Abstract
Background
Bronchial artery embolization (BAE) is currently an important treatment for hemoptysis. However, there is no consensus in the efficacy and safety of BAE compared to conservative treatment for hemoptysis, which limits the widespread use of BAE in hemoptysis. The objective was to assess the clinical benefit of BAE versus conservative treatment in patients with hemoptysis.
Methods
A systematic search was conducted on the PubMed, Embase, ScienceDirect, CochraneLibrary, and ClinicalTrials up to March 2023. Both randomized controlled trials (RCTs) and cohort studies reporting rates of recurrent hemoptysis, clinical success, mortality, and complication by BAE and conservative treatment alone for hemoptysis were included. Data were pooled and compared by the use of odds ratio (OR) and 95% confidence interval (CI).
Results
Twelve studies (three RCTs, nine cohorts) involving 1231 patients met the eligibility criteria. Patients treated with BAE had lower recurrence rates of hemoptysis (26.5% vs. 34.6%; OR 0.37, 95% CI 0.14–0.98), higher clinical success rates (92.2% vs. 80.9%; OR 2.77, 95% CI 1.66–4.61), and lower hemoptysis-related mortality (0.8% vs. 3.2%; OR 0.20, 95% CI 0.05–0.84) compared with conservative treatment alone. There was no significant difference in all-cause mortality between the two groups. In terms of security, the incidence of major complications and minor complications in patients undergoing BAE treatment was 0.2% (1/422) and 15.6%, respectively.
Conclusions
BAE was more effective than conservative treatment alone in controlling hemoptysis, reducing recurrence, and decreasing hemoptysis-related mortality, with an almost negligible risk of major complications.
Similar content being viewed by others
Introduction
Hemoptysis is a life-threatening respiratory emergency that requires prompt investigation and management. At present, the treatment of hemoptysis mainly includes conservative treatment (including bronchoscopy), endovascular treatment and surgery.
Conservative treatment includes monitoring, oxygen therapy, postural drainage, the administration of antibiotics or hemostatic drugs, and the use of bronchoscope. It is mainly suitable for mild to moderate hemoptysis [1], which has the advantages of availability and convenience. However, the effect of conservative treatment on hemoptysis varies from person to person, and the risk of recurrence is high [2].
Surgery was once regarded as the first-line treatment of hemoptysis, however, the status of emergency surgery has gradually declined because of high operative mortality rates. With the improvements of interventional radiology, nowadays, bronchial artery embolization (BAE) has been the first-line treatment of massive and recurrent hemoptysis [2,3,4]. Also, a survey by the American College of Chest Physicians showed that a higher proportion of chest physicians favored interventional radiology over either conservative or surgical management [5].
Although the status of BAE seems to be higher than conservative treatment, there is lack of strong evidence from randomized trials. In the available observational studies [6,7,8], there is heterogeneity in the efficacy and safety of BAE compared to conservative treatment for hemoptysis, which limits the widespread use of BAE in hemoptysis. Therefore, we conducted this systematic review and meta-analysis. At present, there is no meta-analysis on comparing the efficacy and safety of BAE and conservative treatment for hemoptysis.
Materials and methods
This study is reported under the Preferred Reporting Items for Systematic Evaluation and Meta-Analysis (PRISMA) Statement [9] and is registered with PROSPERO9 (https://www.crd.york.ac.uk/PROSPERO) (registration number CRD42024548571).
Search strategy and study selection
To report this meta-analysis, we followed the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines. A systematic search was performed in electronic databases (PubMed, Embase, ScienceDirect, CochraneLibrary, and ClinicalTrials) up to March 2023 to identify all available studies on BAE vs. conservative treatment for hemoptysis. The following search terms were used (as medical subject headings and text words): (Bronchial artery embolization [Title/Abstract]) AND (("Hemoptysis" [Mesh]) OR ((haemoptysis [Title/Abstract]) OR (Hemoptyses [Title/Abstract]))). Two independent authors (S.F. and X.C.) independently analyzed the lists of retrieved articles and performed the study selection. Disagreement was resolved by consensus or opinion of a third author (W.H.) if necessary. The Institutional Review Board approval or exemption was not necessary for this study due to the lack of original human and animal information.
