Abstract
Background
Digitally fabricated dentures may require relining due to continual alveolar ridge resorption. However, studies evaluating the tensile bond strength (TBS) of digitally fabricated dentures bonded to denture liners are lacking. This study aimed to evaluate the TBS of autopolymerized, heat-polymerized, milled, and 3D printed denture base materials bonded to 2 acrylic-based and 2 silicone-based denture liners, both before and after thermocycling. Additionally, the impact of thermocycling on the TBS were also evaluated.
Methods
The TBS of 4 different denture base materials (Palapress (PL), Vertex Rapid Simplified (VR), Smile CAM total prosthesis (SC), and NextDent denture 3D+ (ND)) bonded to 2 acrylic-based (GC Soft-Liner (GC) and Tokuyama Rebase II (RB)) and 2 silicone-based (Ufi Gel P (UP) and Sofreliner Tough M (ST)) denture liners were tested. Specimens (n = 8) were divided into non-thermocycling and thermocycling groups. Non-thermocycling specimens were tested after 24-hours water immersion, while thermocycling specimens were underwent 5000 cycle and were immediately tested. Mode of failure was examined under a stereomicroscope. Data were analyzed using 2-way ANOVA and Tukey HSD tests (α = 0.05), and independent samples t test (α = 0.05) for TBS between non-thermocycling and thermocycling groups.
Results
For the non-thermocycling groups, within the same denture liner material, no significant differences were found between denture base materials, except the ND + RB group, which had significantly lower TBS. For the thermocycling groups, within the same denture liner material, the TBS in the PL group exhibited the highest and the ND group exhibited the lowest. Within the same denture base material, in both non-thermocycling and thermocycling groups, the TBS in the ST group exhibited the highest; in contrast, that in the GC group exhibited the lowest. No significant differences were observed in TBS between non-thermocycling and thermocycling groups, except for denture base materials bonded to the ST group, SC + UP, and ND + UP groups.
Conclusions
Milled denture base can be relined with acrylic-based or silicone-based denture liner. However, cautions should be exercised when relining 3D printed denture base. Thermocycling did not affect TBS between acrylic-based denture liners and denture bases. In contrast, it affected the bond between silicone-based denture liner and denture base.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Complete dentures have been a standard treatment for patients who present with complete edentulism, offering affordability, simplicity, esthetics, and functionality.1 For fabricating conventional complete denture bases, polymethyl methacrylate (PMMA) material is commonly used due to its favorable properties, such as low density, esthetics, cost-effectiveness, and ease of manipulation [1]. However, PMMA material has several drawbacks, such as high polymerization shrinkage, lack of radiopacity, allergic reactions to residual monomers, and low wear resistance in saliva [2, 3].
Digital technology has gained popularity in many fields including dentistry [4]. Digital denture workflows can reduce the number of appointments and chair time, and enable denture replacement for patients who lose their dentures by fabricating them from existing data. The advancement of digital technology has also changed the approach to denture processing methods. Complete dentures can now be produced using computer-aided design-computer-aided manufacturing (CAD-CAM) techniques, alongside conventional heat-polymerized and autopolymerization methods [5]. Two main CAD-CAM techniques commonly used for fabricating dentures are subtractive manufacturing and additive manufacturing [5]. In subtractive manufacturing, the denture base is milled from a pre-polymerized PMMA blank, and the denture teeth are subsequently bonded to the base. Using the PMMA blank can reduce the denture base’s surface porosity and polymerization shrinkage. The main disadvantage of the subtractive manufacturing technique is the waste from unused portions of the PMMA blank. The additive manufacturing, also known as 3D printing, is a method that utilizes photosensitive thermoset liquid monomers to polymerize materials layer by layer, forming the object and its supporting structures [6]. Despite having inferior values for mechanical strength, the additive manufacturing provides several benefits such as reducing material waste, minimizing the number of steps to reach final product, and therefore requiring less human intervention and reducing possibility for errors [7, 8]. Moreover, the strength of material produced by additive manufacturing depends on the printing orientation [9] and particle incorporation [10].
