Abstract
Background
The quadriceps-sparing and subvastus approaches are two of the most commonly used minimally-invasive approaches in total knee arthroplasty (TKA). However, the conclusion among studies still remains controversial. The purpose of this meta-analysis was to compare the clinical efficacy of the subvastus and quadriceps-sparing approaches with the standard parapatellar approach in TKA.
Methods
Randomized controlled trials (RCTs) comparing the quadriceps-sparing or subvastus approach with the standard parapatellar approach was identified in the databases of PubMed, the Cochrane library, EMBASE and Web of Science up to July 2014. Two authors extracted the following data: the basic characteristics of patients, the methodological quality and clinical outcomes from the included RCTs independently. RevMan 5.2.7 software was used for meta-analysis.
Results
A total of 19 RCTs (1578 patients) were included for meta-analysis. The results suggested that the quadriceps-sparing approach showed better outcomes in knee society score (KSS) and visual analog score (VAS), but this approach required a longer operative time than the standard parapatellar approach. There were no differences in total complications, wound infection, deep vein thrombosis, blood loss and hospital stay between the quadriceps-sparing and standard approaches. The subvastus approach showed better outcomes in VAS, knee range of motion (ROM), straight leg raise and lateral retinacular release than the standard parapatellar approach. There were no differences in KSS, total complication, wound infection, deep vein thrombosis, blood loss and hospital stay between the quadriceps-sparing and standard approaches.
Conclusions
The current evidence showed that, when compared with the standard parapatellar approach, the quadriceps-sparing approach was associated with better outcomes in KSS and VAS but required a longer operative time, and the subvastus approach was associated with better outcomes in VAS, ROM, straight leg raise and lateral retinacular release.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Total knee arthroplasty (TKA) has been one of the most successful operations for patients with end-stage knee diseases. As the standard approach, the medial parapatellar approach has been popularized for the excellent operative visualization. However, this approach requires the compromise of peripatellar blood supply and the quadriceps muscle, which might cause avascular necrosis and anterior knee pain [1].
In the last decade, the minimally invasive approaches such as mini-medial parapatellar, midvastus, subvastus and quadriceps-sparing approach, have provided promising advantages over the standard approach. The mini-medial parapatellar and midvastus approaches were less minimally invasive than the standard approach, but both disrupted quadriceps mechanism during surgery [2–4]. Compared with the above two approaches, the quadriceps-sparing and subvastus approaches were regarded as truly “anatomic” techniques in TKA because both avoided the disruption of the quadriceps tendon and the insertion of the vastus medialis in TKA [5–7]. Therefore, these two techniques also were described as the least minimally invasive approaches for TKA [8–10].
Theoretically, the quadriceps-sparing and subvastus approaches could offer better clinical outcomes for patients [11–15]. Previously, many studies have compared the clinical outcomes between the quadriceps-sparing or subvastus approach with the standard parapatellar approach. However, their conclusions among studies still remain conflicting. Some studies advocated the use of subvastus or quadriceps-sparing approach. They reported that these two approaches had significant advantages in knee society scores (KSS) [1, 16, 17], straight-leg raise [17–19], visual analogue score (VAS) [17] and range of motion (ROM) [16, 18, 20, 21]. However, other studies did not support this viewpoint. They found that the standard parapatellar approach provided less complications and better knee function than the subvastus or the quadriceps-sparing approaches [14, 19, 22–26].
To quantitatively compare the clinical efficacy and safety of the quadriceps-sparing and subvastus approaches to the standard parapatellar approach in TKA, we included all the published randomized controlled trials (RCTs) and conducted this meta-analysis.
Methods
This meta-analysis was performed in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines [27].
Inclusion criteria
The studies were included if they were randomized controlled trials (RCTs) comparing the subvastus or quadriceps-sparing approach with the standard parapatellar approach in TKA. Case report, cohort study, quasi-RCT and non-RCT were excluded in this study not considered for inclusion. The included participants should be adult patients who underwent the primary TKA. The extracted outcomes included: KSS and VAS, ROM, lateral retinacular release, straight leg raise, blood loss, operative time, hospital stay and postoperative complications (wound infection, deep vein thrombosis and total complications).
