Abstract
Purpose
This study aimed to compare the clinical outcomes and differences in biomechanical characteristics between the femoral neck system (FNS) and cannulated cancellous screws (CCSs) in the treatment of femoral neck fractures.
Methods
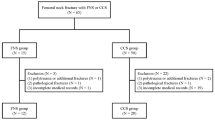
This study retrospectively analysed a cohort of 38 registered cases of femoral neck fractures treated surgically with either the FNS (n = 17) or CCSs (n = 21) between January 2020 and December 2023. Indicators such as fluoroscopy frequency, length of hospital stay, and fracture healing time were compared between the two groups. Functional status was evaluated via the Harris hip score (HHS) and visual analogue scale (VAS), whereas prognosis was assessed based on changes in the neck shaft angle and femoral neck shortening. Additionally, six sets of femoral neck fracture models were developed based on Pauwels angles of 30°, 40°, 50°, 60°, 70°, and 80°. Two experimental groups, FNS and CCS, were established, and a joint reaction force of 1800 N was applied to the proximal femur. The displacement, stress, and stiffness of the components of interest in the different models were tested and compared.
Results
The distributions of all the baseline characteristics were similar between the two groups (p > 0.05). The FNS group presented significantly shorter fluoroscopy frequency, length of hospital stay, and fracture healing time (p < 0.05). Harris and VAS scores were higher in the FNS group than in the CCS group (p < 0.05). Postoperative changes in the neck shaft angle and femoral neck shortening were significantly lower in the FNS group than in the CCS group (p < 0.05). The results of the finite element analysis indicated that the maximum stress on the femoral head and varus angle were generally lower in the FNS group than in the CCS group and that the maximum displacement of the femoral head and FNS was generally lower in the FNS group than in the CCS group. However, the superiority of FNS over CCS decreased with increasing Pauwels angle. Additionally, the effectiveness of FNS in limiting displacement of the femoral neck upper wall was not as favourable as that of CCS.
Conclusions
The treatment of femoral neck fractures with FNS is superior and contributes to improved hip joint function. Biomechanical research has confirmed its structural stability and advantages in resisting femoral head varus. However, challenges to its fixation efficacy persist, particularly at higher Pauwels angles.
Similar content being viewed by others
Introduction
Femoral neck fracture is a common orthopaedic condition that accounts for approximately 57% of hip fractures [1]. It often occurs in elderly individuals as a result of low-energy falls. With advances in medical technology, the treatment outcomes of femoral neck fractures have significantly improved [2]. However, elderly individuals with hip fractures still face many risks, including decreased quality of life, increased care demands, secondary osteoporosis, and mortality [3]. Once a fracture occurs, the mortality rate within one year can increase from 14 to 36% [4]. How to treat these femoral neck fracture patients quickly and effectively is a problem that clinical doctors must address.
There are various methods of internal fixation for femoral neck fractures, with commonly used options including dynamic hip screws (DHSs) and multiple cannulated screws. Currently, the most widely used method is fixation with three cannulated cancellous screws (CCSs). However, there is no correlation among the three screws, and their positioning is susceptible to subjective and objective factors related to the surgeon. As a result, their resistance to vertical shear and torsion is relatively poor, which may lead to loosening and displacement of the fracture ends, avascular necrosis and nonunion of the femoral head, and shortening of the femoral neck [5]. There is still an early complication rate of 10–30%, including nonunion and internal fixation failure [6].
According to Pauwels, femoral neck fractures are classified into three types based on the the angle between the fracture line in the coronal plane and the superior margin of the acetabulum: Pauwels type I when the angle is less than 30°, type II when it ranges between 30° and 50°, and type III when the angle exceeds 50°. The greater the Pauwels angle is, the closer the fracture line is to the vertical direction, leading to increased shear forces at the fracture site and greater instability, which are often associated with a greater incidence of fixation failure and nonunion [7]. Studies report nonunion rates of 16–59% and avascular necrosis rates of 11–86% for unstable Pauwels type III femoral neck fractures [8]. The femoral neck system (FNS) was developed in 2017 by Stoffel et al. [9]. Combining the advantages of minimally invasive and angle-stable internal fixation systems offers a new option for femoral neck fracture treatment. The FNS comprises fixation plates, antirotation screws, tension screws, multifunctional targeting frames, and guide wire correctors, promoting treatment efficacy through comprehensive mechanical properties such as compression, antirotation, and shear resistance [10]. Biomechanical testing and finite element analysis have shown that the FNS integrates the advantages of minimally invasive cannulated screws while preserving more blood supply to the femoral head and maintaining stability and sliding compression, similar to dynamic hip screws (DHSs) [11, 12]. However, there is limited scholarly research on the sensitivity of the femoral neck system (FNS) and cannulated cancellous screws (CCSs) with respect to the Pauwels angle.
We conducted a retrospective statistical analysis of clinical data from January 2020 to December 2023, comprising 38 cases of internal fixation surgery for femoral neck fractures at our institution. We compared the short-term clinical efficacy of the femoral neck system (FNS) with that of cannulated cancellous screws (CCSs) in the treatment of femoral neck fractures. Furthermore, we explored the biomechanical differences between the two internal fixation methods for treating femoral neck fractures with different Pauwels angles. While the results of simulation experiments may not necessarily reflect reality, they can indicate the mechanical trends of different experimental subjects. Huang et al. [13] compared the mechanical differences between FNS and CCSs at Pauwels angles of 55°, 65°, and 75° and reported that FNS exhibited superior anti-displacement stability to CCS at 55° and 65°. We hypothesized that the superior mechanical performance of FNS may be related to variations in the Pauwels angle. Clarifying this mechanical feature may help increase our understanding of the value of FNS in terms of structural stability and anti-hip varus. These findings provide compelling evidence for objectively evaluating the role of FNS in treating femoral neck fractures.
Materials and methods
All methods in this study were conducted in accordance with relevant guidelines and regulations. All experimental protocols were approved by the Institutional Ethical Review Board of Zhangjiagang Fifth People’s Hospital (L2024004).
