Abstract
Background
Periodontal diseases is considered the most important global oral health burden according to the world health organization (WHO) (Oral health. https://www.who.int/news-room/fact-sheets/detail/oral-health#Overviewth (who.int). Accessed 21 Sep 2023). It is a common local inflammatory disease associated with hypertension, this study aims to explore the relationship between periodontitis and uncontrolled hypertension and whether inflammation indication such as white blood cell (WBC) count or neutrophil count is a mediator of this relationship.
Methods
One thousand four hundred eighty-eight elders attending annual physical and oral examinations in Zhejiang province were included in this study. The staging of Periodontitis was classified as none, mild-moderate and severe. Participants are categorized into two groups based on blood pressure: hypertensive( positive high blood pressure( HBP) history or underwent HBP medication or blood pressure( BP) ≥ 140/90 mmHg) and uncontrolled hypertensive (systolic blood pressure( SBP) ≥ 140 mmHg or distolic blood pressure( DBP) ≥ 90 mmHg). Peripheral blood samples were collected, information on hypertension history and potential confounders (age, sex, smoking, alcohol consumption, exercise frequency, diabetes) was collected in questionnaires. The correlation between periodontitis and hypertension was investigated using logistics regression analyses, mediation analysis was assessed for the effect of inflammation on hypertension.
Results
The study population includes 1,488 participants aged 55–90 years. Odds of uncontrolled hypertension increased significantly along with periodontitis in the regression models both in unadjusted model (odds ratio( OR): 1.407, 95% confidence intervals( CI): 1.037 ~ 1.910) and fully adjusted model (OR: 1.950, 95% CI: 1.127 ~ 3.373). Mediation analysis confirmed that WBC and neutrophic count function as a full mediator of the association between periodontitis and uncontrolled hypertension either in the unadjusted or the adjusted model.
Conclusions
In a study of urban elderly population in southeast China, periodontitis is found to be significantly associated with uncontrolled hypertension, such relation is mediated by WBC and neutrophil count. Periodontitis can increase the difficulty of controlling hypertension. Promotion of periodontal health strategies in the dental setting could help reduce the burden of hypertension and its complications.
Similar content being viewed by others
Background
Periodontal disease is one of the most frequent diseases with a prevalence of 45–50% of the world population [1], almost 750 million people aged from 15 to 99 worldwide present with moderate to severe symptoms of periodontitis [2]. The Chinese fourth national oral health survey revealed that the prevalence of periodontitis in people over 55 years old is 64.6%, and the prevalence of severe periodontitis is 37.3% [3]. Periodontal disease is associated with many non-communicable diseases( NCDs) including cardiovasculardisease [4], diabetes [5], chronic respiratory disease [6], obesity [7] and chronic kidney disease [8]. If not treated effectively, the disease ultimately leads to tooth loss, decreased oral function and negatively affects patients’ quality of life [9, 10].
Systemic arterial hypertension is the most prevalent chronic NCD in the world. Numerous epidemiological studies have demonstrated a strong association between hypertension and the development of various cardiovascular diseases, including coronary artery disease, heart failure, stroke, and peripheral vascular disease. The population attributable fraction of high blood pressure for cardiovascular disease mortality is 40.6% (95% CI, 24.5%–54.6%) [11,12,13]. More than 30% of adults are estimated to have the disease worldwide with higher frequencies found with increasing age [14]. A 15% to 50% of individuals, however, are unaware of their hypertension, [15] meanwhile many of those with an established diagnosis fail to achieve an optimal BP control despite their prescribed medications [11].
Previous epidemiological studies and meta-analyses have reported the relation between oral health and cardiovascular diseases, suggesting periodontal disease is associated with hypertension [15,16,17,18,19,20]. However the relationship and mediation between periodontitis and uncontrolled hypertension has not been reported. Since hypertension and its control level is closely linked with socioeconomic status (SES), and Hangzhou is holding the 19th Asian Games in Sep. 2023, which represents the economically developed regions of China. Data on China’s economically developed regions is inadequate, we performed this cross-sectional study to investigate the relationship between the two diseases in Hangzhou and find out the mediation of the relationship.
Materials and methods
Population and study design
We used data on urban elderly population (aged from 55–90 years) from a routine physical examination from 6 community hospitals in Hangzhou, capital city of Zhejiang province which has a high economic level according to the national gross domestic product in mainland China. This study was conducted following the Declaration of Helsinki and approved by the Ethics Committee of Stomatology Hospital Affiliated to Zhejiang University School of Medicine (Ethics Approval No. 2021–075).
