Abstract
Background
Oral cancer is one of the most common cancers in China and seriously threaten life and health of Chinese people. We analysed the trends and disparities of oral cancer mortality rates and the disease burden of oral cancer in China from 2006 to 2021 to provide a reference for its prevention and control.
Methods
Annual death data for oral cancer was gleaned from the China Death Surveillance Database. The age-standardized mortality rate (ASMR), annual percentage change (APC), and average APC (AAPC) were used to analyze the trend of mortality. Loss of life expectancy (LLE) and years of life lost (YLL) were adopted to assess disease burden.
Results
From 2006 to 2021, the overall ASMR of oral cancer lightly declined (AAPC: − 0.97%; 95% CI: − 1.89%, − 0.04%), and the similar trend was observed among females (AAPC: − 1.22%; 95% CI: − 1.89%, − 0.55%). The ASMR of males was 2.31–3.16 times higher than that of females per year. The median of LLE for overall, males and females caused by oral cancer from 2006 to 2021 were 0.05, 0.06 and 0.03 years, respectively. There was a decrease of standardized YLL rate from 2006 to 2021 for overall (AAPC: − 1.31%, 95% CI: − 2.24% ~ − 0.37%) and for female (AAPC: − 1.63%, 95% CI: − 2.30% ~ − 0.95%). ASMR in urban areas was 1.02–1.28 times higher than that in rural areas from 2006 to2011, but 0.85–0.97 times lower in urban areas than that in rural areas from 2018 to 2021. The disease burden was higher in urban areas than in rural areas in 2006, whereas the reverse was observed in 2021.
Conclusions
There are severe health gaps and disparities in trends between sexes and different areas in China. Males and rural populations need to be focused on targeted interventions for the main influencing factors.
Similar content being viewed by others
Background
As one of the most common cancers in the world, oral cancer is diagnosed with more than 300,000 cases each year, which is poor in prognosis and has become an important part of the global oral health problem [1, 2]. In 2020, cancer of the lip and oral cavity was estimated to rank 16th in incidence and mortality worldwide and was a common cause of cancer death in men across much of South and Southeast Asia and the Western Pacific [3]. Significant differences persist among countries, nearly two-thirds of cases occur in developing countries, half of them in South Asia [4]. Studies predicted that due to global demographic adjustment, the global incidence of oral cancer will increase by 62% to 856,000 cases by 2035 [5]. More than 90% of oral cancers are squamous cell carcinomas, which are easy to be ignored or misdiagnosed, so that many oral cancer patients are in the middle and advanced stages at the time of being diagnosed, resulting in a low 5-year survival rate [6].
As with systemic malignancies, the pathogenesis of oral malignancies has so far been considered a multifactorial problem. There are many studies on oral cancer, and risk factors are gradually discovered or verified, but its etiology and pathogenesis are still not fully understood. Current studies suggested that smoking, alcohol consumption, human papillomavirus (HPV) infection and betel nut chewing were recognized as etiologies or risk factors for oral cancer [7,8,9,10]. Where risk factors are prevalent, further analysis of mortality and disease burden due to oral cancer is needed.
In 2020, the number of new cases of oral cancer in China was more than 30,100, and the number of deaths was more than 14,700, which poses a serious threat to the life and health of Chinese residents [3]. In a study based on the Global Burden of Disease, the Age-Standardized Incidence Rate (ASIR) and ASMR of oral cancer in China increased from 1990 (1.40 and 0.92 per 100,000) to 2019 (2.25 and 1.16 per 100,000). In 2019, both ASIR and ASMR were higher in males (3.48 and 1.95 per 100,000) compared to females (1.16 and 0.50 per 100,000) [11]. Additionally, in 2011, the ASIR and ASMR were higher in urban areas (2.42 and 0.94 per 100,000) than in rural areas (1.88 and 0.84 per 100,000) [12]. The crude incidence rate of oral cancer in China was predicted to increase from 2.26 to 3.21 per 100,000 person-years over the next 20 years [13]. However, there is a lack of recent studies on mortality and disease burden trends of oral cancer in China. So further analysis of mortality and disease burden trends of oral cancer in China is needed to take measures to take a local, tailored approach to optimally reduce the burden of lip, oral and pharyngeal malignancies in the coming decades.
