Abstract
Background
Recreational water activities at beaches are popular among Canadians. However, these activities can increase the risk of recreational water illnesses (RWI) among beachgoers. Few studies have been conducted in Canada to determine the risk of these illnesses. This protocol describes the methodology for a study to determine the risk and burden of RWI due to exposure to fecal pollution at beaches in Canada.
Methods
This study will use a mixed-methods approach, consisting of a prospective cohort study of beachgoers with embedded qualitative research. The cohort study involves recruiting and enrolling participants at public beaches across Canada, ascertaining their water and sand contact exposure status, then following-up after seven days to determine the incidence of acute RWI outcomes. We will test beach water samples each recruitment day for culture-based E. coli, enterococci using rapid molecular methods, and microbial source tracking biomarkers. The study started in 2023 and will continue to 2025 at beaches in British Columbia, Manitoba, Ontario, and Nova Scotia. The target enrollment is 5000 beachgoers. Multilevel logistic regression models will be fitted to examine the relationships between water and sand contact and RWI among beachgoers. We will also examine differences in risks by beachgoer age, gender, and beach location and the influence of fecal indicator bacteria and other water quality parameters on these relationships. Sensitivity analyses will be conducted to examine the impact of various alternative exposure and outcome definitions on these associations. The qualitative research phase will include focus groups with beachgoers and key informant interviews to provide additional contextual insights into the study findings. The study will use an integrated knowledge translation approach.
Discussion
Initial implementation of the study at two Toronto, Ontario, beaches in 2023 confirmed that recruitment is feasible and that a high completion rate (80%) can be achieved for the follow-up survey. While recall bias could be a concern for the self-reported RWI outcomes, we will examine the impact of this bias in a negative control analysis. Study findings will inform future recreational water quality guidelines, policies, and risk communication strategies in Canada.
Similar content being viewed by others
Background
Going to the beach is a popular seasonal activity among Canadians. For example, the percentage of Canadian households that reported swimming, going to the beach, surfing, scuba diving, or snorkeling close to home in the past 12 months more than tripled (6% to 21%) from 2011 to 2021 [1]. These activities are associated with numerous health benefits, including improved cardiovascular health, mental health, quality-of-life, and well-being [2, 3]. In addition, beach tourism contributes substantially to local economies. For example, in Ontario, Canada, there were an estimated 6.5 million beach visits in 2014, contributing $1.6 billion in beachgoer spending – representing 6.6% of all visitor spending in the province that year [4]. Despite these benefits, recreational water activities can expose beachgoers to pathogens that cause recreational water illness (RWI) [5,6,7,8,9,10,11]. Water contact at beaches impacted by fecal pollution sources primarily increases the risk of acute gastrointestinal illness (AGI), but can also lead to an increased risk of respiratory, skin, ear, and eye infections [5, 7,8,9, 11, 12].
In the U.S., approximately 90 million cases of RWI occur each year, resulting in annual costs of US$2.2–3.7 billion [12]. The costs of AGI specifically due to swimming or wading in beach water are > US$1,600 (range of $425–2,743) per 1,000 beachgoers, with lost productivity (e.g., having to stay home from school or work due to illness) the major driver of these costs [13]. Additionally, recreational water quality is a health equity issue, presenting disproportionate risks for different sociodemographic groups. For example, children and youth experience more severe health outcomes from beach water exposures [12]. They tend to spend more time in the water and playing in the sand, swallow more water, and have developing immune and digestive systems that place them at greater risk of illness [5, 10, 14,15,16].
In Canada, Health Canada publishes guidelines for recreational water quality at beaches. The most recent updates to the guidelines were published in 2024 [17]. These guidelines are used by local and provincial public and environmental health authorities across Canada who are responsible for local beach water monitoring, risk management, and risk communication. The guidelines recommend that authorities take public health action (e.g., issue a swimming advisory, investigate pollution sources) if ‘beach action values’ (BAV) are exceeded [17]. The BAVs are derived from epidemiological studies conducted in the U.S. from the 1990s to 2010, and correspond to an AGI rate of ~ 36 illnesses/1,000 bathers [18, 19]. The direct applicability and suitability of these BAVs for Canadian settings is unclear, because RWI incidence and fecal indicator bacteria levels are driven by diverse and varying pollution sources, environmental and weather patterns, and beachgoer activities [8, 20,21,22]. There is a need to conduct prospective research on RWI in Canadian settings to better inform these guidelines and public health risk management decisions with Canada-specific data.
While extensive data are available from the U.S. and other countries on the risk and burden of RWI in beachgoers [8], the last prospective cohort study in Canada to estimate the risk of RWI was conducted in 1980 [23]. Timely, updated information is needed on the incidence of AGI and other types of RWI in Canada. This manuscript describes a protocol for a national, prospective beach cohort study that will provide important baseline data on RWI risks at popular freshwater and marine beaches across multiple Canadian provinces and settings. The study will aim to identify RWI risks among demographic groups under different environmental and water quality conditions to inform beach water management policies and local risk management strategies.
Methods
Study objectives
The purpose of this study is to determine the burden of RWI among beachgoers at beaches across five regional sites in Canada. The specific objectives are to:
-
1.