Literature search
The databases of PubMed, the Cochrane library, EMBASE, Chinese Biomedical Database and ISI Web of Knowledge were searched for the relevant studies from January 1982 to July 2014. The following search strategies were used for literature search: #1, “Arthroplasty, Replacement, Knee” [Mesh]; #2, knee arthroplasty; #3. knee replacement, #4. medial parapatellar; #5. standard OR conventional approach; # 6. subvastus; #7. mini-subvastus; #8. quadriceps-sparing; #9. quad-sparing; #10. quadriceps sparing; #11. #1 OR #2 OR # 3 OR; # 12. #4 OR # 5; # 13. #6 OR #7 OR #8 OR # 9 OR #10; # 11 AND # 12 AND # 13. In addition, the lists of references and Google scholar were also searched for other potential RCTs.
Data collection and quality assessment
Two authors independently screened the titles and abstracts. If the studies possibly met the inclusion criteria, the full text was retrieved for the final decision. Data extraction was completed by two blind authors. If insufficient data was reported, efforts were made to contact the authors for the additional information. The methodological quality was evaluated using the following items recommended by the Cochrane Collaboration [28]: randomization; allocation concealment; blinding of participants; blinding of outcome assessors; incomplete outcome data; selective reporting; and other bias. Each item was classified into “Yes”, “No”, or “Unclear”: “Yes” - low risk of bias, “No” - high risk of bias, “Unclear” - lack of information or unknown risk of bias. Any disagreement in assessments was resolved by discussing with a third author.
Statistical analysis
The software of Review Manager 5.2.7 [28] was used to perform meta-analysis. Odds ratios (OR) and 95 % confidence interval (95 % CI) was calculated to test the overall effects for dichotomous outcomes, and mean difference (MD) and 95 % CI were used for continuous outcomes. Heterogeneity was tested using I2 statistic (I2 > 50 % indicating significant heterogeneity, and I2 ≤ 50 % indicating no significant heterogeneity) [29]. If significant heterogeneity (I2 > 50 %) was found in the meta-analysis, random-effect model was used, otherwise, using fix-effect model. Subgroup analysis was performed for outcomes with different time points.
Results
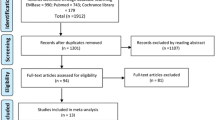
Figure 1 showed the flow chart of literature screening. From the initial database search, a total of 423 citations were yielded. After removing 165 duplicates, 258 studies were reserved for abstract screening and full-text screening. Finally, nineteen RCTs [12, 14, 16, 18–26, 30–36] were considered to be eligible for meta-analysis. Of the included studies, nine [14, 17, 19, 22, 31–35] RCTs comparing the quadriceps-sparing approach with the standard parapatellar approach and ten [12, 16, 18, 20, 21, 23–26, 30] comparing the subvastus approach with the standard parapatellar approach were included.
The characteristics and quality assessment of the included RCTs
The characteristics of the included RCTs were summarized in Table 1. A total of 1633 TKAs were performed in 1578 adult patients (male: 31.8 %; female: 68.2 %). The mean age ranged from 62.5–73.8, the mean BMI ranged from 24.6–30.97, and the follow-up duration ranged from 13 days to 3 years. The patients’ parameters (age, BMI, patient/TKA number, preoperative knee function) were reported similar between groups.
Regarding the methodological quality, all the included studies were randomized using various methods: eight (42.1 %) used the computer-generated random number and seven (36.8 %) used random number table. Allocation concealment was reported in 10 studies (52.6 %); the method of blind was used in 16 studies (84.2 %) (Table 2).
