Abstract
Background
There has been a significant increase in the incidence of cardiovascular disease (CVD) in Malaysia. It is important to identify the group at high risk of CVD. This study aimed to assess the population distribution and factors associated with 10-year CVD risk among adults aged 40 to 74 years in Malaysia.
Methods
This study used secondary data from the NHMS 2019, a nationally representative cross-sectional population study. The following measurements were collected: anthropometric, systolic blood pressure, fasting blood glucose, total cholesterol, smoking, and sociodemographic. The 2019 WHO Southeast Asia laboratory-based charts were used to estimate individuals’ CVD risk. These charts predict significant cardiovascular events over ten years. Multiple logistic regression analysis was employed to ascertain the factors that are linked to elevated or extremely elevated risk of CVD.
Results
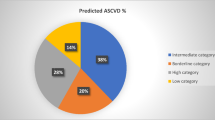
A total of 5,503 respondents were included in the analysis. Less than one-quarter of the respondents were current smokers and obese. Approximately 41.7%, 30.9%, and 22.5% of the participants had extremely low risk (less than 5%), low risk (between 5% and less than 10%), and moderate risk (between 10% and less than 20%), respectively. A total of 4.9% of the participants were categorised as having high (20% to < 30%) or very high (CVD) risk (≥ 30%). This classification was more prevalent among males (7.3%) than among females (2.5%; p < 0.001). The factors associated with high/very high CVD risk were unemployment (aOR = 1.88, 95% CI = 1.47–2.40), those with non-formal and primary education level (aOR = 2.36, 95% CI = 1.36 − 4.12 and aOR = 3.28, 95% CI = 2.10 − 5.12, respectively), and being physically inactive with obesity (aOR = 2.19, 95% CI = 1.18 − 4.08).
Conclusions
This study revealed that almost 5% of the population in Malaysia has a high 10-year CVD risk. These findings highlight Malaysia’s urgent need for comprehensive CVD prevention efforts.
Similar content being viewed by others
Background
Cardiovascular diseases (CVDs), mainly ischaemic heart disease (IHD) and stroke are the foremost causes of worldwide mortality and are significant contributors to disability [1]. In Malaysia, the burden of mortality and morbidity associated with CVD has been on the rise for the past three decades [2]. It was the number one cause of death and contributed approximately 21.65% and 23.79% of all ten principal causes of death in 2018 [3]. The significant risk factors for CVD identified in Malaysia are hypertension, diabetes, high cholesterol levels, and obesity [2,3,4]. An increased incidence of and mortality from CVD has an indirect relationship with modifiable risk factors [3].
The increasing incidence of CVD can be ascribed to the rapid phenomenon of urbanisation, sedentary behaviour adoption, and alterations in dietary habits [5]. CVD-related mortality can be reduced by predicting CVD risk and subsequently reducing CVD risk factors. As part of CVD prevention and control efforts, a reliable risk predictor for identifying high-risk populations is needed.
This approach facilitates the possibility of estimating and monitoring the distribution of CVD risk at the population level, with the goal of informing recommendations for CVD treatment policies [6]. To predict the risk of CVD over a 10-year period, numerous risk prediction models have been developed. The 2019 WHO CVD prediction chart, Framingham, INTERHEART, SCORE, GLOBORISK, and the Pooled Cohort Equation are among the current CVD risk calculators that have been evaluated in various populations [7]. We utilised the 2019 WHO CVD prediction chart for our analysis. This tool leverages comprehensive contemporary estimates of cardiovascular disease incidence and risk factor values to adapt (i.e., recalibrate) the risk models for diverse populations using a simpler and more generalisable approach [8]. Furthermore, the recalibration methodology allows for rapid updates to the CVD models, ensuring flexibility as new epidemiological data emerge for various geographical areas [8]. Notably, this chart provides estimates for 21 regions defined by Global Burden of Disease (GBD), including Malaysia, enhancing the applicability compared to previous WHO charts [6, 8, 9]. We can assess population CVD risk using WHO prediction tables and the total risk approach on a nationally representative sample [6]. The prediction chart can cost-effectively measure total cardiovascular risk using age, sex, diabetes status, smoking status, systolic blood pressure, and total serum cholesterol.