As one of the most populous countries in the world, trends in resident mortality in China may serve as early indicators to support the progress of public health initiatives to reduce the burden of disease and improve the quality of life. In this study, we analysed the death data of lip, oral and pharyngeal malignancies based on sex and areas from the China Death Surveillance Database, aimed to evaluate the trends and disparities of mortality and disease burden of the major oral cancers from 2006 to 2021 in China. It will help identify high-risk groups of oral cancer, and provide basic data for prevention and health interventions.
Methods
Data source
This analysis based on data of mortality from the "China death cause surveillance dataset" (https://ncncd.chinacdc.cn/jcysj/siyinjcx/syfxbg/), which is nationally representative and the data had been widely used to evaluate the disease burden in China. The database was collected by Death Surveillance Points system (DSPs), which was selected from 31 provinces in mainland China by using an iterative method involving multistage stratification [14, 15]. The content includes the number of overall, sex-specific and area-specific people in each age group in the monitoring areas and the number of deaths from 2006 to 2021 (see Additional file 1, Supplementary Table 1 and Supplementary Table 2). Causes of death were coded by International Classification of Diseases-Tenth Revision (ICD-10). Lip, oral and pharyngeal malignancies were coded as C00-C14 (see Additional file 1, Supplementary Table 3).
Statistical analysis
Age-standardized mortality rate (ASMR), annual percentage change (APC) and average APC (AAPC) were calculated to evaluate the trend of mortality by using Joinpoint 5.2.0 software. Joinpoint regression models were used to determine the periods for increases or decreases of ASMR and to calculate the APC with 95% confidence interval (CI). We employed the grid search method to select the grid point with the lowest mean as the segmentation function joinpoint. Monte Carlo permutation method [16] with 4499 randomly permuted data set was used and the overall asymptotic significance level was maintained through a Bonferroni correction. The default maximum number of connection points depends on the number of data points, and according to the algorithm recommendations provided by the Joinpoint Help System, the default value of 16 data points is 2. The AAPC with 95%CI were obtained from Joinpoint models to describe the average APCs. Loss of life expectancy (LLE), years of life lost (YLL), and YLL rates were used as indicators of disease burden [17]. The LLE and the proportion of expected life lost (PELL) were calculated by life table, and they were computed as e′0–e0 and (e′0–e0)/e0 respectively, where e′0 as the life expectancy at birth in the absence of lip, oral and pharyngeal malignancies and e0 as the life expectancy at birth in the presence of lip, oral and pharyngeal malignancies. YLL was obtained by multiplying the corresponding standard life expectancy by the number of deaths in the age group [18]. Standardized YLL rate is the ratio of YLL to the number of monitored populations according to the age distribution of standard population. AAPC of standardized YLL rate were calculated by Joinpoint 5.2.0 software. Statistical significance among subpopulations was determined using the chi-square test and Mann–Whitney U Test in IBM SPSS Statistics 26.0. The World Health Organization’s World Standard Population (2000–2025) was selected as the standard population [19]. The inspection level was set to α = 0.05.
Results
Mortality trends of lip, oral and pharyngeal malignancies during 2006–2021
The ASMR of overall oral cancer decreased from 2.12 per 100,000 in 2006 to 1.95 per 100,000 in 2021 (see Additional file 1, Supplementary Table 4). The trends of overall oral cancer ASMR were statistically significant from 2006 to 2021 (AAPC: − 0.97%; 95% CI: − 1.89%, − 0.04%). There was a decrease from 2.12 in 2006 to 1.96 per 100 000 in 2013 (APC: − 1.73%; 95% CI: − 3.28%, − 0.15%) and a decrease from 2.16 in 2018 to 1.95 per 100 000 in 2021 (APC: − 3.44%; 95% CI: − 6.00%, − 0.81%) (Table 1).
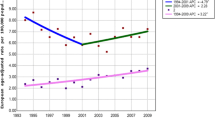
The ASMR was 2.31–3.16 times higher for males than that for females per year (see Additional file 1, Supplementary Table 4). For males, the APC were not statistically significant from 2006 to 2021. For females, the AAPC decreased by − 1.22% (95% CI: − 1.89%, − 0.55%) per year from 2006 to 2021 (Fig. 1a and Table 1).