Exclusion criteria for study participants were as follows: (1) data for blood test or questionnaires were missing, (2) did not complete oral and periodontal examinations. (3) presence of systemic infections, (4) systemic antibiotic treatment in the past 3 months, (5) undergoing periodontal treatment in the past three months.
Five thousand eight hundred nineteen participants were attending the routine physical examination in 2021, of which 4014 received oral examinations and blood pressure values were available for 3668 participants. After excluding those who did not perform oral and systemic examinations, 1488 participants remained.
A post hoc power analysis was carried out using the G-POWER 3.1 programme at the end of the study. At an effect size of 0.02 and α of 0.05, a sample size of 1400 can achieve a power of 0.97.
Periodontal examination and diagnosis
All the periodontal examinations were finished by well-trained and calibrated periodontists. Periodontal examinations were conducted on two-diagonal quadrants randomly, one in the maxilla and the other in the mandible, excluding third molars and implants. Measurements were taken at four sites per tooth (distobuccal (DB), mesiobuccal (MB), mesiolingual (ML), and distolingual (DL)). Probing depth (PD) and clinical attachment loss (CAL) were assessed by a manual UNC-15 probe (Hu-Friedy, Chicago, IL). Tooth loss was also recorded at the same time. Periodontitis status was classified into three categories, namely, severe periodontitis, mild-moderate periodontitis, and no periodontitis. Periodontitis classification was based on a modified half-reduced CDC/AAP definition (CDC, Center of Disease Control; AAP, the American Academy of Periodontology) [21, 22]. Severe periodontitis was defined as ≥ 1 interproximal site with ≥ 6 mm CAL and ≥ 1 interproximal site(s) with ≥ 5 mm PD (on the same site with CAL ≥ 6 mm or different sites). Moderate periodontitis was defined as ≥ 1 interproximal site with ≥ 4 mm CAL or 1 site with ≥ 5 mm PD. Mild periodontitis was defined as ≥ 1 interproximal site with CAL ≥ 3 mm, and ≥ 1 interproximal sites with PD ≥ 4 mm (on the same site with CAL ≥ 3 mm or different sites). No periodontitis was defined as no evidence of mild, moderate, or severe periodontitis [23].
Assessment of arterial hypertension
The diagnosis of arterial hypertension was based on a medical history, with focus on antihypertensive drugs, a blood pressure measurement, and patients’ self-report. Blood pressure was measured on both arms each for 2 times after the initial rest of 5 min and a one-minute interval between each. Resting BP was recorded and calculated as the average of 4 readings. The Sixth Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure defined that the diagnosis of hypertension is made when the average of 2 or more diastolic BP measurements on at least 2 subsequent visits is ≥ 90 mm Hg or when the average of multiple systolic BP readings on 2 or more subsequent visits is consistently ≥ 140 mm Hg [24]. Hypertensive individuals were classified into 2 groups:” hypertensive”: with a positive HBP history or underwent HBP medication or BP ≥ 140/90 mmHg, “uncontrolled hypertension”: participants who fail to maintain to less than 140/90 mm Hg regardless of medication use or treatment [11, 25].
Confounders
Questionnaires were distributed to all participants, including sex, age, height, weight, alcohol consumption, exercise frequency, and smoking habits. sex was categorized as female and male. Body mass index (BMI) was calculated from weight /height2 (kg/m2). Alcohol consumption was classified into 3 groups: (1) never, (2) often, and (3) daily. Exercise frequency was categorized into 3 groups: (1) never, (2) 1–3 times per week, (3) 4–7 times per week [26]. Smoking habits were classified into 3 groups: (1) current smoker, (2) former smoker, and (3) nonsmoker. Former smokers were defined as those who had smoked in the past but quit smoking for at least 6 months. WBC, neutrophil count, lymphocyte count, Fasting glucose and triglycerides, high-density lipoprotein( HDL); low-density lipoprotein( LDL), and total cholesterol were measured by routine laboratory tests.
Statistical analysis
Data analysis was performed using IBM SPSS Statistics version 25.0 for Windows (IBM, ARMONK, NY, USA). Continuous variables were reported as means ± standard deviation (SD). Categorical variables were reported as number of cases (n) and percentage (%). Comparisons between different periodontal status were conducted using chi-squared test for categorical variables and ANOVA for continuous ones.
