Abstract
Background
We report a rare case of posterior cruciate ligament (PCL) calcification, which has only been reported in two case studies on PubMed.
Case presentation
A 71-year-old man developed left popliteal pain in the morning without any history of trauma and the pain became severe that night. On the following day, he presented to our department. The patient could not flex his left knee at all due to pain and swelling. CT and MRI scans showed calcification behind the PCL with mild osteoarthritic changes and accumulation of synovial fluid in the joint. Synovial fluid analysis did not reveal any crystals. Blood tests at first admission showed inflammation, hyperglycemia, and low blood uric acid levels. Although the patient’s knee joint was injected with steroids, his symptoms did not improve. Thus, we performed arthroscopic surgery two days after symptoms had appeared. Intraoperatively, we observed a white, soft tissue in the synovial membrane behind the PCL. Part of this tissue was collected for histological analysis, which revealed sparse fibers with calcium deposits. Immediately after surgery, the patient’s symptoms were completely gone. Afterward, the patient remained asymptomatic one month after surgery.
Conclusion
This is the first reported case of debridement of PCL calcification and ossification that was performed soon after symptoms appeared. In addition, we demonstrated that early debridement led to complete recovery.
Similar content being viewed by others
Background
Knee ligament calcification is rare but calcification of vessel walls and the rotator cuff is commonly observed. Patients with calcification in the articulation experience severe pain even at rest and often cannot sleep due to the pain. The literature in PubMed includes several reports of medial collateral ligament (MCL) calcification in the knee ligament [1, 2] and a few reports of anterior cruciate ligament (ACL) calcification [3,4,5]. However, there is only one report of posterior cruciate ligament (PCL) calcification [6] and one report of PCL ossification [7]. In these two cases, arthroscopic debridement was performed more than a year after symptoms had appeared. Herein, we report a patient in whom arthroscopic debridement of calcium deposits was performed two days after symptoms had appeared.
Case presentation
A 71-year-old man was admitted to our outpatient clinic and complained that he had been experiencing left popliteal pain since the day before. His symptoms appeared in the morning and acutely got worse that night without any history of trauma. The pain was severe even during rest, and the patient was not able to sleep. On the following day, he presented to our department. His past medical history included diagnoses of diabetes and hyperlipidemia. He had not experienced any fever since the symptoms first appeared, but the popliteal fossa was observed to be tender. The patient’s knee was swollen and had a positive ballottement test. The skin of the knee had a normal temperature and did not exhibit any redness. However, the patient could not flex his knee at all (0 degrees of flexion) and he could not walk because of the pain.
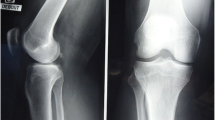
Blood tests at first admission showed that the white blood cell count was 9700 /µL, the CRP level was 1.45 mg/dL, the glucose level was 202 mg/dL, hemoglobin A1c was 7.4%, and the uric acid level was 2.4 mg/dL. X-rays revealed a high-density mass within the intercondylar notch (Fig. 1). Multi-planar computed tomography (CT) showed a mass with heterogeneous density behind the PCL (Fig. 2A). Magnetic resonance imaging (MRI) showed the mass behind the PCL with mild osteoarthritic changes, accumulation of synovial fluid in the articulation, and inflammation of the synovial membrane in the popliteal fossa (Fig. 2B). Synovial fluid was collected, and its analysis did not reveal any crystals.
Although the patient’s knee joint was injected with steroids, he was still in severe pain the next day. We performed arthroscopic surgery two days after symptoms had first appeared in order to conduct further examinations and initiate treatment. Since the pain was preventing the patient from sleeping at night, he wanted to be diagnosed and treated as soon as possible. Intraoperatively, a partial medial meniscus posterior root tear (MMPRT) that appeared to be old and degraded was found (Fig. 3A), the lateral tibia cartilage was observed to be fibrillated (Fig. 3B), and a white, soft toothpaste-like tissue was noted in the synovial membrane behind the PCL. A minimal portion of the synovial membrane of the PCL was removed and the calcification was pushed out to retain as much of the PCL as possible. The MMPRT was not treated since the medial meniscus posterior root did not show any instability. The majority of the unknown tissue behind the PCL broke apart in the synovial fluid, but a part of the tissue was collected for further histological analysis (Fig. 4A, B). H-E staining revealed sparse fibers and multi-nucleated giant cells within the tissue (Fig. 5A). Von-Kossa staining showed calcium deposits in most of the fibrous tissue (Fig. 5B).
The patient’s symptoms were completely gone after surgery. He was allowed full range of motion and could walk without pain. A small amount of calcification was observed on postoperative CT scans (Fig. 6). One month later, X-rays with a posterior gravity sagging view showed no posterior sagging of the proximal tibia. The patient remains asymptomatic one month after surgery.