The ASMR was 1.02–1.28 times higher for urban areas than that for rural areas from 2006 to 2011, but it was 0.85–0.97 times lower for urban areas than that for rural areas from 2018 to 2021 (see Additional file 1, Supplementary Table 4). For urban areas, there was a decrease from 2.46 in 2006 to 1.90 per 100 000 in 2012 (APC: − 2.98%; 95% CI: − 5.83%, − 0.05%) and a decrease from 2.12 in 2018 to 1.75 per 100 000 in 2021 (APC: − 6.21%; 95% CI: − 10.24%, − 2.00%). For rural areas, the APC were not statistically significant from 2006 to 2021 (Fig. 1b and Table 1).
Disease burden of lip, oral and pharyngeal malignancies in China
The median of LLE for overall, males and females due to oral cancer from 2006 to 2021 were 0.05, 0.06 and 0.03 years, respectively (Fig. 2). Males had a higher LLE compared with that of females. The LLE of the urban areas was higher than those of the rural from 2006 to 2010, while it was not prominent from 2014 to 2021 (Table 2).
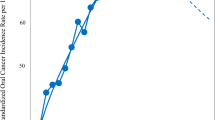
The overall standardized YLL rate of oral cancer in China ranged from 21.96/105 to 27.46/105, and there was a decrease from 2006 to 2021 (AAPC: − 1.31%, 95% CI: − 2.24% ~ − 0.37%) (Table 3). The standardized YLL rate of females showed a downward trend (AAPC: − 1.63%, 95% CI: − 2.30% ~ − 0.95%), while it did not change significantly for males. The standardized YLL rate was 2.61–3.36 times higher for males than that for females per year (Fig. 3a and Table 3). The standardized YLL rate of urban areas showed a downward trend (AAPC: − 1.94%, 95% CI: − 2.73% ~ − 1.16%), while the rural areas did not change significantly. In 2006, the YLL rate of urban areas was higher than that of rural areas, but the YLL rate of rural areas was higher than that of urban in 2021 (Fig. 3b and Table 3).
Discussion
In this nationally representative population-based study, the most recent current and spatial dynamics of major oral cancers were identified in different subpopulations in China. We found that overall ASMR and standardized YLL rates for oral cancer decreased from 2006 to 2021, with this trend also occurring in females and urban areas. The ASMR and standardized YLL rates of oral cancer in males were 2.31–3.16 times higher and 2.61–3.36 times higher than in females per year, respectively. Males had higher LLE than females due to oral cancer from 2006 to 2021. ASMR was 1.02–1.28 times higher in urban areas than in rural areas from 2006 to 2011, but 0.85–0.97 times lower from 2018 to 2021. The burden of disease also changed from higher in urban areas in 2006 to higher in rural areas in 2021.
The overall ASMR and standardized YLL rates in China were generally stable and slightly declining, and they showed a downward trend in 2006–2013 and 2018–2021, which was consistent with the global trend [20]. The slight increase after 2013 may be related to the enhancement of China's cancer screening capacity, the formulation and implementation of cancer prevention and control policies, and the low 5-year survival rate of oral cancer. For example, it coincides with the release and implementation of policies such as the Outline of China Cancer Prevention and Control Plan (2004 ~ 2010) and the Project Management Measures for Early Diagnosis and Treatment of Urban Cancer (Trial). The decline of ASMR of overall oral cancer after 2018 may be related to the improvement of dietary patterns and structure, as well as other influencing factors such as ultraviolet radiation (UVR) and the reduction of high-risk human papillomavirus (HPV) infection [21,22,23]. HPV-based testing is a pivotal part for cervical cancer screening besides cytology-based tests. To restrict and standardize HPV testing market, China released guidelines for the clinical performance evaluation for HPV testing against clinical endpoints in 2015 [24]. China has launched five vaccines since 2016, including Cervarix, Gardasil, Gardasil-9, Cecolin and Walrinvax. In addition, HPV vaccines are only approved for females, with RCTs in males ongoing [25]. It has been assessed that vaccination has effectively avoided a large number of cases and deaths [26]. In addition, some specific biomarkers are helpful to identify early oral cancer, make a better treatment plan for patients and improve the prognosis [27, 28].