This approach can aid population-level CVD risk management decisions by policymakers. Using 2019 WHO CVD risk prediction tables, we aimed to establish the distribution of absolute CVD risk and the factors associated with high or very high 10-year CVD risk in individuals in Malaysia aged 40–74 years.
Methods
Study design and participants
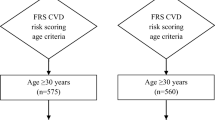
The data were obtained from the National Health and Morbidity Survey (NHMS) 2019, a nationwide cross-sectional, population-based study. A two-stage stratified random sampling method was used to ensure the national representativeness of the population. The primary stratum included all Malaysian states and Federal Territories, and the secondary stratum included urban and rural areas. The National Household Sampling Frame from Statistics Malaysia’s 2010 Population and Housing Census was used. Each secondary stratum was sampled independently. In sample selection, enumeration blocks (EBs) were followed by living quarters (LQs). All the eligible selected LQ households were invited to participate in this survey. The NHMS 2019 methodology was detailed elsewhere [4]. We analysed data from only 40 to 74-year-old adults in this study. Information sheets and consent forms were given to all eligible respondents prior to the interviews. Participant information collected for this study was kept private.
Research instruments and data collection methods
The sociodemographic profile of the respondent, which included age, sex, smoking status, total cholesterol measurements, anthropometric measurements, systolic blood pressure, and fasting blood glucose measurements for diabetic status, was collected during the study. The survey collected data through the use of validated questionnaires. CardioChek® PA was used to measure cholesterol and blood glucose levels via finger prick. Blood pressure was measured in millimeters of mercury (mmHg) using the Omron Digital Automated Blood Pressure Monitor Model HEM-907, which was properly calibrated. The measurements were taken while the participant was in a seated position. The height was measured via a Seca 206 Bodymeter, while weight was assessed utilising a TANITA HD-319 digital weighing machine.
Measurement of outcome variables
These variables were categorised based on the previous literature related to factor associated with CVD risk. A total cholesterol concentration equal or greater than 5.2 mmol/L or a diagnosis of hypercholesterolemia reported by medical personnel were considered hypercholesterolemia [10]. A diagnosis of hypertension was made if the average systolic and diastolic blood pressure was 140 and 90 mmHg or greater or if the respondent was told by medical personnel to have hypertension [4]. Obesity was defined by the WHO as a BMI of 30 kg/m2 or greater. Diabetes was diagnosed if the respondent had fasting capillary blood glucose levels above 7.0 mmol/L or a random blood glucose equal or above 11.1 mmol/L or if the respondent was told by medical personnel to have high glucose [11]. Physical inactivity was assessed using the International Physical Activity Questionnaire (IPAQ) [4]. According to the IPAQ, individuals who do not meet the criteria for Categories 2 or 3 are considered “insufficiently active”. Category 2, or “sufficiently active,” includes individuals who meet any of the following three criteria: engaging in vigorous activity for at least 20 minutes per day on three or more days per week; engaging in moderate-intensity activity or walking for at least 30 minutes per day on five or more days per week; and participating in any combination of walking, moderate-intensity, or vigorous-intensity activities that accumulate at least 600 Metabolic Equivalent of Task (MET)-minutes per week [4]. Meanwhile, Category 3, or “Health Enhancing Physical Activity(HEPA) active” (a more active category), includes individuals who engage in vigorous-intensity activity for a minimum of 1500 MET-minutes per week on at least three days, and participate in any combination of walking, moderate-intensity, or vigorous-intensity activities that accumulate at least 3000 MET-minutes per week [4]. Marital status was categorised into two: married and not married [12, 13]. Meanwhile, education levels were categorised into four groups: non-formal education, primary education, secondary education, and tertiary education [14, 15]. For occupational status, categories were defined as employed and unemployed [16]. For obesity status, individuals were categorised as obese and non-obese [17]. Age, sex, systolic blood pressure, total cholesterol levels, smoking status, and diabetes mellitus status were the variables included in the 2019 WHO CVD prediction chart for the calculation of risk prediction of CVD in 10 years (Attachment 1). Thus, those factors were not included in multiple logistic regression to ascertain factors associated with elevated or extremely elevated risk of cardiovascular diseases.