Measure the risk and burden of five different RWI outcomes (AGI, respiratory, eye, ear, and skin infections) in beachgoers that engage in different levels of water and sand contact;
-
2.
Identify differences in RWI risks by beachgoer gender, age, and beach location;
-
3.
Determine relationships between various fecal indicator bacteria measures, environmental parameters, and the risk of AGI among beachgoers; and
-
4.
Understand beachgoer risk perceptions and behaviours related to recreational water quality and socio-political issues that may impact RWI risks among beachgoers.
Study design
We will use a mixed-methods approach in this study: a quantitative prospective cohort study will be conducted to address the first three objectives, with embedded qualitative research to address the fourth objective [24]. This approach combines the strengths of both methods to provide a more comprehensive understanding of this complex public health issue [24]. A prospective cohort study design was selected for consistency with and allowing comparability to prior studies, including the U.S. National Epidemiological and Environmental Assessment of Recreational water (NEEAR) study [5, 8, 11, 14, 25,26,27,28]. The qualitative research phase will include focus groups with beachgoers during and after the cohort study and key informant interviews to provide additional contextual insights into the study findings. The study is registered at ClinicalTrials.gov (ID: NCT06413485; registration date: May 9, 2024).
Study settings
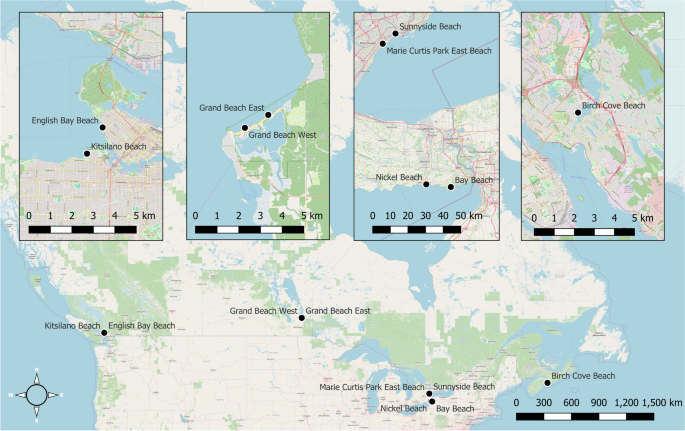
The study will take place at beaches across five regional sites in British Columbia, Manitoba, Ontario, and Nova Scotia (Fig. 1). In British Columbia, recruitment will be conducted at two City of Vancouver marine water beaches in 2024: English Bay Beach and Kitsilano Beach. In Manitoba, recruitment will be conducted at Grand Beach East and West in 2024, both located on the East side of Lake Winnipeg. Two sites will be included from Ontario: Toronto and Niagara Region. In Toronto, recruitment was conducted in the summer of 2023 at Sunnyside and Marie Curtis Park East beaches on Lake Ontario. In Niagara Region, recruitment will be conducted in 2025 at Bay Beach in Fort Erie and Nickel Beach in Port Colborne, both located on Lake Erie. In Nova Scotia, recruitment will be conducted in 2025 at Birch Cove Beach on Lake Banook. The sites were selected to provide a diverse cross-section of beach types (i.e., marine and freshwater), pollution sources, and geographic regions. The specific beaches at each site were identified in consultation with regional collaborators as the best candidate sites for this study because the beaches are popular and frequently used for water and sand contact activities by families with young children and beach water quality is variable, reflecting one or more persistent or recurring sources of fecal contamination [29].
Participant enrolment and eligibility
Trained data collectors will recruit beachgoers at one to two beaches per site for ~ 35 days throughout the summer months (June to September). Data collectors will approach as many beachgoers as possible each day for enrolment, prioritizing families with children given their higher risk of RWI. Based on initial study recruitment in 2023 and prior studies [5, 25, 30], we anticipate recruiting ~ 15 households per day, with ~ 1.7 individuals per household. This corresponds to a total sample size of ~ 5000 beachgoers (~ 3000 households), with an average of ~ 1000 per site. Household members will be recruited and surveyed together. Each household member will be considered a separate study participant. Eligibility criteria will include: (a) ability to provide informed consent for the study and complete the surveys in English or French; (b) home address in Canada or the U.S.; and (c) not having participated in the study in the past 21 days. Given the acute and self-limiting outcomes, individuals will be allowed to participate again after a 21-day washout period [14, 25, 30, 31].
Survey process
Two surveys will be conducted with each enrolled participant: (1) beach survey, and (2) follow-up survey (see Additional file 1). Upon recruitment, beachgoers will be advised to visit our study tables setup near entrances to complete the beach survey before they leave. The beach survey will determine contact information, sociodemographic characteristics, other pre-identified confounding variables, and exposures at the beach [14, 25,26,27, 30,31,32]. The beach survey will be implemented on tablets using a web-based survey platform. The follow-up survey will be completed seven days after participants’ beach visits. Participants will have an option of completing the follow-up survey online or by telephone. This survey will ask about RWI outcomes experienced since the beach visit. Questionnaires were adapted from the U.S. NEEAR study [14, 25], and initial pre-testing was conducted with 10 individuals using a cognitive interviewing approach [33]. We then piloted the questionnaires and study feasibility at a Toronto beach in 2022 [34], made enhancements, and implemented the initial round of recruitment at the Toronto study site in 2023.