ASMR and standardized YLL rates are significantly higher for males than that for females, indicating a sex difference in the burden of oral cancer disease, which is consistent with previous studies [29]. Other countries with similarly high ratios of male-to-female ASMR, including Brazil, Russia and the United States [30, 31]. This difference may be related to sex-specific lifestyles, occupational exposures, and physiological factors, with males being more exposed than females to risk factors such as smoking, alcohol and betel nut chewing [5, 32,33,34,35]. A study has shown that the risk of oral cancer is 123 times higher in the population who smoke, drink and chew betel nut than in the general population [36]. In China, smoking is much more prevalent among men than women, with rates of 47.2% and 2.7% respectively in 2013. The standardized smoking prevalence has remained consistently high: 26.0% in 2003, 24.9% in 2008, and 25.2% in 2013, with no statistically significant changes [37]. Alcohol consumption is significantly higher among Chinese men (55.6%) than women (15%) in 2007 [38]. In East Asia, including China, DPR Korea, and Taiwan, per capita alcohol consumption rose from 4.4 L in 1990 to 7.3 L in 2017, projected to reach 10.0 L by 2030 [39]. Pakistan, India and Bangladesh had the highest rates of oral cancer mortality, with the highest tobacco chewing prevalence, revealing a strong relationship between tobacco chewing and oral cancer. Brazil has adopted measures control tobacco, and the burden of oral cancer has been reduced, which is worth learning. Tobacco control may be the most cost-effective solution to reduce the burden of oral cancer [29]. Notably, the combination of smoking and drinking shows a synergistic effect [40]. Occupational exposure is also a risk factor for oral cancer in modern society, with more time occupational exposure to chlorinated solvents, oxygenated solvents, welding and other environments [6, 41]. For the perspective of physiological factors, the female body secretes estrogen and benefits from the protection of endogenous estrogen, thereby improving its adaptability to the environment [42]. Therefore, the disease burden of oral cancer for males in China is higher than that for females, suggesting that males are the key population in reducing the disease burden and we should pay more attention to this high-risk groups.
The mortality rates were higher in urban areas than in rural areas from 2006 to 2017, and higher in rural areas than in urban areas from 2018 to 2021, and the gap between urban and rural areas gradually narrowed and then widened. Higher stress in fast-paced urban populations may explain the high mortality rates in urban areas. A study in India has shown a significantly increased risk of oral cancer in the sample of stress and current health problems [43]. Studies have shown that tooth trauma and bleeding gums are highly associated with oral cancer [44]. The mortality rate lower in urban areas than in rural areas in recent years, may be related to the fact that the urban medical system is more complete than the rural one, the oral health awareness is stronger, and it is easier to be diagnosed and treated early [45].
Therefore, Chinese need to avoid or delay oral cancer through a healthy diet, maintaining oral hygiene, quitting smoking and limiting alcohol, and timely examination and treatment of oral related diseases, especially males and people in rural areas. In addition, educational attainment and socioeconomic status also have an impact on the disease burden of oral cancer [46, 47]. A cross-sectional study from Latin America showed that greater inequality, higher health expenditure per capita and greater investment in research and development were associated with a higher mortality rate from oral cancer [48]. An ecological study from Brazil showed that greater Bolsa Família Program (BFP) coverage was associated with lower oral cancer mortality rates, suggesting that Egalitarian strategies such as BFP can reduce the risk of death from oral cancer [49]. Targeted poverty alleviation policies may helpful to reduce the oral cancer mortality rate in this regard in China.
The advantage of this study is to analyze the changing trend of oral cancer mortality and disease burden by sex and area based on the Chinese death surveillance database, identify high-risk groups, and then explore the favorable measures and unfavorable factors of high-risk groups of oral cancer death, so as to provide early prevention strategies for reducing oral cancer mortality and disease burden in China. However, some limitations in this study should be considered. As data are not available in the China Death Surveillance Database, we have not yet analysed the burden of disease in different subsites. Morbidity information, Disability Adjusted Life Year (DALY) as the other two indicators of disease burden were not calculated because the surveillance content was mainly death data. Additionally, the latest available surveillance data is currently 2021. Since ICD codes were used to assess the cause of death, there might be certain selection bias or tendency in determining the main causes of death in how reporting is carried out at the national/areal/level. As the Chinese population ages, the trend of mortality and burden of disease in different age groups should be included in future studies.
By China Death Surveillance Database (2006–2021), our study analysed the trend of mortality and disease burden of lip, oral and pharyngeal malignancies, founding that the changing trends and disease burden of the major oral cancer are related to sex and area, to help achieve accurate early screening and warning of high-risk groups, and to provide a scientific basis for the government to formulate policies and improve the health status of residents in China.