We employed logistic regression models to evaluate the multivariable association between periodontal disease and hypertension. Independent variables were selected among clinical and demographic characteristics, age, sex, systolic blood pressure, diastolic blood pressure, fasting plasma glucose, cholesterol, triglycerides, high-density lipoprotein, white blood cells, neutrophil count, lymphocyte count, body mass index, smoking and alcohol consumption were included. Following the initial crude model (model 1, unadjusted), 4 extended models were generated with adjustment for age and sex (model 2), additional inclusion of BMI and waist circumference (model 3), an additional inclusion of inflammation indexes including white blood cell, neutrophil count, and lymphocyte count (model 4), lifestyle habits including smoking, exercising and alcohol consumption were added in model 5. Odds ratios and 95% CI were reported.
Finally, we used 2 mediation models to identify and explain the pathways or processes underlying the relationship between periodontitis and uncontrolled hypertension, via the hypothetical mediator of inflammation factors.
Results
Baseline characteristics of the study group
Baseline characteristics of the study are presented in Table 1, subdivided by the severity of periodontitis. Our final sample after subject selection includes 1,488 participants aged 55–90 years, of which 602 (40.46%) were male and 886 (59.54%) were female. Their mean age was 64.446 ± 7.765 years. 1254(84.27%) had a history of hypertension diagnosis or were observed to have high blood pressure, 924(62.10%) were observed to have high blood pressure, the prevalence of uncontrolled hypertension was 63.46% (382/602) for men and 61.17% (542/886) for women. The prevalence of periodontal disease was 1295(87.03%), including 539(36.22%) people exhibited severe periodontitis and 756(50.81%) people exhibited mild-moderate periodontitis and 193(12.97%) exhibited no periodontitis. Of those who had periodontitis the prevalence for male is 91.03% (548/602) and 84.31% (747/886) for female.
Association between periodontitis and hypertension
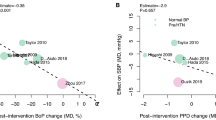
Of the hypertensive participants (with both hypertension history and a tested high blood pressure), after adjusting for all potential confounders, we did not observe any association between periodontitis and hypertension. When we categorized our study population into periodontally healthy and periodontitis and restrict our analysis to UNCONTROLLED high blood pressure only, we found a significant effect of periodontitis on the odds of hypertension (Table 2). In the unadjusted model (model1), odds ratio (OR) for uncontrolled hypertension is 1.407, 95% confidence interval (CI) is 1.037 ~ 1.910, p < 0.05. After adjusted for sex and age (model2), OR and 95% CI is 1.367(1.005 ~ 1.861), p < 0.05. Model3 introduced serum lipids indexes, OR and 95% CI is 1.405(1.024 ~ 1.928), p < 0.05. Model4 introduced inflammation indexes, OR and 95% CI is 1.421(1.034 ~ 1.953), p < 0.05. Model5 adjusted for lifestyle habits, OR and 95% CI gets to 1.950(1.127 ~ 3.373), p < 0.05. The result of the regression models confirmed that the parameter selection of the periodontitis models does not affect the result of the study that odds of uncontrolled hypertension increased significantly along with periodontitis in the regression models.
Mediation analysis
Because both a (the regression coefficient of periodontitis on mediators) and b (the regression coefficient of mediators on uncontrolled hypertension) are significant, and c' (the regression coefficient of periodontitis on uncontrolled hypertension) is not significant, it is considered that WBC and neutrophil count function as a full mediator of the association between periodontitis and uncontrolled hypertension either in the unadjusted or the fully adjusted model. While lymphocyte count did not function as a mediator. Results of the mediation analysis are summarized in Table 3.
Discussion
Currently, there is a lack of standardized diagnostic criteria for periodontitis in epidemiological surveys, making Full mouth periodontal examinations (FMPE) the “gold standard” for evaluating periodontal health. In our study, we implemented a protocol for partial mouth periodontal examinations (PMPE). Since PMPE protocols involve examining fewer probing sites compared to FMPE, applying a case definition designed for FMPE may result in underestimating the prevalence of the disease. Among various protocols for PMPE, such as Ramfjord teeth (RT) and community periodontal index (CPI), the two random diagonal quadrants protocol demonstrates the highest level of accuracy [27]. For our study, we utilized a modified half-reduced CDC/AAP definition that was specifically tailored for PMPE [22]. It has been reported that when using the half-reduced CDC/AAP definition, the half-mouth four-site protocol yielded minimal absolute bias in estimating the prevalence of moderate periodontitis and severe periodontitis compared to FMPE.