Exposures and outcomes of interest
The primary exposure of interest is level of recreational water contact activities (vs. no water contact) among beachgoers. Specifically, we will examine a graded classification of this exposure based on individuals’ minimum level of water contact: 1) no water contact; 2) minimal contact; 3) body immersion; and 4) swallowed water [5, 10, 28, 30]. This classification will allow us to determine a possible dose–response relationship between water contact and illness. Minimal contact is defined as water contact that does not result in body immersion (e.g., wading below one’s waist, boating, fishing). Body immersion is defined as entering the water above one’s waist (e.g., swimming, surfing, snorkelling), and swallowing water as ingestion of any amount of water [5, 28, 30]. A secondary exposure of interest is sand contact activities (e.g., digging in the sand) [35].
The primary outcome measure is AGI in the 7-day period following beach water contact, which corresponds with incubation periods of viral and bacterial enteric pathogens of concern [36, 37]. We define AGI using an internationally accepted definition as one or more of: (a) diarrhea (≥ 3 loose stools in 24 h); (b) vomiting; (c) nausea with stomach cramps; or (d) nausea or stomach cramps that interfere with regular daily activities (e.g., missed work or school) [5, 14, 25,26,27]. Secondary outcome measures include: acute respiratory illness (fever with sore throat, fever with nasal congestion, or cough with phlegm); skin infection (rash or itchy skin); ear infection or earache; and eye infection or irritation [14, 25,26,27, 31]. Days of missed work, school, or vacation, use of medications to treat symptoms, and medical consultations related to AGI will also be collected as indicators of illness severity [5, 38].
Water quality and environmental parameters
We will measure various water quality and environmental indicators of fecal contamination as effect modifiers on the water contact-illness outcome relationships. In Canada, culture-based E. coli is still primarily used as the fecal indicator bacteria of interest for beach water quality. We will collect water samples each recruitment day to test for E. coli following standard culture-based methods [39]. In addition, we will also test water samples for enterococci using the U.S. EPA-validated qPCR method and for microbial source tracking (MST) biomarkers using digital PCR analysis [40,41,42,43,44]. The molecular approach to testing for enterococci was added to the most recent version of the Canadian guidelines for recreational water quality as a recommended, rapid approach for fecal indicator bacteria monitoring [18]. The MST analysis will detect and quantify host-specific DNA biomarkers to characterize the contribution of different sources of fecal contamination at study beaches [40, 44]. This analysis will use standard probes and primers for human sewage (HF183), seagulls (Gull4), Canada geese (mitochondrial DNA), dogs (DG3), and ruminants (Rum-2-Bac) [40, 44]. Additionally, we will collect information on beach environmental conditions, including air temperature and precipitation from the nearest weather station and water turbidity using a turbidimeter. Together, these data will support future decision-making about which fecal indicator and environmental measures are more strongly associated with AGI in Canada under different conditions.
Confounding variables
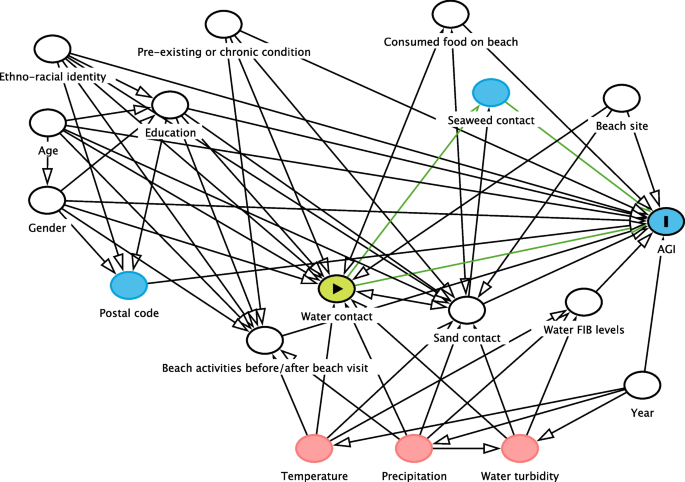
We will measure and adjust for important confounding variables in our analyses to mitigate the impact of possible confounding bias. We have compiled all potentially confounding variables into directed acyclic graphs (DAG) to determine the minimal sufficient adjustment sets for each exposure-outcome of interest [45, 46]. The DAG for the water contact and AGI relationship is shown in Fig. 2. The key participant-level confounding variables that require adjustment include age, gender, ethno-racial identity, education level, pre-existing or chronic conditions, other beach activities engaged in before or after the beach visit, sand contact, and consumption of food on the beach. We will also adjust for beach site, year, and beach water fecal indicator bacteria levels. Other listed variables do not require adjustment in the main-effects model. Confounders for other outcomes are summarized in Additional file 2.