Conclusions
To summarize, our study shows that the disease burden of oral cancer ASMRs in China remains stable or declining. Despite this, China still bears a huge burden of oral cancer. Males are much higher than females in both mortality and disease burden, and the gap of mortality and disease burden remains between rural and urban areas. Males and rural populations need to be focused on targeted interventions for the main influencing factors.
Availability of data and materials
The datasets generated and/or analysed during the current study are available in the "China death cause surveillance dataset" [https://ncncd.chinacdc.cn/jcysj/siyinjcx/syfxbg/].
Abbreviations
- ASMR:
-
Age-standardized Mortality Rates
- APC:
-
Annual Percent Changes
- AAPC:
-
Average Annual Percent Changes
- CI:
-
Confidence Interval
- DSPs:
-
Death Surveillance Points system
- GBD:
-
Global Burden of Disease
- ICD:
-
International Classification of Diseases
- LLE:
-
Loss of Life Expectancy
- PELL:
-
Proportion of Expected Life Lost
- YLL:
-
Years of Life Lost
References
Liu H, Huang Y, Huang M, Huang Z, Wang Q, Qing L, et al. Current Status, opportunities, and challenges of exosomes in oral cancer diagnosis and treatment. Int J Nanomedicine. 2022;17:2679–705.
Attar E, Dey S, Hablas A, Seifeldin IA, Ramadan M, Rozek LS, et al. Head and neck cancer in a developing country: a population-based perspective across 8 years. Oral Oncol. 2010;46(8):591–6.
Cancer Today. Available from: https://gco.iarc.fr/today/fact-sheets-cancers. Accessed 1 Sept 2023
Warnakulasuriya S, Kerr AR. Oral cancer screening: past, present, and future. J Dent Res. 2021;100(12):1313–20.
Shield KD, Ferlay J, Jemal A, Sankaranarayanan R, Chaturvedi AK, Bray F, et al. The global incidence of lip, oral cavity, and pharyngeal cancers by subsite in 2012. CA Cancer J Clin. 2017;67(1):51–64.
Gupta B, Johnson NW, Kumar N. Global epidemiology of head and neck cancers: a continuing challenge. Oncology. 2016;91(1):13–23.
Kumar M, Nanavati R, Modi TG, Dobariya C. Oral cancer: Etiology and risk factors: a review. J Cancer Res Ther. 2016;12(2):458–63.
Fioretti F, Bosetti C, Tavani A, Franceschi S, La Vecchia C. Risk factors for oral and pharyngeal cancer in never smokers. Oral Oncol. 1999;35(4):375–8.
D’Souza G, Kreimer AR, Viscidi R, Pawlita M, Fakhry C, Koch WM, et al. Case-control study of human papillomavirus and oropharyngeal cancer. N Engl J Med. 2007;356(19):1944–56.
Blot WJ, McLaughlin JK, Winn DM, Austin DF, Greenberg RS, Preston-Martin S, et al. Smoking and drinking in relation to oral and pharyngeal cancer. Cancer Res. 1988;48(11):3282–7.
Xie L, Shang Z. Changing trend of oral cancer disease burden in China from 1990 to 2019 and the forecast for the next 20 years. Oral Dis. 2024;30(2):195–206.
Zhang SK, Zheng R, Chen Q, Zhang S, Sun X, Chen W. Oral cancer incidence and mortality in China, 2011. Chin J Cancer Res. 2015;27(1):44–51.
Zhang LW, Li J, Cong X, Hu XS, Li D, Wu LL, et al. Incidence and mortality trends in oral and oropharyngeal cancers in China, 2005–2013. Cancer Epidemiol. 2018;57:120–6.
Liu S, Wu X, Lopez AD, Wang L, Cai Y, Page A, et al. An integrated national mortality surveillance system for death registration and mortality surveillance, China. Bull World Health Organ. 2016;94(1):46–57.
Wan X, Ren H, Ma E, Yang G. Mortality trends for ischemic heart disease in China: an analysis of 102 continuous disease surveillance points from 1991 to 2009. BMC Public Health. 2017;18(1):52.
Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19(3):335–51.
Wang Y, Chiang CJ, Lee WC. Age-standardized expected years of life lost: quantification of cancer severity. BMC Public Health. 2019;19(1):486.
Tsai SP, Wen CP, Tsai MK, Lu PJ, Wai JPM, Wen C, et al. Converting health risks into loss of life years - a paradigm shift in clinical risk communication. Aging (Albany NY). 2021;13(17):21513–25.