Inclusion and exclusion criteria
Studies were included in the analysis in the presence of all the following criteria: (1) original study is in English; (2) the design of two-arms which have both BAE group and conservative treatment group; (3) follow-up data was complete; (4) availability of data on the incidence of recurrent hemoptysis, clinical success, mortality, major complications, and minor complications; (5) publication after 1985.
Studies were excluded if they met any one of the criteria as follows: (1) review article, systematic review, meta-analysis, comment, discussion, editorial, letter, book, case report, animal experiment, conference paper, and guideline; (2) duplicate articles reporting the same data; (3) the BAE and control groups in the study were not conducted during the same period of time; (4) studies without prognostic and survival data; (5) full-texts were not retrieved, and attempts to contact the author failed.
Data extraction
All original articles selected for inclusion in the meta-analysis were independently reviewed by two authors (S.F. and X.C.), and the following data were extracted, when available: general data (author, year of publication, study type), population characteristics (inclusion criteria, exclusion criteria, number of included patients, etiology and severity of hemoptysis), intervention of the BAE treatment group (including embolic material) and conservative treatment group, and duration of follow up. For patients in the BAE and conservative treatment groups, information on the following separate outcomes were collected: details of recurrence, clinical success, hemoptysis-related mortality, all-cause mortality, major complications, and minor complications. Disagreements between reviewers were resolved by consensus or by discussion with a third reviewer (W.H.).
Assessment of quality and risk of bias
The Cochrane Risk of Bias Tool (RoB) was used to evaluate the quality of randomized controlled trials (RCTs) [10]. We rated the overall risk of bias as “low”, “high”, or “unclear” risk of bias according to the different domains. The Newcastle–Ottawa Scale (NOS) was used to assess the quality of cohort studies [11]. The full score was 9, with 0–4 being low quality, 5–6 being moderate quality, and 7–9 being high quality. Two reviewers (S.F. and X.C.) assessed independently, and discrepancies were solved by discussion among all review authors.
Publication bias was assessed with Egger’s test and represented graphically by funnel plots of the standard difference in means versus the standard error.
Outcomes
The primary outcome of this meta-analysis is recurrent hemoptysis, defined as post-BAE recurrence of hemoptysis requiring readmission, repeat BAE, or lobectomy during follow-up. The secondary outcomes included clinical success, hemoptysis-related mortality, all-cause mortality, major complications and minor complications. Clinical success is defined as the combination of cessation or reduction of hemoptysis during study period. Major complications are defined as unplanned sequelae that may require medical intervention during hospitalization or even death, such as spinal injury, severe diaphragmatic palsy, and other unexpected systematic artery embolization. Minor complications are mild self-limiting symptoms which are relieved by symptomatic treatment or rest, such as fever, back pain, dysphagia, etc. The original data were verified twice.
Statistical analysis
Data were analyzed using Mantel–Haenszel statistics. The odds ratio (OR) and 95% confidence interval (CI) were calculated for each study, and results were compared by the use of a fixed-effects (FE) model or a random-effects (RE) model. A P-value of < 0.05 was considered to be statistically significant. Between-study heterogeneity was determined based on the following: (1) a significant Q test of heterogeneity, (2) an I2 test > 60%, and (3) visual inspection of the forest plot.
When the heterogeneity was significant, subgroup analysis, sensitivity analysis and meta-regression were used to find the source of heterogeneity. Subgroup analysis was performed according to the study type (randomized controlled trial or cohort study). The effect on the outcome was explored using sensitivity analysis by eliminating studies that were at a high risk of bias. Meta-regression was used according to the study type, disease and nation to analyze the source of heterogeneity.
