Abstract
Background
Lipodystrophy is characterized by progressive loss of adipose tissue and consequential metabolic abnormalities. With new treatments emerging for lipodystrophy, there is a growing need to understand the prevalence of specific comorbidities that may be commonly associated with lipodystrophy to contextualize the natural history of lipodystrophy without any disease modifying therapy.
Objective
To examine the risk of specific clinical characteristics in people living with lipodystrophy (LD) in 2018–2019 compared with the general US population, among the commercially insured US population.
Methods
A retrospective cohort study was conducted using the 2018–2019 Clinformatics® Data Mart database. An adult LD cohort (age ≥ 18 years) with at least ≥ 1 inpatient or ≥ 2 outpatient LD diagnoses was created. The LD cohort included non-HIV-associated LD (non-HIV-LD) and HIV-associated LD (HIV-LD) subgroups and compared against age- and sex-matched control groups with a 1:4 ratio from the general population with neither an LD or an HIV diagnosis using odds ratios (ORs) with 95% confidence intervals.
Results
We identified 546 individuals with non-HIV-LD (mean age, 60.3 ± 14.9 years; female, 67.6%) and 334 individuals with HIV-LD (mean age, 59.2 ± 8.3 years; female, 15.0%) in 2018–2019. Compared with the general population, individuals with non-HIV-LD had higher risks (odds ratio [95% confidence interval]) for hyperlipidemia (3.32 [2.71–4.09]), hypertension (3.58 [2.89–4.44]), diabetes mellitus (4.72 [3.85–5.79]), kidney disease (2.78 [2.19–3.53]), liver fibrosis or cirrhosis (4.06 [1.66–9.95]), cancer (2.20 [1.59–3.01]), and serious infections resulting in hospitalization (3.00 [2.19–4.10]). Compared with individuals with HIV, those with HIV-LD have higher odds of hypertension (1.47 [1.13–1.92]), hyperlipidemia (2.46 [1.86–3.28]), and diabetes (1.37 [1.04–1.79]).
Conclusions
LD imposes a substantial burden on affected individuals due to a high prevalence of metabolic comorbidities and other complications as compared with the general non-LD population. Future longitudinal follow-up studies investigating the causality between LD and observed comorbidities are warranted.
Similar content being viewed by others
Background
Lipodystrophy (LD) is a group of rare disorders of selective deficiency of adipose tissue affecting various areas of the body and is associated with significant metabolic abnormalities [1]. LD is classified into generalized LD (GLD) and partial LD (PLD), which are characterized by near-complete loss or selective loss of adipose tissue, respectively. Both GLD and PLD are sub-divided into genetic (i.e. congenital GLD and familial PLD) and acquired subtypes (i.e. acquired GLD and acquired PLD) based on etiology [2, 3]. HIV-associated LD (HIV-LD) is a distinct subtype of acquired PLD and is the most prevalent type of LD [4, 5]. Although abnormal fat distribution appears in varying presentations, HIV-LD tends to represent peripheral subcutaneous fat loss (i.e. lipoatrophy) with or without central fat accumulation (i.e. lipohypertrophy) [6, 7]. While the exact etiology of HIV-LD is still unknown, there is growing evidence indicating that HIV-associated lipoatrophy is associated with the older thymidine analog-containing highly active antiretroviral therapies stavudine and zidovudine [6, 8, 9]. The presentation of HIV-associated lipoatrophy is similar to that seen in non-HIV-associated LD (non-HIV-LD), while HIV-associated lipohypertrophy shares similar features with metabolic syndrome [10,11,12].
LD is commonly associated with metabolic comorbidities, including dyslipidemia, elevated triglyceride levels, insulin resistance/diabetes, metabolic dysfunction-associated steatotic liver disorder (MASLD), recurrent acute pancreatitis, autoimmune disorders, nephropathy, and reproductive dysfunction [13]. However, the literature has yet to explore the common comorbidities associated with LD as compared to the general populations. Furthermore, with the emergence of new disease modification treatment options for LD, there is growing awareness of the need to understand the prevalence of specific clinical comorbidities commonly associated with LD, and to evaluate whether these are prevalent in the natural history of LD without disease modifying treatment. Therefore, we aim to examine specific LD-associated clinical characteristics in a commercially insured US population using a nationwide administrative claims database between 2018 and 2019.