World (WHO 2000–2025) Standard. Available from: https://seer.cancer.gov/stdpopulations/world.who.html. Accessed 1 May 2023
Zhu S, Zhang F, Zhao G, Zhang X, Zhang X, Li T, et al. Trends in the global burden of oral cancer joint with attributable risk factors: Results from the global burden of disease study 2019. Oral Oncol. 2022;134: 106189.
Kreimer AR, Randi G, Herrero R, Castellsagué X, La Vecchia C, Franceschi S. Diet and body mass, and oral and oropharyngeal squamous cell carcinomas: analysis from the IARC multinational case-control study. Int J Cancer. 2006;118(9):2293–7.
Chaturvedi AK, Anderson WF, Lortet-Tieulent J, Curado MP, Ferlay J, Franceschi S, et al. Worldwide trends in incidence rates for oral cavity and oropharyngeal cancers. J Clin Oncol. 2013;31(36):4550–9.
Mathur S, Conway DI, Worlledge-Andrew H, Macpherson LM, Ross AJ. Assessment and prevention of behavioural and social risk factors associated with oral cancer: protocol for a systematic review of clinical guidelines and systematic reviews to inform Primary Care dental professionals. Syst Rev. 2015;4:184.
Zhang S, Xu H, Zhang L, Qiao Y. Cervical cancer: Epidemiology, risk factors and screening. Chin J Cancer Res. 2020;32(6):720–8.
Zhao C, Zhao Y, Li J, Li M, Shi Y, Wei L. Opportunities and challenges for human papillomavirus vaccination in China. Hum Vaccin Immunother. 2024;20(1):2329450.
Zhou L, Gu B, Wang J, Liu G, Zhang X. Human papillomavirus vaccination at the national and provincial levels in China: a cost-effectiveness analysis using the PRIME model. BMC Public Health. 2022;22(1):777.
Chu HW, Chang KP, Hsu CW, Chang IY, Liu HP, Chen YT, et al. Identification of Salivary Biomarkers for Oral Cancer Detection with Untargeted and Targeted Quantitative Proteomics Approaches. Mol Cell Proteomics. 2019;18(9):1796–806.
Lu Z, He Q, Liang J, Li W, Su Q, Chen Z, et al. miR-31-5p Is a potential circulating biomarker and therapeutic target for oral cancer. Mol Ther Nucleic Acids. 2019;16:471–80.
Zhang SZ, Xie L, Shang ZJ. Burden of oral cancer on the 10 most populous countries from 1990 to 2019: estimates from the global burden of disease study 2019. Int J Environ Res Public Health. 2022;19(2):875.
Antunes J, Toporcov TN, Biazevic MG, Boing AF, Bastos JL. Gender and racial inequalities in trends of oral cancer mortality in Sao Paulo. Brazil Rev Saude Publica. 2013;47(3):470–8.
Lipsky MS, Su S, Crespo CJ, Hung M. Men and oral health: a review of sex and gender differences. Am J Mens Health. 2021;15(3):15579883211016360.
Lee YA, Li S, Chen Y, Li Q, Chen CJ, Hsu WL, et al. Tobacco smoking, alcohol drinking, betel quid chewing, and the risk of head and neck cancer in an East Asian population. Head Neck. 2019;41(1):92–102.
Guo SE, Huang TJ, Huang JC, Lin MS, Hong RM, Chang CH, et al. Alcohol, betel-nut and cigarette consumption are negatively associated with health promoting behaviors in Taiwan: a cross-sectional study. BMC Public Health. 2013;13:257.
Lu Y, Sobue T, Kitamura T, Matsuse R, Kitamura Y, Matsuo K, et al. Cigarette smoking, alcohol drinking, and oral cavity and pharyngeal cancer in the Japanese: a population-based cohort study in Japan. Eur J Cancer Prev. 2018;27(2):171–9.
Chen F, He BC, Yan LJ, Liu FP, Huang JF, Hu ZJ, et al. Tea consumption and its interactions with tobacco smoking and alcohol drinking on oral cancer in southeast China. Eur J Clin Nutr. 2017;71(4):481–5.
Murphy N, Strickler HD, Stanczyk FZ, Xue X, Wassertheil-Smoller S, Rohan TE, et al. A prospective evaluation of endogenous sex hormone levels and colorectal cancer risk in postmenopausal women. J Natl Cancer Inst. 2015;107(10):djv210.