Results of meta-analysis
Quadriceps-sparing versus the standard parapatellar approach
Nine RCTs [14, 17, 19, 22, 31–35] comparing the quadriceps-sparing with the standard parapatellar approaches were included for meta-analysis (n = 725 patients with 775 TKAs) (Table 3).
Primary outcomes
Meta-analysis showed that, when compared with the standard approach, the quadriceps-sparing approach significantly improved KSS at postoperative 3 months (MD = 2.88, 95 % CI [1.17, 4.60], P = 0.001) and 2 years (MD = 1.75, 95 % CI [0.45, 3.06], p = 0.08), and decreased VAS at postoperative 1 week (MD = −0.69, 95 % CI [−1.10, −0.29], P < 0.05). There were no differences in KSS at postoperative 4–6 weeks (MD = −0.91, 95 % CI [−3.08, 1.25], P = 0.41) and VAS at postoperative 4–6 weeks (MD = 0.14, 95 % CI [−0.29, 0.58], P = 0.52) between both groups. No significant heterogeneity was found in the meta-analysis of KSS and VAS (I2 ≤ 50 %) (Table 3).
Secondary outcomes
Meta-analysis showed that the quadriceps-sparing and the standard parapatellar approaches had similar results in total complication (MD = 1.00, 95 % CI [0.21, 4.72], P = 0.49), wound infection (MD = 1.21, 95 % CI [0.29, 5.05], P = 0.80), deep vein thrombosis (MD = 0.65, 95 % CI [0.13, 3.31], P = 0.60), ROM from 1 week (MD = 5.79, 95 % CI [−6.26, 17.85], P = 0.35 %)–24 months (MD = −0.18, 95 % CI [−1.91, 1.56], P = 0.84), blood loss (MD = −57.00, 95 % CI [−213.73, 99.73]) and hospital stay (MD = −2.00, 95 % CI [−3.19, −0.81], P = 0.10). However, the quadriceps-sparing approach significantly increased operative time when compared with the standard parapatellar approach (MD = 18.22, 95 % CI [9.92, 26.51], P < 0.05). The heterogeneity was significant in ROM, operative time and hospital stay (I2 > 50 %) (Table 3).
Subvastus versus Medial parapatellar approach
Ten RCTs [12, 16, 18, 20, 21, 23–26, 30] comparing the subvastus with the standard parapatellar approach were included for meta-analysis (Table 4).
Primary outcomes
Meta-analysis showed that the subvastus approach significantly reduced VAS score at postoperative 12 months (MD = −0.14, 95 % CI [−0.28, −0.01], P = 0.04) compared with the standard approach. There were no differences in KSS from postoperative 4 weeks (MD = −1.86, 95 % CI [−8.59, 4.88], P = 0.59)–12 months (MD = 3.25, 95 % CI [−0.60, 7.10]), and VAS from postoperative 1 week (MD = −0.56, 95 % CI [−1.42, 0.29], P = 0.19)–3 months (MD = −0.03, 95 % CI [−0.32, 0.27], P = 0.87) between the standard and subvastus groups (Table 3). Significant heterogeneity was found in KSS (4–6 weeks) and VAS (1 week–3 months) (I2 > 50 %).
Secondary outcomes
Meta-analysis showed that the subvastus approach had significant advantages over the standard parapatellar approach in ROM at postoperative 1 week (MD = 3.96, 95 % CI [3.20, 4.72], P < 0.05) and 12 months (MD = 6.80, 95 % CI [0.94, 12.66], P < 0.05), straight leg raise (OR = −2.77, 95 % CI [−4.07, −1.47], P =0.02) and lateral retinacular release (OR = 0.34, 95 % CI [0.14, 0.79], P = 0.01). The two groups showed similar results in ROM at postoperative 4–6 weeks (MD = 3.79, 95 % CI [−0.44, 8.03], P = 0.08) and 3 months (MD = 3.24, 95 % CI [−0.90, 7.38], P = 0.12), total complication (MD = 0.81, 95 % CI [0.44, 1.49], P = 0.49), wound infection (MD = 1.11, 95 % CI [0.40, 3.08]) and blood loss (MD = −100.76, 95 % CI [−223.42, 21.89], P = 0.11) (Table 4).