Methods
Data source and study design
We examined specific LD-associated clinical characteristics using the Clinformatics® Data Mart database from January 1, 2018, to December 31, 2019. Clinformatics Data Mart is an integrated US healthcare claims database that includes privately insured enrollees with commercial or Medicare Advantage plans affiliated with Optum. The database contains statistically de-identified and Health Insurance Portability and Accountability Act-compliant medical claims, including healthcare services performed in inpatient and outpatient settings, and pharmacy claims for approximately 15–20 million individuals annually. The Clinformatics Data Mart population is geographically representative, spanning all 50 US states. In addition to medical and pharmacy claims, the database includes provider data and information on patient enrollment and demographics [14]. Clinformatics Data Mart utilizes internal and external sources to comprehensively capture death information, such as the Death Master File maintained by the Social Security Office, enrollment data files in Medicare data, obituary data, facility claims, member coverage information, and Optum EHR data.
Study population
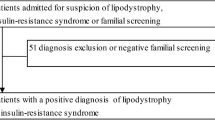
First, we assembled an all-adult cohort, including all eligible adult individuals (aged ≥ 18 years on January 1, 2018) who continuously enrolled from January 1, 2018 until December 31, 2019 (or until they died, if this was before the end date of the study period), allowing a 45-day enrollment gap (Fig. 1). Next, a cohort comprising patients with a diagnosis of HIV disease was identified to include individuals who had at least 1 inpatient or 2 outpatient HIV diagnoses (i.e. International Classification of Diseases [ICD]-9-CM: 042, 079.53, V08; ICD-10-CM: B20, B97.35, Z21) on separate calendar dates among the all-adult cohort. This identification algorithm was modified from the validated Medicaid-based algorithm to identify people living with HIV [15, 16]. An LD cohort was also created from the all-adult cohort by identifying LD diagnosis (i.e. ICD-9-CM: 272.6; ICD-10-CM: E88.1) in medical claims, or metreleptin prescription (National Drug Code: 66780-310-01, 76431-210-01) in pharmacy claims. In order to increase specificity and decrease misclassification due to rule-out diagnosis, at least 1 inpatient or 2 outpatient LD diagnoses on separate calendar dates were required. The LD cohort was further divided into non-HIV-LD and HIV-LD subgroups. We defined the non-HIV-LD group as individuals without any HIV diagnosis, and the HIV-LD group as individuals with at least 1 inpatient or 2 outpatient HIV diagnoses among the LD cohort. By definition, the non-HIV-LD group included all individuals with GLD or non-HIV-associated PLD, and the HIV-LD group included HIV-associated lipoatrophy and lipohypertrophy.
Flow chart for clinical characteristic analysis in 2018–2019. aIndividuals who had at least 1 inpatient or 2 outpatient HIV diagnoses (i.e. ICD-9-CM: 042, 079.53, V08; ICD-10-CM: B20, B97.35, Z21) on separate calendar dates are qualified to have HIV. Abbreviations: HIV-LD, lipodystrophy associated with HIV; ICD, International Classification of Diseases; non-HIV-LD, lipodystrophy not associated with HIV; PWHD, people living with HIV disease
Individuals in the non-HIV-LD group were matched by age and sex in a 1:4 ratio to controls from the all-adult cohort without HIV. The controls were required to have neither an LD nor an HIV diagnosis. To minimize the effect of fat alterations associated with HIV infection and antiretroviral therapy, individuals in the HIV-LD group were matched by age and sex in a 1:4 ratio to controls from the people living with HIV cohort. The people living with HIV controls were required not to have an LD diagnosis.
