Abstract
Background
Dental simulation games are virtual educational games that help children get familiar with different dental procedures. This study aimed to evaluate the pretreatment exposure to the “Baby Panda Dental Care” game in reducing pain and anxiety in comparison with the tell-show-do (TSD) technique during primary molars pulpotomy for patients aged 6–10 years.
Materials and methods
It was a triple-blinded, two-arm, parallel-group, randomized, active-controlled trial. It was done on 60 patients, who were randomly divided into two groups: the control group, TSD technique (n = 30), and the experimental group, “Baby Panda Dental” Care (n = 30). For the TSD technique, children were provided with a verbal explanation followed by a demonstration of the dental treatment in a non-threatening way. The “do” phase is then initiated during performing treatment. For the “Baby Panda dental care” game, children were asked to play for 5 min before treatment, selecting root canal therapy procedures. Pulse rate and RMS pictorial scale were recorded at four time points: (1) at the baseline (t0). (2) After conditioning the child (t1). (3) During treatment (t2). (4) After finishing the treatment (t3). Face, Legs, Activity, Cry, Consolability (FLACC) behavioral pain scale was recorded during treatment (t2).
Results
The pulse rate is higher in the control group at t1 (p = 0.012) and t2 (p = 0.015). There was a statistically significant difference in the mean RMS pictorial scale score at t1 (p < 0.001), t2 (p = 0.006), and t3 (p < 0.001), a statistically significant difference was noticed in FLACC behavioral pain assessment between the two groups (p = 0.033).
Conclusions
The mobile dental game showed better results than the TSD technique, but neither technique did not reduce anxiety and pain effectively during dental treatment.
Trial registration
The trial was registered at the ISRCTN registry (ISRCTN30470866) on 19/04/2024.
Similar content being viewed by others
Background
Dental anxiety is considered a vicious cycle, where avoidance of attending the clinic and lack of cooperation during treatment are common consequences. Thus, dental anxiety leads to poor oral health and painful dental experiences, which escalate over time. In addition, uncontrolled behavior during dental sessions leads to subsequent dental failure [1]. Otherwise, dental pain and anxiety are two sides of the same coin since painful dental experiences lead to dental anxiety, and dental anxiety exaggerates dental pain [2]. According to Grisolia et al. [3], the global prevalence of dental anxiety is 25.8%.
Primary molars pulpotomy is the most common dental procedure among pediatric patients, which consists of several distressing steps. Receiving multiple injections, the sight of sharp metallic instruments, unfamiliar smells, and applying bulky apparatus such as rubber dam can induce anxiety. The sound of the high-pitched drill and the suctioning sound can even trigger anxiety in the waiting room before dental treatment [4, 5]. Therefore, according to the American Academy of Pediatric Dentistry (AAPD), the pediatric dentist must master various behavior guidance techniques to meet the intellectual, physical, and emotional needs of the pediatric patient. Tell-show-do (TSD) is a basic guidance technique that includes a verbal explanation of the dental procedure, followed by a demonstration of different sensory aspects of the treatment, and then completion of the treatment in correspondence with explanation and demonstration. TSD technique aims to address the fear evoked by the unknown and is considered the gold standard of the non-pharmacological behavior guidance technique [6].
Dental simulation games are virtual educational games that help children get familiar with different dental procedures and tools and increase acceptance towards treatment [7]. Baby Panda Dental Care is a mobile app that lets children enjoy the experience of being a dentist and perform different dental procedures such as extraction, scaling, drilling, filling, aligning brackets, and much more. This study aimed to evaluate the pre-treatment exposure to the Baby Panda Dental Care game in reducing pain and anxiety in comparison with the TSD technique during primary molars pulpotomy in pediatric patients aged 6–10 years.
Materials and methods
Study setting and ethical considerations
This study was designed as a triple-blinded, two-arm, parallel-group randomized active-controlled trial and conducted at the Department of Pediatric Dentistry, Faculty of Dentistry, Damascus University, Syria, between February 2024 and March 2024. The study was performed in full accordance with the CONSORT checklist [8] and the World Medical Association Declaration of Helsinki on experimentation involving human subjects, as revised in 2013 [9]. The legal guardians provided written informed consent before the participants’ inclusion in the study, and the participants’ anonymity was preserved. The dental procedure was explained in detail. No child was excluded based on their gender, race, and socioeconomic status, and excluded children still received complete treatment. Ethical approval was obtained from the Ethical Committee of Damascus University (N1325/2024), and the trial was approved and registered at the ISRCTN registry (ISRCTN30470866) on 19/04/2024.