The dynamic nature of alveolar bone continual remodeling requires periodic maintenance for denture adjustments to maintain fit and stability [11, 12]. Therefore, denture relining procedures have become increasingly important for solving ill-fitting denture issues. Denture processing methods have been shown to influence the surface properties of denture base material, which will affect the bonding to denture liners [13]. Since CAD-CAM is a new technique of denture manufacturing, there are limited information on the bonding properties of digitally fabricated denture bases to denture liner materials. Denture liner materials can be categorized into 2 groups based on chemical composition: acrylic-based and silicone-based. Acrylic-based denture liner is produced by adding plasticizers and alcohol-based liquid to the acrylic resin. Silicone-based denture liner is a mixture of siloxane and silica that remains soft after cross-linking [14]. 40% of digital dentures required relining due to loss of retention during an initial (≤ 4 weeks after insertion) and functional period (> 4 weeks after insertion) [15]. A previous study also reported that denture relining was the most common procedure during the maintenance phase of conventional complete dentures [16].
Thermocycling is a process commonly used in dental laboratory research to simulate temperature changes in the oral environment, leading to the continuous expansion and contraction of both the denture liner and the denture base material. This process creates tension at the bonded interface and results in thermal volumetric changes [17]. Studies have reported that the tensile bond strength of denture bases bonded to silicone-based denture liners, such as Molloplast B and Permaflex, decreased after thermocycling [18, 19]. Recent studies have evaluated the bond strength between denture liner materials to additive-manufactured denture base compared with subtractive-manufactured, conventional heat-polymerized, and autopolymerized denture bases [20,21,22,23]. However, these studies had limited denture liner material tested and tested with individual experimental setting.
The purposes of this study were that: (1) to evaluate the tensile bond strength of autopolymerized, heat-polymerized, milled, and 3D printed denture base materials bonded to 2 acrylic-based and 2 silicone-based denture liners, both before and after thermocycling, and (2) to evaluate the impact of thermocycling on the resulting tensile bond strength. The null hypotheses were that: (1) there would be no significant difference in tensile bond strength between different denture bases bonded to various denture liner materials, and (2) there would be no significant difference in the tensile bond strength for each experimental group (denture base + denture liner group) before and after thermocycling.
Materials and methods
Four types of denture base materials were used in this study: PL - Palapress (Haraeus Kulzer, Hanau, Germany); VR - Vertex Rapid Simplified (Vertex-Dental B.V, Soesterberg, Netherlands); SC - Smile CAM total prosthesis (Pressing Dental, San Marino); ND - NextDent denture 3D+ (NextDent, Soesterberg, Netherlands). Tested denture liner materials in the present study consists of 4 groups, with 2 acrylic-based groups: GC - GC Soft-liner (GC Corp., Tokyo, Japan); RB - Tokuyama Rebase II (Tokuyama Dental Corp., Tokyo, Japan) and 2 silicone-based groups: UP - Ufi Gel P (VOCO, Cuxhaven, Germany); ST - Sofreliner Tough M (Tokuyama Dental Corp., Tokyo, Japan). All materials details are listed in Table 1.
Specimen preparation
For each denture liner group, 128 denture base specimens in a size of 25 × 25 × 3-mm and 20 × 20 × 3-mm were prepared according to International Organization for Standardization (ISO) 10139-2:2016. The specimen preparation in each group were described as follows;
-
The PL specimens were fabricated from the resin polymer mixture at a powder-liquid monomer ratio equal to 10:7 in silicone molds. Polymerization was completed in the pressure curing unit at 55 °C under 2 bar for 20 min.
-
The VR specimens were fabricated from the resin polymer mixture at a powder- liquid monomer equal to 2.3 :1 in dental flasks. Polymerization was completed in the water bath at 100 °C for 20 min.
-
The SC specimens, in a size of 25 × 25 × 25-mm and 20 × 20 × 25-mm, were milled using a 5-axis dental milling machine (S2 Milling machine; VHF, Ammerbuch, Germany) and subsequently cut into 3-mm thickness using a low-speed cutting machine (Isomet Low Speed Saw; Buehler, Illinois, USA).