Analyses were performed with REVIEW MANAGER 5.4 (The Cochrane Collaboration, Oxford, UK) and STATA/MP17 (StataCorp LP, College Station, TX, USA).
Results
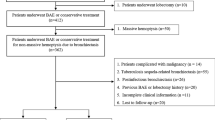
We identified 1534 articles from our initial search strategy and 1203 articles remained after removal of duplicates, of which 1055 were in the English language. Review article (n = 80), systematic review/meta-analysis (n = 2), ongoing study (n = 6), animal experiment (n = 2), conference abstract (n = 146), guideline (n = 3), comment/editorial/letter/book (n = 45), case series (n = 39) and case report (n = 351) were excluded. After scanning the title and/or abstract, 350 articles were excluded (7 of them have no full text). Full-text versions of the remaining relevant articles (n = 31) were assessed for eligibility, and 19 articles were excluded after applying the inclusion/exclusion criteria. Finally, a total of 12 articles were included for the systematic review. The flow chart of the selection process is shown in Fig. 1.
Baseline characteristics of included studies
Twelve studies that included a total of 1231 patients were included. Table 1 provides basic summaries of these studies. Published between 2002 and 2023, these studies reported that patients with hemoptysis received BAE or conservative treatment due to the diverse etiologies of cystic fibrosis, lung cancer, tuberculosis (TB), nontuberculous mycobacteria (NTM), bronchiectasis, chronic thromboembolic pulmonary hypertension (CTEPH), etc. 8 studies were used to pool the data of the recurrent rate of hemoptysis, while 7 studies were used for the evaluation of clinical success. We also respectively evaluated 7 studies and 5 studies to estimate all-cause mortality and hemoptysis-related mortality. Finally, we analyzed major and minor complications secondary to BAE to evaluate its safety.
Risk of bias and quality of evidence
The RoB was used to assess the quality of 3 RCTs [2, 13, 17] (Fig. 2). The results showed that the included articles were of moderate quality. The NOS was used to assess the quality of 9 cohort studies [6,7,8, 12, 14,15,16, 18, 19] (Table 2). The average NOS score of cohort studies was 6.5 (ranging from 4 to 9).
Outcome
Results for each outcome are shown in Table 3 and are also described below.
Primary outcome
Eight studies reported on the rates of recurrent hemoptysis. The pooled analysis of these studies confirmed that the recurrence rate in the BAE group is lower than that in the control group (904 patients; 26.5% versus 34.6%; RE model, OR 0.37, 95% CI 0.14–0.98, I2 = 84%) (Fig. 3a).
Recurrent hemoptysis in patients receiving BAE treatment or conservative treatment according to study design. a Forest plot before sensitivity analysis. b Forest plot after sensitivity analysis. c Sensitivity analysis. d Funnel plot. BAE, bronchial artery embolization; CI, confidence interval; df, degrees of freedom; M-H, Mantel–Haenszel; RCT, randomized controlled trial
Due to the great heterogeneity, subgroup analysis, sensitivity analysis and meta-regression were performed. Subgroup analysis (Fig. 3a) showed that there was no significant difference (χ2 = 0.89, P = 0.35, I2 = 0%) in the rate of recurrent hemoptysis between RCTs (1 studies, 72 patients; RE model, OR 0.19, 95% CI 0.06–0.60) and cohort studies (7 studies, 832 patients; RE model, OR 0.41, 95% CI 0.14–1.20, I2 = 85%). Sensitivity analysis (Fig. 3c) showed that two studies (choi 2018 and Lu 2022) had a significant impact on the effect size. After removing these two studies, the result of pooled analysis remained robust without significant heterogeneity (509 patients; 23.7% versus 38.6%; FE model, OR 0.41, 95% CI 0.27–0.62, I2 = 33%) (Fig. 3b). There was no significant difference in meta-regression according to nation (P = 0.95) and study type (P = 0.24). Reporting bias was not evident (P = 0.30, Egger test) as presented by funnel plot (Fig. 3d).
