliness on CVD risk; b) Assessing the effect of social isolation or loneliness on low-grade inflammation; c) Evaluating the effect of low-grade inflammation on CVD risk, adjusting for the exposure (social isolation or loneliness) and other confounders. The indirect effect of social isolation or loneliness on CVD risk through low-grade inflammation was calculated as the product of the effect of social isolation or loneliness on inflammation and the effect of inflammation on CVD risk. The proportion of mediation was obtained by dividing the indirect effect by the total effect. All confounders included in the multivariate-adjusted Cox regression model (Model 4) were similarly adjusted in the mediation analyses to control for potential confounding effects.
In our pursuit of robust and reliable findings, an array of sensitivity analyses was undertaken. These analyses explored the influence of including only CVD cases occurring at least 2 or 5 years since baseline, thereby minimizing potential reverse causality effects. Stratified analysis was performed for age (≥ 38 to < 50 years, ≥ 50 to < 60 years, ≥ 60 to < 70 years and ≥ 70 to ≤ 73 years), sex (female, male), education (with or without/below university degree), Townsend deprivation index, depression status (with or without depression), smoking (never, current, previous), alcohol consumption (never/special occasions only, one to three times a month/once or twice a week, three or four times a week / daily or almost daily), physicial activity (yes, no), and sleep duration (< 7 h, 7–8 h and > 8 h). Additionally, a competing risk analysis was conducted, considering death as a competing event. Finally, interaction effects of behaviors (such as smoking) and morbidity status (depression, diabetes, and hypertension) with social isolation and loneliness on the risk of CVD were examined by introducing a product interaction term to the model. The significance of the interaction effect was determined by calculating p values through comparing models with and without the added product interaction. All statistical analyses were executed using R software, version 4.2.1, and a two-sided p value of 0.05 or less was considered indicative of statistical significance.
Results
Following the exclusion of individuals with missing data and baseline CVD, our analysis focused on 427,942 participants. Among them, there were 20,608 incident CVD cases, including 7,972 incident stroke cases and 12,742 incident myocardial infarction cases. Participants were stratified into social isolation and loneliness groups to examine CVD risk over a median follow-up of 13.8 years [Table 1]. The average survival time was 10.7 (10.6–10.8) years for CVD, 7.5 (7.4–7.6) years for stroke, and 12.6 (12.5–12.7) years for myocardial infarction [see Additional file 1 Figure S15-20], with incidence rates of 360.0, 139.3, and 222.6 per 100,000 person-years, respectively. Participants, with a mean age of 56.8 years (SD 8.1), comprised 55.8% females and 44.2% males. A predominant 95.6% identified as White. The prevalence of social isolation was higher among older adults and males. Specifically, 8.5% of participants aged 60–70 years and 8.9% of those aged 70–73 years reported social isolation, compared to 7.9% of those aged 38–50 years. Additionally, 9.2% of males reported social isolation versus 8.3% of females.
Those identified as high risk of CVD during follow-up (20,608 CVD cases) were more likely to be older (3.6% vs. 7.1% in 50–60 years group and 60–70 years group), of Asian ethnicity (6.2% vs. 4.8% White), with lower education (5.4% vs. 3.6% university degree), current smokers (7.7% vs. 3.8% never-smokers), frequent salt intake (6.6% vs. 4.5% never/rarely add salt), and having depression (5.4% vs. 4.8%), diabetes (11.7% vs. 4.5%), or hypertension (8.1% vs. 3.7%).
In the multivariable model, social isolation and loneliness emerged as significant influencers of CVD risk. The HRs for CVD were 1.11 (95% CI: 1.06 to 1.16) and 1.17 (95% CI: 1.11–1.23) for social isolation and loneliness, respectively. Consistent findings extended to CVD subtypes like stroke and myocardial infarction [Table 2]. The forest plot highlighted increased CVD risk for participants using insulin, diagnosed with diabetes, hypertension, and depression [see Additional file 1 Figure S2-4], with HRs of 1.68 (95% CI: 1.54 to 1.85), 1.35 (95% CI: 1.28 to 1.42), 1.28 (95% CI: 1.23 to 1.34), and 1.25 (95% CI: 1.19 to 1.31), respectively. Sensitivity analyses affirmed result robustness, maintaining consistency across scenarios [see Additional file 1 Table S2-4].