Directed acyclic graph for the water contact and AGI relationship. Legend: Directed acyclic graph of the minimal adjustment set of confounding variables for the relationship between level of water contact and AGI. The water contact variable is the exposure of interest, while all variables with white circles require adjustment in the analysis to determine unbiased estimates of effect
Data analysis plan
We will construct multilevel logistic regression models under a Bayesian analysis framework to determine the causal effects of water and sand contact exposures on our five binary health outcomes of interest [47,48,49]. Each of the five health outcomes, as well as missed activities, medication use, and medical consultations due to AGI, will be evaluated in separate models. Varying intercepts will be included to adjust for clustering of participants by household, recruitment date, and beach location [47, 49]. All models will adjust for a minimal set of confounding variables specific to the exposure-outcome relationship. Differences in risks by beachgoer age and gender will be examined through their influence as effect modifiers. We will examine gender-specific differences in RWI, following recommended categories: boy/man, girl/woman, transgender, gender fluid [50]. We will examine risk differences between the following age groups (0–4, 5–9, 10–14, 15–19, and 20 +) [20]. The relationship between different measures of beach water fecal indicator bacteria (E. coli, enterococci, and MST biomarkers) and AGI will be determined by examining their interaction with the exposure.
Weakly informative prior probability distributions for model parameters will be determined from prior research and evaluated to ensure the model is skeptical of highly unlikely or implausible values [47, 48]. The appropriateness of priors will be assessed via prior predictive checking, and the impact of priors on each model will be assessed via sensitivity analysis [51]. Causal effects will be determined by examining and contrasting posterior probability distributions of parameters and their summary measures (mean and 95% credible intervals) [47,48,49]. Marginal effects plots will be created to visualize the effects of each predictor of interest, as well as interactions, on the predicted probability of each outcome [52]. Sensitivity analyses will be conducted to evaluate the impact of alternate exposure and outcome definitions (e.g., time spent in the water vs. level of water contact, diarrhea vs. AGI) and post-exposure illness timeframes (e.g., 3 and 5 vs. 7 days). Alternative models and variable specifications will be compared and selected using leave-one-out cross-validation [53]. Additionally, we will conduct a negative control analysis by examining the association between fecal indicator bacteria levels and AGI rates among the unexposed participants to identify possible residual confounding or differential outcome reporting bias [5, 54, 55]. Based on prior research, we expect findings will be robust to these possible biases [5, 14, 26, 27].
Power and precision analysis
We conducted a power and precision analysis using the planned approach described above for the main-effect relationship between level of water contact and AGI incidence [56]. For this analysis, we assumed that ~ 60% of beachgoers will have water contact, of which ~ 35% will immerse their body and ~ 10% will swallow water [13, 20, 34]. We specified weakly informative prior distributions for each water contact parameter (minimal contact, body immersion, and swallowing water compared to no water contact), based on previously reported measures of effect [8, 10, 25]. These mean effects correspond to odds ratios of approximately 1.35, 1.5, and 1.8 for each respective exposure level compared to no water contact. Across 500 simulated datasets and analyses, the anticipated sample size of 5000 beachgoers (assuming a 20% attrition rate for the follow-up survey) should have precise credible intervals and an average power of 87% and 94%, respectively, to detect a positive association with body immersion and swallowing water compared to no water contact (with a posterior probability > 0.95). See Additional file 3 for full details and results of this simulation.
Embedded qualitative research
Embedded qualitative research will be conducted to inform, enrich, and enhance the value of the cohort study [24, 57, 58]. We will approach the qualitative research through a pragmatist paradigm that aims to produce policy-relevant outcomes that can prevent and mitigate RWI [58]. Focus groups will be conducted with parents and guardians of beachgoing children and youth to identify recreational water quality risk perceptions and behaviours [59]. Participants will be recruited through online panels or advertisements. We will recruit participants with diverse identity characteristics to capture a range of perspectives. Key informant interviews will also be conducted with public health inspectors and managers who oversee beach water quality programs in Canada and with representatives of other stakeholder groups (e.g., beach operators, beachgoer associations). We anticipate that these interviews will identify and highlight additional socio-political factors relevant to our data interpretation and recommendations. Interview participants will be recruited through professional listservs, stakeholder referrals, online searches, and policy documents.
We will conduct six to eight focus groups with 6–8 participants per group, and 15–20 key informant interviews, which should provide adequate saturation of themes [59,60,61]. Focus groups and interviews will be conducted virtually and will follow semi-structured question guides. The qualitative data will be analyzed using thematic analysis [59, 62]. Analysis will be guided by the Health Belief Model and Theoretical Domains Framework [63, 64]. Two independent analysts will conduct the analysis by applying theory-based and inductive codes to the transcribed audio recordings. Codes will be sorted and grouped to determine key experiences, priorities, opportunities, and challenges for improving beach water quality risk management and communication.
The focus group and interview results will be integrated with the cohort study at the interpretation level [57]. This will include narrative integration, where findings of both components will be jointly discussed by thematic area [57]. Additionally, we will develop joint displays, where cohort study results will be compared visually in tables or figures alongside the focus group results [57, 65]. For example, if we find sociodemographic differences in RWI risks, the focus group results may provide additional contextual insights that can explain and enrich the findings.