Descriptive data analysis 2018–2019
We examined patient demographics (i.e. age, sex, and race/ethnicity), estimated their Elixhauser Comorbidity Index [17] (identification of 38 different pre-existing conditions based on secondary diagnoses) and estimated the prevalence of clinical characteristics among the non-HIV-LD and HIV-LD cohorts. The specific clinical characteristics evaluated included hyperlipidemia, diabetes mellitus, hypertension, acute myocardial infarction (AMI), MASLD or metabolic dysfunction-associated steatohepatitis (MASH), liver fibrosis or cirrhosis, acute pancreatitis, kidney disease (i.e. acute or chronic glomerulonephritis, acute or chronic renal failure, nephritis or nephrotic syndrome, renal failure or proteinuria), autoimmune diseases (i.e. systematic lupus erythematosus [SLE], rheumatoid arthritis, autoimmune thyroiditis), cancers excluding non-melanoma skin cancers, and serious infections (i.e. bacteremia, pneumonia, skin/soft tissue infection, gastrointestinal infection, acute osteomyelitis, acute pyelonephritis, acute meningitis) resulting in hospitalization. We examined the prevalence of overall cancer and specific types of cancers (i.e. lymphoma, breast cancer, prostate cancer). Lymphoma was identified with at least 1 inpatient diagnosis or 2 outpatient lymphoma diagnoses on separate calendar dates occurring at least 2 months apart. This approach was a modified version of a validated algorithm developed by Setoguchi et al., expecting > 80% sensitivity and > 90% specificity [18]. We also applied the same identification algorithm to other cancers [18]. To identify AMI, we applied an identification algorithm yielding 86.0% positive predictive value from a primary hospital discharge diagnosis of AMI [19]. Acute pancreatitis was identified from a primary hospital discharge diagnosis of acute pancreatitis [20]. To identify SLE, we modified a claims-based identification algorithm by using at least 1 inpatient diagnosis or 2 outpatient diagnoses at least 2 months apart [21].
Furthermore, we used a case definition of serious infections resulting in hospitalizations [22]. For hyperlipidemia, diabetes mellitus, and hypertension, we used the Centers for Medicare and Medicaid Services (CMS) Chronic Condition Warehouse (CCW) algorithms using at least 1 inpatient or 2 outpatient diagnoses on separate calendar dates [23].
Statistical analysis
The patient demographics and clinical characteristics among non-HIV-LD and HIV-LD cases were presented as percentages for categorical variables, and as means and standard deviations for continuous variables. We compared demographics and clinical characteristics between the LD cohorts and matched controls using the Chi-square test, Fisher’s exact test, and student t-test, as appropriate. Logistic regression models were used to estimate the odds ratios (ORs) and accompanying 95% confidence intervals (CIs) for each clinical characteristic among non-HIV-LD and HIV-LD cohorts compared with the matched controls. All analyses were performed using Health Data software (Panalgo, Boston, MA, USA) with a two-sided level of statistical significance of 0.05.
Data and resource availability
All data analyzed during this study are from the Clinformatics Data Mart database that is cited in the Methods section. All analyses conducted in this study are presented in the manuscript.
Results
Clinical characteristics of individuals with non-HIV-LD versus matched controls from the all-adult cohort without HIV
We identified 546 individuals with non-HIV-LD (mean age, 60.3 ± 14.9 years; female, 67.6%; non-Hispanic White, 53.8%) and 2184 age- and sex-matched controls from the all-adult cohort without HIV between 2018 and 2019. Individuals with non-HIV-LD were more likely to use healthcare services compared with matched controls as follows: having ≥ 2 hospitalizations (17.9% vs 4.3%; P < 0.001), having ≥ 2 emergency department visits (29.7% vs 12.0%; P < 0.001), and having ≥ 10 outpatient visits (93.6% vs 63.7%; P < 0.001) during the 2-year study period (Table 1). Compared to matched controls, individuals with non-HIV-LD had higher odds of having all of the identified metabolic comorbidities and complications (i.e. hypertension, hyperlipidemia, diabetes mellitus, MASLD/MASH, AMI, liver fibrosis or cirrhosis, and acute pancreatitis; Table 2). In addition, those with non-HIV-LD had increased odds of having kidney diseases, identified autoimmune diseases, serious infections resulting in hospitalization, and any cancer, mostly breast cancer and prostate cancer (Table 2). The Elixhauser index was greater in individuals with non-HIV-LD (6.5 ± 4.1) than in matched controls (3.2 ± 3.5; P < 0.001; Table 1).