According to our study findings, the presence of periodontitis was associated with elevated blood pressure. However, there was no statistically significant difference between the severity of periodontitis and either SBP or DBP, nor with the prevalence of hypertension. Similar findings have been observed in other observational studies conducted among various populations, including Korean female adults [16], the Puerto Rico elderly population [17], the central China population [18], the hamburg population [19], and the Portuguese population [20]. These studies have also reported a significant positive correlation between periodontal disease and an increased risk of hypertension. However, the factors contributing to this correlation are complex and not fully understood. Systemic inflammation and subsequent vascular endothelial damage are considered the primary pathomechanisms responsible for the elevation of blood pressure in individuals with periodontitis [28,29,30]. Periodontitis triggers a systemic inflammatory response mediated by various factors, including C-reactive protein, interleukin 1b (IL-1b), interleukin 6 (IL-6), tumor necrosis factor alpha (TNF-α), and others [31]. These factors can directly impact the vascular endothelium, resulting in impaired vasodilatory function [32]. The findings of the genome-wide association study revealed an association between single nucleotide polymorphisms (SNPs) and periodontitis [33]. A study by Czesnikiewicz-Guzik et al. showed that all four studied SNPs showed also concordant effect direction [34]. The outcomes of this study provide an explanation for one potential reason behind the frequent coexistence of both periodontitis and arterial hypertension.
There are some limitations in the study. As our oral epldemiological study was carried out on a community level, the x-ray were not taken and radiographic bone loss could not be assesed. Secondly, the study categorized hypertensive patients into two groups: hypertension vs. uncontrolled hypertension. It could be more accurate if reclassified as controlled hypertension (defined as having a medical history or currently taking medication with blood pressure under control) vs. uncontrolled hypertension. However, due to medical history being based on self-reported questionnaires, its accuracy is insufficient. Also, lack of case–control studies is a limitation of cross-sectional research, and blood pressure outcomes following periodontal treatment were not provided. Further research is needed to enhance the evidence supporting this correlation and to elucidate the mechanisms through which periodontal pathogens or the subsequent inflammation contribute to elevated blood pressure.
China has become an aging society due to improvement in living standards and the extension of life expectancy. Our study took place in Hangzhou, capital city of Zhejiang province. It’s holding the 19th Asian Games in Sep. 2023, which represents the economically developed regions of China, thus the data reflects a general trend for the impact periodontal status puts on general health. The National Healthcare Security Administration of China is reducing oral medical cost though centralized procurement, considering oral health is an important factor that affects the quality of life, policymakers need to address oral health needs and consider adding coverage for comprehensive oral health benefits.
Conclusion
The study found the significant association between periodontitis and uncontrolled hypertension is mediated by WBC and neutrophil count. Periodontitis can increase the difficulty of controlling hypertension. Promotion of periodontal health strategies in the dental setting could help reduce the burden of hypertension and its complications.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author, but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of the corresponding author.
Abbreviations
- WHO:
-
World Health Organization
- WBC:
-
White blood cells
- HBP:
-
High blood pressure
- BP:
-
Blood pressure
- SBP:
-
Systolic blood pressure
- DBP:
-
Diastolic blood pressure
- OR:
-
Odds ratio
- CI:
-
Confidence interval
- NCDs:
-
Non-communicable diseases
- SES:
-
Socioeconomic status
- DB:
-
Distobuccal
- MB:
-
Mesiobuccal
- ML:
-
Mesiolingual
- DL:
-
Distolingual
- PD:
-
Probing depth
- CAL:
-
Clinical attachment loss
- CDC:
-
Center of Disease Control
- AAP:
-
The American Academy of Periodontology
- BMI:
-
Body mass index
- FPG:
-
Fasting plasma glucose
- HDL:
-
High-density lipoprotein
- LDL:
-
Low-density lipoprotein
- FMPE:
-
Full mouth periodontal examinations
- PMPE:
-
Partial mouth periodontal examination protocol
- SNPs:
-
Single nucleotide polymorphisms
References
de Boer SPM, Cheng JM, Rangé H, Garcia-Garcia HM, Heo JH, Akkerhuis KM, et al. Antibodies to periodontal pathogens are associated with coronary plaque remodeling but not with vulnerability or burden. Atherosclerosis. 2014;237(1):84–91.
Frencken JE, Sharma P, Stenhouse L, Green D, Laverty D, Dietrich T. Global epidemiology of dental caries and severe periodontitis - a comprehensive review. J Clin Periodontol. 2017;44(Suppl 18):S94-105.