Sample size
Sample size calculation was done using G*Power version 3.1.9.4 (G*Power 3.1.9, Heinrich Hein Universität Düsseldorf, Düsseldorf, Germany). A sample size of 60 patients achieved a small effect size f (0.36), 80% Power (1 - β err prob) [10], and a significance level of 0.05 [11]. The effect size was estimated based on a pilot study on 10 subjects [12].
Participant recruitment and grouping
67 patients who were referred to the Department of Pediatric Dentistry were screened according to the following recruitment criteria:
Inclusion criteria
-
1.
Children aged 6–10 years.
-
2.
Children are categorized as definitely positive or positive ratings, according to Frankel’s behavior rating scale.
-
3.
Children requiring pulpotomy for a primary molar.
-
4.
Children who are familiar with smartphone games.
Exclusion criteria
-
1.
Children with oral, mental, and/or systemic conditions.
-
2.
Children are categorized as definitely negative or negative ratings, according to Frankel’s behavior rating scale.
-
3.
Children with previous exposure to local anesthesia.
Based on inclusion criteria, 60 patients were recruited and randomly divided into two groups:
-
Group 1: control group, TSD technique (n = 30).
-
Group 2: experimental group, Baby Panda Dental Care game (Baby Panda Dental Care, BabyBus Co., Fuzhou, China) (n = 30).
Randomization and blinding
Participants were randomly assigned into two groups in a ratio of 1:1 according to the randomization online software: https://www.randomizer.org. The number of sets was 2, with 30 patients per set, and the number range was from 1 to 60. It was a triple-blinded trial where the pediatric dentist and the outcome assessors were masked to the group allocation. In addition, participants were not aware of the grouping and the aim of the study.
Primary outcome measures
The following primary outcome measures were considered:
-
1.
Pulse rate.
The pulse rate was measured using a finger pulse oximeter (Alpha, Prolinx GmbH, Düsseldorf, Germany) at four time points: (1) at the baseline in the waiting room (t0). (2) After conditioning the child before initiating the treatment (t1). (3) Mean pulse rate during treatment (t2). The pulse rate was recorded after injection and immediately after amputation of the pulp. (4) After finishing the treatment (t3) [13]. Pulse rate is an objective measurement of dental anxiety [14].
-
2.
RMS Pictorial Scale.
RMS pictorial scale was recorded at four time points: (1) at the baseline in the waiting room (t0). (2) After conditioning the child before initiating the treatment (t1). (3) Immediately after amputating of the pulp (t2). (4) After finishing the treatment (t3). RMS pictorial scale is a subjective measurement of dental anxiety [15].
-
3.
Face, Legs, Activity, Cry, Consolability (FLACC) behavioral pain scale.
FLACC behavioral pain scale was recorded during treatment (t2). FLACC behavioral pain assessment scale is a non-verbal pain scale (Table 1) [16].
Procedure
The baseline anxiety level in the waiting room was assessed by recording the pulse rate and using the RMS pictorial scale. Children were presented with two sets of five faces based on their gender and were asked to select the most suitable face that matched their current level of anxiety. For the TSD technique group, children were provided with a verbal explanation followed by a demonstration of the dental treatment in a friendly, non-threatening way. The “do” phase was performed after initiating the dental treatment without deviating from the verbal explanation and demonstration. For the Baby Panda dental care game, Arabic was installed, and children were asked to play for 5 min. It includes five dental procedures: restoring chipped teeth, filling cavities, performing root canal therapy, extracting decayed teeth, and performing orthodontic treatment for five little animals: a cat, hippo, mouse, bunny, and monkey. The different stages of the selected procedure are presented in Fig. 1. Children were presented with two animals in the waiting room, and then a root canal therapy virtual procedure was selected. Children were instructed to remove the dental calculus using an ultrasonic scaler, clean teeth using a water gun, and then suction dirty water. Children were instructed to perform an intraoral radiograph of the decayed tooth, drill the decayed cavity, anesthetize the nerve cells using an electric gun, fill the tooth, polish the teeth to fit well with the dental crown, and then put the dental crown. Pulse rate and RMS pictorial scale were recorded after conditioning the child when sitting on a dental chair before initiating the dental treatment. The conventional pulpotomy method was performed according to AAPD guidelines. During treatment, the FLACC behavioral pain scale and pulse rate were recorded by two blinded investigators. After finishing the cavity preparation and amputation of the pulp RMS pictorial scale was recorded. It was recorded during controlling hemorrhage using a wet cotton pellet. After removing the rubber dam and cementing the stainless steel crown, the pulse rate and RMS pictorial scale were recorded [13, 15]. Cohen’s Kappa coefficient values of intra-examiner and inter-examiner reliability were > 0.8 [17].