Secondary outcomes
Clinical success
The pooled analysis of 7 studies reporting comparisons between BAE and conservative treatment showed a significant increase in the rate of clinical success in patients receiving BAE as compared with controls (676 patients; 92.2% versus 80.9%; FE model, OR 2.77, 95% CI 1.66–4.61, I2 = 12%) (Fig. 4a).
In addition, subgroup analysis (Fig. 4a) of these 7 studies was performed through study type, and there was insignificant difference (χ2 = 4.00, P = 0.05, I2 = 75.0%) in the rate of clinical success between RCTs (3 studies, 276 patients; FE model, OR 4.14, 95% CI 2.14–8.01, I2 = 0%) and cohort studies (4 studies, 400 patients; FE model, OR 1.39, 95% CI 0.60–3.22, I2 = 20%). Not much impact on effect size was observed during sensitivity analysis (Fig. 4b). Also, there was no significant difference in meta-regression according to nation (P = 0.99) and study type (P = 0.25). Reporting bias was not evident (P = 0.28, Egger test), as the funnel plot was symmetric (Fig. 4c).
Hemoptysis-related mortality
Five cohort studies reported on number of hemoptysis-related mortality. The odds in the BAE group for hemoptysis-related mortality was 0.20 times the odds in the control group (497 patients; 0.8% versus 3.2%; FE model, OR 0.20, 95% CI 0.05–0.84, I2 = 10%) (Fig. 5a). Because of the small number of studies and inapparent heterogeneity, subgroup analysis, sensitivity analysis and meta-regression were not performed. Reporting bias was not evident (P = 0.74, Egger test) as presented by funnel plot (Fig. 5b).
All-cause mortality
Seven cohort studies reported on the incidences of all-cause mortality. The odds in the BAE group for all-cause mortality was 0.70 times the odds in the control group (649 patients; 4.3% versus 7.6%; FE model, OR 0.70, 95% CI 0.32–1.56, I2 = 55%), but results were statistically insignificant (Fig. 6a).
All-cause mortality in patients receiving BAE treatment or conservative treatment according to study design. a Forest plot before sensitivity analysis. b Forest plot after sensitivity analysis. c Sensitivity analysis. d Funnel plot. BAE, bronchial artery embolization; CI, confidence interval; df, degrees of freedom; M-H, Mantel–Haenszel
Due to the heterogeneity among groups, sensitivity analysis was performed, which showed that one study (Vidal 2006) had a significant impact on the effect size (Fig. 6c). After removing this study, the result of pooled analysis confirmed that the all-cause mortality in the BAE group was significantly lower than that in the control group (592 patients; 1.6% versus 7.3%; FE model, OR 0.29, 95% CI 0.09–0.93, I2 = 8%) (Fig. 6b). Reporting bias was not evident (P = 0.18, Egger test) as presented by funnel plot (Fig. 6d).
Complication
Nine studies reported the complications after BAE. Of all the 422 patients, only one had major complications, manifested as spinal cord ischemia with splenic, renal and pancreatic infarction. Sixty-six of 422 patients had minor complications, of which chest pain was the most common. The major and minor complications are listed in Table 4.
Discussion
In this study, we evaluated the efficacy and safety of BAE and conservative treatment for hemoptysis. Overall, patients treated with BAE had lower recurrence rates of hemoptysis (26.5% vs. 34.6%; OR 0.37, 95% CI 0.14–0.98), higher clinical success rates (92.2% vs. 80.9%; OR 2.77, 95% CI 1.66–4.61), and lower hemoptysis-related mortality (0.8% vs. 3.2%; OR 0.20, 95% CI 0.05–0.84) compared with conservative treatment alone. In terms of security, the incidence of major complications in patients undergoing BAE treatment remained negligible (1/518), and the incidence of minor complications was 12.7%.