Clinical research
Inclusion and exclusion criteria
The inclusion criteria were as follows: (1) normal hip joint function on the injured side prior to injury; (2) fresh femoral neck fracture within 3 weeks; (3) age at injury ≤ 75 years; (4) willing to undergo FNS or CCS treatment; and (5) complete follow-up data.
The exclusion criteria were as follows: (1) concurrent severe medical conditions; (2) open fractures or pathological femoral neck fractures; (3) concurrent significant vascular, nerve, or organ injuries; (4) preexisting abnormal hip joint function; and (5) incomplete follow-up data.
Patient baseline data
A retrospective analysis of the clinical data of patients with femoral neck fractures treated in our hospital from January 2020 to December 2023 was conducted, with a total of 38 patients meeting the aforementioned criteria included in the study. Seventeen patients were treated with FNS fixation based on the results of doctor‒patient communication, and 21 patients were treated with CCS fixation. The general preoperative data of the two groups of patients are shown in Table 1. There were no statistically significant differences in age, sex, body mass index (BMI), cause of injury, side, Garden classification, or Pauwels classification between the two groups (P > 0.05).
Surgical methods
After general anaesthesia combined with sciatic nerve block anaesthesia, the patient lay supine on the traction bed. Closed reduction is attempted under fluoroscopy, and if unsuccessful after three attempts, Kocher’s needle is used for percutaneous leverage reduction, followed by open reduction through a small incision. Once satisfactory reduction is achieved under fluoroscopy, the traction bed maintains the reduction, and surgical procedures are performed.
FNS Group: Starting from the centre of the lesser trochanter plane, a 4-cm lateral longitudinal incision was made to expose the lateral aspect of the femur. A guide pin was inserted at an angle of 130° between the centre plane of the lesser trochanter and the femoral shaft, ensuring under fluoroscopy that the guide pin was centrally located in the femoral head and 5 mm below the cartilage. After depth measurement, a cannulated drill was used to create a medullary canal pathway, and a dynamic rod was inserted along the pathway to a depth of 5 mm below the cartilage, followed by removal of the central guide pin. A lateral sleeve plate was then inserted and snugly fit against the femoral shaft, with locking screws inserted along the plate. Using an anti-rotation guide, holes were drilled, and anti-rotation screws were inserted. If there was any detachment at the fracture ends under fluoroscopy, traction was released, and the black nut was rotated counterclockwise for intraoperative compression. If there was no detachment, the handle was slid downward, the wound was irrigated, and layered closure was performed.
CCS Group: Approximately 2 cm below the greater trochanter on the lateral cortex, a percutaneous incision was made parallel to the long axis of the femoral neck for the insertion of the first guide pin. Under fluoroscopy, the anteroposterior view shows the image close to the superior aspect of the femoral cortex, and the lateral view aligns with the midpoint of the femoral neck. The pin was advanced to 5 mm below the cartilage. Using a parallel guide, the second and third guide pins were inserted, closely following the anterior and posterior walls of the femoral neck and creating a triangular arrangement with the three guide pins. Hollow drills were used along the guide pins to create holes, and three hollow screws were inserted along the guide pins. Once fluoroscopy confirmed satisfactory screw positions, the guide pins were removed, the wound was irrigated, and layered closure was performed.
Perioperative management
Postoperatively, antibiotics were administered for prophylaxis for 24 h. Low-molecular-weight heparin sodium anticoagulation therapy was initiated 12 h postoperatively. On the second postoperative day, intravenous pumps were used to prevent thrombosis formation, and muscle contraction exercises of the affected limb were initiated along with passive knee and hip joint movements. Gradual sitting in bed was started within two weeks postoperatively, and non-weight-bearing activities were recommended for the first three months. The timing for abandoning crutches and walking without support was determined on the basis of imaging assessment of fracture healing within 3 months postoperatively.
Establishment of finite element models
General information
The orthopaedic clinic recruited a 50-year-old male volunteer with a height of 170 centimetres and a weight of 72 kg. The volunteer had no history of systemic disease, and there was no history of hip joint injury or surgery. Physical examinations and radiological assessments ruled out acute or chronic hip joint diseases. The volunteer provided informed consent for participation in this study and signed the informed consent form.
Establishment of the proximal femoral model and fracture model
The volunteers were positioned in a supine neutral posture, with both lower limbs relaxed and the pelvis leveled. The left hip joint was scanned via a 64-row CT scanner (GE Healthcare, USA). The CT images were stored in DICOM format and imported into the reverse modelling software Mimics 19.0 (Materialise, Belgium). Appropriate grayscale values were selected to distinguish bone and surrounding soft tissues. Commands such as region growing and mask editing from the tool panel were utilized to generate a three-dimensional model of the proximal femur. The model was saved as an STL file and imported into Geomagic Wrap 2017 (Geomagic, USA) software for smoothing, mesh division, and surface fitting. The skeletal solid model was constructed and saved as an IGS file. Next, the IGS femoral component was loaded into Pro/E 5.0 software (PTC, USA). A reference horizontal plane was established through the centre of the femoral head, and secondary reference planes were created at 30°, 40°, 50°, 60°, 70°, and 80° angles relative to the horizontal plane. The proximal femur model was then segmented via the secondary reference planes at various angles to simulate Pauwels type II-III femoral neck fractures.
Internal fixation model establishment and simulated surgery
The product manuals of the femoral neck system (FNS) provided by the American company Synthes and the cannulated cancellous screws (CCSs) offered by China Kangli Orthopaedic Instrument Co., Ltd., were referenced. Using Pro/E 5.0 software, models of both FNS and CCSs were separately created. The femoral neck system consists of four components: a plate, a bolt, an antirotation, and a locking nail. The locking plate serves as a 130° angle stabilizing device, and the locking nail has a diameter of 5 mm. The bolt has a length of 90 mm, a diameter of 8 mm, and a round head and is threadless. The anti-rotation component has a diameter of 6 mm, and after bolt tightening, it enhances the rotational resistance, improving the stability of the device. Each cannulated cancellous screw has a total length of 84 mm, a diameter of 4.2 mm, and a thread length of 22 mm. The established models of the two internal fixation systems and fracture models with different Pauwels angles were loaded into the assembly system of Pro/E 5.0 software for Boolean operations. After the overlapping geometric entities were removed, various types of fracture-internal fixation models were obtained. The assembly models were saved as Parasolid files separately (Fig. 1).