Discussion
Clinically, the quadriceps-sparing and subvastus approaches are very similar techniques, as both avoid the incision into the quadriceps tendon and the vastus medialis muscle during surgery. The quadriceps-sparing approach was first introduced by Tria et al. [7] from the minimally invasive unicondylar knee replacement. This technique used a more curvilinear medial incision without quadriceps damage and patella eversion. The advantage of the quadriceps-sparing approach was that, if needed, this technique can easily be extended or converted in the standard parapatellar approach [10]. However, critics indicated that this approach is not anatomically correct. Pagnano et al. [37] designed a magnetic resonance study in 200 cadaver specimens, and demonstrated that the vastus medialis obliquus was inserted to the midpole of the patella. Therefore, the quadriceps-sparing approach inevitably damaged the vastus medialis obliquus. The subvastus approach was first developed by Hofmann in 1991 [38]. It preserved the integrity of the extensor mechanism and minimized the injury to the patellar vascularity. Previous studies considered that the subvastus approach should be the true “quadriceps-sparing” approach in TKA [8, 18, 39].
For the subject concerning the superior approach for TKA, the conclusion was highly controversial. Among the included RCTs, five studies [17, 31, 32, 34, 35] favored the quadriceps-sparing approach, five [12, 16, 18, 20, 21] favored subvastus approach, four [14, 22, 30, 33] favored medial parapatellar approach, and others [19, 23–26] found no differences between groups. Therefore, we conducted a meta-analysis to quantitatively compare the clinical outcomes between the different approaches.
In our study, the most primary findings were that, the quadriceps-sparing approach had significant advantages in KSS and VAS over the standard approach, but had disadvantages in operative time. The subvastus approach provided better outcomes in VAS, ROM, straight leg raise and lateral retinacular release. There were no differences in other clinical outcomes when compared the quadriceps-sparing approach or subvastus with the standard group.
To date, there was no meta-analysis compared the quadriceps-sparing with the standard parapatellar approach in TKA. Totally, we included nine RCTs for meta-analysis. The results demonstrated that the quadriceps-sparing approach achieved better outcomes in KSS (postoperative 3 months and 2 years) and VAS (postoperative 1 week). This result supported the theory of minimally invasive technique. However, the level of this evidence was relatively weak due to the insufficient number of the included RCTs. In addition, our results also showed that the quadriceps-sparing group significantly increased operative time. The explanation was the quadriceps-sparing approach was technically more demanding. That required considerable efforts to obtain sufficient operative view during surgery [10].
Regarding the subvastus versus the standard parapatellar approach, ten RCTs were available for meta-analysis. Our meta-analysis showed that the subvastus approach had significant advantages over the standard approach in VAS (postoperative 6 months), ROM (postoperative 1 week and 12 months), straight leg raise and lateral retinacular release, and no disadvantages were found associated with the subvastus approach. Our conclusion was a little different with the published meta-analysis [1, 40]. Teng et al. [1] performed a meta-analysis including 8 RCTs and 1 quasi-RCTs, and concluded that the subvastus approach improved KSS score and decreased lateral retinacular release compared with the parapatellar approach. However, they found similar ROM in the two groups. The possible reason is that one quasi-RCT they included might bias the result of the meta-analysis. Additionally, despite surgical difficulty was high for the subvastus approach, the operative time showed no difference between the two groups. Our conclusion was in accordance with earlier studies [1, 23, 25, 40, 41] who also found no difference in operative time between both groups. The familiar exposure and new specific instrumentation contributed to the learning curve of subvastus technique.