-
The ND specimens were designed using a CAD software program (Solidworks 3D CAD software; Dassault Systèmes, Vélizy-Villacoublay, France), printed using a digital light processing printer (Nextdent 5100; 3DSystems, South Carolina, USA), pre-cleaned for 3 min in isopropyl alcohol using an ultrasonic bath to remove any uncured resin, and left for 10 min to ensure that they were free of residual alcohol. Post-polymerization was performed for 30 min using a post-curing unit (NextDent LC-3DPrint Box; 3DSystems, South Carolina, USA).
All specimens were wet ground using a polishing machine (Minitech 233; Presi, Eybens, France) with P500 silicon carbide abrasive paper, ultrasonically cleaned in deionized water for 10 min, and stored in deionized water at 37 °C for 7 days.
Before applying the denture liners, the surface of each specimen was treated according to the manufacturer’s instructions. A plastic collar (internal diameter 10 mm and height 3 mm) was then placed at the center of the 25 × 25 × 3-mm denture base specimen. Each denture liner material was prepared according to the manufacturer’s instructions and loaded into the hole of the plastic collar. Another 20 × 20 × 3-mm denture base specimen was then placed on top of the plastic collar, followed by a 2-kg weight. After complete setting of denture liner materials, all specimens were stored in deionized water at 37 °C for 24 h and then divided into 2 groups: non-thermocycling (NT) and thermocycling (T). An a priori sample size calculation was conducted by using a software program (G*Power v3.1.9.2; Heinrich Heine University Düsseldorf, Düsseldorf, Germany; α = 0.05; power = 80%). According to the data in a previous study [21], an effect size of 1.57 was identified and used to determine the total sample size of the study. The sample size for each group were equal to 8 (n = 8). For the NT group, specimens were tested immediately after 24 h of water immersion. For the T group, specimens were subjected to 5000 cycles of thermocycling in a water bath, alternating temperatures between 5 °C and 55 °C, with a dwell time of 30 s, and immediately tested.
Tensile bond strength test
A diagram of the tensile bond strength testing apparatus is presented in Fig. 1. The tensile bond strength test was conducted using a universal testing machine (EZ-S; Shimadzu, Kyoto, Japan) at a crosshead speed of 10 mm/min. The maximum force needed to debond the specimens was recorded. The tensile bond strength values (MPa) were calculated as the maximum load (N) divided by the cross-sectional area of the interface (mm2).
Mode of failure
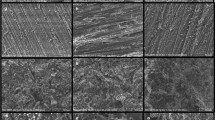
The type of failure was observed using a stereomicroscope (SZ 61, Olympus, Tokyo, Japan) with a magnification of 6.7× and classified into 3 types: type 1 adhesive, type 2 cohesive, and type 3 mixed failure.
Statistical analysis
The tensile bond strength data were statistically analyzed by using SPSS version 28.0 (IBM, USA). Normal distribution of data was evaluated with the Shapiro-Wilk test. Two-way ANOVA was used to analyze the interaction between the 2 main factors (denture liner and denture base material), followed by the Tukey HSD tests for multiple comparisons (α = 0.05). Additionally, the tensile bond strengths between the NT and T groups in each experimental group (denture base + denture liner) were separately compared using the independent samples t test.
Results
Two-way ANOVA results are presented in Table 2.
The results of the NT group showed significant interactions between denture base and denture liner material (P < 0.05). In contrast, the result of the T group showed no significant interactions between denture base and denture liner materials (P > 0.05). However, there were statistically significant differences in tensile bond strength in 2 main effects (P < 0.05). Descriptive and statistical results of tensile bond strength for the NT and the T groups are presented in Tables 3 and 4.
For the NT group, within the same denture liner material, no significant differences were found between denture base materials, except the ND + RB group which showed significantly lower tensile bond strength than the other denture base material groups (P < 0.05). Within the same denture base material, the ST group exhibited the highest tensile bond strength, in contrast, the GC group showed the lowest tensile bond strength significantly (P < 0.05).
For the T group, within the same denture liner material, the PL group showed the highest tensile bond strength, followed by the VR and SC groups. The ND group showed the lowest tensile bond strength significantly (P < 0.05). Within the same denture base material, the ST group exhibited the highest tensile bond strength significantly (P < 0.05). In contrast, the GC group showed the lowest tensile bond strength significantly (P < 0.05).