Recurrence after BAE remains an inevitable problem and occurs in approximately 30% of patients [20,21,22]. In our study, the recurrence rate in the BAE group was 26.5%, compared with 34.6% in the control group. We excluded two study by Choi et al. [8] and Lu et al. [6] due to significant heterogeneity. In the study by Choi et al. [8], the proportion of patients with active bleeding in the BAE group was higher, about 10 times that of the control group, which may be an important reason for the high recurrence. Lu et al. [6] indicated that the cystic type of bronchiectasis was a risk factor for the recurrence of hemoptysis. In his study, the proportion of patients with cystic type in the control group was about twice that of the BAE group, which may have increased the recurrence rate. After excluding these two studies, the recurrence rate in the BAE group was 23.7%, which is consistent with the results of a previous single-arm meta-analysis (recurrence rate in the BAE group was 23.7%; 95% CI: 18.5%-28.9%) [23]. Hemoptysis recurrences mostly occur in lung cancer, mycetoma or cavitary lesions, and may be related to incomplete embolization, recanalization of previously embolized arteries, as well as to the recruitment of new collaterals due to the progression of the underlying disease [24,25,26]. Other studies [20, 27, 28] have shown that tuberculosis sequelae, bronchial-pulmonary shunts, aberrant bronchial artery, non-bronchial systemic collaterals are also independent risk factors for recurrence after BAE treatment. For patients with the above risk factors, long-term comprehensive management is still required after successful hemostasis. If hemoptysis recurs, repeated BAE or even surgery may be necessary.
In our study, the clinical success rate in the BAE group was significantly higher than that in the control group (92.2% versus 80.9%). However, compared with the result of a previous meta-analysis by Zheng et al. [23], the clinical success rate in our study was lower (92.2% versus 99.5%). Different from the design of Zheng et al., our study defined clinical success as the cessation or reduction of hemoptysis throughout the study period, while they thought that clinical success (“immediate success” in their article) refers to the absence of bleeding within 24 h post-BAE. The longer the observation of clinical outcome, the lower the probability of clinical success. Therefore, this may be the reason for the lower rate of clinical success after BAE treatment in our study. Mild or moderate hemoptysis can often be managed by conservative treatment of the underlying pathology. For massive hemoptysis or recurrent hemoptysis, BAE is required because conservative treatment has little effect. If the hemoptysis continues after BAE, aberrant bronchial arteries or nonbronchial systemic arteries should be excluded as bleeding source [1, 29]. If still no bleeding site is found, the pulmonary arterial circulation has to be investigated [30].
In our study, the all-cause mortality in the BAE group was 4.3%, compared with 7.6% in the control group. We excluded one study by Vidal et al. [16] due to significant heterogeneity. In this study, two variables were unbalanced between groups at the time of embolization or matching, with greater prevalences in the BAE group of oxygen dependence (40.0% vs. 22.2%; P = 0.17) and multidrug-resistant Pseudomonas species infection (56.7% vs. 29.6%; P = 0.06) [16]. The poor baseline conditions may be a major contributor to the higher all-cause mortality in the BAE group. After excluding this study, the all-cause mortality in the BAE group was 1.6%, which was consistent with the results of a previous single-arm meta-analysis (mortality rate in the BAE group was 2%; 95% CI: 0–3%) [23]. The hemoptysis-related mortality rate in the BAE group was significantly lower than that in the control group (0.8% versus 3.2%), which further demonstrates that BAE is effective in controlling bleeding and reducing recurrence.