Jiao J, Jing W, Si Y, Feng X, Tai B, Hu D, et al. The prevalence and severity of periodontal disease in Mainland China: Data from the Fourth National Oral Health Survey (2015–2016). J Clin Periodontol. 2021;48(2):168–79.
Yu Y-H, Chasman DI, Buring JE, Rose L, Ridker PM. Cardiovascular risks associated with incident and prevalent periodontal disease. J Clin Periodontol. 2015;42:21–8.
Campus G, Salem A, Uzzau S, Baldoni E, Tonolo G. Diabetes and Periodontal Disease: A Case-Control Study. J Periodontol. 2005;76:418–25.
Bansal M, Khatri M, Taneja V. Potential role of periodontal infection in respiratory diseases - a review. J Med Life. 2013;6:244–8.
Al-Zahrani MS, Bissada NF, Borawski EA. Obesity and Periodontal Disease in Young, Middle-Aged, and Older Adults. J Periodontol. 2003;74:610–5.
Wahid A, Chaudhry S, Ehsan A, Butt S, Kahn AA. Bidirectional relationship between chronic kidney disease & periodontal disease: a review. Pak J Med Sci. 2013;29(1):211–5.
Tonetti MS, Jepsen S, Jin L, Otomo-Corgel J. Impact of the global burden of periodontal diseases on health, nutrition and wellbeing of mankind: A call for global action. J Clin Periodontol. 2017;44(5):456–62.
Iwasaki M, Usui M, Ariyoshi W, Nakashima K, Nagai-Yoshioka Y, Inoue M, et al. Validation of a self-report questionnaire for periodontitis in a Japanese population. Sci Rep. 2021;11(1):15078.
Abdalla M, Bolen SD, Brettler J, Egan BM, Ferdinand KC, Ford CD, et al. Implementation strategies to improve blood pressure control in the United States: a scientific statement from the American Heart Association and American Medical Association. Hypertension. 2023;80(10):e143–57.
Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, et al. Heart Disease and Stroke Statistics—2019 Update: a report from the American Heart Association. Circulation. 2019;139(10):e56–28.
Prospective Studies Collaboration, Lewington S, Whitlock G, Clarke R, Sherliker P, Emberson J, et al. Blood cholesterol and vascular mortality by age, sex, and blood pressure: a meta-analysis of individual data from 61 prospective studies with 55,000 vascular deaths. Lancet. 2007;370:1829–39.
Mills KT, Bundy JD, Kelly TN, Reed JE, Kearney PM, Reynolds K, et al. Global Disparities of Hypertension Prevalence and Control: A Systematic Analysis of Population-Based Studies From 90 Countries. Circulation. 2016;134(6):441–50.
Scholes S, Conolly A, Mindell JS. Income-based inequalities in hypertension and in undiagnosed hypertension: analysis of Health Survey for England data. J Hypertens. 2020;38(5):912–24.
Ahn YB, Shin MS, Byun JS, Kim HD. The association of hypertension with periodontitis is highlighted in female adults: results from the Fourth Korea National Health and Nutrition Examination Survey. J Clin Periodontol. 2015;42(11):998–1005.
Rivas-Tumanyan S, Campos M, Zevallos JC, Joshipura KJ. Periodontal disease, hypertension, and blood pressure among older adults in Puerto Rico. J Periodontol. 2013;84(2):203–11.
Zhao MJ, Qiao YX, Wu L, Huang Q, Li BH, Zeng XT. Periodontal Disease Is Associated with Increased Risk of Hypertension: A Cross-Sectional Study. Front Physiol. 2019;10:440.
Könnecke H, Schnabel RB, Walther C, Lamprecht R, Heydecke G, Seedorf U, et al. Cross-sectional study on the association of periodontitis with arterial hypertension in the Hamburg City Health Study. Eur J Med Res. 2022;27:181.
Machado V, Aguilera EM, Botelho J, Hussain SB, Leira Y, Proença L, et al. Association between Periodontitis and High Blood Pressure: Results from the Study of Periodontal Health in Almada-Seixal (SoPHiAS). JCM. 2020;9(5):1585.
Centers for Disease Control and Prevention. Mobile exam center components descrip-tions [Online]. Atlanta, GA: Centers for Dis-ease Control and Prevention. 2013. Available: http://www.cdc.gov/nchs/data/nhanes/nhanes_09_10/meccomp_f.pdf. Accessed 21 Sep 2023.