Figure 2 demonstrates the tensile bond strength compared between the T and NT groups. There were no statistically significant differences in the tensile bond strength between the T and NT groups in all experimental groups except all denture base materials bonded to the ST group, which exhibited significantly higher tensile bond strength after thermocycling. In contrast, the SC + UP and ND + UP groups exhibited significantly lower tensile bond strength after thermocycling (P < 0.05).
The mode of failure analysis is presented in Figs. 3 and 4. An adhesive failure was observed in all experimental groups (Fig. 4A) except the PL + GC, VR + GC, and SC + GC groups, which presented a cohesive failure (Fig. 4C). Mixed failure was found mostly in the denture base specimens bonded to the ST group (Fig. 4B).
Discussion
The strength and stability of the bond between the denture base and denture liner are crucial for the long-term success of complete dentures, as any bond failure may promote bacterial growth, plaque formation, and calculus accumulation. The present study aimed to compare the tensile bond strength of acrylic-based and silicone-based denture liner materials when applied to digitally-fabricated denture base materials compared with conventional autopolymerized and heat-polymerized denture base materials. The result demonstrated that there were statistically significant differences in the tensile bond strength among different denture bases bonded to various denture liner materials (P < 0.05). Therefore, the first null hypothesis was rejected. Moreover, there were statistically significant differences in tensile bond strength for each experimental group (denture base + denture liner) before and after thermocycling (P < 0.05), leading to the rejection of the second null hypothesis.
For the NT groups, the printed denture base material had the lowest mean tensile bond strength in 3 of 4 denture liner materials tested (GC, RB, and ST) compared with other denture base materials. While, for the T groups, the printed denture base material also showed significantly lower tensile bond strength with all denture liner materials tested compared with other denture base materials (P < 0.05). Our results are consistent with previous studies [20,21,22], which reported the lowest tensile bond strength values in printed denture base materials when bonded to both acrylic-based and silicone-based denture liners. This might be explained by the extent of solubility and swelling of the PMMA material, depending on its cross-linking degree [24]. As a result, the crosslinked resin in the printed denture bases (ND) which are less soluble compared with the linearly bonded PMMA in conventional and milled denture bases (PL, VR, and SC), resulting in lower tensile bond strength [21].
Comparing acrylic-based denture liner groups, the tensile bond strength in the GC group was significantly lower than that in the RB group. The difference in bond strength may be attributed to the use of a primer in the RB group, which contains acetone and ethyl acetate, to swell and penetrate the PMMA material, forming an improved interpenetrating network. Additionally, based on Kawano’s criteria as used in several studies [20, 22, 25, 26], minimum bond strength of 0.44 MPa is considered clinically acceptable for denture lining materials [27]. Even though the VR + GC, SC + GC, and ND + GC groups did not meet this standard, The GC Soft-Liner, a plasticized methacrylate polymer, has similar chemical structure to the PMMA denture bases, allowing for chemical bonding without additional agents [21]. Mode of failure for the GC group bonded to the PL, VR, and SC groups showed a 100% cohesive failure (Fig. 4C), indicating a stronger bond between the denture base material and GC Soft-Liner than the bond of the GC Soft-Liner itself [13]. In contrast, the GC + ND specimens exhibited an adhesive failure (Fig. 4A), similar to the previous findings [28], suggesting a weaker bond due to less chemical bonding between GC Soft-Liner and the printed denture base. Since the printed denture base is not pure PMMA but includes various additives, it can be concluded that there was less chemical bonding, resulting in predominantly adhesive failure [28].
The UP group displayed significantly lower tensile bond strength compared with the ST group, despite both are silicone-based denture liners. The difference in bond strength can be attributed to the mixing process. The UP material is mixed by hand, leading to the formation of air bubbles, reducing the contact area between the materials and weakening the bond. On the other hand, the ST material is mixed using mixing tips, ensuring no visible air bubbles inside the material. Additionally, careful application of the ST material on the denture base material prevented air bubbles from forming on the contact surface between the 2 materials, potentially contributing to its stronger bond [28, 29].