The 2019 World Health Organisation (WHO) CVD risk prediction charts were used to calculate the estimated 10-year risk of developing CVD. The provided charts depict the projected probability of experiencing a myocardial infarction or stroke, resulting in either fatality or nonfatality, over a period of 10 years. Two charts were generated for each region based on the laboratory findings. The CVD risk of the participants was evaluated using laboratory-based tables for Southeast Asia provided by the World Health Organisation (WHO) in 2019 as shown in Fig. 1. These charts considered various factors, including age, sex, systolic blood pressure, total cholesterol levels, smoking status, and diabetes mellitus status. The combined occurrence of acute myocardial infarction and stroke (both fatal and nonfatal) risk categories over a 10-year period were as follows: less than 5% for the very low-risk category, 5% to less than 10% for the low-risk category, 10% to less than 20% for the moderate risk category, 20% to less than 30% for the high-risk category, and greater than 30% for the highest risk category [6].
The outcome of high-risk CVD was a combination of high and very-high CVD risk (CVD risk categories > 20%) to determine the percentage of the population in Malaysia at high and very high risk for CVD in this paper. Meanwhile, the very low, low and moderate were combined to become non high risk.
Statistical analysis
The data were examined using IBM Statistical Package Social Sciences (SPSS) statistical software version 21. Complex sample analysis, with the addition of poststratification weighting, was employed to analyse the data after adjusting for stratification. The sociodemographic data are presented as proportions for categorical variables. Logistic regression analysis was conducted to identify factors associated with elevated or extremely elevated risk of CVD among adults’ population in Malaysia, with the outcome variable categorised as high risk of CVD and non-high risk of CVD. High risk CVD coded as 1, and low risk of CVD coded as 0. The factor variables include marital status, occupation status, educational level, BMI status and physically inactive. Possible multicollinearity and all possible two-way interaction terms were checked one by one with main effect. We include the interaction term in the final model together with other factors. Goodness-of-fit statistics (a classification table and receiver operating characteristic curve (ROC)) were used to assess model fitness.
Results
Table 1 shows the background characteristics of the adult respondents in Malaysia. Among the 5,503 respondents included in the analysis, the mean age was 55.22 years. The majority of the participants had received formal education (94.3%) and lived in urban areas (78.8%).
Table 2 presents the percentages of CVD risk factors observed among the study population. Approximately 36% of the participants had hypertension, while 55.9% had hypercholesterolaemia.
Table 3 provides a summary of the distribution of CVD risk in the population stratified by sex. Approximately 41.7%, 30.9%, and 22.5% of the participants had extremely low risk (less than 5%), low risk (between 5% and less than 10%), and moderate risk (between 10% and less than 20%), respectively. In the present study, 4.9% of the participants were categorised as having high (20% to < 30%) or very high (CVD) risk (≥ 30%). This classification was more prevalent among males (7.3%) than among females (2.5%; p < 0.001).
Factors associated with 10-year risk for CVD among adults in Malaysia
The factors associated with the 10-year risk of CVD, as determined by a logistic regression model, are detailed in Table 4. The crude logistic regression analysis was first conducted to screen potential variables for inclusion in the adjusted model. Following the results of the crude logistic analysis, all variables were found to be associated with CVD risk and those variables which also deemed important due to biological plausibility were included in the model for the adjusted logistic model. These variables included occupational status, education levels, obesity status, and physical inactivity.