Mesh division and material properties
The Hypermesh 2014 software (Altair, USA) was used to open the fracture-internal fixation assembly file in Parasolid format. After completing geometric cleaning, tetrahedral elements are employed to mesh and discretize the assembly model. Typical four-node tetrahedral elements (T4) are used for meshing. Each part within the models is exported in INP format and saved, and mesh models for different assemblies are obtained.
The parts in the INP format are imported into Abaqus 6.14 software (Dassault, France) for material assignment. In this work, the internal fixation metal components are simplified as isotropic linear elastic materials. Due to the uneven distribution of material in the femur, referring to the results of previous studies, material assignment for each element is performed individually on the basis of the grayscale value formula. The apparent density [\(\:\rho\:(Kg/{m}^{3})\)] and Young’s modulus [E(MPa)] of the bone are calculated from the HU values of the CT scans (with water density as the reference for zero calibration) according to the following formula [14]:
The material details of each component are shown in Table 2.
Load and boundary condition settings
In research conducted by Freitas et al. [15], a load equivalent to the force exerted while standing on a single leg was applied to the corresponding cartilage surface of the femoral head, producing a joint reaction force of 1800 N, α = 69° and β = 7° (Fig. 2). To prevent femoral motion during the analysis process, the distal end of the femur was constrained in all directions of freedom [16]. Frictional contact conditions were established, with a friction coefficient of 0.46 between the fracture ends, 0.42 between the bone and the implant, and 0.2 between the implants [17].
A 54-year-old woman in the FNS group experienced left hip pain and limited mobility after being hit by a motor vehicle. (a) Preoperative radiographs showed a left femoral neck fracture (Garden IV, Pauwels III). (b) Postoperative anteroposterior and lateral X-rays demonstrated satisfactory fracture reduction and an acceptable position of the internal implant. (c, d) Anteroposterior X-rays at 3 and 12 months postoperatively revealed fracture healing. Another 50-year-old male in the FNS group developed left hip pain and restricted movement following a fall. (e) Preoperative radiographs indicated a left femoral neck fracture (Garden III, Pauwels II). (f) Postoperative anteroposterior and lateral X-rays showed satisfactory fracture reduction and an acceptable position of the internal implant. (g, h) Anteroposterior X-rays at 3 and 20 months postoperatively displayed fracture healing. In the CCS group, a 52-year-old male experienced right hip pain and restricted movement after being struck by a heavy object. (i) Preoperative radiographs revealed a right femoral neck fracture (Garden IV, Pauwels II). (j) Postoperative anteroposterior and lateral X-rays demonstrated satisfactory fracture reduction and an acceptable position of the internal implant. (k, l) Anteroposterior X-rays at 3 and 17 months postoperatively showed fracture healing. Another 63-year-old female in the CCS group developed left hip pain and restricted movement after a fall. (m) Preoperative radiographs indicated a left femoral neck fracture (Garden IV, Pauwels II). (n) Postoperative anteroposterior and lateral X-rays showed satisfactory fracture reduction and an acceptable position of the internal implant. (o, p) Anteroposterior X-rays at 3 and 12 months postoperatively displayed fracture healing
Convergence test
In this study, we conducted convergence tests using tetrahedral meshes with three resolutions. The results indicate that the equivalent stress values calculated with Mesh2 are close to those obtained with Mesh1. Accordingly, the femur and internal fixation meshes were further subdivided into sizes ranging from 0.5 to 1.0 mm to generate meshes and elements. The element and node counts for the three finite element models are presented in Table 3.
Observation indicators
Clinical indicators
Postoperatively, we conducted follow-ups on patients for 12 ± 6 months. Records were made and compared between the two groups of patients for surgical time (from the start of surgery to skin closure), blood loss, incision length, intraoperative fluoroscopy frequency, length of hospital stay, time to fracture healing, Harris hip function score at the last follow-up, pain-related VAS score, changes in the hip internal rotation angle, and femoral neck shortening length (the difference in femoral head position between immediate postoperative and last follow-up radiographs) [18]. Routine postoperative radiographs were used to assess fracture reduction quality (Grade I: AP 160°, Lateral 180°; Grade II: AP 155°, Lateral 180°; Grade III: AP < 155° or Lateral > 180°; Grade IV: AP < 150°, Lateral > 180°; among these, Grades III and IV are considered to indicate poor reduction quality [19]), healing status, and internal fixation position. The complications considered included incisional infection, loosening or failure of internal fixation, nonunion of fractures (defined by the U.S. Food and Drug Administration as no significant change in the fracture gap after 9 months postfracture or 3 consecutive months), and femoral head necrosis.
FEA indicators
Comparisons were made between two types of internal fixation in different femoral fracture models, including maximum stress on the proximal femoral fracture fragment (predicting the risk of secondary fractures), maximum displacement, and internal rotation angle (spatial indicators predictive of prognosis), maximum relative displacement at the fracture site (assessing the risk of nonunion, this practical approach has been used in our study of fracture surface distance measurements [20]), maximum stress on internal fixation (assessing the risk of failure), stiffness, and maximum displacement of internal fixation (assessing stability). Additionally, observing femoral displacement clouds, displacement, and stress clouds via the two internal fixation methods can clarify the displacement and stress distributions.