As a silicone-based resilient denture liner does not have chemical adhesion to PMMA, the use of an adhesive is necessary [30]. Therefore, their bonding mechanism seems to rely on treating the surface layer with a primer and partially impregnating it with a polymer solution, rather than forming a direct chemical bond between the denture base and denture liner. The tensile bond strength values between different denture base materials and the UP group did not show any statistically significant differences, consistent with the findings of Wemken et al. [21]. The adhesive primer of the Ufi Gel P contains a solvent, 2-butanone. When the adhesive is applied, the solvent causes the swelling of upper layers of the denture base. The adhesive also contains a special silane which consists of a reactive polymer with carbon chains and a reactive silicone component that has Si-H and vinyl groups. After the solvent evaporates, the carbon chains create a mechanical bond with the denture base, and the siliceous part of the primer polymer chemically bonds with the Si-H and vinyl groups of polysiloxane in the denture liner. As a result, bonding occurs through the intermediate adhesive rather than direct chemical bonding between the denture liner and the denture base material itself. Therefore, minor differences in the composition of the denture base materials are considered insignificant. Using the adhesive containing coupling agents has been reported to be successful in improving adhesion to digitally-fabricated denture bases [22].
Regardless of the thermocycling procedure, the ST group demonstrated the highest tensile bond strength when bonded to all tested denture base groups. The adhesive bonding agent in the Sofreliner Tough M contains PMMA and polyorganosilane in ethyl acetate solution. The presence of polymethyl methacrylate enhances bonding to the denture base material by strengthening the connection between the methacrylate groups in the adhesive and the pendant methacrylate groups of the PMMA resin on the bonding surface. In combination with polyorganosilane, the methacrylate groups of the silane serve as a cross-linker, aiding the bond between the denture liner and the denture base resin surface [13]. This may elucidate the high bond strength observed in the ST group with PMMA denture base resin across all groups. In the NT group, the ST group displayed higher tensile bond strength to the PL and VR group than the SC and ND group, possibly due to varying quantities of pendant methacrylate groups present on the surface of the denture materials.
The effects of 5000-cycle thermocycling on the bond strength of denture liners bonded to denture bases were also examined in this study, which were correlated with a simulated intraoral exposure equivalent to 6 months of use [17]. Thermocycling causes continuous expansion and contraction of both the denture liner and denture base material, resulting in stress accumulation at the bonded interface and thermal volumetric alterations [31]. Moreover, thermocyclic stress on acrylic-based denture liners results in water absorption and leaching out of plasticizers, leading to rapid hardening of the material [19, 31]. The result of the present study showed that thermocycling had no effect on the bonding of the acrylic-based denture liner (GC and RB); in contrast, it affected the bond of the silicone-based denture liner (UP and ST). The tensile bond strength in the UP group decreased after thermocycling, especially when bonded to in the digitally-fabricated denture base materials (SC and ND), similar to a previous study [19]. This result could be due to the impact of hydrolysis and differences in swelling behavior between the denture base and the denture liner material, which creates stress on the bonding surface [21]. This result contradicted with previous studies [25, 30], that reported no significant difference after thermocycling for Ufi Gel denture liner. However, the previous studies conducted less thermal cycle compared with the present study, making a direct comparison challenging due to differing protocols. A silicone-based denture liner does not contain a plasticizer; however, it does contain filler. Water absorption by the filler could lead to increased softness when stored in water, resulting in more elasticity, lower bond strength, and prone to a cohesive failure [19]. However, direct comparisons with these studies are challenging due to differences in the denture liners, denture base materials, and number of thermocycling applied. Interestingly, the ST group showed an increased bond strength with all tested denture base materials after thermocycling. This result might be explained by ongoing polymerization processes within the denture liner material. The authors are unaware of previous studies that have investigated the effect of thermocycling on the tensile bond strength of Sofreliner Tough M and the denture base, preventing direct result comparisons.
The limitations of this study include the use of tensile test set up for bond strength measurement regarding ISO 10139-2:2016, making direct comparisons challenging due to different testing methods compared with other studies. Future studies should compare printed denture bases from various brands to ensure consistent results. Additionally, conducting long-term studies in real oral environments would provide valuable insights into the practical durability and performance of denture liners over extended periods.
Conclusion
Based on the findings of this in vitro study, the following conclusions were drawn:
-
1)
Regardless of the tested denture base, Sofreliner Tough M exhibited the highest bond strength and mostly presented adhesive failure. In contrast, GC Soft-Liner exhibited the lowest bond strength and presented cohesive failure.