Multicollinearity checks revealed no issues. However, the interaction term between obesity status and physical inactivity showed evidence of association with CVD risk. Therefore, we present our final model, adjusted for marital status, occupational status, education levels, obesity status, physical inactivity, and the interaction term between obesity status and physical inactivity.
Our final model suggests that unemployed individuals may be more likely to develop CVD within the next ten years compared to employed individuals (aOR = 1.88, 95% CI = 1.47 − 2.40). Similarly, individuals with non-formal education and primary education were 2.36 times (95% CI = 1.36 − 4.12) and 3.28 times (95% CI = 2.10 − 5.12) more likely, respectively, to develop CVD within the next ten years compared to those with tertiary education.
Notably, the interaction between obesity and physical inactivity indicates a synergistic effect, as individuals who are both obese and physically inactive have more than double the risk of CVD (aOR = 2.19, 95% CI = 1.18 − 4.08) compared to those who are neither. Initially, obesity appeared to be associated with a lower risk of CVD in the crude analysis, likely due to confounding factors not accounted for. Even in the adjusted model without the interaction term, obesity seemed protective. However, including the interaction between obesity and physical inactivity clarifies that obesity increases the risk of CVD when combined with physical inactivity, aligning with existing knowledge and emphasizing the need to consider both factors together. Therefore, our final model will consider this interaction effect to provide a more accurate understanding of CVD risk in the population.
Discussion
In the present study, utilising a sample from a population that is representative of the entire nation, it was determined that most adults, specifically 72.6%, exhibit a low cardiovascular disease (CVD) risk level, defined as a level less than 10%. According to a study published in the Lancet in 2019, the majority of nations in Southeast Asia exhibit a CVD risk level less than 10% [8]. The prevalence of individuals with minimal CVD risk is comparatively greater in regions such as Central Asia, Eastern Europe, and Oceania than in other regions [8].
It is important to note that 4.9% of the adult population, predicted to be approximately 677,533 individuals by the year 2030, exhibit a high (20% to < 30%) and very high (30%) risk of experiencing a CVD event within the upcoming decade. This risk factor was more prevalent among males (7.3%) than females (2.5%; p < 0.001). According to the 2019 Lancet publication by the WHO CVD Risk Chart Working Group, an analysis of regional data revealed that certain countries within the Southeast Asia region exhibit a nearly 5% probability of experiencing a high (20% to < 30%) or very high (30%) risk of CVD occurrence within the upcoming decade [8]. A study published in The Lancet al. so reported a comparable observation, indicating that the risk of CVD is greater in men than in women. This finding is consistent with other research [6]. Overall, men consistently exhibited greater high-risk CVD risk scores than women did in all comparisons. Compared with women, men in this study had a greater risk of CVD, partially due to a greater percentage of current smokers. Furthermore, the combination of smoking with other risk factors increases CVD risk scores and the likelihood of experiencing CVD events in the near future [7]. Smoking is particularly linked to increased levels of oxidative stress, which renders individuals who smoke more prone to the onset of CVD. The tobacco control programme in the country, in accordance with the WHO Framework Convention on Tobacco Control (WHO FCTC) MPOWER, should be enhanced to effectively decrease the prevalence of current smokers [4].
It was also reported from our study that respondents who were unemployed were approximately twice as likely to develop CVD in the upcoming decade than were those who were employed. This finding is in agreement with a study in which unemployment status was shown to be a risk factor for an acute cardiovascular event [17].