Statistical analysis
Continuous variables are presented as the means ± standard deviations (SDs). The normality test uses the Shapiro‒Wilk test to determine whether the data meet the application conditions of the Student’s t test. If the data do not conform to a normal distribution, consideration is given to using a nonparametric alternative method. The data were assessed via Student’s t test. Categorical variables were analysed via the chi-square test. The Mann‒Whitney U test was employed for ranked data. All the statistical analyses were conducted via SPSS 26.0 (SPSS Inc., Chicago, IL, USA). A significance level of p < 0.05 was considered statistically significant.
Results
Clinical outcomes of the two surgical procedures
In total, 38 patients under the age of 75 years were enrolled, with surgeries performed via the FNS method in 17 patients and the CCS method in 21 patients. The follow-up duration ranged from 3 to 22 months (mean 6.3 ± 5.2 months). The analysis results are as follows (Table 4).
The operative time, blood loss, incision length, and incidence of complications were not significantly different between the two groups (p > 0.05). However, patients receiving FNS treatment had a lower fluoroscopy frequency (15.1 ± 3.5 vs. 18.6 ± 5.0, p = 0.019) and shorter hospital stays (12.5 ± 3.3 vs. 16.4 ± 5.4 mL, p = 0.014). The fracture healing time in the FNS group was 3.8 ± 0.8 months, which was significantly shorter than that in the CCS group (5.4 ± 3.9 months; p = 0.002).
The HHS of the FNS group was significantly greater than that of the CCS group (89.2 ± 4.0 vs. 83.6 ± 4.7, p < 0.001), whereas the VAS pain score at the last follow-up was lower in the former group than in the latter group (0.9 ± 1.1 vs. 2.0 ± 1.4, p = 0.014).
The change in NSA was lower in the FNS group than in the CCS group (1.5 ± 1.7 vs. 2.9 ± 1.9°, p = 0.021). Both groups experienced femoral neck shortening postoperatively. Femoral neck shortening was significantly less common in the FNS group than in the CCS group (1.4 ± 1.4 mm vs. 4.2 ± 2.7 mm, p < 0.001).
Comparison of the maximum stress in the proximal fracture fragment
The maximum stress measurements of the proximal femoral fractures in the different models are shown in Fig. 4a. The maximum stress of the proximal fracture in the CCS group was always greater than that in the FNS group. From the perspective of the changing trend, the maximum stress of the former decreased with increasing PauWels angle, rebounded to the maximum value after 60°, and then decreased. The CCS group achieved the maximum value of 242.4 MPA when the Pauwels angle was 70°, whereas the maximum stress of the latter increased slowly with increasing PauWels angle, and the maximum value of 127.0 MPa was obtained at 70°. The risk of fatigue fracture of the proximal femur in the FNS group was lower than that in the CCS group.
Biomechanical properties comparison in different finite element models. (a) Peak stress of the proximal fracture fragment; (b) Max displacement of the proximal fragment; (c) Varus angle of the proximal fracture fragment; (d) Max displacement of fracture surface at the broken end; (e) Peak stress of the proximal internal fixation; (f) Max displacement of internal fixation. Change (%) = (FNS value – CCS value) / CCS value * 100%
Comparison of the maximum displacement and displacement distribution of the proximal fracture fragment
The maximum displacement of the proximal femoral fragment of the two internal fixation methods in the different fracture models gradually increased as the Pauwels angle increased, as shown in Fig. 4b. The displacement of the proximal femoral fracture fragment in the FNS group only exceeded that in the CCS group at 60° and 70°. The numerical difference between the FNS group and the CCS group was the largest at 30°, with values of 2.6 and 2.9 mm, respectively, whereas the difference between the two groups was 80°. The minimum values were both 4.8 mm. The displacement cloud diagram shows that when the angle in the FNS group was between 30° and 60°, the transition of the equivalent displacement cloud diagram between the femoral head and the diaphysis was still gentle, indicating that the displacements of the femoral head and the diaphysis were generally coordinated, whereas during the period of 70° to 80°, the transition of the equivalent displacement cloud between the femoral head and the diaphysis was smooth. There was an obvious interruption in the diaphyseal displacement cloud map, indicating that the magnitude of femoral head displacement increased. The change trend of the femoral head displacement nephogram in the CCS group was similar to that in the FNS group, but the degree of femoral head displacement did not increase significantly until 80° was reached (Fig. 5). These findings indicate that the stability of FNS fixation of the proximal femur is slightly better than that of CCS fixation.
Femoral head varus angle comparison
Figure 4c illustrates the changing trends of the femoral head varus angle in different fracture models with two types of internal fixation. As the Pauwels angle increased, both the FNS and CCS groups presented an increase in the femoral head varus angle, reaching their respective maximum values at 80°, which were 4.2° and 4.5°, respectively. The smallest difference in varus angle values between the two groups occurred at 70°, with values of 3.7° and 3.7°, respectively. These findings suggest that FNS is more effective than CCS in resisting femoral head varus.
Comparison of the maximum relative displacement of the fracture surface
We examined the maximum relative displacement between the fracture sections for the two internal fixation methods, as shown in Fig. 4d. In contrast to the results of the comparison of the femoral head varus angle, although the relative maximum displacement of the fracture sections in both the FNS and CCS groups increased with increasing Pauwel angle, the FNS group exhibited more significant activity here. The values in the FNS group surpassed those in the CCS group, with the difference peaking at 68.9% at 60°. This reflects that FNS is less effective than CCS in stabilizing the fracture ends.
Comparison of the maximum stress and stress distributions of the two types of internal fixation
The results of the maximum stress tests for the two internal fixation methods are shown in Fig. 4e. As the Pauwels angle increases, both internal fixation methods show an increasing trend in maximum stress. In the different fracture models, the maximum stress in the FNS group’s internal fixation exceeds that in the CCS group, with the difference peaking at 101.3% at 70°. Figure 6 displays stress contour maps for both internal fixation methods, revealing that high-stress regions for both methods appear near the fracture section. However, the FNS high-stress region is significantly more extensive than the CCS region. This suggests that the risk of failure associated with the FNS is greater than that with the CCSs.