Strengths and Limitations of this study
Two earlier systematic review or meta-analysis [1, 40] had compared the clinical efficiency between the subvastus and the standard aprraoch in TKA. However, the authors included quasi-RCT, which reduced the level of the evidence. Additionally, the published meta-analysis only investigated the short-term outcomes. The strengthens of this study included that: (1) the results of our meta-analysis were based on RCTs, which provided high-level evidence for clinical practice; (2) our study first reported a meta-analysis comparing the quadriceps-sparing with the standard approach.
Several limitations should be noted in our study. (1). Although some outcomes were reported in the full text, data was not sufficiently provided to perform meta-analysis. (2) Although efforts were made to minimize the heterogeneity by conducting subgroup analysis, for example, using random-effect model and setting strict inclusion criteria, the heterogeneity among the included studies was still significant in several meta-analyses, which might decrease the reliability of the conclusion. Readers should be cautious for the results when heterogeneity existed. (3) Although all the included RCTs used randomization, some RCTs did not used allocation concealment and blinding to the patients and surgeons, which also might lead to high risks of selection and detection bias; besides, the most RCTs included were performed in single center with small samples, therefore, multi-center RCTs with large-samples are still lacking to verify our conclusion. (4) For a superior approach in TKA, it should include the following criteria: simple technique, sufficient visibility, less complication rates and improve clinical outcomes. Obviously, the quadriceps-sparing or subvastus approach did not involve all the criteria above. Therefore, TKA surgeons should get a balanced perspective for the two approaches.
Conclusion
Based on the current evidence, our study finds that, in comparison with the standard parapatellar approach, the quadriceps-sparing approach showed better outcomes in KSS and VAS, and the subvastus approach shows better outcomes in VAS, ROM, straight leg raise and lateral retinacular release, but the quadriceps-sparing technique requires longer operative time.
Abbreviations
- TKA:
-
Total knee arthroplasty
- RCTs:
-
Randomized controlled trials
- KSS:
-
Knee society scores
- VAS:
-
Visual analogue score
- ROM:
-
Range of motion
- OR:
-
Odds ratios
- CI:
-
Confidence interval
- MD:
-
Mean difference
- BMI:
-
Body mass index
- SV:
-
Subvastus
- SP:
-
Standard parapatellar
- QS:
-
Quadriceps-sparing
- N.S:
-
Not significant
References
Teng Y, Du W, Jiang J, Gao X, Pan S, Wang J, et al. Subvastus versus medial parapatellar approach in total knee arthroplasty: meta-analysis. Orthopedics. 2012;12:e1722–1731.
Heekin RD, Fokin AA. Mini-midvastus versus mini-medial parapatellar approach for minimally invasive total knee arthroplasty: outcomes pendulum is at equilibrium. J Arthroplasty. 2014;2:339–42.
Li XG, Tang TS, Qian ZL, Huang LX, Pan WM, Zhu RF. Comparison of the mini-midvastus with the mini-medial parapatellar approach in primary TKA. Orthopedics. 2010;10:723.
Zhang Z, Zhu W, Gu B, Zhu L, Chen C. Mini-midvastus versus mini-medial parapatellar approach in total knee arthroplasty: a prospective, randomized study. Arch Orthop Trauma Surg. 2013;3:389–95.
Niki Y, Mochizuki T, Momohara S, Saito S, Toyama Y, Matsumoto H. Is minimally invasive surgery in total knee arthroplasty really minimally invasive surgery? J Arthroplasty. 2009;4:499–504.
Hofmann AA, Plaster RL, Murdock LE. Subvastus (Southern) approach for primary total knee arthroplasty. Clin Orthop Relat Res. 1991;269:70–7.
Tria Jr AJ, Coon TM. Minimal incision total knee arthroplasty: early experience. Clin Orthop Relat Res. 2003;416:185–90.
Scuderi GR, Tenholder M, Capeci C. Surgical approaches in mini-incision total knee arthroplasty. Clin Orthop Relat Res. 2004;428:61–7.
Tenholder M, Clarke HD, Scuderi GR. Minimal-incision total knee arthroplasty: the early clinical experience. Clin Orthop Relat Res. 2005;440:67–76.