Clinical characteristics of individuals with HIV-LD versus matched controls from the people living with HIV cohort
We identified 334 individuals with HIV-LD (mean age, 59.2 ± 8.3 years; female, 15.0%; non-Hispanic White, 56.9%) and 1336 age- and sex-matched controls from the people living with HIV cohort between 2018 and 2019. Individuals with HIV-LD were more likely to have ≥ 10 outpatient visits compared to matched people living with HIV controls during the 2-year study period (92.2% vs 81.3%; P < 0.001); however, there were no statistically significant differences between those having ≥ 2 hospitalizations (9.3% vs 9.4%; P = 0.80) and those having ≥ 2 emergency department visits (21.0% vs 22.8%; P = 0.51; Table 1). Compared to matched people living with HIV individuals, those with HIV-LD had higher odds of having hypertension (68.6% vs 59.7%; P = 0.004, OR: 1.47; 95% CI: 1.13–1.92), hyperlipidemia (75.7% vs 55.9%; P < 0.001, OR: 2.46, 95% CI: 1.86–3.28), and diabetes mellitus (31.1% vs 24.9%; P = 0.02, OR: 1.37, 95% CI: 1.04–1.79; Table 2). The Elixhauser index was greater in individuals with HIV-LD (6.1 ± 3.7) than in matched people living with HIV controls (5.5 ± 3.8; P = 0.01; Table 1). However, the prevalence of other clinical characteristics was comparable between those with HIV-LD and matched people living with HIV controls (Tables 1 and 2).
Discussion
Our study yielded 2 important findings using a US nationwide cohort of the commercially insured adult population. The findings of this study demonstrate the high prevalence of metabolic abnormalities and comorbidities in individuals with LD. The study findings may also shed light on the suspected association between immune dysregulation, cancer development, and LD.
The association between LD and metabolic comorbidities is well recognized in the literature. Our results were consistent with previous research, as we observed a high burden of metabolic comorbidities among individuals with non-HIV-LD, although due to the design of our study we were not able to explore the incidence of these comorbidities. Similar to the findings from the study by Gonzaga-Jauregui and colleagues [24], we observed higher ORs of having hypertension, hyperlipidemia, diabetes mellitus, and MASLD/MASH among individuals with non-HIV-LD compared with age- and sex-matched controls from the all-adult cohort without HIV. Our study also demonstrated the higher odds between non-HIV-LD and complications of metabolic comorbidities, such as AMI, liver fibrosis or cirrhosis, and acute pancreatitis as compared to the general population. An increased risk of metabolic comorbidities can lead to accelerated coronary artery disease [25]. MASH is one of the leading causes of advanced liver disease, such as liver fibrosis and cirrhosis, and type 2 diabetes is identified as a strong risk factor for progressive liver disease [26,27,28]. In addition, hypertriglyceridemia is an infrequent but well-established cause of acute pancreatitis [29]. The aforementioned evidence indicates that individuals with LD are at higher risk of AMI, liver fibrosis or cirrhosis, and acute pancreatitis. Consistent with non-HIV-LD, individuals with HIV-LD are more likely to have hypertension, hyperlipidemia, or diabetes mellitus compared with age- and sex-matched controls from the people living with HIV cohort.
Some studies are suggestive of a potential association between LD and autoimmune diseases [30,31,32]. We observed higher odds of autoimmune diseases in the non-HIV-LD cohort, as higher odds were observed for rheumatoid arthritis, autoimmune thyroiditis, and lupus compared with the age- and sex-matched controls from the all-adult cohort without HIV.