Comparison of the maximum displacement, stiffness and displacement distributions of the two internal fixations
Figure 4f shows that under the action of the load, the trends of the maximum displacement changes for the two internal fixation methods are similar to the trends in the stress changes. The maximum displacement of the FNS was only slightly greater than that of the CCS group by 0.3% at 70°, whereas in the other models, it maintained lower values. In the comparison of stiffness, the intermediate value of FNS stiffness was 572.5 N/mm, exceeding that of CCS, which was 530.2 N/mm, indicating that FNS has good structural stability (Fig. 7). The stress contour maps illustrate the displacement distribution for the two internal fixations (Fig. 8), and with reference to the femoral head displacement contour map shown in Fig. 5, the maximum displacement occurred in the proximal region associated with the activity of the femoral head.
Discussion
In this study, we investigated the short-term efficacy of the FNS and CCSs in treating femoral neck fractures and conducted clinical follow-ups to assess joint function and radiographic data. Moreover, we explored the differences in the mechanical performance of the two internal fixation methods in treating femoral neck fractures with different Pauwels angles through finite element analysis. Our study is organized as follows. First, compared with those in the CCS group, patients in the FNS group had higher postoperative hip joint scores and less radiographic evidence of reduction loss. Second, employing finite element analysis, in addition to confirming that FNS offers better stability than CCS, we also observed that as the Pauwels angle increases, the advantages of the FNS over CCSs in terms of stability and anti-hip varus tend to diminish.
Due to the unique anatomical structure of the femoral neck, blood vessels are highly vulnerable to damage when fractures occur [21]. The success of surgery requires not only anatomical reduction but also strong internal fixation, protecting the fragile blood supply and providing a stable environment for bone remodelling, which can reduce the incidence of femoral head necrosis and nonunion [22]. There is still controversy regarding the choice of internal fixation for femoral neck fractures. Traditional internal fixation devices such as dynamic hip screws and hollow pressure screws have a relatively high rate of complications, affecting patient prognosis and quality of life. To meet clinical needs, new internal fixation devices must inherit the advantages of traditional devices and improve upon their shortcomings. The FNS, as a plate-screw system, provides effective angular and rotational stability through the design of antirotation and locking screws [9], thus achieving stronger fixation. In clinical studies, the FNS has been shown to be an effective treatment for Pauwels III fractures, with faster recovery rates and fewer complications [23]. With the introduction of the concept of rapid recovery, an increasing number of hip fracture patients are recommended for early weight-bearing exercises. Evidence from cellular, animal, computer model, and clinical studies has shown that mechanical loading from weight-bearing aids in accelerating fracture healing [24, 25]. Early weight-bearing can reduce hospital stay, postoperative pain, and mortality rates while improving joint function [26, 27]. However, due to concerns about the fixation strength and reliability of internal fixation devices, many conservative doctors still recommend prolonged bed rest. Recently, Kenmegne et al. [28] conducted a series of clinical studies and reported that the fracture healing time in the FNS group was significantly shorter than that in the CCS group (p < 0.05). FNS, as a novel internal fixation device, has a greater design strength than CCS and offers better stability and lower failure risk in the face of high-stress fractures, such as unstable fractures [28]. Zhang et al. [29] reported through a meta-analysis that patients in the FNS group were able to mobilize earlier than those in the CCS group. Additionally, the shorter fracture healing period observed in the FNS group can provide additional confidence in rehabilitation, thus encouraging early weight-bearing and improving patient outcomes. Similar to the results of the previously published meta-analysis [30], the results of this study show that, compared with the CCS group, the FNS group had less intraoperative blood loss, shorter incisions, significantly reduced intraoperative fluoroscopy times, significantly shorter hospital stays, and earlier postoperative full weight-bearing walking times. Although a large amount of research shows that compression and micromotion at the fracture site can promote fracture healing, this healing theory for the femoral neck should be based on effective control of shear forces [10, 13, 31]. Unlike the parallel placement of hollow screws, the unique nail plate locking and angular structure of FNS prevent sliding of the femoral head, providing greater stability to the femoral head and effectively preventing femoral neck shortening. The antirotation screw design in the FNS, with a 7.5° angle to the tension screw, can effectively resist rotation, provide good biomechanical stability, prevent the “Z” effect on the femoral head, and effectively resist vertical shear forces. The design of the tension screw tip thread firmly grasps the fracture end, providing strong active compression during surgery; linear insertion maintains effective fracture reduction; and providing angular stability effectively prevents reduction loss [5].
Femoral neck shortening commonly occurs after femoral neck fractures, potentially leading to symptoms such as limb pain, limping, and fixation failure. The International Society for Fracture Repair acknowledges that effective resistance to varus and rotational forces is necessary for treating femoral neck fractures and that appropriate axial stress facilitates fracture healing [32]. Hollow screw designs allow compression through sliding of fracture fragments during healing; however, excessive absorption of fracture ends, especially in cases of comminuted fractures, can lead to significant shortening of the femoral neck or even screw cut-out. Stoffel et al. [9] reported that over half of patients experienced femoral neck shortening exceeding 5 mm, with nearly one-third experiencing shortening greater than 10 mm, severely impacting limb function. In our study, both groups had femoral neck shortening of less than 5 mm, with FNS demonstrating superior fixation performance and stronger stability, resulting in significantly less femoral neck shortening than that in the CCS group. However, some degree of shortening still occurred, with good hip joint mobility postoperatively. Hu et al. [33] compared the efficacy of FNS and three hollow screws and reported that both groups experienced femoral neck shortening postoperatively, with the FNS group exhibiting significantly less shortening than the three hollow screws group did, which is consistent with our findings and literature reports. Thus, the FNS system provides greater stability at the fracture site. Additionally, the incidence of complications was lower in the FNS group than in the CCS group in this study. Similar to our study, Tang et al. [34] compared FNS and inverted hollow cancellous screws and reported that angular fixation devices may have better resistance to varus deformity and micromotion than traditional triangular screws. The FNS has yielded promising clinical results in resisting femoral neck shortening and complications.