Additionally, the study found that individuals with lower education levels, specifically those with non-formal and primary education, had a 2.36- and 3.28-times higher likelihood, respectively, of developing CVDs compared to those with tertiary education. This finding aligns with previous research that associates lower educational status with increased cardiovascular risk [18, 19]. Lower educational attainment correlates with reduced health literacy, which is essential for understanding and applying public health and preventive CVD recommendations. Improved health literacy promotes healthier behaviours like smoking cessation and adherence to dietary and activity guidelines, reducing healthcare demand and enhancing quality of life [18]. Our study also reported a physical inactivity associated with a risk of having CVDs, as it confers about a 1.44 likelihood of developing CVDs compared with physically active respondents. Physical inactivity exacerbates the impact of other risk factors, such as hypertension, elevated triglyceride levels, diabetes, and obesity. Consequently, this heightened combination of risk factors significantly elevates the likelihood of developing CVD. One study revealed that exercise lowered blood pressure, cholesterol, and triglycerides [20]. The programme should enhance the promotion of physical activity for the public to better comprehend its health benefits and functional capacity enhancement [4]. Moreover, the Wellness Month, a yearly event organised in September by the Ministry of Health in collaboration with interministerial entities, commercial sectors, non-governmental organisations (NGOs), and community involvement, facilitates the government’s mission to foster a healthy population in Malaysia through the promotion of a healthy lifestyle with a whole-of-nation approach [21].
Obesity is a well-known modifiable risk factor for vascular diseases. However, contrary to the widely accepted view of the harmful effects of obesity, several observational studies have reported better outcomes after stroke in obese patients [22,23,24]. Similarly, in both our unadjusted model and the model without the interaction term, obese respondents were less likely to develop CVD compared to non-obese respondents. A systematic review also suggests that observational data indicate a survival benefit for obese patients after stroke, though several methodological concerns have been noted [25]. This phenomenon is referred to as the “obesity paradox,” where, in certain populations, obese individuals appear to have longer lifespans. This paradox has been observed in patients with coronary artery disease [26], heart failure [27], type 2 diabetes, and other conditions [28, 29]. While the exact mechanisms by which obesity might offer protection to individuals with established coronary heart disease (CHD) remain unclear, epidemiological research suggests that changes in body composition associated with obesity could play a role in some of the observed advantages [30]. For instance, non-obese populations may include patients who have lost weight due to more severe illness. Most risk prediction and causation models in epidemiology are based on the additive combination of risk factors within a regression model framework, implying that variables typically act independently unless interaction effects are introduced. Our analysis demonstrates that when the interaction between obesity and physical inactivity is included, the apparent protective effect of obesity disappears, revealing an increased risk of CVD. This suggests that the interaction term captures a complex relationship between these factors, offering a more nuanced understanding of the CVD risk profile in obese individuals. The disappearance of the obesity paradox in the adjusted model with the interaction term indicates that physical inactivity significantly modifies the impact of obesity on CVD risk. This observation is supported by a study showing that individuals who are obese and engage in limited physical activity have a higher risk of CVD than those who maintain normal weight and engage in high levels of physical exercise [31]. In public health campaigns, it is crucial to prioritise the promotion of physical activity among people while also emphasising the importance of managing body weight [31].
There is a pressing necessity to promptly execute efficacious interventions for the targeted population (particularly individuals who are unemployed, those with non-formal and primary education, physically inactive and obese) to mitigate the avoidable burden of cardiovascular diseases in Malaysia. This urgency arises from the projected estimation that approximately 677,533 individuals will be at a high or very high risk of experiencing CVD events within a decade. A comprehensive approach encompassing the identification and mitigation of several risk factors, the promotion of healthy lifestyles, and the enhancement of healthcare systems is necessary. Public health campaigns, affordable screening programmes, and promotion of physical exercise are effective measures that governments can employ to decrease cardiovascular risk. Policy measures should be implemented to promote nutritional education, impose limitations on the advertising of unhealthy food, and facilitate the integration of care. Implementing workplace wellness programmes and specifically targeting interventions towards high-risk populations, such as the unemployed and individuals with lower levels of education, are also of utmost importance.
NCDs have been recognised as the leading factor responsible for 72% of premature mortality cases in Malaysia, with CVD emerging as the dominant contributor to this outcome [32]. According to the Organisation for Economic Cooperation and Development (OECD), premature mortality has severe repercussions for economies, healthcare systems, and families, leading to extensive implications for productivity, equity, and social well-being. This statement emphasises the pressing need for comprehensive initiatives aimed at reducing economic losses, guaranteeing healthcare accessibility, and fostering societal resilience, as highlighted by the World Health Organisation in 2017.