We observed that individuals with non-HIV-LD and HIV-LD have an increased risk of cancer compared with matched controls. Specifically, individuals with non-HIV-LD are more likely to have breast cancer and prostate cancer, whereas individuals with HIV-LD had numerically higher odds of having lymphoma compared with the people living with HIV cohort; however, this was not statistically significant.
All studies utilizing secondary data sources have inherent limitations, and our study is no exception. We did not perform subgroup analyses for GLD and PLD, since there are no specific ICD-9/10-CM codes for LD subtypes, or validated algorithms currently available. However, we categorized LD into non-HIV-LD and HIV-LD using a combination of ICD-9/10-CM codes for LD and HIV, which is consistent with previous studies [24, 33]. Due to its rarity, heterogeneity, and similarity in disease manifestation with metabolic syndrome (particularly for PLD) [13], LD is commonly underrecognized and misdiagnosed in clinical practice. This may have contributed to the under-identification of LD cases in our study. However, the use of the ICD-9/10-CM codes provides a standard approach to identify the frequency of LD diagnosis in real-world settings. In addition, there is a potential for misclassification of comorbidities due to improper coding or rule-out diagnosis. Therefore, we conducted a thorough search to identify validated claims-based algorithms. Where no such algorithm existed, we adopted the “1 inpatient or 2 outpatient diagnoses” approach to increase specificity and minimize misclassification resulting from rule-out diagnosis. This approach was also consistent with most CCW algorithms to identify chronic conditions in the CMS administrative claims data [23]. As a limitation inherent in cross-sectional studies, we did not investigate the temporal dynamic of clinical characteristics; thus, the findings of this study cannot be used to establish causality between LD and clinical characteristics. Additionally, we did not adjust for medications that have known associations with LD. However, it is still meaningful to understand the general prevalence of comorbidities in individuals with LD. To the best of our knowledge, this study is the first large claims-based study to explore clinical characteristics observed in patients with LD.
Conclusions
In summary, although LD is a group of rare diseases, it imposes a substantially high burden on affected individuals, and has an increased odds with a range of comorbidities and complications (metabolic abnormalities, autoimmune diseases, cancers, serious infections resulting in hospital admissions). Future longitudinal follow-up studies are warranted to investigate the temporal dynamics between LD and observed clinical characteristics.
Availability of data and materials
All data analyzed during this study are from the Clinformatics® Data Mart database that is cited in the Methods section. All analyses conducted in this study are presented in the manuscript.
Abbreviations
- AMI:
-
Acute myocardial infarction
- CMS:
-
Centers for Medicare and Medicaid Services
- CCW:
-
Chronic condition warehouse
- CI:
-
Confidence interval
- EHR:
-
Electronic health record
- GLD:
-
Generalized LD
- HIV-LD:
-
HIV-associated LD
- ICD:
-
International Classification of Diseases
- LD:
-
Lipodystrophy
- MASLD:
-
Metabolic dysfunction-associated steatotic liver disease
- MASH:
-
Metabolic dysfunction-associated steatohepatitis
- OR:
-
Odds ratio
- PLD:
-
Partial LD
- SLE:
-
Systematic lupus erythematosus
References
Brown RJ, Araujo-Vilar D, Cheung PT, et al. The diagnosis and management of lipodystrophy syndromes: a multi-society practice guideline. J Clin Endocrinol Metab. 2016;101(12):4500–11.
Garg A. Lipodystrophies: genetic and acquired body fat disorders. J Clin Endocrinol Metab. 2011;96(11):3313–25.
Garg A. Lipodystrophies. Am J Med. 2000;108(2):143-52.
Garg A. Acquired and inherited lipodystrophies. N Engl J Med. 2004;350(12):1220–34.
Carr A, Samaras K, Burton S, et al. A syndrome of peripheral lipodystrophy, hyperlipidaemia and insulin resistance in patients receiving HIV protease inhibitors. AIDS. 1998;12(7):F51–8.