The previous text reviewed and analysed the efficacy and pros and cons of the FNS and CCSs in fixing femoral neck fractures, highlighting the importance of comparative evaluation for clinical application. To further explore the mechanical differences between these two internal fixation methods in treating femoral neck fractures with different Pauwels angles, we designed a finite element simulation experiment. Compared with that in the CCS group, the maximum stress value of the proximal fracture block in the FNS group was lower, with the former fluctuating between 120 and 240 MPa and the latter fluctuating around 120 MPa. These findings indicate that, compared with the FNS group, the CCS group has a greater risk of femoral head fracture and collapse. When the FNS is used, the risk of internal fixation loosening, cutting, and femoral fractures is minimal, effectively protecting the integrity of the bone near the fracture. This trend aligns with the finite element study conducted by Xia et al. [35], which simulated a Pauwels angle of 70° Pauwels III femoral neck fracture and observed the biomechanical performance of different devices after applying a load of 2100 N. The results revealed that the maximum stress value of the bone in the FNS group was 107.9 MPa, whereas it was 486.3 MPa in the CCS group. In the present study, relative to the proximal bone block, the internal fixation device resulted in greater stress. With increasing Pauwels angle, the maximum stress of both internal fixations tended to increase. In the different fracture models, the maximum stress of internal fixation in the FNS group exceeded that of the CCS group, with the difference reaching a peak of 101.3% in the Pauwels 70° model. The stress distribution was mainly concentrated on the screw surface near the fracture line, with the FNS group bearing the maximum stress among the groups. Although the FNS bears greater stress, the internal fixation displacement test revealed that the FNS is more stable overall than the CCSs, with a stiffness exceeding that of the latter by 7.9%. This finding indicates that FNS has greater strength after internal fixation, making it less prone to deformation, loss of reduction, and other complications. The superiority of the femoral neck internal fixation system over hollow screws can be explained as follows. Within the femoral neck internal fixation system, dynamic hip screws and locking antirotation screws provide robust angular support and effectively maintain the fracture in the proper position. Compared with the use of a hollow screw in conjunction with a dynamic hip screw, the femoral neck internal fixation system locks the locking antirotation screw with the main screw more securely, forming a unified whole and providing better antirotation action. However, inserting a 5-mm-diameter locking screw at the distal end of the locking plate can integrate the locking plate and femoral shaft into a single entity. Therefore, biomechanically, the femoral neck internal fixation system offers better anchoring than the hollow screw fixation system does, helping to reduce stress on the proximal femur and decrease displacement of both the femur and internal fixation implants, thereby creating a favourable mechanical environment for fracture healing.
Mechanical experiments indicate that, compared with CCSs, the FNS is more effective in preventing femoral neck shortening [9]. In the face of unstable femoral neck fractures, CCSs result in a lower ultimate load-bearing capacity [36]. With an increase in the Pauwels angle, the shear force becomes the primary external force leading to internal fixation failure [37]. CCSs lack sufficient angular stability and have a relatively poor ability to withstand shear stress. In finite element analysis of Pauwels III fractures, the distal double-hole FNS demonstrated stronger biomechanical stability and lower failure risk than the CCSs [38]. In this study, we extensively compared the differences in the femoral head varus angle and displacement between the FNS and CCSs in femoral neck fractures with different Pauwels angles. Similar to previous reports, we found that the FNS indeed has some advantages in resisting femoral head varus and constraining displacement. However, between Pauwels angles of 30–70°, the advantage of the FNS gradually diminishes with increasing Pauwels angle, reflecting that the superiority of the FNS over CCSs is conditionally limited and that the increase in shear stress poses a significant challenge to the stability of FNS. Interestingly, as the Pauwels angle increased, the separation displacement of the upper wall of the femoral neck also increased, with the FNS resulting in greater separation displacement than CCSs. Given that the FNS provides central fixation while CCSs offer distributed fixation, the lever arm of the FNS causing separation of the fracture ends is greater than that of CCSs. The same physiological load can result in greater separation displacement of the fracture ends in the FNS group. Although this difference has not been clinically confirmed to have adverse effects on fracture healing, our study indicates that the FNS is not a flawless device.
This study has several limitations: (1) The clinical research involved retrospective analysis, with nonrandom patient selection, potentially introducing selection bias. In the measurement of femoral neck shortening, errors may exist due to nonstandard patient positioning during X-ray imaging. The duration of FNS surgery was relatively short, and the follow-up period in the study was insufficient, providing only early reports on postoperative complications such as femoral neck shortening, nonunion, and avascular necrosis of the femoral head. Further long-term efficacy assessments require additional follow-up observations. (2) The finite element modelling method treats fractures as flat surfaces, whereas real fracture ends are often jagged and uneven contact surfaces, resulting in some disparity between the model and reality. Furthermore, whether the mechanical conclusions of the CCS obtained from this study can cover all clinical application scenarios still requires further verification. (3) The experiment applied a single load (joint reaction force) without considering the tensile effects of muscles around the greater and lesser trochanters. Future research should consider the impact of muscles around the hip joint on femoral loading.