The different stages of the virtual root canal therapy procedure. (A) The little animal with root canal therapy was selected. (B) The removal of the dental calculus using an ultrasonic scaler. (C) Rinsing teeth using a water gun (D) suctioning dirty water. (E) Performing a dental X-ray. (F) Drilling the decayed cavity. (G) Anesthetizing the nerve cells using an electric gun. (H) Filling the tooth. (I) Polishing the teeth to fit well with the dental crown. (J) Putting the dental crown [30]
Statistical analysis
Statistical analysis was performed using IBM SPSS software version 24 (IBM SPSS Statistics® version 24, IBM Corp., New York, USA). Descriptive statistics were presented as mean and standard deviation (SD). The normality of data was checked by performing the Kolmogorov–Smirnov test. Fisher’s exact test and Mann-Whitney U test were performed to compare baseline demographic and clinical characteristics between groups. Mann-Whitney U test was used for comparing pulse rate, RMS pictorial scale, and FLACC behavioral pain assessment scale scores between control and experimental groups. The statistical significance level was adjusted at 0.5 (p < 0.5).
Results
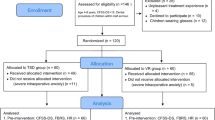
The CONSORT flow diagram is presented in Fig. 2. A total of 60 patients completed the full treatment. Table 2 shows the baseline demographic and clinical characteristics of participants. Of the participants, 71.67% were male, and 28.33% were female. The mean age was 7.47 (SD 1.08; range 6–10 years). Most participants (93.33%) had a previous dental experience, and among those who had a previous dental experience, 42.86% were definitely positive, and 57.14% were positive, according to Frankel’s behavior rating scale. 48.33% of dental procedures were located in the maxilla, and 51.67% were located in the mandible. No statistically significant difference was found between the baseline characteristics of the study participants with p = 1.000, p = 0.429, p = 0.612, p = 0.787, and p = 1.000, respectively, suggesting that the baseline demographic clinical characteristics were homogenous.
Table 3 shows the pain and anxiety scores of the study participants at different time points. There was no statistically significant difference in the mean pulse rate between the experimental and the control group at t0 (p = 0.994). In addition, there was no statistically significant difference between the control and the experimental group in the mean RMS pictorial scale score at t0 (p = 0.522), indicating that the baseline level of anxiety was homogenous among participants. There was a statistically significant difference in the mean pulse rate between the control and the experimental group at t1 (p = 0.012) and t2 (p = 0.015). Similarly, the mean change in the pulse rate from the baseline to these time points was a statistically significant difference between the experimental and the control group, with p = 0.013 and p = 0.001, respectively. In the control group, the mean pulse rate was higher at t1 (99.63 ± 13.50) compared to t0 (89.63 ± 12.32). On the contrary, the mean pulse rate was higher at t0 (91.47 ± 9.50) compared to t1 (88.57 ± 13.36) in the experimental group. These results indicate that the physiological response to dental anxiety is higher in the control group compared to the experimental group after conditioning the child and performing the dental treatment (Fig. 3). However, the mean pulse rate of both groups at t2 was higher than the pulse rate at t0, indicating that both techniques did not reduce anxiety effectively during dental treatment. There was no statistically significant difference in the mean pulse rate between the experimental and the control group at t3 (p = 0.158) and in the mean change in the pulse rate from the baseline to t3 (p = 0.122), suggesting that the level of anxiety after finishing the treatment was similar to that at the baseline (Fig. 3). However, there was a statistically significant difference in the mean RMS pictorial scale score between the control and the experimental group at t1 (p < 0.001), t2 (p = 0.006), and t3 (p < 0.001), indicating that children’s subjective report of anxiety was higher in the control group compared to the experimental group after conditioning the child, during the dental procedure, and after completion the treatment. Regarding pain level during dental treatment, there was a statistically significant difference between the control and the experimental group in FLACC behavioral pain assessment at t2 (p = 0.033), indicating that the pain reported was higher in the control group compared to the experimental group.