Stratified analysis revealed that social loneliness and loneliness were more significant for CVD risk in vulnerable groups—specifically, old age, female gender, low socioeconomic status, lower education levels, alcohol drinkers, current smokers, physically inactive, and sleep-deprived [see Additional file 1 Table S5-13]. Statistically significant interactions were noted for depression, smoking, diabetes, hypertension, and CVD. Associations were particularly prominent in high-risk groups, such as those with depression, current or previous smokers, and previous diseases. The combined exposure to social isolation and loneliness heightened these interactions beyond the effects of the individual exposures [see Additional file 1 Figure S5-8].
In mediation analyses, inflammation played a pivotal role, mediating 4.5% of the total effect on CVD risk for loneliness [Table 3]. This underscores the intricate relationship between psychosocial factors and CVD, suggesting inflammation as a key mechanistic link.
Discussion
CVD presents a formidable global health challenge, demanding nuanced exploration to decipher the intricacies of risk factors [1]. In our study focused on individuals aged 38 and above, we delved into the multifaceted dimensions of CVD risks beyond conventional metabolic parameters [3,9,24].
Our baseline analysis unearthed a distinctive risk profile among older adults experiencing social isolation. This group exhibited correlations with lower education, socioeconomic status, obesity, depression, higher proportions of current smokers, alcohol drinkers, lack of physical activity and individuals with shorter sleep duration, and diabetes. These findings align with existing research, emphasizing the interplay between unfavorable socioeconomic and lifestyle factors and the heightened risk of social isolation and loneliness [10,31,32,33]. The distinct risk profile observed among socially isolated individuals aged 38 and above sheds light on the complex interplay of sociodemographic and lifestyle factors. In published stuides, emotional repercussions, including fear and anxiety, can arise, prompting individuals to withdraw from social interactions [34,35]. Our findings underline the emotional toll, including heightened fear and anxiety, as additional dimensions influencing social isolation in this age group. This broader understanding emphasizes the imperative for holistic, multidimensional interventions aimed at alleviating social isolation.
In this cohort study, we established a robust association between social isolation, loneliness, and incident CVD, highlighting the pivotal role of psychosocial elements in CVD risk assessments. Notably, even after adjusting for an extensive array of health behaviors and outcomes, social isolation and loneliness retained an 11.0% and 17.0% attributable risk proportion for incident CVD, respectively. The mechanisms underpinning the association between social isolation, loneliness, and CVD may partially involve health behaviors and changing health status [36]. Longitudinal studies indicate that individuals exposed to social isolation and loneliness exhibit a higher prevalence of behavioral risk factors, including smoking, alcohol use, physical inactivity, and sleep insufficiency [37,38,39]. Moreover, the presence of chronic disease such as diabetes and hypertension can escalate an individual’s risk of CVD [40].
Moving beyond the mere identification of social isolation and loneliness as contributors to CVD risk, our study substantiates the robustness of these associations through a meticulous exploration of various scenarios in sensitivity analyses, including various scenarios and stratified analyses. The latter enriches our insights by revealing moderating effects, particularly in vulnerable groups. This group, predominantly female, exhibited correlations with lower education, socioeconomic status, and higher proportions of current smokers, alcohol drinkers, and individuals with shorter sleep duration. This highlights the dynamic and context-dependent nature of social isolation’s impact on CVD risk, urging tailored interventions that acknowledge the diversity within this age group.
The independent associations of social isolation and loneliness with incident CVD, even after meticulous adjustment for a spectrum of health behaviors and outcomes, provoke deeper reflection. While health behaviors and changing health status may partly explain these associations, the residual effects suggest a complex interplay that extends beyond conventional risk factors. Our study prompts a reconsideration of the conventional narrative, encouraging researchers to explore the intricate pathways linking social psychological states to cardiovascular health.
Aging and inflammation are recognized as pivotal factors in CVD risk among older adults [4]. The leading theories focus on aging and inflammation, suggesting one of the mechanisms cause chronic inflammation of CVD is the accumulation of senescent cells in many tissues [41,42]. CVD begins in senescent cells or damaged endothelial cells that allow accumulation of cholesterol-containing low-density lipoprotein (LDL) particles, which tend to oxidize in the vessel wall. This initiates a strong inflammatory reaction that occurs with the effect of the triggering factors, including the interaction of the innate and the adaptive immune cells and the endothelial cells [43]. In the advanced process, inflammation is exacerbated by the accumulation of apoptosis and senescent cells. Complications such as plaque rupture, plaque hemorrhage and acute vascular occlusion may develop [44].
Our mediation analysis enhances this understanding by quantifying the role of inflammation in connecting social isolation to CVD. The proportion of the effect mediated by inflammation provides numerical insight into the significance of this pathway, enriching our comprehension of the interplay between social factors and cardiovascular health.