Strengths and limitations
To the best of our knowledge, this study represents an inaugural endeavour in Malaysia to employ the 2019 WHO CVD risk prediction model for the purpose of estimating CVD risk. The present study also utilised a substantial dataset derived from the NHMS 2019, which is a representative sample of the adult population in Malaysia. When assessing our findings, it is crucial to consider the constraints associated with this analytical approach. Models pertaining to the 10-year risk of CVD have been recalibrated by incorporating data from the GBD project, with the aim of ensuring accurate representation of LMICs. Nevertheless, the GBD data lack nation-specific disease risk estimates [6]. Hence, it is probable that the estimation obtained from the chart for each region would be relevant to the largest country within that region or the country from which most of the data are sourced. According to Islam et al. (2020), risk prediction charts provide approximate assessments of CVD risk for persons who do not have a prior history of CHD, stroke, or other atherosclerotic diseases. In addition, the current study was a cross-sectional study; thus, the findings need to be confirmed with a cohort study.
Conclusions
Approximately 5% or 680,000 adults in Malaysia are at high or very high risk of experiencing CVD events, respectively. Individuals who are unemployed, had lower education status, those obese with physically inactive are at higher risk and therefore should be targeted for public health interventions. Reducing cardiovascular risk necessitates a holistic approach involving multiple organisations to identify risk factors, promote healthy lifestyles, and improve healthcare systems. Key strategies include public health campaigns, affordable screenings, exercise promotion, nutritional education, advertising restrictions on unhealthy foods, integrated care, workplace wellness programmes, and targeted interventions for high-risk groups.
Data availability
No datasets were generated or analysed during the current study.
References
World Health Organization. Cardiovascular diseases (CVDs) [https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds).
Firus Khan AY, Ramli AS, Abdul Razak S, Mohd Kasim NA, Chua YA, Ul-Saufie AZ et al. The Malaysian HEalth and WellBeing AssessmenT (MyHEBAT) study protocol: an initiation of a National Registry for Extended Cardiovascular Risk evaluation in the community. Int J Environ Res Public Health. 2022;19(18).
Thangiah N, Su TT, Chinna K, Jalaludin MY, Mohamed MNA, Majid HA. Longitudinal assessment between lifestyle-related risk factors and a composite cardiovascular disease (CVD) risk index among adolescents in Malaysia. Sci Rep. 2021;11(1):19135. https://doi.org/10.1038/s41598-021-98127-0.
Institute for Public Health. National Health and Morbidity Survey (NHMS). 2019: Non-Communicable Diseases, Risk Factors & Other Health Problems. 2019 [http://www.iku.gov.my/images/IKU/Document/REPORT/NHMS2019/4_NCD_Risk_Factors_2019.pdf
World Health Organization. Noncommunicable diseases country profiles 2017: World Health Organization. 2017 [https://www.who.int/nmh/countries/mys_en.pdf
Islam JY, Zaman MM, Moniruzzaman M, Ara Shakoor S, Hossain A. Estimation of total cardiovascular risk using the 2019 WHO CVD prediction charts and comparison of population-level costs based on alternative drug therapy guidelines: a population-based study of adults in Bangladesh. BMJ Open. 2020;10(7):e035842.
Che Nawi CMNH, Omar MA, Keegan T, Yu Y-P, Musa KI. The ten-year risk prediction for Cardiovascular Disease for Malaysian adults using the Laboratory-based and Office-based (Globorisk) Prediction Model. Medicina. 2022;58(5):656.
World Health Organization cardiovascular disease. Risk charts: revised models to estimate risk in 21 global regions. Lancet Glob Health. 2019;7(10):e1332–45.