Knowledge translation plan
The study is using an integrated knowledge translation approach. Knowledge users helped conceive the study, set the objectives, and create the protocol. They will continue to be involved throughout the study through a stakeholder steering group that meets 2–3 times per year. Results of the study will be submitted for presentations at relevant conferences and published in peer-reviewed journals. Additional knowledge translation techniques will include but are not limited to presentations at knowledge-user events or webinars, dissemination of infographics and policy briefs, and implementation of a project website.
Discussion
Our 2022 feasibility pilot study and 2023 implementation in the first study site achieved very high household participation rates (60–70%), similar to prior studies [5, 26, 27, 29, 30], suggesting that there should be no issues with recruitment feasibility. In our 2022 limited-resource feasibility study at a Toronto beach, we had a very high attrition rate (65%), which was likely due to a lack of monetary incentive [34]. Therefore, we made several enhancements that have been incorporated into this protocol and were implemented successfully in the 2023 initial recruitment site, leading to a much lower attrition rate (20%). The enhancements included: $10 gift card incentive for each participating household (given after completion of the first beach survey); additional prize draw for households that complete the follow-up survey; more frequent follow-up reminders sent by multiple modes (email, text message, phone); and enhanced training for data collectors to emphasize the importance of the follow-up survey to participants upon enrolment [66,67,68]. Our 2023 data and prior research found that those who were lost to follow-up had similar characteristics to those completing the follow-up survey [14, 25, 30, 31], suggesting attrition should not affect our estimation of measures of association and inferences [69]. If our recruitment targets are not met after the 2025 season, additional recruitment may be conducted at one or more other beaches in 2026 depending on available resources.
Conducting a feasibility pilot and full implementation of the study at the first site has provided field experience to anticipate and adapt to other logistical issues that may arise over the course of the study. For example, recruitment days will be flexible, scheduled each week depending on weather conditions to avoid days with expected low attendance (e.g., rainy days). While recall bias could be a concern for follow-up measures, prior studies have found that associations were robust to this possible bias [14, 26, 27, 30]. Use of non-specific, symptom-based, and internationally comparable outcome measures allows a pragmatic and cost-effective approach to assess numerous possible etiological causes of RWI. Further, self-reported RWI outcomes have been shown to be strongly associated with laboratory-confirmed infection due to common etiological agents of concern [70, 71]. Our negative control analysis will assess possible impacts of this bias, as the water fecal indicator bacteria levels are unlikely to be related to participants’ recall of RWI.
This study will provide Canadian-specific data that may be used to support updates to the Canadian recreational water quality guidelines and inform policies and risk communication strategies [17]. The results can also be used to inform targeted surveillance strategies, exposure and risk assessments, and source attribution activities of Canadian enteric disease initiatives [72]. Local and provincial public and environmental health authorities can use the results to guide risk management at public beaches, including development of site-specific strategies for fecal indicator bacteria monitoring and swimming advisories. In addition, the risk perception and behaviour data from the embedded qualitative research can enhance beach water risk communication and public messaging strategies. This will help beachgoers, particularly families with young children, to make more informed decisions about when to visit the beach and how to reduce their risk of RWI (e.g., lower vs. higher risk activities).
Availability of data and materials
Upon completion of the study, an anonymized version of the dataset will be made publicly available for non-commercial purposes.
Data availability
No datasets were generated or analysed during the current study.
References
Statistics Canada. Table 38–10–0121–01: participation in outdoor activities. 2023. https://doi.org/10.25318/3810012101-eng. Accessed 17 June 2024.
Denton H, Aranda K. The wellbeing benefits of sea swimming. Is it time to revisit the sea cure? Qual Res Sport Exerc Health. 2019;12:647–63.
Lazar JM, Khanna N, Chesler R, Salciccioli L. Swimming and the heart. Int J Cardiol. 2013;168:19–26.
Ontario Ministry of Tourism, Culture and Sport. Ontario beach tourism statistics 2014. 2017. https://rto12.ca/wp-content/uploads/2014/04/Ontario-Beach-Tourism-2014.pdf. Accessed 17 June 2024.
Arnold BF, Wade TJ, Benjamin-Chung J, Schiff KC, Griffith JF, Dufour AP, et al. Acute gastroenteritis and recreational water: highest burden among young US children. Am J Public Health. 2016;106:1690–7.
Wade TJ, Pai N, Eisenberg JNS, Colford JM. Do U.S. Environmental Protection Agency water quality guidelines for recreational waters prevent gastrointestinal illness? A systematic review and meta-analysis. Environ Health Perspect. 2003;111:1102–9.
Mannocci A, Torre GL, Spagnoli A, Solimini AG, Palazzo C, De Giusti M, et al. Is swimming in recreational water associated with the occurrence of respiratory illness? A systematic review and meta-analysis. J Water Health. 2016;14:590–9.
Russo GS, Eftim SE, Goldstone AE, Dufour AP, Nappier SP, Wade TJ. Evaluating health risks associated with exposure to ambient surface waters during recreational activities: a systematic review and meta-analysis. Water Res. 2020;176:115729.