Aglietti P, Baldini A, Sensi L. Quadriceps-sparing versus mini-subvastus approach in total knee arthroplasty. Clin Orthop Relat Res. 2006;452:106–11.
Lin TC, Wang HK, Chen JW, Chiu CM, Chou HL, Chang CH. Minimally invasive knee arthroplasty with the subvastus approach allows rapid rehabilitation: a prospective, biomechanical and observational study. J Phys Ther Sci. 2013;5:557–62.
Jain S, Wasnik S, Mittal A, Hegde C. Outcome of subvastus approach in elderly nonobese patients undergoing bilateral simultaneous total knee arthroplasty: A randomized controlled study. Indian J Orthop. 2013;1:45–9.
Jackson G, Waldman BJ, Schaftel EA. Complications following quadriceps-sparing total knee arthroplasty. Orthopedics. 2008;6:547.
Kim YH, Kim JS, Kim DY. Clinical outcome and rate of complications after primary total knee replacement performed with quadriceps-sparing or standard arthrotomy. J Bone Joint Surg Br. 2007;4:467–70.
Chen AF, Alan RK, Redziniak DE, Tria Jr AJ. Quadriceps sparing total knee replacement. The initial experience with results at two to four years. J Bone Joint Surg Br. 2006;11:1448–53.
Varela-Egocheaga JR, Suarez-Suarez MA, Fernandez-Villan M, Gonzalez-Sastre V, Varela-Gomez JR, Rodriguez-Merchan C. Minimally invasive subvastus approach: improving the results of total knee arthroplasty: a prospective, randomized trial. Clin Orthop Relat Res. 2010;5:1200–8.
Shen H, Zhang XL, Wang Q, Shao JJ, Jiang Y. [Minimally invasive total knee arthroplasty through a quadriceps sparing approach: a comparative study]. Zhonghua Wai Ke Za Zhi. 2007;16:1083–6.
Roysam GS, Oakley MJ. Subvastus approach for total knee arthroplasty: a prospective, randomized, and observer-blinded trial. J Arthroplasty. 2001;4:454–7.
Lin WP, Lin J, Horng LC, Chang SM, Jiang CC. Quadriceps-sparing, minimal-incision total knee arthroplasty: a comparative study. J Arthroplasty. 2009;7:1024–32.
Bridgman SA, Walley G, MacKenzie G, Clement D, Griffiths D, Maffulli N. Sub-vastus approach is more effective than a medial parapatellar approach in primary total knee arthroplasty: a randomized controlled trial. Knee. 2009;3:216–22.
Sastre S, Sanchez MD, Lozano L, Orient F, Fontg F, Nunez M. Total knee arthroplasty: better short-term results after subvastus approach: a randomized, controlled study. Knee Surg Sports Traumatol Arthrosc. 2009;10:1184–8.
Chiang H, Lee CC, Lin WP, Jiang CC. Comparison of quadriceps-sparing minimally invasive and medial parapatellar total knee arthroplasty: a 2-year follow-up study. J Formos Med Assoc. 2012;12:698–704.
Weinhardt C, Barisic M, Bergmann EG, Heller KD. Early results of subvastus versus medial parapatellar approach in primary total knee arthroplasty. Arch Orthop Trauma Surg. 2004;6:401–3.
Pan WM, Li XG, Tang TS, Qian ZL, Zhang Q, Zhang CM. Mini-subvastus versus a standard approach in total knee arthroplasty: a prospective, randomized, controlled study. J Int Med Res. 2010;3:890–900.
Van Hemert WL, Senden R, Grimm B, van der Linde MJ, Lataster A, Heyligers IC. Early functional outcome after subvastus or parapatellar approach in knee arthroplasty is comparable. Knee Surg Sports Traumatol Arthrosc. 2010;6:943–51.