Discussion
Dental pain and anxiety are two sides of the same coin, and they often lead to poor oral health due to the avoidance of dental treatment and uncontrolled behavior during various procedures [1, 2]. Primary molar pulpotomy is the most common dental treatment among pediatric patients, and it consists of several irritating steps that can induce pain and anxiety [4, 5]. Dental stimulation games help children get familiar with different dental procedures and instruments that address the fear of the unknown [7]. Therefore, this study aimed to evaluate the pretreatment exposure to the Baby Panda Dental Care game in reducing pain and anxiety compared with the TSD technique during primary molars pulpotomy in pediatric patients aged 6–10.
Children belonging to the 6–10 years category group were included in the current study because they are expected to cooperate during dental treatment, accurately express their pain and anxiety according to different scales [18, 19], and follow the instructions while playing virtual games [4]. In addition, primary molar pulpotomies are frequent among this age group [20].
Pulse rate is an objective and physiological measurement of dental anxiety [14], while the RMS pictorial scale is a subjective measurement where children themselves report their current level of anxiety. RMS pictorial scale is a validated anxiety assessment scale, which is quick, simple, and efficient as it is colorful, attractive, and consists of original photographs for males and females [21]. FLACC behavioral pain assessment scale is a non-verbal pain scale that is reliable and accurate [16].
Baby Panda Dental Care Game is a virtual educational game that provides dental care for little animals, and children help them solve their dental problems by applying various procedures and using different tools and instruments. It includes five dental procedures: restoring chipped teeth, filling cavities, performing root canal therapy, extracting decayed teeth, and performing orthodontic treatment for five little animals: a cat, hippo, mouse, bunny, and monkey. The root canal therapy virtual game was chosen because it is similar to pulpotomy treatment since it requires local anesthesia, caries removal, access cavity preparation, stamping the pulp with appropriate dental materials, and putting a dental crown. TSD technique was selected as the control group because it is the gold standard behavior guidance technique, widely accepted, and most dentists are familiar with it [22].
The results of the current study indicated that the physiological response to dental anxiety and children’s subjective reports of anxiety are higher in the control group compared to the experimental group after conditioning the child. In addition, the level of anxiety after applying the TSD technique was higher than the baseline level. The result can be attributed to the fact that mobile games present the dental procedure in an attractive, interactive, and playful manner, and children can imagine themselves in a friendly, joyful environment [11, 15]. According to Derbala et al. [23], 55% of communication is based on visual elements, and 7% is based on words, which makes the TSD technique a less attractive manner for presenting dental procedures. The result is consistent with Meshki et al. [13] findings, which concluded that the TSD technique exaggerates anxiety. A dental simulation game reduces the physiological response to dental anxiety immediately after conditioning the child. According to Tahersoltani et al. [24], the pulse rate is not affected after applying the TSD technique, while the tiny dentist game significantly reduces the pulse rate. However, Radhakrishna et al. [25] suggested that both the TSD technique and the smartphone dental game significantly reduce dental anxiety. The controversial results can be attributed to the differences in the study designs and age range. Similarly, the results of the current study showed that the physiological response to dental anxiety and children’s subjective reports of anxiety are higher in the control group compared to the experimental group during dental treatment. This result is in agreement with Radhakrishna et al. [25] findings, which suggested that mobile App is superior to TSD techniques in reducing anxiety during dental treatment. However, the objective and subjective levels of anxiety of both groups during treatment were higher than the anxiety level at the baseline, indicating that both techniques did not reduce anxiety effectively during dental treatment. The increase in the pulse rate can be attributed to vasoconstrictors added to local anesthetics [26]. The result is consistent with Tahersoltani et al. [24] and Meshki et al. [13] findings. However, the current result is in contrast with Sedky et al. [27], Aziz et al. [28], Abbasi et al. [29], and Elicherla et al. [15], which suggested that the pulse rate during treatment in the mobile dental game group was lower than the baseline. However, these disagreements can be attributed to the differences in dental treatment, clinical settings, and methodologies. The current results suggested that the pain reported was higher in the control group compared to the experimental group, and this can be attributed to the fact that anxious children experience pain more intensely. The result is in contrast with Meshki et al. [13] findings, which suggested that playing mobile games does not affect the pain level. The pulse rate after finishing the treatment was similar to that at the baseline in both groups. However, children’s subjective report of anxiety was higher in the control group compared to the experimental group after completion of the treatment. The lack of consistency between objective and subjective expression of postoperative anxiety can be explained by the existence of an unpleasant memory of a painful experience in the TSD technique group.