Yau V, Wade TJ, de Wilde CK, Colford JM. Skin-related symptoms following exposure to recreational water: a systematic review and meta-analysis. Water Qual Expo Health. 2009;1:79–103.
Wade TJ, Arnold BF, Schiff K, Colford JM, Weisberg SB, Griffith JF, et al. Health risks to children from exposure to fecally-contaminated recreational water. PLoS One. 2022;17:e0266749.
Leonard AF, Singer A, Ukoumunne OC, Gaze WH, Garside R, et al. Is it safe to go back into the water? A systematic review and meta-analysis of the risk of acquiring infections from recreational exposure to seawater. Int J Epidemiol. 2018;47:572–86.
DeFlorio-Barker S, Wing C, Jones RM, Dorevitch S. Estimate of incidence and cost of recreational waterborne illness on United States surface waters. Environ Health. 2018;17:3.
DeFlorio-Barker S, Wade TJ, Jones RM, Friedman LS, Wing C, Dorevitch S. Estimated costs of sporadic gastrointestinal illness associated with surface water recreation: a combined analysis of data from NEEAR and CHEERS studies. Environ Health Perspect. 2017;125:215–22.
Wade TJ, Calderon RL, Brenner KP, Sams E, Beach M, Haugland R, et al. High sensitivity of children to swimming-associated gastrointestinal illness: results using a rapid assay of recreational water quality. Epidemiol. 2008;19:375–83.
Dufour AP, Behymer TD, Cantú R, Magnuson M, Wymer LJ. Ingestion of swimming pool water by recreational swimmers. J Water Health. 2017;15:429–37.
Deflorio-Barker S, Arnold BF, Sams EA, Dufour AP, Colford JM, Weisberg SB, et al. Child environmental exposures to water and sand at the beach: findings from studies of over 68,000 subjects at 12 beaches. J Expo Sci Environ Epidemiol. 2018;28:93–100.
Health Canada. Guidelines for Canadian recreational water quality: summary document. 2024. https://www.canada.ca/en/health-canada/services/publications/healthy-living/guidelines-canadian-recreational-water-quality-summary-document.html. Accessed 17 June 2024.
Health Canada. Guidelines for Canadian recreational water quality: indicators of fecal contamination. 2023. https://www.canada.ca/en/health-canada/services/publications/healthy-living/recreational-water-quality-guidelines-indicators-fecal-contamination.html. Accessed 17 June 2024.
US EPA. Recreational water quality criteria. EPA 820-F-12-058. 2012. https://www.epa.gov/sites/default/files/2015-10/documents/rwqc2012.pdf. Accessed 17 June 2024.
Collier SA, Wade TJ, Sams EA, Hlavsa MC, Dufour AP, Beach MJ. Swimming in the USA: beachgoer characteristics and health outcomes at US marine and freshwater beaches. J Water Health. 2015;13:531–43.
Nevers MB, Whitman RL. Efficacy of monitoring and empirical predictive modeling at improving public health protection at Chicago beaches. Water Res. 2011;45:1659–68.
Francy DS, Stelzer EA, Duris JW, Brady AMG, Harrison JH, Johnson HE, et al. Predictive models for Escherichia coli concentrations at inland lake beaches and relationship of model variables to pathogen detection. Appl Environ Microbiol. 2013;79:1676–88.
Seyfried PL, Tobin RS, Brown NE, Ness PF. A prospective study of swimming-related illness I. Swimming-associated health risk. Am J Public Health. 1985;75:1068–70.
Creswell JW, Plano Clark VL. Designing and conducting mixed methods research. Los Angeles: SAGE Publications, Inc.; 2018.
Wade TJ, Calderon RL, Sams E, Beach M, Brenner KP, Williams AH, et al. Rapidly measured indicators of recreational water quality are predictive of swimming-associated gastrointestinal illness. Environ Health Perspect. 2006;114:24–8.
Wade TJ, Sams E, Brenner KP, Haugland R, Chern E, Beach M, et al. Rapidly measured indicators of recreational water quality and swimming-associated illness at marine beaches: a prospective cohort study. Environ Health. 2010;9:66.
Dorevitch S, Pratap P, Wroblewski M, Hryhorczuk DO, Li H, Liu LC, et al. Health risks of limited-contact water recreation. Environ Health Perspect. 2012;120:192–7.
Colford JM, Schiff KC, Griffith JF, Yau V, Arnold BF, Wright CC, et al. Using rapid indicators for Enterococcus to assess the risk of illness after exposure to urban runoff contaminated marine water. Water Res. 2012;46:2176–86.
Wade TJ, Sams EA, Haugland RA, Brenner KP, Li Q, Wymer L, et al. Report on 2009 national epidemiologic and environmental assessment of recreational water epidemiology studies. Washington, DC: U.S. Environmental Protection Agency; 2010.
Arnold BF, Schiff KC, Griffith JF, Gruber JS, Yau V, Wright CC, et al. Swimmer illness associated with marine water exposure and water quality indicators: impact of widely used assumptions. Epidemiol. 2013;24:845–53.