Guaraldi G, Stentarelli C, Zona S, Santoro A. HIV-associated lipodystrophy: impact of antiretroviral therapy. Drugs. 2013;73(13):1431–50.
Kotler DP. HIV infection and lipodystrophy. Prog Cardiovasc Dis. 2003;45(4):269–84.
Brinkman K, ter Hofstede HJ, Burger DM, Smeitink JA, Koopmans PP. Adverse effects of reverse transcriptase inhibitors: mitochondrial toxicity as common pathway. AIDS. 1998;12(14):1735-44.
Jacobson DL, Knox T, Spiegelman D, Skinner S, Gorbach S, Wanke C. Prevalence of, evolution of, and risk factors for fat atrophy and fat deposition in a cohort of HIV-infected men and women. Clin Infect Dis. 2005;40(12):1837–45.
Bacchetti P, Gripshover B, Grunfeld C, et al. Fat distribution in men with HIV infection. J Acquir Immune Defic Syndr. 2005;40(2):121–31.
Mallon PW, Miller J, Cooper DA, Carr A. Prospective evaluation of the effects of antiretroviral therapy on body composition in HIV-1-infected men starting therapy. AIDS. 2003;17(7):971–9.
Mulligan K, Parker RA, Komarow L, et al. Mixed patterns of changes in central and peripheral fat following initiation of antiretroviral therapy in a randomized trial. J Acquir Immune Defic Syndr. 2006;41(5):590–7.
Fiorenza CG, Chou SH, Mantzoros CS. Lipodystrophy: pathophysiology and advances in treatment. Nat Rev Endocrinol. 2011;7(3):137–50.
Optum’s de-identified Clinformatics® Data Mart Database (2007–2020). Available from: https://www.optum.com/business/life-sciences/real-world-data/claims-data.html.
Macinski SE, Gunn JKL, Goyal M, Neighbors C, Yerneni R, Anderson BJ. Validation of an optimized algorithm for identifying persons living with diagnosed HIV from New York State Medicaid Data, 2006–2014. Am J Epidemiol. 2020;189(5):470–80.
Chronic Conditions Data Warehouse. Human Immunodeficiency Virus and/or Acquired Immunodeficiency Syndrome (HIV/AIDS). Available from: https://www2.ccwdata.org/web/guest/condition-categories.
Agency for Healthcare Research and Quality. Elixhauser Comorbidity Software Refined for ICD-10-CM Healthcare Cost and Utilization Project (HCUP). Available from: https://hcup-us.ahrq.gov/toolssoftware/comorbidityicd10/comorbidity_icd10.jsp#:~:text=The%20Elixhauser%20Comorbidity%20Indices%20Refined%20for%20ICD%2D10%2DCM%20is,%2Dday%2C%20all%2Dcause%20readmission.
Setoguchi S, Solomon DH, Glynn RJ, Cook EF, Levin R, Schneeweiss S. Agreement of diagnosis and its date for hematologic malignancies and solid tumors between medicare claims and cancer registry data. Cancer Causes Control. 2007;18(5):561–9.
Cutrona SL, Toh S, Iyer A, et al. Validation of acute myocardial infarction in the Food and Drug Administration’s Mini-Sentinel program. Pharmacoepidemiol Drug Saf. 2013;22(1):40–54.
Moores K, Gilchrist B, Carnahan R, Abrams T. A systematic review of validated methods for identifying pancreatitis using administrative data. Pharmacoepidemiol Drug Saf. 2012;21(Suppl 1):194–202.
Bernatsky S, Linehan T, Hanly JG. The accuracy of administrative data diagnoses of systemic autoimmune rheumatic diseases. J Rheumatol. 2011;38(8):1612–6.
Lore V 3rd, Carbonari DM, Jacob J, et al. Validity of ICD-10-CM diagnoses to identify hospitalizations for serious infections among patients treated with biologic therapies. Pharmacoepidemiol Drug Saf. 2021;30(7):899–909.