Conclusion
In summary, the FNS demonstrates superior clinical efficacy compared with CCS in treating femoral neck fractures, with the former being more beneficial for improving hip joint function. Biomechanical research results confirm the advantages of FNS in terms of structural stability and anti-hip varus effects. However, as the Pauwels angle increases, the superiority of the FNS over CCSs is conditional, as significant shear stress still poses a challenge to the fixation effect of the FNS.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
- FNS:
-
Femoral neck system
- CCS:
-
Cannulated cancellous screws
- DHS:
-
dynamic hip screws
- FEA:
-
Finite element analysis 3D: Three-dimensional
- Harris:
-
Harris Hip Score
- VAS:
-
Visual Analog Scale for Pain
- NSA:
-
Neck shaft angle
References
Zelle BA, Salazar LM, Howard SL, Parikh K, Pape HC. Surgical treatment options for femoral neck fractures in the elderly. Int Orthop. 2022;46(5):1111–22. https://doi.org/10.1007/s00264-022-05314-3
Miller BJ, Callaghan JJ, Cram P, Karam M, Marsh JL, Noiseux NO. Changing trends in the treatment of femoral neck fractures: a review of the American board of orthopaedic surgery database. J Bone Joint Surg Am. 2014;96(17):e149. https://doi.org/10.2106/JBJS.M.01122
Roberts KC, Brox WT, Jevsevar DS, Sevarino K. Management of hip fractures in the elderly. J Am Acad Orthop Surg. 2015;23(2):131–7. https://doi.org/10.5435/JAAOS-D-14-00432
Zuckerman JD. Hip fracture. N Engl J Med. 1996;334(23):1519–25. https://doi.org/10.1056/NEJM199606063342307
Su M, He Z, Huang N, Lin X, Fang K, Dai Z. Superior short-term outcomes of FNS in combination with a cannulated screw in treating femoral neck fractures. BMC Musculoskelet Disord. 2023;24(1):823. https://doi.org/10.1186/s12891-023-06959-w
Yang JJ, Lin LC, Chao KH, Chuang SY, Wu CC, Yeh TT, et al. Risk factors for nonunion in patients with intracapsular femoral neck fractures treated with three cannulated screws placed in either a triangle or an inverted triangle configuration. J Bone Joint Surg Am. 2013;95(1):61–9. https://doi.org/10.2106/JBJS.K.01081
Bartonícek J. Pauwels’ classification of femoral neck fractures: correct interpretation of the original. J Orthop Trauma. 2001;15(5):358–60. https://doi.org/10.1097/00005131-200106000-00009
Liporace F, Gaines R, Collinge C, Haidukewych GJ. Results of internal fixation of Pauwels type-3 vertical femoral neck fractures. J Bone Joint Surg Am. 2008;90(8):1654–9. https://doi.org/10.2106/JBJS.G.01353
Stoffel K, Zderic I, Gras F, Sommer C, Eberli U, Mueller D, et al. Biomechanical evaluation of the femoral Neck System in Unstable Pauwels III femoral Neck fractures: a comparison with the dynamic hip screw and cannulated screws. J Orthop Trauma. 2017;31(3):131–7. https://doi.org/10.1097/BOT.0000000000000739
Yan SG, Cui Y, Li D, Liu F, Hua X, Schmidutz F. Femoral Neck System versus three cannulated screws for fixation of femoral Neck fractures in younger patients: a retrospective cohort study. J Invest Surg. 2023;36(1):2266752. https://doi.org/10.1080/08941939.2023.2266752
Teng Y, Zhang Y, Guo C. Finite element analysis of femoral neck system in the treatment of Pauwels type III femoral neck fracture. Med (Baltim). 2022;101(28):e29450. https://doi.org/10.1097/MD.0000000000029450
Jiang X, Liang K, Du G, Chen Y, Tang Y, Geng K. Biomechanical evaluation of different internal fixation methods based on finite element analysis for Pauwels type III femoral neck fracture. Injury. 2022;53(10):3115–23. https://doi.org/10.1016/j.injury.2022.08.038
Huang SL, Zhang YZ, Zhang X, Zhou CQ, Li WB, Wang YQ, et al. Comparison of femoral neck system and three cannulated cancellous screws in the treatment of vertical femoral neck fractures: clinical observation and finite element analysis. Biomed Eng Online. 2023;22(1):20. https://doi.org/10.1186/s12938-023-01083-1
Xue H, Bai H, Zhou R, Wang J, Zhou B, Wang X, et al. Novel Design of the compound sleeve and stem prosthesis for treatment of proximal femur bone defects based on Topology optimization. Front Bioeng Biotechnol. 2022;10:938337. https://doi.org/10.3389/fbioe.2022.938337
Freitas A, Toledo Júnior JV, Ferreira Dos Santos A, Aquino RJ, Leão VN. Péricles De Alcântara W. Biomechanical study of different internal fixations in Pauwels type III femoral neck fracture - A finite elements analysis. J Clin Orthop Traum. 2021;14:145–50. https://doi.org/10.1016/j.jcot.2020.06.006
Liu Y, Song W, Liang H, Li C, Niu W, Shao H, et al. Comparison of femoral mechanics before and after internal fixation removal and the effect of sclerosis on femoral stress: a finite element analysis. BMC Musculoskelet Disord. 2022;23(1):930. https://doi.org/10.1186/s12891-022-05888-4
Wang Y, Chen W, Zhang L, Xiong C, Zhang X, Yu K, et al. Finite element analysis of proximal femur bionic nail (PFBN) compared with proximal femoral nail antirotation and InterTan in treatment of intertrochanteric fractures. Orthop Surg. 2022;14(9):2245–55. https://doi.org/10.1111/os.13247
Felton J, Slobogean GP, Jackson SS, Della Rocca GJ, Liew S, Haverlag R, et al. Femoral Neck Shortening after hip fracture fixation is Associated with Inferior hip function: results from the FAITH trial. J Orthop Trauma. 2019;33(10):487–96. https://doi.org/10.1097/BOT.0000000000001551
Garden RS. Stability and union in subcapital fractures of the femur. J Bone Joint Surg Br. 1964;46:630–47. PMID: 14251448.
Sun J, Wu L, Fang N, Liu L. IFM calculator: an algorithm for interfragmentary motion calculation in finite element analysis. Comput Methods Programs Biomed. 2024;244:107996. https://doi.org/10.1016/j.cmpb.2023.107996
Hoaglund FT, Low WD. Anatomy of the femoral neck and head, with comparative data from caucasians and Hong Kong Chinese. Clin Orthop Relat Res. 1980;152:10–6. PMID: 7438592.