-
2)
Milled denture bases can be relined with either acrylic-based or silicone-based denture liner, similar to autopolymerized and heat-polymerized denture bases, however, cautions should be exercised when relining 3D printed denture base.
-
3)
Thermocycling did not affect the bond strength between acrylic-based denture liner and denture base material. In contrast, it affected the bond strength between silicone-based denture liner and denture base material.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- TBS:
-
tensile bond strength
- PL:
-
Palapress
- VR:
-
Vertex Rapid Simplified
- SC:
-
Smile CAM total prosthesis
- ND:
-
NextDent denture 3D+
- GC:
-
GC Soft-Liner
- RB:
-
Tokuyama Rebase II
- UP:
-
Ufi Gel P
- ST:
-
Sofreliner Tough M
- PMMA:
-
Polymethyl methacrylate
- CAD-CAM:
-
Computer-aided design-computer-aided manufacturing
- ISO:
-
International organization for standardization
- NT:
-
Non-thermocycling
- T:
-
Thermocycling
References
Zafar MS. Prosthodontic applications of Polymethyl Methacrylate (PMMA): an update. Polym (Basel). 2020;12:2299.
Gautam R, Singh RD, Sharma VP, Siddhartha R, Chand P, Kumar R. Biocompatibility of polymethylmethacrylate resins used in dentistry. J Biomed Mater Res B Appl Biomater. 2012;100:1444–50.
Hada T, Kanazawa M, Iwaki M, Katheng A, Minakuchi S. Comparison of Mechanical properties of PMMA disks for digitally designed dentures. Polym (Basel). 2021;13:1745.
Miyazaki T, Hotta Y, Kunii J, Kuriyama S, Tamaki Y. A review of dental CAD/CAM: current status and future perspectives from 20 years of experience. Dent Mater J., Goodacre CJ, Garbacea A, Naylor WP, Daher T, Marchack CB, Lowry J. CAD/CAM fabricated complete dentures: concepts and clinical methods of obtaining required morphological data. J Prosthet Dent. 2012;107:34–46.
Van Noort R. The future of dental devices is digital. Dent Mater. 2012;28:3–12.
Takeda Y, Lau J, Nouh H, Hirayama H. A 3D printing replication technique for fabricating digital dentures. J Prosthet Dent. 2020;124:251–6.
Sulaiman TA. Materials in digital dentistry-A review. J Esthet Restor Dent. 2020;32:171–81.
Dimitrova M, Corsalini M, Kazakova R, Vlahova A, Chuchulska B, Barile G, et al. Comparison between conventional PMMA and 3D printed resins for denture bases: a narrative review. J Compos Sci. 2022;6:87.
Altarazi A, Haider J, Alhotan A, Silikas N, Devlin H. Assessing the physical and mechanical properties of 3D printed acrylic material for denture base application. Dent Mater. 2022;38:1841–54.
Altarazi A, Haider J, Alhotan A, Silikas N, Devlin H. 3D printed denture base material: the effect of incorporating TiO2 nanoparticles and artificial ageing on the physical and mechanical properties. Dent Mater. 2023;39:1122–36.
Atwood DA. Bone loss of edentulous alveolar ridges. J Periodontol. 1979;50:11–21.
Boucher CO. Complete denture prosthodontics—the state of the art. J Prosthet Dent. 1975;34:372–83.
Mutluay MM, Ruyter IE. Evaluation of bond strength of soft relining materials to denture base polymers. Dent Mater. 2007;23:1373–81.
Alqutaibi AY, Alnazzawi AA, Farghal AE, Bakr RM, Mahmoud II. Impact of Acrylic and silicone-based soft-liner materials on biting Force and Quality of Life of the complete denture wearers: a Randomized Clinical Trial. J Clin Med. 2023;12:2073.
Schlenz MA, Schmidt A, Wöstmann B, Rehmann P. Clinical performance of computer- engineered complete dentures: a retrospective pilot study. Quintessence Int. 2019;50:706–11.
Dorner S, Zeman F, Koller M, Lang R, Handel G, Behr M. Clinical performance of complete dentures: a retrospective study. Int J Prosthodont. 2010;23:410–7.