While confirming existing theories, particularly the link between aging, inflammation, and CVD, our findings highlight the importance of inflammation as a mechanistic link in the social isolation/lonesliness-CVD connection. This contributes to a nuanced understanding of CVD trajectories in middle-aged and older adults. Future research directions should explore targeted interventions addressing inflammation and its modifiable determinants. This comprehensive insight reinforces the significance of tailored interventions in managing CVD risk in this demographic.
The strength of our study lies in its large sample size, longitudinal design, and the incorporation of a comprehensive set of variables. Also, we used mediation analysis to quantify the effects by low-grade inflammation explaining the possible underlying mechanisms of specific association between traditional risk factors control of CVD, social isolation and the risk of CVD. Nevertheless, this study has some relevant limitations. First, the study population was overwhelmingly White, thus the findings may not be generalizable to other populations. Second, the effect of residual confounding might remain, even though we had considered a wide range of confounders. Third, our mediation analysis approach, while informative, may be subject to biases inherent in the traditional regression-based methods, such as mediator-outcome confounding and exposure-mediator interaction [45]. Furthermore, our study primarily relied on baseline data for covariate assessment, which limits our ability to capture changes in variables over time that could influence CVD risk. This approach was chosen to ensure data quality and consistency across participants throughout the study period. However, it restricts our analysis from exploring the dynamic interplay of risk factors over time, which may affect the robustness of our findings in understanding long-term CVD outcomes. Finally, the observational nature and psychological factors such as the personality factors of the particpants could not be controlled limits our ability to establish causation. Furthermore, the reliance on self-reported data on social isolation introduces potential biases. Future research should consider alternative mediation analysis approaches, such as inverse probability weighting or the G-formula [45], which may better account for the complexities of mediator-outcome relationships in observational data. Additionally, employing more extensive psycho-social assessments and biomarker measurements could enhance understanding of the intricate connections identified in our study.
In conclusion, our study goes beyond the surface by recognizing social isolation and loneliness as substantive psycho-social factors influencing CVD risk among individuals aged 38 and above. The discussion elevates these findings from mere observations to a deeper understanding of the complexities involved. By embracing the nuanced interplay of sociodemographic, emotional, and biological factors, our research sets the stage for targeted, effective interventions, ultimately contributing to improved cardiovascular outcomes in this high-risk demographic.
Data availability
1) Data sharing: https://biobank.ndph.ox.ac.uk/showcase/index.cgi (UK Biobank)0.2) Resource sharing: https://biobank.ndph.ox.ac.uk/showcase/index.cgi (UK Biobank).This research has been conducted using the UK Biobank Resource under Application Number 95180.
References
Roth GA, Mensah GA, Johnson CO, et al. Global Burden of Cardiovascular diseases and Risk factors, 1990–2019. J Am Coll Cardiol. 2020;76(25):2982–3021.
Soppert J, Lehrke M, Marx N, Jankowski J, Noels H. Lipoproteins and lipids in cardiovascular disease: from mechanistic insights to therapeutic targeting. Adv Drug Deliv Rev. 2020;159:4–33.
Tinetti ME, Fried TR, Boyd CM. Designing Health Care for the most common chronic Condition—Multimorbidity. JAMA. 2012;307(23).
Forman DE, Maurer MS, Boyd C, et al. Multimorbidity in older adults with Cardiovascular Disease. J Am Coll Cardiol. 2018;71(19):2149–61.
Fuchs FD, Whelton PK. High blood pressure and Cardiovascular Disease. Hypertension. 2020;75(2):285–92.
Francula-Zaninovic S, Nola IA. Management of Measurable Variable Cardiovascular Disease’ risk factors. Curr Cardiol Rev. 2018;14(3):153–63.
Badimon L, Chagas P, Chiva-Blanch G. Diet and Cardiovascular Disease: effects of foods and nutrients in Classical and Emerging Cardiovascular Risk factors. Curr Med Chem. 2019;26(19):3639–51.
Yusuf S, Joseph P, Rangarajan S, et al. Modifiable risk factors, cardiovascular disease, and mortality in 155 722 individuals from 21 high-income, middle-income, and low-income countries (PURE): a prospective cohort study. Lancet. 2020;395(10226):795–808.
Costantino S, Paneni F, Cosentino F. Ageing, metabolism and cardiovascular disease. J Physiol. 2016;594(8):2061–73.
Fakoya OA, McCorry NK, Donnelly M. Loneliness and social isolation interventions for older adults: a scoping review of reviews. BMC Public Health. 2020;20(1):129.
Xia N, Li H, Loneliness. Social isolation, and Cardiovascular Health. Antioxid Redox Signal. 2018;28(9):837–51.