Discussion and conclusions
This is the first reported case of early debridement of PCL calcification and ossification that was performed soon after symptoms appeared. In addition, this procedure led to complete recovery. There is only one report of PCL calcification [6] and one report of PCL ossification [7] in the literature. In both cases, arthroscopic debridement was performed more than a year after symptoms had appeared.
The diagnosis of ligament calcification was based on MRI and arthroscopic findings of this case and previous reports. Arthroscopic images showed that the calcification was in the synovial membrane of the PCL and were similar to findings observed in a previous report of ACL calcification [3]. Synovial mesenchymal stem cells can also differentiate into chondrocytes [8], which may have given rise to the calcification in the synovial membrane. However, there have been no reports of intrasynovial calcification other than in solid tumor tissue. In our case, the calcification in the synovial cavity developed among sparse fibers in the absence of tumor tissue. One possible scenario is that the lining integrity of the synovial barrier was disrupted during joint inflammation and monocytes which can undergo autophagy migrated to the synovial cavity [9].
Differential diseases in this case included MMPRT and crystal-induced arthritis. It was difficult to diagnose the MMPRT on MRI because it was an incomplete tear (type 1) [10] and had no extrusion (stage 0) [11]. MMPRTs can sometimes lead to severe pain. However, the pain experienced by our patient could not have been due to osteoarthritis of the knee and MMPRT because he had severe pain even at rest, the MMPRT was not fresh, and only the PCL calcification was treated through debridement. Additionally, the patient did not have crystal-induced arthritis because synovial fluid analysis did not reveal any crystals. Thus, we concluded that the pain had been caused by the PCL calcification.
Arthroscopic surgery was selected for treatment and also for conducting further examinations, since the patient could not sleep at night due to the pain and wanted to be diagnosed and treated as soon as possible. During the operation, a minimal amount of the synovial membrane of the PCL was removed and the calcification was pushed out to retain as much of the PCL as possible. This led to some of the calcification being retained behind the PCL, as was observed in postoperative CT scans. However, the patient was able to completely recover. This suggests that the calcification does not have to be removed completely for an optimal outcome. A previous study also demonstrated that ultrasound-guided debridement of MCL calcification led to early complete recovery with a small calcification left behind [12]. In our case study, arthroscopic surgery was performed to determine if there was another cause for the pain, but ultrasound-guided debridement might have had a similar outcome.
The histological analysis led us to believe that calcification was present. Calcification is defined as the deposit of calcium salts in tissue. In contrast, ossification is defined as the formation of bone (calcification in the collagen matrix) whether or not there is bone marrow [13]. In our case, calcium deposits were found in the fibrous tissue but the fibers were sparse and there was no bone-like tissue. Therefore, we speculated that the calcium deposits were not indicative of bone formation but of calcification. Calcification can occur in vessels, muscles, tendons, and ligaments [14]. Trauma, overuse, and metabolic disorders like diabetes can cause calcification in the articulation [14,15,16,17,18]. However, the pathogenesis of that process remains unclear. Our patient had a history of diabetes. The reference range for serum uric acid in humans is 1.5-6.0 mg/dL for women and 2.5-7.0 mg/dL for men, while hypouricemia is commonly diagnosed when levels drop to 2.0 mg/dL or less. There is currently no report regarding any correlation between calcification in the joint and uric acid. However, it has been reported that hypouricemia can increase oxidant stress [19], which in turn can lead to vessel calcification [20]. In our case study, low blood uric acid levels could have also led to low uric acid levels in the joint, resulting in oxidant stress and calcification. Our patient had diabetes as well as relatively low blood uric acid, which could have easily induced calcification in the body. However, it remains unclear why calcification did occur behind the PCL in this case.
The underlying mechanism for calcification within the knee joint remains unclear. Calcification of the rotator cuff is induced by chondrocyte-like cells [21], which may be involved in endochondral ossification. In addition, calcific tendonitis of the rotator cuff can lead to severe pain during the resorption phase because of inflammation around the calcification [21]. In this phase, the deposit has a creamy or toothpaste-like consistency while it has a stiff mass like chalk in the calcific phase [14]. In our case, the calcium deposit may have been in the resorption phase because the tissue contained multi-nucleated giant cells and was soft enough to break apart in the synovial fluid. This could have led to inflammation of the synovial membrane and severe pain.
In conclusion, PCL calcification is rare. In our case, metabolic disorder may have been the cause of the calcification. This is the first report where debridement of calcification was performed soon after symptoms first appeared, leading to complete recovery.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
- MCL:
-
Medial collateral ligament
- ACL:
-
Anterior cruciate ligament
- PCL:
-
Posterior cruciate ligament
- CT:
-
Computed tomography
- MRI:
-
Magnetic resonance imaging
- MMPRT:
-
Medial meniscus posterior root tear
References
Muschol M, Müller I, Petersen W, Hassenpflug J. Symptomatic calcification of the medial collateral ligament of the knee joint: a report about five cases. Knee Surg Sports Traumatol Arthrosc. 2005;13(7):598–602.