Tran DT, Gay I, Du XL, Fu Y, Bebermeyer RD, Neumann AS, et al. Assessment of partial-mouth periodontal examination protocols for periodontitis surveillance. J Clin Periodontol. 2014;41(9):846–52.
Zhu H, Ye G, Xie Y, Zhu K, Zhu F, Chen Q. Association of high-density lipoprotein cholesterol and periodontitis severity in Chinese elderly: a cross-sectional study. Clin Oral Invest. 2022;26:4753–9.
The sixth report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure. Arch Intern Med. 1997;157:2413–46.
Hajjar I, Kotchen TA. Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988–2000. JAMA. 2003;290:199–206.
Piercy KL, Troiano RP. Physical Activity Guidelines for Americans From the US Department of Health and Human Services: Cardiovascular Benefits and Recommendations. Circ Cardiovasc Qual Outcomes. 2018;11:e005263.
Peres MA, Peres KG, Cascaes AM, Correa MB, Demarco FF, Hallal PC, et al. Validity of partial protocols to assess the prevalence of periodontal outcomes and associated sociodemographic and behavior factors in adolescents and young adults. J Periodontol. 2012;83(3):369–78.
Tsioufis C, Kasiakogias A, Thomopoulos C, Stefanadis C. Periodontitis and blood pressure: the concept of dental hypertension. Atherosclerosis. 2011;219(1):1–9.
Leong XF, Ng CY, Badiah B, Das S. Association between hypertension and periodontitis: possible mechanisms. ScientificWorldJournal. 2014;2014: 768237.
Macedo Paizan ML, Vilela-Martin JF. Is there an association between periodontitis and hypertension? Curr Cardiol Rev. 2014;10(4):355–61.
Garlet GP. Destructive and Protective Roles of Cytokines in Periodontitis: A Re-appraisal from Host Defense and Tissue Destruction Viewpoints. J Dent Res. 2010;89(12):1349–63.
Muñoz Aguilera E, Suvan J, Buti J, Czesnikiewicz-Guzik M, Barbosa Ribeiro A, Orlandi M, et al. Periodontitis is associated with hypertension: a systematic review and meta-analysis. Cardiovasc Res. 2020;116(1):28–39.
Munz M, Richter GM, Loos BG, Jepsen S, Divaris K, Offenbacher S, et al. Genome-wide association meta-analysis of coronary artery disease and periodontitis reveals a novel shared risk locus. Sci Rep. 2018;8(1):13678.
Czesnikiewicz-Guzik M, Osmenda G, Siedlinski M, Nosalski R, Pelka P, Nowakowski D, et al. Causal association between periodontitis and hypertension: evidence from Mendelian randomization and a randomized controlled trial of non-surgical periodontal therapy. Eur Heart J. 2019;40(42):3459–70.
Acknowledgements
The authors would like to thank The Second People’s Hospital of Gongshu District. The community examination work was organized by the Guidance Center for Oral Health of Zhejiang Province, and the site arrangement was mainly completed by The Second People’s Hospital of Gongshu District.
Funding
This work was supported by Natural Science Foundation of Zhejiang Province (LGC22H140001), CSA Research Fund on Improvement of Caries Prevention Ability for Stomatological Practitioners No. CSA-ICP2022-04, The Research and Development Project of Stomatology Hospital Zhejaing University School of Medcine No. RD2022JCEL32 and No. RD2022DLZD01, Natrual Science Foundation of Zhejiang Province No. LTGY23H140006.
Author information
Authors and Affiliations
Contributions
All authors gave their final approval and agreed to be accountable for all aspects of the work. All authors reviewed final manuscript. YC: study design, data analysis, writing manuscript. JZ: data collection, data analysis and investigation. DN: data collection, data analysis and investigation. DZ: data collection, data analysis and investigation.HZ: conceptualization and resources, supervision, project administration.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The protocol was reviewed and approved by the Ethics Committee of Stomatology Hospital Affiliated to Zhejiang University School of Medicine (Ethics Approval No. 2021–075). All methods were performed in accordance with relevant guidelines and regulations. All the patients provided informed consent for their data to be used for research purposes.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chen, Y., Zheng, J., Ni, D. et al. The correlation between periodontitis and uncontrolled hypertension is mediated by inflammatory markers: results from a cross-sectional study of urban elderly population in southeast China. BMC Oral Health 23, 919 (2023). https://doi.org/10.1186/s12903-023-03680-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12903-023-03680-x