Wang F, Gao Y, Han Z, et al. A systematic review and meta-analysis of 90 cohort studies of social isolation, loneliness and mortality. Nat Hum Behav. 2023;7(8):1307–19.
Kang W, Malvaso A. Mental Health in Coronary Heart Disease (CHD) patients: findings from the UK Household Longitudinal Study (UKHLS). Healthcare. 2023;11(10):1364.
Kang W. Exploring the retrospective and prospective associations between the big five personality traits and clinical diagnosis of angina in middle-aged and older adults. J Psychosom Res. 2024;182:111803.
World Health Organization. Social isolation and loneliness have serious health consequences. Published November 14. 2023. Accessed December 15, 2023. https://www.who.int/multi-media/details/social-isolation-and-loneliness-have-serious-health-consequences
Landeiro F, Barrows P, Nuttall Musson E, Gray AM, Leal J. Reducing social isolation and loneliness in older people: a systematic review protocol. BMJ Open. 2017;7(5):e013778.
Ferrucci L, Fabbri E. Inflammageing: chronic inflammation in ageing, cardiovascular disease, and frailty. Nat Rev Cardiol. 2018;15(9):505–22.
Chai S, Davis K, Zhang Z, Zha L, Kirschner K. Effects of Tart Cherry juice on biomarkers of inflammation and oxidative stress in older adults. Nutrients. 2019;11(2):228.
Caleyachetty R, Littlejohns T, Lacey B, et al. United Kingdom Biobank (UK Biobank). J Am Coll Cardiol. 2021;78(1):56–65.
Ghaferi AA, Schwartz TA, Pawlik TM. STROBE reporting guidelines for Observational studies. JAMA Surg. 2021;156(6):577.
Song Y, Zhu C, Shi B, et al. Social isolation, loneliness, and incident type 2 diabetes mellitus: results from two large prospective cohorts in Europe and East Asia and mendelian randomization. eClinicalMedicine. 2023;64:102236.
Golaszewski NM, LaCroix AZ, Godino JG, et al. Evaluation of social isolation, loneliness, and Cardiovascular Disease among older women in the US. JAMA Netw Open. 2022;5(2):e2146461.
Zhou J, Tang R, Wang X, Li X, Heianza Y, Qi L. Improvement of social isolation and loneliness and excess mortality risk in people with obesity. JAMA Netw Open. 2024;7(1):e2352824.
Ciumărnean L, Milaciu MV, Negrean V, et al. Cardiovascular Risk factors and physical activity for the Prevention of Cardiovascular diseases in the Elderly. Int J Environ Res Public Health. 2021;19(1):207.
Lyall LM, Wyse CA, Graham N, et al. Association of disrupted circadian rhythmicity with mood disorders, subjective wellbeing, and cognitive function: a cross-sectional study of 91 105 participants from the UK Biobank. Lancet Psychiatry. 2018;5(6):507–14.
Victor C et al. Dancing with loneliness in later life: a pilot study mapping seasonal variations. 2015.
Bonaccio M, Di Castelnuovo A, Pounis G, et al. A score of low-grade inflammation and risk of mortality: prospective findings from the Moli-Sani study. Haematologica. 2016;101(11):1434–41.
Lee H, Cashin AG, Lamb SE, et al. A Guideline for reporting mediation analyses of randomized trials and observational studies: the AGReMA Statement. JAMA. 2021;326(11):1045.
Zhang Z, Zheng C, Kim C, Van Poucke S, Lin S, Lan P. Causal mediation analysis in the context of clinical research. Ann Transl Med. 2016;4(21):425.
Imai K, Keele L, Tingley D. A general approach to causal mediation analysis. Psychol Methods. 2010;15(4):309–34.
Dahlberg L, McKee KJ, Frank A, Naseer M. A systematic review of longitudinal risk factors for loneliness in older adults. Aging Ment Health. 2022;26(2):225–49.
Freak-Poli R, Ryan J, Tran T, et al. Social isolation, social support and loneliness as independent concepts, and their relationship with health-related quality of life among older women. Aging Ment Health. 2022;26(7):1335–44.
Hoang P, King JA, Moore S, et al. Interventions Associated with reduced loneliness and social isolation in older adults: a systematic review and Meta-analysis. JAMA Netw Open. 2022;5(10):e2236676.
Kraynak TE, Marsland AL, Gianaros PJ. Neural mechanisms linking emotion with Cardiovascular Disease. Curr Cardiol Rep. 2018;20(12):128.