This study has limitations. First, this study only evaluated the short-term effect of playing the game in the waiting room of the dental clinic. Second, the unequal distribution of gender across the study groups. Third, the application of a rubber dam is one of the steps in the pulpotomy procedure which is not there in the game.
Conclusions
Based on our findings, the mobile dental game was superior to the TSD technique in controlling subjective and objective anxiety levels and pain during primary molars pulpotomy. However, both the mobile dental game and the TSD technique did not reduce anxiety and pain effectively during dental treatment.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Caltabiano ML, Croker F, Page L, Sklavos A, Spiteri J, Hanrahan L, Choi R. Dental anxiety in patients attending a student dental clinic. BMC Oral Health. 2018;18:1–8.
Sakamoto E, Yokoyama T. Pain and anxiety in dentistry and oral and maxillofacial surgery focusing on the relation between pain and anxiety. Ann Pain Med. 2018;1:1002.
Grisolia BM, Dos Santos AP, Dhyppolito IM, Buchanan H, Hill K, Oliveira BH. Prevalence of dental anxiety in children and adolescents globally: a systematic review with meta-analyses. Int J Pediatr Dent. 2021;31:168–83.
Alsibai E, Bshara N, Alzoubi H, Alsabek L. Assessing an active distracting technique during primary mandibular molar pulpotomy (randomized controlled trial). Clin Experimental Dent Res. 2023;9:283–9.
Antoniadou M, Tziovara P, Antoniadou C. The Effect of Sound in the Dental Office: practices and recommendations for Quality Assurance—A narrative review. Dentistry J. 2022;10:228.
Townsend JA, Wells MH. Behavior guidance of the pediatric dental patient. In Pediatric dentistry 2019:352–370. Elsevier.
Varun P, Rekha V, Annamalai S. Effectiveness of simulation games in behaviour modification of children. Int J Contemp Dentistry. 2016;7.
Cuschieri S. The CONSORT statement. Saudi J Anaesth. 2019;13:S27–30.
World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310:2191–4.
Gupta KK, Attri JP, Singh A, Kaur H, Kaur G. Basic concepts for sample size calculation: critical step for any clinical trials! Saudi J Anaesth. 2016;10:328–31.
Miller J, Ulrich R. The quest for an optimal alpha. PLoS ONE. 2019;14:e0208631.
Fritz CO, Morris PE, Richler JJ. Effect size estimates: current use, calculations, and interpretation. J Exp Psychol Gen. 2012;141:2.
Meshki R, Basir L, Alidadi F, Behbudi A, Rakhshan V. Effects of pretreatment exposure to dental practice using a smartphone dental simulation game on children’s pain and anxiety: a preliminary double-blind randomized clinical trial. J Dentistry (Tehran Iran). 2018;15:250.
Kalra N, Sabherwal P, Tyagi R, Khatri A, Srivastava S. Relationship between subjective and objective measures of anticipatory anxiety prior to extraction procedures in 8-to 12-year-old children. J Dent Anesth pain Med. 2021;21:119.