World Health Organization. HEARTS technical package for cardiovascular disease management in primary health care: risk based CVD management. 2020 [https://iris.who.int/bitstream/handle/10665/333221/9789240001367-eng.pdf?sequence=1
National Cholesterol Education Program (NCEP) Expert Panel on Detection E. Treatment of high blood cholesterol in adults (Adult Treatment Panel III),. Third report of the National Cholesterol Education Program (NCEP) Expert Panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) final report. Circulation. 2002;106(25):3143–421.
American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010;33:e57.
Humbert X, Rabiaza A, Fedrizzi S, Alexandre J, Menotti A, Touzé E et al. Marital status and long-term cardiovascular risk in general population (Gubbio, Italy). Sci Rep. 2023;13(1):6723. https://doi.org/10.1038/s41598-023-33943-0.
Wong CW, Kwok CS, Narain A, Gulati M, Mihalidou AS, Wu P et al. Marital status and risk of cardiovascular diseases: a systematic review and meta-analysis. Heart. 2018;104(23):1937–48. https://doi.org/10.1136/heartjnl-2018-313005. Epub 2018 Jun 19. Erratum in: Heart. 2019;105(14). https://doi.org/10.1136/heartjnl-2018-313005corr1.
Kelli HM, Mehta A, Tahhan AS, Liu C, Kim JH, Dong TA et al. Low educational attainment is a predictor of adverse outcomes in patients with coronary artery disease. J Am Heart Assoc. 2019;8(17). https://doi.org/10.1161/JAHA.119.013165. Epub 2019 Sep 2.
Kubota Y, Heiss G, MacLehose RF, Roetker NS, Folsom AR. Association of Educational Attainment with Lifetime Risk of Cardiovascular Disease: the atherosclerosis risk in communities Study. JAMA Intern Med. 2017;177(8):1165–72.
Meneton P, Kesse-Guyot E, Méjean C, Fezeu L, Galan P, Hercberg S, Ménard J. Unemployment is associated with high cardiovascular event rate and increased all-cause mortality in middle-aged socially privileged individuals. Int Arch Occup Environ Health. 2015;88(6):707–16.
Held C, Hadziosmanovic N, Aylward PE, Hagström E, Hochman JS, Stewart RAH, et al. Body Mass Index and Association with Cardiovascular outcomes in patients with stable Coronary Heart Disease – A STABILITY Substudy. J Am Heart Association. 2022;11(3):e023667.
Khan N, Javed Z, Acquah I, Hagan K, Khan M, Valero-Elizondo J, et al. Low educational attainment is associated with higher all-cause and cardiovascular mortality in the United States adult population. BMC Public Health. 2023;23(1):900.
Magnani JW, Ning H, Wilkins JT, Lloyd-Jones DM, Allen NB. Educational Attainment and Lifetime Risk of Cardiovascular Disease. JAMA Cardiol. 2024;9(1):45–54.
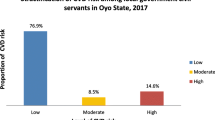
Babatunde OA, Olarewaju SO, Adeomi AA, Akande JO, Bashorun A, Umeokonkwo CD, Bamidele JO. 10-year risk for cardiovascular diseases using WHO prediction chart: findings from the civil servants in South-western Nigeria. BMC Cardiovasc Disord. 2020;20(1):154.
Health Education Division MoHM. Bulan Malaysia Sihat Sejahtera (Wellness Month) [https://www.infosihat.gov.my/bulan-malaysia-sihat-sejahtera-wellness-month.html
Kim BJ, Lee SH, Jung KH, Yu KH, Lee BC, Roh JK, For Korean Stroke Registry investigators. Dynamics of obesity paradox after stroke, related to time from onset, age, and causes of death. Neurol. 2012;79(9):856–63. https://doi.org/10.1212/WNL.0b013e318266fad1.
Vemmos K, Ntaios G, Spengos K, Savvari P, Vemmou A, Pappa T et al. Association between obesity and mortality after acute first-ever stroke: the obesity-stroke paradox. Stroke. 2011;42(1):30–6. https://doi.org/10.1161/STROKEAHA.110.593434. Epub 2010 Dec 2. PMID: 21127299.