Harshfield EL, Pennells L, Schwartz JE, et al. Association between depressive symptoms and Incident Cardiovascular diseases. JAMA. 2020;324(23):2396.
Cacioppo JT, Hawkley LC, Crawford LE, et al. Loneliness and health: potential mechanisms. Psychosom Med. 2002;64(3):407–17.
Kobayashi LC, Steptoe A. Social isolation, loneliness, and Health behaviors at older ages: Longitudinal Cohort Study. Ann Behav Med. 2018;52(7):582–93.
Qi X, Malone SK, Pei Y, Zhu Z, Wu B. Associations of social isolation and loneliness with the onset of insomnia symptoms among middle-aged and older adults in the United States: a population-based cohort study. Psychiatry Res. 2023;325:115266.
Valtorta NK, Kanaan M, Gilbody S, Ronzi S, Hanratty B. Loneliness and social isolation as risk factors for coronary heart disease and stroke: systematic review and meta-analysis of longitudinal observational studies. Heart. 2016;102(13):1009–16.
Wang X, Ma H, Li X, Heianza Y, Fonseca V, Qi L. Joint association of loneliness and traditional risk factor control and incident cardiovascular disease in diabetes patients. Eur Heart J. 2023;44(28):2583–91.
Shivakoti R, Biggs ML, Djoussé L, et al. Intake and sources of Dietary Fiber, inflammation, and Cardiovascular Disease in older US adults. JAMA Netw Open. 2022;5(3):e225012.
Soysal P, Arik F, Smith L, Jackson SE, Isik AT, Inflammation. Frailty and Cardiovascular Disease. In: Veronese N, editor. Frailty and Cardiovascular diseases. Advances in Experimental Medicine and Biology. Volume 1216. Springer International Publishing; 2020. pp. 55–64.
Libby P, Ridker PM, Hansson GK. Progress and challenges in translating the biology of atherosclerosis. Nature. 2011;473(7347):317–25.
Tabas I, Bornfeldt KE. Macrophage phenotype and function in different stages of atherosclerosis. Circ Res. 2016;118(4):653–67.
Richiardi L, Bellocco R, Zugna D. Mediation analysis in epidemiology: methods, interpretation and bias. Int J Epidemiol. 2013;42(5):1511–9.
Acknowledgements
The authors would like to acknowledge the support of all paper participants to this paper.
Funding
This study was supported by Key Discipline of Zhejiang Province in Public Health and Preventive Medicine (First Class, Category A), Hangzhou Medical College; Natural Science Foundation of Zhejiang Province (No.LTGY23H260009), China; and Zhejiang Province Key Science and Technology Plan for Medicine and Health (No. WKJ-ZJ-2333).
Author information
Authors and Affiliations
Contributions
Contributions of all paper participants to this papermanuscript. Ruoqi Dai researched data. Xiao Tan, Yingjun Li reviewed/edited the manuscript. Lilu Ding and Ruoqi Dai wrote the main manuscript text. Jing Qian, Hui Zhang, Jingyou Miao, Jing Wang contributed to discussion. The authors thank Xiao Tan, Yingjun Li for help with preparing the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The experimental protocol was established, according to the ethical guidelines of the Helsinki Declaration and was approved by the Human Ethics Committee of North West Multi-centre Research Ethics Committee. Written informed consent was obtained from individual or guardian participants. The ethics approval number is 21/NW/0157.
Questionnaire/interview/survey
1)Touchscreen questionnaire: http://biobank.ctsu.ox.ac.uk/crystal/label.cgi? id=100025 id=100025(UK Biobank).
2)Verbal interview: http://biobank.ctsu.ox.ac.uk/crystal/label.cgi? id=100071id=100071 (UK Biobank).
3)Physical measures: http://biobank.ctsu.ox.ac.uk/crystal/label.cgi? id=100006id=100006 (UK Biobank).
4)Web-based questionnaires: http://biobank.ctsu.ox.ac.uk/crystal/label.cgi?id=100089 (UK Biobank).
5)Physical activity monitor: http://biobank.ctsu.ox.ac.uk/crystal/label.cgi?id=1008 (UK Biobank).
Consent for publication
All authors of the manuscript have read and agreed to its content and are accountable for all aspects of the accuracy and integrity of the manuscript in accordance with ICMJE criteria.
That the article is original, has not already been published in a journal, and is not currently under consideration by another journal.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ding, L., Dai, R., Qian, J. et al. Psycho-social dimensions of cardiovascular risk: exploring the impact of social isolation and loneliness in middle-aged and older adults. BMC Public Health 24, 2355 (2024). https://doi.org/10.1186/s12889-024-19885-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-19885-w