The incidence of complication after BAE in our study was 15.9%, which is similar to the results by Zheng et al. (13.4%; 95% CI: 7.6–19.2%). Only one patient (1/422) in our study had major complication, manifested as spinal cord ischemia with splenic, renal and pancreatic infarction. Although this patient had a favorable outcome, it should be noted that guiding the procedure with imaging, specifically multidetector computed tomography angiography (MDCTA), and the use of modern ionic contrast media and superselective catheterization of bronchial arteries are essential to decrease the rate of complications related to the procedure [2, 24, 31, 32]. The incidence of minor complications was 15.6% (66/422), as mentioned in the literatures [1, 29, 33], chest pain is the most common complication after BAE. Although minor complications such as chest pain, fever and dysphagia occurred often after BAE, these events were easily controlled with medical treatment and did not compromise the clinical outcomes [16, 18].
Strengths and limitations
It should be considered that a meta-analysis has inherent weaknesses, owing to the combination of heterogenous datasets. There were differences between the studies in terms of etiology (bronchiectasis, cystic fibrosis, tuberculosis, etc.), severity of hemoptysis (mild hemoptysis, massive hemoptysis, etc.) and therapeutic measures (hemostatic agents, antibiotics, embolic materials, etc.). In addition, definitions of clinical outcome were also inconsistent in some studies. For example, some studies defined the recurrence of hemoptysis as a hemoptysis event that required admission, whereas other studies provided different definitions, such as any hemoptysis or an event that required another BAE. Second, the low methodological quality of the included studies overall could have influenced the results of the analysis. Most of the studies are small-sample single-center retrospective investigations, and only a few randomized controlled studies have been included. Third, there were also heterogeneities within some studies, such as differences in the etiology and severity of hemoptysis among patients in the same cohort. There were also some differences in baseline characteristics between the BAE and conservative treatment groups. Therefore, high-quality prospective multicenter randomized controlled trials are needed to validate our findings in the future.
Conclusion
In brief, our meta-analysis shows that BAE is superior to conservative treatment alone in controlling hemoptysis, reducing recurrence, and decreasing hemoptysis-related mortality, with an almost negligible risk of major complications. The small number of participants and low strength of evidence in this meta-analysis suggests more studies especially randomized controlled trials regarding the treatment of hemoptysis is needed.
Availability of data and materials
All data generated or analyzed during this study are included in this published article and its supplementary information files.
Abbreviations
- 95% CI:
-
95% Confidence interval
- BAE:
-
Bronchial artery embolization
- CT:
-
Computed tomography
- CTEPH:
-
Chronic thromboembolic pulmonary hypertension
- Df:
-
Degrees of freedom
- ICU:
-
Intensive care unit
- ICW:
-
Intermediate care ward
- MDCTA:
-
Multidetector CT-angiography
- M-H:
-
Mantel-Haenszel
- NA:
-
Not available
- NTM:
-
Nontuberculous mycobacteria
- OR:
-
Odds ratio
- PH:
-
Pulmonary hypertension
- PVA:
-
Polyvinyl alcohol
- RCT:
-
Randomized controlled trial
References
Ittrich H, Bockhorn M, Klose H, Simon M. The Diagnosis and Treatment of Hemoptysis. Dtsch Arztebl Int. 2017;114(21):371–81.
Fartoukh MDAS, Simon T. Randomised trial of first-line bronchial artery embolisation for non-severe haemoptysis of mild abundance. Bmj Open Respir Res. 2021;8(1):e000949.
Davidson K, Shojaee S. Managing massive hemoptysis. Chest. 2020;157(1):77–88.
Ramírez MA, Méndez MJ, Vásquez-Caicedo ML, Bustos GDCA, Cabeza MB, Ferreirós DJ. Radiological evaluation and endovascular treatment of hemoptysis. Curr Probl Diagn Rad. 2016;45(3):215–24.
Haponik EF, Fein A, Chin R. Managing life-threatening hemoptysis: has anything really changed? Chest. 2000;118(5):1431–5.
Lu GD, Yan HT, Zhang JX, Liu S, Shi HB, Zu QQ. Bronchial artery embolization for the management of frequent hemoptysis caused by bronchiectasis. Bmc Pulm Med. 2022;22(1):394.