Wohlfahrt P, Nordestgaard BG, Munthe-Kaas MC et al. The obesity paradox and survivors of ischemic stroke. J Stroke Cerebrovasc Dis. 2015;24(6):1443–50.
Barba R, Marco J, Ruiz J, Canora J, Hinojosa J, Plaza S, Zapatero-Gaviria A. The obesity paradox in stroke: impact on mortality and short-term readmission. J Stroke Cerebrovasc Dis. 2015 Apr;24(4):766–70. https://doi.org/10.1016/j.jstrokecerebrovasdis.2014.11.002.
Romero-Corral A, Montori VM, Somers VK, Korinek J, Thomas RJ, Allison TG et al. Association of bodyweight with total mortality and with cardiovascular events in coronary artery disease: a systematic review of cohort studies. Lancet. 2006;368(9536):666–78. https://doi.org/10.1016/S0140-6736(06)69251-9. PMID: 16920472.
Oreopoulos A, Padwal R, Kalantar-Zadeh K, Fonarow GC, Norris CM, McAlister FA. Body mass index and mortality in heart failure: a meta-analysis. Am Heart J. 2008;156(1):13–22. https://doi.org/10.1016/j.ahj.2008.02.014. PMID: 18585492.
Carnethon MR, De Chavez PJ, Biggs ML, Lewis CE, Pankow JS, Bertoni AG et al. Association of weight status with mortality in adults with incident diabetes. JAMA. 2012;308(6):581–90. https://doi.org/10.1001/jama.2012.9282. Erratum in: JAMA. 2012;308(20):2085.
Zhao W, Katzmarzyk PT, Horswell R, Wang Y, Li W, Johnson J, et al. Body Mass Index and the risk of all-cause mortality among patients with type 2 diabetes Mellitus. Circulation. 2014;130(24):2143–51.
Carbone S, Canada JM, Billingsley HE, Siddiqui MS, Elagizi A, Lavie CJ. Obesity paradox in cardiovascular disease: where do we stand? Vasc Health Risk Manag. 2019;15:89–100.
Koolhaas CM, Dhana K, Schoufour JD, Ikram MA, Kavousi M, Franco OH. Impact of physical activity on the association of overweight and obesity with cardiovascular disease: the Rotterdam Study. Eur J Prev Cardiol. 2017;24(9):934–41.
Khaw WF, Chan Y, Nasaruddin NH, et al. Malaysian burden of disease: years of life lost due to premature deaths. BMC Public Health. 2023;23:1383. https://doi.org/10.1186/s12889-023-16309-z.
Acknowledgements
We would like to thank the Director General of Health Malaysia for his permission to publish this article.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
H.M.R. contributed to the conceptualisation, methodology, visualisation, original draft writing, and final manuscript review and editing. K.S.W. contributed to the conceptualisation, methodology, and review and editing of the final manuscript. M.A.O. contributed to the conceptualisation, methodology, analysis, supervision, and review and editing of the final manuscript. W.S.R.H. contributed to the analysis, review and editing of the final manuscript. All the authors contributed to the article and approved the submitted version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All participants provided written informed consent prior to the interviews. All data were anonymised before being used in this study. For participants who were illiterate, informed consent was obtained from their legal guardians or representatives. Thumbprint impressions were taken from the participants, with a literate person acting as a witness. The survey protocol was approved by the Medical Research and Ethics Committee (MREC), Ministry of Health Malaysia (NMRR-18-3085-44207(IIR)).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Rifin, H.M., Omar, M.A., Wan, K.S. et al. 10-year risk for cardiovascular diseases according to the WHO prediction chart: findings from the National Health and Morbidity Survey (NHMS) 2019. BMC Public Health 24, 2513 (2024). https://doi.org/10.1186/s12889-024-19993-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-19993-7