Abstract
Background
This single-blind randomized controlled trial was aimed to evaluate the microbiological and clinical effects of Zeger therapy on gingival health.
Methods
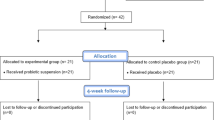
Twenty-four adults with gingivitis were recruited and monitored micro-biologically and clinically at baseline (Day 0), 4 weeks (Day 29) after therapy. All volunteers received one-stage full-mouth supragingival scaling as basic oral health care for baseline, and then randomly divided into experimental (koumiss, n = 12) or control (none, n = 12) group. The koumiss was used once a day for 4 weeks.
Results
The microbial diversity of the experimental group increased significantly after drinking koumiss (p < 0.05), mainly owing to increasing of Gram-positive bacteria (p = 0.038) and oral health-related microbes (Rothia, Corynebacterium, Actinomyces, Saccharibacteria_TM7, etc.), decreasing of Gram-negative bacteria (p = 0.009) and periodontal disease-related microbes (Porphyromonas, Fusobacterium, Veillonella, etc.), while the microbial diversity of the control group had no significant change (p > 0.05). However, there was no significant difference between the two groups in the clinical parameters (p > 0.05).
Conclusions
Zeger therapy promotes the diversity of supragingival microbiome in adults with gingivitis and increases the abundance of some beneficial flora while decreasing some harmful without clinical parameters marked changing, which holds promise for improving of gingivitis and may be a valuable oral health care approach in the future.
Trial registration
The clinical trial was approved by the Medical Ethics Committee of West China Hospital of Stomatology, Sichuan University, batch No. WCHSIRB-D-2021-428. Before patient registration began, the prospective clinical trial was registered in www.clinicaltrials.gov public repository in China under the registration number ChiCTR2200060555 on 04/06/2022.
Similar content being viewed by others
Introduction
Zeger therapy, entailing the consumption of koumiss, also known as kymyz or qymyz, a probiotic-rich beverage fermented from mare’s milk, holds significance in traditional Asian steppe diets and features prominently in ethnomedicine. Initially localized to specific regions, the widespread adoption of koumiss ensued later, driven by its manifold benefits, including low cholesterol levels and a high content of polyunsaturated fatty acids. Consequently, koumiss has garnered increased attention, particularly in Europe, notably in countries like France and Germany [1]. Mare’s milk, the primary ingredient in koumiss, bears a striking resemblance to human milk in terms of protein composition, sugar content, and salt levels [2]. The substantial sugar content in mare’s milk undergoes fermentation by microorganisms, yielding lactic acid, alcohol, and various functional molecules, such as p-pyruvate, 20-HETE, 4-aminobutanoate, uracil, acetoacetate, and γ-linolenic acid, imparting a distinctive flavor, texture, and acidity to the beverage [1, 3]. Leveraging the unique attributes of koumiss, Zeger therapy manifests several advantageous effects, predominantly in three key domains. Firstly, it plays a pivotal role in regulating microbial community homeostasis by inhibiting potentially harmful genera like Pseudomonas and Acinetobacter [4], countering pathogenic Escherchia coli. and Staphylococcus aureus [5]. Secondly, its anti-inflammatory and immunomodulatory effects are evident in studies demonstrating enhanced intestinal immunity, reversal of thymus and spleen atrophy in immunosuppressed model rats, and an increase in leukocyte and lymphocyte counts, along with the CD4+/CD8 + ratio in peripheral blood lymphocytes [6, 7]. Thirdly, its antioxidant properties are corroborated by studies indicating cholesterol reduction, atherosclerosis prevention [5, 6, 8], and protection against liver damage by enhancing antioxidant activity [9, 10]. However, research into the clinical and microbiological effects of probiotic-related Zeger therapy in oral health remains limited.
The current state of gingival health is significantly compromised by periodontal inflammatory diseases, constituting a burgeoning public health challenge that affects up to 90% of the global population and imposes substantial burdens on both health and the economy [11,12,13]. Gingivitis typically represents the initial stage of periodontal diseases, primarily driven by an imbalance in commensal microbiota within dental biofilms. Characterized by symptoms such as gingival hyperemia, swelling, pain, and gingival bleeding, gingivitis can progress to periodontitis, ultimately culminating in tooth loss among adults, thereby detrimentally impacting quality of life [14, 15]. Currently, various scientifically validated or exploratory approaches are employed to maintain gingival health and prevent gingivitis [16]. Notably, probiotic therapy has garnered considerable attention for its significant potential and promising prospects, albeit remaining insufficiently researched. Probiotics, as defined by the Food and Agriculture Organization of the United Nations/World Health Organization, refer to “live micro-organisms which, when administered in adequate amounts, confer a health benefit on the host” [16]. Multiple systematic reviews and meta-analyses have underscored the substantial clinical benefits of probiotic supplementation for patients with gingivitis or other periodontal diseases, including improvements in plaque index (PI), gingival index (GI), probing pocket depth (PD), clinical attachment level (CAL), gingival bleeding index (GBI), and reductions in the levels of major subgingival periodontal pathogens such as Porphyromonas, Fusobacterium, and Tannerella [17,18,19,20]. However, research on the effects of probiotic-related Zeger therapy on gingival health remains sparse.