Wang M, Luo X, Xu S, Liu W, Ding F, Zhang X, et al. Trends in smoking prevalence and implication for chronic diseases in China: serial national cross-sectional surveys from 2003 to 2013. Lancet Respir Med. 2019;7(1):35–45.
Li Y, Jiang Y, Zhang M, Yin P, Wu F, Zhao W. Drinking behaviour among men and women in China: the 2007 China Chronic Disease and Risk Factor Surveillance. Addiction. 2011;106(11):1946–56.
Manthey J, Shield KD, Rylett M, Hasan OSM, Probst C, Rehm J. Global alcohol exposure between 1990 and 2017 and forecasts until 2030: a modelling study. Lancet. 2019;393(10190):2493–502.
Chi AC, Day TA, Neville BW. Oral cavity and oropharyngeal squamous cell carcinoma–an update. CA Cancer J Clin. 2015;65(5):401–21.
Carton M, Barul C, Menvielle G, Cyr D, Sanchez M, Pilorget C, et al. Occupational exposure to solvents and risk of head and neck cancer in women: a population-based case-control study in France. BMJ Open. 2017;7(1):e012833.
Clegg D, Hevener AL, Moreau KL, Morselli E, Criollo A, Van Pelt RE, et al. Sex hormones and Cardiometabolic health: role of estrogen and estrogen receptors. Endocrinology. 2017;158(5):1095–105.
Dholam KP, Chouksey GC. Squamous cell carcinoma of the oral cavity and oropharynx in patients aged 18–45 years: A case-control study to evaluate the risk factors with emphasis on stress, diet, oral hygiene, and family history. Indian J Cancer. 2016;53(2):244–51.
Marques LA, Eluf-Neto J, Figueiredo RA, Góis-Filho JF, Kowalski LP, Carvalho MB, et al. Oral health, hygiene practices and oral cancer. Rev Saude Publica. 2008;42(3):471–9.
Gupta B, Bray F, Kumar N, Johnson NW. Associations between oral hygiene habits, diet, tobacco and alcohol and risk of oral cancer: a case-control study from India. Cancer Epidemiol. 2017;51:7–14.
Balaram P, Sridhar H, Rajkumar T, Vaccarella S, Herrero R, Nandakumar A, et al. Oral cancer in southern India: the influence of smoking, drinking, paan-chewing and oral hygiene. Int J Cancer. 2002;98(3):440–5.
Kadashetti V, Chaudhary M, Patil S, Gawande M, Shivakumar KM, Patil S, et al. Analysis of various risk factors affecting potentially malignant disorders and oral cancer patients of Central India. J Cancer Res Ther. 2015;11(2):280–6.
Freire AR, Freire D, de Araújo ECF, de Almeida Carrer FC, PuccaJúnior GA, de Sousa SA, et al. Socioeconomic indicators and economic investments influence oral cancer mortality in Latin America. BMC Public Health. 2021;21(1):377.
Costa EM, Rocha N, Rocha TAH, Lima HLO, Vissoci JRN, Queiroz RCS, et al. Bolsa Família Program and deaths from oral cancer in Brazil: an ecological study. Rev Panam Salud Publica. 2022;46:e208.
Acknowledgements
Authors thank Dr. Jianying Zhang for his support and helpful comments for this study.
Funding
This work was supported by the Funded Project of International Training of High-level talents in Henan Province [no number] and the Project of Tackling Key Problems in Science and Technology of Henan Province [242102311140].
Author information
Authors and Affiliations
Contributions
Peng Wang, Jicun Zhu and Xiaoyue Zhang conducted study design and study concepts. Weihong Xie, Hua Ye, Xiaoyue Zhang, Yaxin Zhang and Zhong Zheng conducted data acquisition and quality control of data and algorithms. Peng Wang, Xiaoyue Zhang and Chong Sheng conducted data analysis and interpretation and statistical analysis. Xiaoyue Zhang, Guiying Sun, Haiyan Liu and Jiaxin LI conducted manuscript preparation and manuscript editing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhang, X., Xie, W., Ye, H. et al. Mortality and disease burden of oral cancer in China: a time-trend analysis on the China Death Surveillance Database from 2006 to 2021. BMC Oral Health 24, 938 (2024). https://doi.org/10.1186/s12903-024-04717-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12903-024-04717-5