Lee SH, Lee JH, Chang JH, Kim SJ, Yoon HY, Shim SS, Kim MU, Choi SY, Ryu YJ. Hemoptysis requiring bronchial artery embolization in patients with nontuberculous mycobacterial lung disease. Bmc Pulm Med. 2019;19(1):117.
Choi J, Baik JH, Kim CH, Song SH, Kim SK, Kim M, Yun S. Long-term outcomes and prognostic factors in patients with mild hemoptysis. Am J Emerg Med. 2018;36(7):1160–5.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. Bmj-Brit Med J. 2009;339: b2700.
Cumpston M, Li T, Page MJ, Chandler J, Welch VA, Higgins JP, Thomas J. Updated guidance for trusted systematic reviews: a new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Db Syst Rev. 2019;10(10):ED000142.
Zeng X, Zhang Y, Kwong JS, Zhang C, Li S, Sun F, Niu Y, Du L. The methodological quality assessment tools for preclinical and clinical studies, systematic review and meta-analysis, and clinical practice guideline: a systematic review. J Evid-Based Med. 2015;8(1):2–10.
Antonelli M, Midulla F, Tancredi G, Salvatori FM, Bonci E, Cimino G, Flaishman I. Bronchial artery embolization for the management of nonmassive hemoptysis in cystic fibrosis. Chest. 2002;121(3):796–801.
Huang Y, Liang H, Yang Z, Liu H, Xu J, Huang Y, Huang Q, Ni G, Ni Y. Effect evaluation of bronchial artery embolization for hemoptysis of lung cancer and changes in serum tumor markers and miR-34 Levels. Contrast Media Mol. 2022;I(2022):2471039.
Reechaipichitkul W, Latong S. Etiology and treatment outcomes of massive hemoptysis. Se Asian J Trop Med. 2005;36(2):474–80.
Savale L, Parrot A, Khalil A, Antoine M, Théodore J, Carette MF, Mayaud C, Fartoukh M. Cryptogenic hemoptysis: from a benign to a life-threatening pathologic vascular condition. Am J Resp Crit Care. 2007;175(11):1181–5.
Vidal V, Therasse E, Berthiaume Y, Bommart S, Giroux MF, Oliva VL, Abrahamowicz M, du Berger R, Jeanneret A, Soulez G. Bronchial artery embolization in adults with cystic fibrosis: impact on the clinical course and survival. J Vasc Interv Radiol. 2006;17(6):953–8.
Xu PXYC, Sun P. Tuberculosis involved the lung field ≥3, pulmonary fungal infection and embolization granules were high-risk factors for short-term rebleeding after bronchial artery embolization. Acta Medica Mediterr. 2020;36(1):667–72.
Yan HT, Lu GD, Zhang JX, Zhou CG, Liu J, Liu S, Shi HB, Zu QQ. Comparison of bronchial artery Embolisation versus conservative treatment for bronchiectasis-related Nonmassive Haemoptysis: a single-Centre retrospective study. Cardiovasc Inter Rad. 2023;46(3):369–76.
Yang S, Wang J, Kuang T, Gong J, Ma Z, Shen YH, Liang L, Yang Y, Huang K. Efficacy and safety of bronchial artery embolization on hemoptysis in chronic thromboembolic pulmonary hypertension: a pilot prospective cohort study. Crit Care Med. 2019;47(3):e182–9.
Hwang JH, Kim JH, Park S, Lee KH, Park SH. Feasibility and outcomes of bronchial artery embolization in patients with non-massive hemoptysis. Resp Res. 2021;22(1):221.
Kato A, Kudo S, Matsumoto K, Fukahori T, Shimizu T, Uchino A, Hayashi S. Bronchial artery embolization for hemoptysis due to benign diseases: immediate and long-term results. Cardiovasc Inter Rad. 2000;23(5):351–7.