Colford JM, Wade TJ, Schiff KC, Wright CC, Griffith JF, Sandhu SK, et al. Water quality indicators and the risk of illness at beaches with nonpoint sources of fecal contamination. Epidemiol. 2007;18:27–35.
Dorevitch S, DeFlorio-Barker S, Jones RM, Liu L. Water quality as a predictor of gastrointestinal illness following incidental contact water recreation. Water Res. 2015;83:94–103.
Peterson CH, Peterson NA, Powell KG. Cognitive interviewing for item development: validity evidence based on content and response processes. Meas Eval Couns Dev. 2017;50:217–23.
Young I, Sanchez JJ, Desta BN, Heasley C, Tustin J. Recreational water exposures and illness outcomes at a freshwater beach in Toronto, Canada: a prospective cohort pilot study. PLoS ONE. 2023;18:e0286584.
Heaney CD, Sams E, Dufour AP, Brenner KP, Haugland RA, Chern E, et al. Fecal indicators in sand, sand contact, and risk of enteric illness among beachgoers. Epidemiol. 2012;23:95–106.
Lee RM, Lessler J, Lee RA, Rudolph KE, Reich NG, Perl TM, et al. Incubation periods of viral gastroenteritis: a systematic review. BMC Infect Dis. 2013;13:1–11.
Chai SJ, Gu W, O’Connor KA, Richardson LC, Tauxe RV. Incubation periods of enteric illnesses in foodborne outbreaks, United States, 1998–2013. Epidemiol Infect. 2019;147:e285.
Deflorio-Barker S, Wade TJ, Turyk M, Dorevitch S. Water recreation and illness severity. J Water Health. 2016;14:713–26.
Health Canada. Guidelines for Canadian recreational water quality: microbiological sampling and analysis. 2023. https://www.canada.ca/en/health-canada/programs/consultation-guidelines-canadian-recreational-water-quality-microbiological-sampling-analysis/document.html. Accessed 17 June 2024.
Edge TA, Boyd RJ, Shum P, Thomas JL. Microbial source tracking to identify fecal sources contaminating the Toronto Harbour and Don River watershed in wet and dry weather. J Great Lakes Res. 2021;47:366–77.
Saleem F, Edge TA, Schellhorn HE. Validation of qPCR method for enterococci quantification at Toronto beaches: application for rapid recreational water monitoring. J Great Lakes Res. 2022;48:707–16.
Shrestha A, Dorevitch S. Slow adoption of rapid testing: beach monitoring and notification using qPCR. J Microbiol Methods. 2020;174:105947.
Saleem F, Schellhorn HE, Simhon A, Edge TA. Same-day Enterococcus qPCR results of recreational water quality at two Toronto beaches provide added public health protection and reduced beach days lost. Can J Public Health. 2023;114:676–87.
Staley ZR, Boyd RJ, Shum P, Edge TA. Microbial source tracking using quantitative and digital PCR to identify sources of fecal contamination in stormwater, river water, and beach water in a Great Lakes area of concern. Appl Environ Microbiol. 2018;84:1634–52.
Tennant PWG, Murray EJ, Arnold KF, Berrie L, Fox MP, Gadd SC, et al. Use of directed acyclic graphs (DAGs) to identify confounders in applied health research: review and recommendations. Int J Epidemiol. 2021;50:620–32.
Textor J, van der Zander B, Gilthorpe MS, Liśkiewicz M, Ellison GT. Robust causal inference using directed acyclic graphs: the R package ‘dagitty.’ Int J Epidemiol. 2016;45:1887–94.
McElreath R. Statistical rethinking. Boca Raton: Chapman and Hall/CRC; 2020.
van de Schoot R, Depaoli S, King R, Kramer B, Märtens K, Tadesse MG, et al. Bayesian statistics and modelling. Nat Rev Methods Primers. 2021;1:1–26.
Bürkner PC. brms: an R package for Bayesian multilevel models using Stan. J Stat Softw. 2017;80:1–28.
Bauer GR, Braimoh J, Scheim AI, Dharma C. Transgender-inclusive measures of sex/gender for population surveys: mixed-methods evaluation and recommendations. PLoS ONE. 2017;12:e0178043.
Gabry J, Simpson D, Vehtari A, Betancourt M, Gelman A. Visualization in Bayesian workflow. J R Stat Soc Ser A Stat Soc. 2019;182:389–402.
Arel-Bundock V, Greifer N, Heiss A. How to intepret statistical models using marginaleffects for R and Python. 2024. https://marginaleffects.com. Accessed 28 Aug 2024.
Vehtari A, Gelman A, Gabry J. Practical Bayesian model evaluation using leave-one-out cross-validation and WAIC. Stat Comput. 2017;27:1413–32.
Arnold BF, Ercumen A, Benjamin-Chung J, Colford JM. Brief report: negative controls to detect selection bias and measurement bias in epidemiologic studies. Epidemiol. 2016;27:637–41.
Lipsitch M, Tchetgen Tchetgen E, Cohen T. Negative controls: a tool for detecting confounding and bias in observational studies. Epidemiol. 2010;21:383–8.