Elicherla SR, Bandi S, Nuvvula S, subbareddy Challa R, Saikiran KV, Priyanka VJ. Comparative evaluation of the effectiveness of a mobile app (little lovely dentist) and the tell-show-do technique in the management of dental anxiety and fear: a randomized controlled trial. J Dent Anesth pain Med. 2019;19:369.
Crellin D, Harrison D, Santamaria N, Babl FE. Comparison of the psychometric properties of the FLACC scale, the MBPS and the observer applied visual analogue scale used to assess procedural pain. J pain Res. 2021:881–92.
McHugh ML. Interrater reliability: the kappa statistic. Biochemia Med. 2012;22:276–82.
Von Baeyer CL. Children’s self-report of pain intensity: what we know, where we are headed. Pain Res Manage. 2009;14:39–45.
von Baeyer CL. Children’s self-reports of pain intensity: scale selection, limitations and interpretation. Pain Res Manage. 2006;11:157–62.
Balamithra S, Govindaraju L. Pulpotomy in children treated under General Anaesthesia-A Retrospective Cohort Study. J Adv Zool. 2023;44.
Shetty RM, Khandelwal M, Rath S, RMS Pictorial Scale (RMS-PS). An innovative scale for the assessment of child′ s dental anxiety. J Indian Soc Pedod Prev Dentistry. 2015;33:48–52.
Zhu M, Yu H, Xie B, Li H, He Q, Li H, Su J, Li X. Experiential learning for children’s dental anxiety: a cluster randomized trial. BMC Oral Health. 2020;20:1–8.
Derbala G, Khalil AM, Soliman RS. Effectiveness of smart phone application in reducing anxiety during pediatric dental procedures: a randomized controlled trial. Alexandria Dent J. 2022;47:196–204.
Tahersoltani A, Heidari A, Ghadimi S, Shamshiri AR. Effect of the tiny dentist game on 4–10 years old children’s anxiety compared with tell-show-do method: a clinical trial. J Dent Probl Solutions. 2021;8:34–41.
Radhakrishna S, Srinivasan I, Setty JV, DR MK, Melwani A, Hegde KM. Comparison of three behavior modification techniques for management of anxious children aged 4–8 years. J Dent Anesth pain Med. 2019;19:29.
Wakita R, Ito T, Fukayama H. Small doses of adrenaline contained in the local anaesthetic may result in prolonged increased cardiac function even after the vital signs return to normal. Adv Oral Maxillofacial Surg. 2021;3:100104.
Sedky MM, Waly N, Abdel Samee P. Mobile app versus tell-Show-Do technique in reduction of anxiety and pain during administration of local anaesthesia in children: a Randomized Clinical Trial. Adv Dent J. 2024;6:1–3.
Aziz SZ, Jafar ZJ. The efficacy of little lovely dentist and tell show do in alleviating dental anxiety in Iraqi children: a Randomized Clinical Trial. J Int Soc Prev Community Dentistry. 2023;13:388–93.
Abbasi H, Saqib M, Jouhar R, Lal A, Ahmed N, Ahmed MA, Alam MK. The efficacy of little lovely dentist, dental song, and tell-show-do techniques in alleviating dental anxiety in paediatric patients: a clinical trial. Biomed Res Int. 2021;2021:1–7.
BabyBus. BabyBus For Kids, For the Future. www.babybus.com. Accessed. 2022.
Acknowledgements
Not applicable.
Funding
This research is funded by Damascus University – funder No. 501100020595.
Author information
Authors and Affiliations
Contributions
M.K. data curation, performed the statistical analysis, wrote the manuscript. M.N.A. & M.L. performed critical revision of the manuscript. N.B. research concept and design, performed critical revision of the manuscript. All authors have approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was obtained from the ethical committee at Damascus University (N1325/2024). The study was performed in accordance with the Declaration of Helsinki, and written informed consent was obtained from participants’ legal guardians.
Consent for publication
Consent for publication was obtained from participants’ legal guardians.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Karkoutly, M., Al-Halabi, M.N., Laflouf, M. et al. Effectiveness of a dental simulation game on reducing pain and anxiety during primary molars pulpotomy compared with tell-show-do technique in pediatric patients: a randomized clinical trial. BMC Oral Health 24, 976 (2024). https://doi.org/10.1186/s12903-024-04732-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12903-024-04732-6