Berry CJ, Tagliero AJ, Diduch DR. Atraumatic calcific tendinitis in medial collateral ligament: a Case Report. J Orthop Case Rep. 2023;13(11):49–52.
Tsujii A, Tanaka Y, Yonetani Y, Iuchi R, Shiozaki Y, Horibe S. Symptomatic calcification of the anterior cruciate ligament: a case report. Knee. 2012;19(3):223–5.
Sarsilmaz A, Gelal F. A new variation: an anterior cruciate ligament attached to the accessory ossicle. Clin Anat. 2011;24(8):991–3.
Devgan A, Mukhopadhyay R, Singh A, Gogna P, Singla R, Magu NK. Ossicle in anterior cruciate ligament: a rare occurrence. Case Rep Orthop. 2014;2014:616715.
Koukoulias NE, Papastergiou SG. Isolated posterior cruciate ligament calcification. BMJ Case Rep 2011, 2011.
Li C, Huang Z, Anil KC, Lao C, Wu Q, Jiang H. Heterotopic ossification in the post cruciate ligament of the knee: a case report and literature review. BMC Musculoskelet Disord. 2021;22(1):304.
Mizuno M, Katano H, Otabe K, Komori K, Kohno Y, Fujii S, Ozeki N, Horie M, Tsuji K, Koga H, et al. Complete human serum maintains viability and chondrogenic potential of human synovial stem cells: suitable conditions for transplantation. Stem Cell Res Ther. 2017;8(1):144.
Knab K, Chambers D, Krönke G. Synovial macrophage and fibroblast heterogeneity in joint homeostasis and inflammation. Front Med (Lausanne). 2022;9:862161.
Kim JY, Bin SI, Kim JM, Lee BS, Oh SM, Cho WJ. A novel arthroscopic classification of degenerative medial Meniscus posterior Root tears based on the tear gap. Orthop J Sports Med. 2019;7(3):2325967119827945.
Swamy N, Wadhwa V, Bajaj G, Chhabra A, Pandey T. Medial meniscal extrusion: detection, evaluation and clinical implications. Eur J Radiol. 2018;102:115–24.
Galletti L, Ricci V, Andreoli E, Galletti S. Treatment of a calcific bursitis of the medial collateral ligament: a rare cause of painful knee. J Ultrasound. 2019;22(4):471–6.
Chan ED, Morales DV, Welsh CH, McDermott MT, Schwarz MI. Calcium deposition with or without bone formation in the lung. Am J Respir Crit Care Med. 2002;165(12):1654–69.
O’Brien EJ, Frank CB, Shrive NG, Hallgrímsson B, Hart DA. Heterotopic mineralization (ossification or calcification) in tendinopathy or following surgical tendon trauma. Int J Exp Pathol. 2012;93(5):319–31.
Harvie P, Pollard TC, Carr AJ. Calcific tendinitis: natural history and association with endocrine disorders. J Shoulder Elb Surg. 2007;16(2):169–73.
Hurt G, Baker CL Jr. Calcific tendinitis of the shoulder. Orthop Clin North Am. 2003;34(4):567–75.
Oliva F, Barisani D, Grasso A, Maffulli N. Gene expression analysis in calcific tendinopathy of the rotator cuff. Eur Cell Mater. 2011;21:548–57.
Mavrikakis ME, Drimis S, Kontoyannis DA, Rasidakis A, Moulopoulou ES, Kontoyannis S. Calcific shoulder periarthritis (tendinitis) in adult onset diabetes mellitus: a controlled study. Ann Rheum Dis. 1989;48(3):211–4.
Otani N, Ouchi M, Mizuta E, Morita A, Fujita T, Anzai N, Hisatome I. Dysuricemia-A New Concept Encompassing Hyperuricemia and Hypouricemia. Biomedicines 2023, 11(5).
Lian Y, Li Y, Liu A, Ghosh S, Shi Y, Huang H. Dietary antioxidants and vascular calcification: from pharmacological mechanisms to challenges. Biomed Pharmacother. 2023;168:115693.
Darrieutort-Laffite C, Blanchard F, Le Goff B. Calcific tendonitis of the rotator cuff: from formation to resorption. Joint Bone Spine. 2018;85(6):687–92.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
YN treated the patient as a primary care physician. YI performed the surgery. KT assisted in the surgery. NA edited the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Institutional review board of Saiseikai Hiroshima Hospital has approved present case study. Consent to participate was obtained from the patient.
Consent for publication
The patient gave written informed consent for their personal and clinical details along with any identifying images to be published in this study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Matsubara, Y., Nitta, Y., Tanaka, K. et al. Early arthroscopic debridement of posterior cruciate ligament calcification after symptom presentation led to immediate recovery: a case report. BMC Musculoskelet Disord 25, 690 (2024). https://doi.org/10.1186/s12891-024-07817-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-024-07817-z