Gale MS, Darvell BW. Thermal cycling procedures for laboratory testing of dental restorations. J Dent. 1999;27:89–99.
Tugut F, Coskun ME, Dogan DO, Kirmali O, Akin H. Tensile Bond Strength between Soft liners and two chemically different denture base materials: Effect of Thermocycling. J Prosthodont. 2016;25:319–23.
Kulak-Ozkan Y, Sertgoz A, Gedik H. Effect of thermocycling on tensile bond strength of six silicone-based, resilient denture liners. J Prosthet Dent. 2003;89:303–10.
Awad AN, Cho SH, Kesterke MJ, Chen JH. Comparison of tensile bond strength of denture reline materials on denture bases fabricated with CAD-CAM technology. J Prosthet Dent. 2023;129:616–22.
Wemken G, Burkhardt F, Spies BC, Kleinvogel L, Adali U, Sterzenbach G, et al. Bond strength of conventional, subtractive, and additive manufactured denture bases to soft and hard relining materials. Dent Mater. 2021;37:928–38.
Azpiazu-Flores FX, Schricker SR, Seghi RR, Johnston WM. Leyva Del Rio D. Adhesive strength of 3 long-term resilient liners to CAD-CAM denture base polymers and heat- polymerized polymethyl methacrylate with thermocycling. J Prosthet Dent. 2022. In press.
Alfaraj A, Chu TG, Alouthah H, Yang CC, Lin WS. Tensile bond strength of auto-polymerizing and heat-polymerizing denture reliners on the conventional and CAD-CAM denture base materials. J Prosthodont. 2023;32:87–95.
Rached RN, Del-Bel Cury AA. Heat-cured acrylic resin repaired with microwave-cured one: bond strength and surface texture. J Oral Rehabil. 2001;28:370–5.
Choi JE, Ng TE, Leong CKY, Kim H, Li P, Waddell JN. Adhesive evaluation of three types of resilient denture liners bonded to heat-polymerized, autopolymerized, or CAD-CAM acrylic resin denture bases. J Prosthet Dent. 2018;120:699–705.
Al Taweel S, Al-Otaibi H, Labban N, Alfouzan A, Al-Shehri H. Soft denture liner adhesion to conventional and CAD/CAM processed poly(Methyl Methacrylate) Acrylic Denture Resins-An In-Vitro Study. Mater (Basel). 2021;14:6614.
Kawano F, Dootz ER, Koran A 3rd, Craig RG. Comparison of bond strength of six soft denture liners to denture base resin. J Prosthet Dent. 1992;68:368–71.
Vuksic J, Pilipovic A, Poklepovic Pericic T, Kranjcic J. Tensile Bond Strength between different denture base materials and soft denture liners. Mater (Basel). 2023;16:4615.
Kim BJ, Yang HS, Chun MG, Park YJ. Shore hardness and tensile bond strength of long- term soft denture lining materials. J Prosthet Dent. 2014;112:1289–97.
Botega DM, Sanchez JL, Mesquita MF, Henriques GE, Consani RL. Effects of thermocycling on the tensile bond strength of three permanent soft denture liners. J Prosthodont. 2008;17:550–4.
Minami H, Suzuki S, Ohashi H, Kurashige H, Tanaka T. Effect of surface treatment on the bonding of an autopolymerizing soft denture liner to a denture base resin. Int J Prosthodont. 2004;17:297–301.
Acknowledgements
Not applicable.
Funding
This research received no external funding.
Author information
Authors and Affiliations
Contributions
Conceptualization, PJ, KK, and MA; methodology, PJ, KK, and WH; formal analysis, PJ, KK, and MA; investigation, MA, KK, and WH; data curation, PJ, KK, WH, and MA; writing original draft preparation, and writing-review and editing, PJ and KK. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable. This study did not include any human/human sample/data.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Janyaprasert, P., Kamonkhantikul, K., Homsiang, W. et al. Effect of thermocycling on tensile bond strength of autopolymerized, heat-polymerized, milled, and 3D printed denture base materials bonded to 4 different denture liners: an in vitro study. BMC Oral Health 24, 1000 (2024). https://doi.org/10.1186/s12903-024-04776-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12903-024-04776-8