Kruschke JK, Liddell TM. The Bayesian new statistics: hypothesis testing, estimation, meta-analysis, and power analysis from a Bayesian perspective. Psychon Bull Rev. 2018;25:178–206.
Fetters MD, Curry LA, Creswell JW. Achieving integration in mixed methods designs - principles and practices. Health Serv Res. 2013;48:2134–56.
Bishop FL. Using mixed methods research designs in health psychology: an illustrated discussion from a pragmatist perspective. Br J Health Psychol. 2015;20:5–20.
Krueger RA, Casey MA. Focus groups: a practical guide for applied research. New Delhi: SAGE Publications Inc.; 2015.
Guest G, Namey E, McKenna K. How many focus groups are enough? Building an evidence base for nonprobability sample sizes. Field Methods. 2017;29:3–22.
Namey E, Guest G, McKenna K, Chen M. Evaluating bang for the buck: a cost-effectiveness comparison between individual interviews and focus groups based on thematic saturation levels. Am J Eval. 2016;37:425–40.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101.
Skinner CS, Tiro J, Champion VL. The health belief model. In: Glanz K, Rimer BK, Viswanath K, editors. Health behavior and health education: theory, research, and practice. San Francisco: Wiley; 2015.
Atkins L, Francis J, Islam R, O’Connor D, Patey A, Ivers N, et al. A guide to using the Theoretical Domains Framework of behaviour change to investigate implementation problems. Implement Sci. 2017;12:77.
Guetterman TC, Fetters MD, Creswell JW. Integrating quantitative and qualitative results in health science mixed methods research through joint displays. Ann Fam Med. 2015;13:554–61.
Booker CL, Harding S, Benzeval M. A systematic review of the effect of retention methods in population-based cohort studies. BMC Public Health. 2011;11:1–12.
Teague S, Youssef GJ, Macdonald JA, Sciberras E, Shatte A, Fuller-Tyszkiewicz M, et al. Retention strategies in longitudinal cohort studies: a systematic review and meta-analysis. BMC Med Res Methodol. 2018;18:1–22.
Abdelazeem B, Abbas KS, Amin MA, El-Shahat NA, Malik B, Kalantary A, et al. The effectiveness of incentives for research participation: a systematic review and meta-analysis of randomized controlled trials. PLoS One. 2022;17:e0267534.
Kristman V, Manno M, Côté P. Loss to follow-up in cohort studies: how much is too much? Eur J Epidemiol. 2004;19:751–60.
Egorov AI, Griffin SM, Ward HD, Reilly K, Fout GS, Wade TJ. Application of a salivary immunoassay in a prospective community study of waterborne infections. Water Res. 2018;142:289–300.
Egorov AI, Converse R, Griffin SM, Bonasso R, Wickersham L, Klein E, et al. Recreational water exposure and waterborne infections in a prospective salivary antibody study at a Lake Michigan beach. Sci Rep. 2021;11:1–10.
Public Health Agency of Canada. FoodNet Canada annual report 2018. 2019. https://www.canada.ca/en/public-health/services/surveillance/foodnet-canada/publications/foodnet-canada-annual-report-2018.html. Accessed 17 June 2024.
Acknowledgements
We acknowledge the anonymous peer reviewers that provided comments, feedback, and suggestions to earlier iterations of this study in multiple rounds of funding submissions to the CIHR Project Grant competition. We acknowledge and thank all the beachgoers that agreed to participate in the data collection for this study to date. We thank the student data collectors from Toronto Metropolitan University that recruited and surveyed beachgoers at the Toronto site in 2023: Jenice Mun, Mariam Ayub, and Emily Mullen.
Funding
This study protocol was peer reviewed and funded by the Canadian Institutes of Health Research (CIHR), grant numbers PJT 185894 and PJT 192023 (P.I. Young).
Author information
Authors and Affiliations
Contributions
Conceptualization and study methodology: all authors. Data analysis plan: IY, BND, JS, SM, DP, and JT. Drafting of protocol: led by IY with contributions from all other co-authors. All authors reviewed and approved the final version for publication.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study protocol was reviewed and approved by the Toronto Metropolitan University Research Ethics Board (2023–043). Study participants will provide informed consent by completing a digitally submitted form. Assent will be sought from children and youth that do not have capacity to provide informed consent, as long as a parent or guardian is present and provides consent for their participation.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
12889_2024_19889_MOESM2_ESM.docx
Additional file 2. Confounding variables for each model. Confounding variables conceptually and/or empirically related to beach water contact exposure and each of the acute water-borne illness outcomes, and that were determined to be part of the minimal sufficient adjustment set in the directed acyclic graph assessment
12889_2024_19889_MOESM3_ESM.docx
Additional file 3. Power and precision analysis. Simulation parameters, details, and results summary for the Bayesian power and precision analysis of the primary relationship of interest
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Young, I., Desta, B.N., Sanchez, J.J. et al. Canadian beach cohort study: protocol of a prospective study to assess the burden of recreational water illness. BMC Public Health 24, 2502 (2024). https://doi.org/10.1186/s12889-024-19889-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-19889-6