Wegrzyn J, Parratte S, Coleman-Wood K, Kaufman KR, Pagnano MW. The John Insall award: no benefit of minimally invasive TKA on gait and strength outcomes: a randomized controlled trial. Clin Orthop Relat Res. 2013;1:46–55.
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;10:1006–12.
Higgins. JPT, Green. S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration. Available at: www.cochrane-handbookorg. Accessed 2 June 2014
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;11:1539–58.
Varnell MS, Bhowmik-Stoker M, McCamley J, Jacofsky MC, Campbell M, Jacofsky D. Difference in stair negotiation ability based on TKA surgical approach. J Knee Surg. 2011;2:117–23.
Xu J, Liu C, Zhou S, Lin Y. Total knee arthroplasty:Comparison between quadriceps sparing approach and medial parapatellar approach. J Clin Rehabilit Tissue Engineering Res. 2013;35:6240–6.
Tasker A, Hassaballa M, Murray J, Lancaster S, Artz N, Harries W, et al. Minimally invasive total knee arthroplasty; a pragmatic randomised controlled trial reporting outcomes up to 2 year follow up. Knee. 2014;1:189–93.
Lin SY, Chen CH, Fu YC, Huang PJ, Lu CC, Su JY, et al. Comparison of the clinical and radiological outcomes of three minimally invasive techniques for total knee replacement at two years. Bone Joint J. 2013;7:906–10.
Matsumoto T, Muratsu H, Kubo S, Mizuno K, Kinoshita K, Ishida K, et al. Soft tissue balance measurement in minimal incision surgery compared to conventional total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2011;6:880–6.
Karpman RR, Smith HL. Comparison of the early results of minimally invasive vs standard approaches to total knee arthroplasty: a prospective, randomized study. J Arthroplasty. 2009;5:681–8.
Shen H, Zhang XL, Wang Q, Shao JJ, Jiang Y. Minimally invasive total knee arthroplasty through a quadriceps sparing approach: a comparative study. Zhonghua Wai Ke Za Zhi. 2007;16:1083–6.
Pagnano MW, Meneghini RM, Trousdale RT. Anatomy of the extensor mechanism in reference to quadriceps-sparing TKA. Clin Orthop Relat Res. 2006;452:102–5.
Hofmann AA, Plaster RL, Murdock LE. Subvastus (Southern) approach for primary total knee arthroplasty. Clin Orthop Relat Res. 1991;269:70–7.
Schroer WC, Diesfeld PJ, Reedy ME, LeMarr AR. Mini-subvastus approach for total knee arthroplasty. J Arthroplasty. 2008;1:19–25.
Hu X, Wang G, Pei F, Shen B, Yang J, Zhou Z, et al. A meta-analysis of the sub-vastus approach and medial parapatellar approach in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2012;21(10):2398–404.
Bourke MG, Jull GA, Buttrum PJ, Fitzpatrick PL, Dalton PA, Russell TG. Comparing outcomes of medial parapatellar and subvastus approaches in total knee arthroplasty: a randomized controlled trial. J Arthroplasty. 2012;3:347–53. e341.
Acknowledgement
This work was supported by National Natural Science Foundation of China (81201425). Thanks for Matthew Crawford (America) for the English editing of this manuscript.
Level of evidence
Therapeutic study Level I
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
Each author has materially contributed to the following five elements of the study: (1). designing the study (XP, XZ); (2). collecting the data (XP, TC, MC); (3). analyzing and interpreting the data (TC, MC, JW); (4). ensuring the accuracy of the data (XP, XZ). (5). writing the initial draft (XP, TC, MC, JW). All authors read and approved the final manuscript.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Peng, X., Zhang, X., Cheng, T. et al. Comparison of the quadriceps-sparing and subvastus approaches versus the standard parapatellar approach in total knee arthroplasty: a meta-analysis of randomized controlled trials. BMC Musculoskelet Disord 16, 327 (2015). https://doi.org/10.1186/s12891-015-0783-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-015-0783-z