Chronic Conditions Data Warehouse. Condition Categories. Available from: https://www2.ccwdata.org/web/guest/condition-categories.
Gonzaga-Jauregui C, Ge W, Staples J, et al. Clinical and Molecular Prevalence of Lipodystrophy in an Unascertained Large Clinical Care Cohort. Diabetes. 2020;69(2):249–58.
Brown JC, Gerhardt TE, Kwon E. Risk Factors For Coronary Artery Disease. Treasure Island (FL): StatPearls Publishing; 2022.
Jarvis H, Craig D, Barker R, et al. Metabolic risk factors and incident advanced liver disease in non-alcoholic fatty liver disease (NAFLD): A systematic review and meta-analysis of population-based observational studies. PLoS Med. 2020;17(4):e1003100.
Smith BW, Adams LA. Nonalcoholic fatty liver disease and diabetes mellitus: pathogenesis and treatment. Nat Rev Endocrinol. 2011;7(8):456–65.
Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64(1):73–84.
Lloret Linares C, Pelletier AL, Czernichow S, et al. Acute pancreatitis in a cohort of 129 patients referred for severe hypertriglyceridemia. Pancreas. 2008;37(1):13–22.
Singh S, Bansal A. Twelve years experience of juvenile dermatomyositis in North India. Rheumatol Int. 2006;26(6):510–5.
Badri T, Ben Hmida M, Benmously-Mlika R, et al. Focal lipodystrophy without metabolic disorders in adult dermatomyositis. Int J Dermatol. 2013;52(11):1422–4.
Lee LA, Hobbs KF. Lipodystrophy and metabolic abnormalities in a case of adult dermatomyositis. J Am Acad Dermatol. 2007;57(5 Suppl):S85–7.
Chiquette E, Oral EA, Garg A, Araujo-Vilar D, Dhankhar P. Estimating the prevalence of generalized and partial lipodystrophy: findings and challenges. Diabetes Metab Syndr Obes. 2017;10:375–83.
Acknowledgements
The authors would like to thank the patients, the data vendors, and the clinical team at Regeneron Pharmaceuticals, Inc for their valuable contributions towards this study. This manuscript was written by authors according to Good Publication Practice guidelines (Link). Editorial support was provided by Prime (Knutsford, UK), funded by Regeneron Pharmaceuticals, Inc. The sponsor participated in the design and conduct of the study, analysis of the data, and preparation of this manuscript. The authors had unrestricted access to study data, were responsible for all content and editorial decisions, and received no honoraria related to the development of this publication.
Funding
This analysis was an intern project and was conducted by the authors at Regeneron Pharmaceuticals, Inc.
Author information
Authors and Affiliations
Contributions
S.Y. and C.K.: Conceptualization; data curation; formal analysis; investigation; validation; writing—review and editing.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This is a retrospective cohort study and was conducted using data from the Clinformatics® Data Mart database and therefore did not qualify/require Ethics Approval or consent to participate. All data analyzed during this study are from the Clinformatics Data Mart database that is cited in the Methods section. The study utilizes the secondary use of commercially available de-identified healthcare data. Identifiable patient information has been stripped and determined to be de-identified in accordance with the HIPAA Privacy Rule by either expert determination (§ 164.514 (b)(1)) or Safe Harbor (§ 164.514 (b)(2)). The use of data would not constitute human subjects research in accordance with the Common Rule (45 CFR 46.102(f)). Therefore, IRB review was not required.
Consent for publication
Not applicable.
Competing interests
S.Y. conducted the analysis and writing as an intern and contractor for Regeneron Pharmaceuticals, Inc.
C.K. is an employee of and shareholder in Regeneron Pharmaceuticals, Inc.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yang, S., Knox, C. Prevalence of clinical characteristics of lipodystrophy in the US adult population in a healthcare claims database. BMC Endocr Disord 24, 102 (2024). https://doi.org/10.1186/s12902-024-01629-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12902-024-01629-x