Lu GD, Zhang JX, Zhou CG, Xia JG, Liu S, Zu QQ, Shi HB. Arterial embolization for hemoptysis in patients with chronic pulmonary tuberculosis and in patients with bronchiectasis. Acta Radiol. 2019;60(7):866–72.
Zheng Z, Zhuang Z, Yang M, Luo J, Zhang W, Yan Z, Wang X. Bronchial artery embolization for hemoptysis: a systematic review and meta-analysis. J Interv Med. 2021;4(4):172–80.
Panda A, Bhalla AS, Goyal A. Bronchial artery embolization in hemoptysis: a systematic review. Diagn Interv Radiol. 2017;23(4):307–17.
Chun JY, Morgan R, Belli AM. Radiological management of hemoptysis: a comprehensive review of diagnostic imaging and bronchial arterial embolization. Cardiovasc Inter Rad. 2010;33(2):240–50.
Maleux G, Matton T, Laenen A, Bonne L, Cornelissen S, Dupont L. Safety and efficacy of repeat embolization for recurrent hemoptysis: A 16-Year Retrospective Study Including 223 Patients. J Vasc Interv Radiol. 2018;29(4):502–9.
Zhang CJ, Jiang FM, Zuo ZJ, Li SS, Zhao YA, Li PJ, Ye DF, Zhang LL, Tong LH, Chen SL, et al. Clinical characteristics and postoperative outcomes of systemic artery-to-pulmonary vessel fistula in hemoptysis patients. Eur Radiol. 2022;32(6):4304–13.
Xu S, Guan LJ, Shi BQ, Tan YS, Zhang XJ. Recurrent Hemoptysis after bronchial artery embolization: prediction using a nomogram and artificial neural network model. Am J Roentgenol. 2020;215(6):1490–8.
Yoon W, Kim JK, Kim YH, Chung TW, Kang HK. Bronchial and nonbronchial systemic artery embolization for life-threatening hemoptysis: a comprehensive review. Radiographics. 2002;22(6):1395–409.
Ferris EJ. Pulmonary hemorrhage. Vascular evaluation and interventional therapy. Chest. 1981;80(6):710–4.
Monroe EJ, Pierce DB, Ingraham CR, Johnson GE, Shivaram GM, Valji K. An Interventionalist’s Guide to Hemoptysis in Cystic Fibrosis. Radiographics. 2018;38(2):624–41.
Khalil A, Fartoukh M, Bazot M, Parrot A, Marsault C, Carette MF. Systemic arterial embolization in patients with hemoptysis: initial experience with ethylene vinyl alcohol copolymer in 15 cases. Am J Roentgenol. 2010;194(1):W104–10.
Rasciti E, Sverzellati N, Silva M, Casadei A, Attina D, Palazzini M, Galie N, Zompatori M. Bronchial artery embolization for the treatment of haemoptysis in pulmonary hypertension. Radiol Med. 2017;122(4):257–64.
Acknowledgements
None.
Funding
This study was funded by (1) National Key R&D Program of China (2023YFC2507203); (2) Health Appropriate Technology Promotion Program of Chongqing (2017jstg31, 2018jstg012, 2019jstg023, 2022jstg005); (3) Famous Teacher Program (Medical Field) of Chongqing Municipal Health Commission (CQYC20220203178); (4) Chongqing Medical Scientific Research Project (Joint Project of Chongqing Health Commission and Science and Technology Bureau) (2022GDRC010).
Author information
Authors and Affiliations
Contributions
SF and XC: study concept and design, data acquisition, literature revision, manuscript writing. XW: critical revision for intellectual content. YL: critical revision for intellectual content, study supervision. WH: arbitration of disagreements, critical revision for intellectual content. HC: critical revision for intellectual content, study supervision.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Fan, S., Cheng, X., Wang, X. et al. Bronchial artery embolization versus conservative treatment for hemoptysis: a systematic review and meta-analysis. BMC Pulm Med 24, 428 (2024). https://doi.org/10.1186/s12890-024-03244-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-024-03244-x