Zhao G, Liu C, Chen K, Lyu J, Chen J, Shi J et al. Nonanatomical reduction of femoral Neck fractures in Young patients (≤ 65 years old) with internal fixation using three parallel cannulated screws. Biomed Res Int 2021:3069129. https://doi.org/10.1155/2021/3069129
Zhou XQ, Li ZQ, Xu RJ, She YS, Zhang XX, Chen GX, et al. Comparison of early clinical results for femoral Neck System and Cannulated screws in the treatment of unstable femoral Neck fractures. Orthop Surg. 2021;13(6):1802–9. https://doi.org/10.1111/os.13098
Kubiak EN, Beebe MJ, North K, Hitchcock R, Potter MQ. Early weight bearing after lower extremity fractures in adults. J Am Acad Orthop Surg. 2013;21(12):727–38. https://doi.org/10.5435/JAAOS-21-12-727
Donohoe E, Roberts HJ, Miclau T, Kreder H. Management of Lower Extremity fractures in the Elderly: a Focus on Post-operative Rehabilitation. Injury. 2020;51(2):118–22. https://doi.org/10.1016/j.injury.2020.04.050
Kuru T, Olçar HA. Effects of early mobilization and weight bearing on postoperative walking ability and pain in geriatric patients operated due to hip fracture: a retrospective analysis. Turk J Med Sci. 2020;50(1):117–25. https://doi.org/10.3906/sag-1906-57
Atzmon R, Drexler M, Ohana N, Nyska M, Palmanovich E, Dubin J. The effect of postoperative weight-bearing status on mortality rate following proximal femoral fractures surgery. Arch Orthop Trauma Surg. 2022;142(6):947–53. https://doi.org/10.1007/s00402-020-03721-y
Kenmegne GR, Zou C, Fang Y, He X, Lin Y, Yin Y. Femoral neck fractures in non-geriatric patients: femoral neck system versus cannulated cancellous screw. BMC Musculoskelet Disord. 2023;24(1):70. https://doi.org/10.1186/s12891-023-06140-3
Zhang J, Chang X, Sun Z, Tang X. Comparison of femoral neck system versus cannulated compression screws in treating femoral neck fractures: a systematic review and meta-analysis. Asian J Surg. 2023;46(8):3259–60. https://doi.org/10.1016/j.asjsur.2023.03.013. Epub 2023 Mar 16.
Jiang J, Chen J, Xing F, Liu H, Xiang Z. Comparison of femoral neck system versus cannulated screws for treatment of femoral neck fractures: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2023;24(1):285. https://doi.org/10.1186/s12891-023-06378-x
Ma J, Zhao Z, Zhi X, Wang H, Wang W. Finite element comparative analysis of three different internal fixation methods in the treatment of Pauwels type III femoral neck fractures. BMC Musculoskelet Disord. 2022;23(1):1030. https://doi.org/10.1186/s12891-022-06003-3
Wang JG, Wu JX, Li YM, Xu YY. Biomechanical analysis of the closed reduction internal fixation with cannulated screw of femoral neck fractures. Med (Baltim). 2021;100(8):e24834. https://doi.org/10.1097/MD.0000000000024834
Hu H, Cheng J, Feng M, Gao Z, Wu J, Lu S. Clinical outcome of femoral neck system versus cannulated compression screws for fixation of femoral neck fracture in younger patients. J Orthop Surg Res. 2021;16(1):370. https://doi.org/10.1186/s13018-021-02517-z
Tang Y, Zhang Z, Wang L, Xiong W, Fang Q, Wang G. Femoral neck system versus inverted cannulated cancellous screw for the treatment of femoral neck fractures in adults: a preliminary comparative study. J Orthop Surg Res. 2021;16(1):504. https://doi.org/10.1186/s13018-021-02659-0
Xia Y, Zhang W, Hu H, Yan L, Zhan S, Wang J. Biomechanical study of two alternative methods for the treatment of vertical femoral neck fractures - a finite element analysis. Comput Methods Programs Biomed. 2021;211:106409. https://doi.org/10.1016/j.cmpb.2021.106409
Panteli M, Rodham P, Giannoudis PV. Biomechanical rationale for implant choices in femoral neck fracture fixation in the non-elderly. Injury. 2015;46(3):445–52. https://doi.org/10.1016/j.injury.2014.12.031
Davidovitch RI, Jordan CJ, Egol KA, Vrahas MS. Challenges in the treatment of femoral neck fractures in the nonelderly adult. J Trauma. 2010;68(1):236–42. https://doi.org/10.1097/TA.0b013e3181c428ce
Fan Z, Huang Y, Su H, Jiang T. How to choose the suitable FNS specification in young patients with femoral neck fracture: a finite element analysis. Injury. 2021;52(8):2116–25. https://doi.org/10.1016/j.injury.2021.05.043
Acknowledgements
We thank the School of Medicine of Tongji University, Shanghai SIEG Machinery Co., Ltd. and Zhangjiagang First People’s Hospital for theoretical guidance and technical support.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
Z.X. and F.H. contributed to the research design and implementation, and made in-depth discussions on research hotspots and technical difficulties. J.S., J.X.Z., Y.P.S. and S.P.F. contributed to model development and data acquisition. J.J.L., Z.R.W and Y.G. contributed to clinical data collection and data acquisition. Z.X., H.Z. and S.J.T. analyzed and interpreted the data and drafted the manuscript. All authors approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This research does not involve any content that violates any personal rights of the subjects. The participation in the study was voluntary and written informed consent was obtained from the participants. This study conforms to the provisions of the Declaration of Helsinki and has been reviewed and approved by the Institutional Review Board of Zhangjiagang Fifth People’s Hospital (L2024004). All protocols are carried out in accordance with relevant guidelines and regulations.
Human Ethics and Consent to participate declarations
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
All authors declare that they have no conflict of interest.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Xu, Z., Sun, J., Li, J. et al. Comparative analysis of the femoral neck system (FNS) vs. cannulated cancellous screws (CCS) in the treatment of Middle-aged and elderly patients with femoral neck fractures: clinical outcomes and biomechanical insights. BMC Musculoskelet Disord 25, 735 (2024). https://doi.org/10.1186/s12891-024-07863-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-024-07863-7