Hence, the hypothesis of this study posited that probiotic-related Zeger therapy would enhance microbiological and clinical outcomes in the treatment of gingival health. The objective of this investigation was to assess the microbiological and clinical effects of probiotic-related Zeger therapy in improving gingival health among individuals with gingivitis, employing a randomized controlled trial design.
Materials and methods
Ethics statement
The clinical trial was approved by the Medical Ethics Committee of West China Hospital of Stomatology, Sichuan University, batch No. WCHSIRB-D-2021-428. Before patient registration, the prospective clinical trial was registered in www.clinicaltrials.gov public repository in China under the registration number ChiCTR2200060555 on 04/06/2022. It was designed as a prospective, randomized, blank-controlled, single-blind clinical trial with volunteers recruited at the West China campus of Sichuan University. All the participants signed written informed consent before enrollment.
Materials preparation
The product used, Koumiss (Lot No.DJ1525240150, provided by Su Niteyouqi Baigali Creamery, Xilin Gol League, Inner Mongolia Autonomous Region, China) is a commercially available probiotic beverage made from fermented fresh mare’s milk, rich in probiotics and a variety of bioactive components. The ingredients are 100% sour mare’s milk. And it needs to be stored at 0–5℃ to ensure the activity, which is closely related to the effect it produces.
Sample size calculation
The lack of data assessing microbiologic outcomes in similar previous studies prevented accurate estimates of changes in microbiologic effects, so clinical outcome variables were used as proxies. Sample size was calculated for the secondaryoutcome variable changing in gingival index (GI) score, based on Vivekananda et al. (2010) [21]. Setting 1-β = 90% and α = 0.05, the formula n = 2*[(Zα + Zβ)σ/δ]^2 was used to calculate, with Zα = 1.96 and Zβ = 1.28. Regarding a standard deviation (σ) of 0.26 and a mean difference (δ) between the experimental and control group of 0.39, it turned out that 10 patients were needed in each group. Furthermore, 2 more people in each group wererequired for the experiment considering a 20% sample withdrawal rate. Therefore, 24 volunteers wererecruited for the experiment in total.
Inclusion criteria and exclusion criteria
Volunteers were selected based on the following inclusion criteria: [1] 18–35 years old [2], no radiographic signs of alveolar bone loss associated with periodontitis at baseline [3], gingival index (GI) > 0 at baseline [4], in good general health, and [5] more than 20 natural teeth (excluding third molars).
Exclusion criteria are as follows: [1] severe systemic and hematological diseases [2], pregnancy or breastfeeding [3], physical or mental disorders that may affect oral health behavior [4], history of dairy allergy [5], use of non-steroidal or steroidal anti-inflammatory drugs, analgesics or antibiotics in the 4 weeks prior to the study [6], ongoing orthodontic treatment (including wearing orthodontics) and other unfinished dental treatment [7] acute oral lesions.
Experimental design
7 days before the beginning of the experiment, all subjects were enrolled for a unified dental examination according to the inclusion and exclusion criteria. Those who met the criteria were given a thorough upper gingival scaling by a professional dentist to remove plaque, stains and calculus.
Day 0 recalled the subjects, rechecked the inclusion and exclusion criteria, such as taking orthopantomogram for all first to exclude patients with invasive periodontitis. And baseline measurements were taken and clinical samples were collected for those who met the criteria. Baseline measurements included gingival index (GI), plaque index (PI) and gingival bleeding index (GBI) of 16,12,24,44,32 and 36 index teeth, along with probing depth (PD) of the whole mouth. GI was measured according to the method proposed by Loe and Silness, PI was referred to modified Silness-Loe, GBI was based on the method proposed by Ainamo and Bay, and PD was defined as the distance from the gingival margin to the bottom of the gingival furrow [22]. Before GI, GBI and PD while after PI were measured, all posterior teeth supragingival plaque were collected and stored at -80℃ for subsequent high-throughput sequencing analysis. All the above measurements were carried out by three professional dentists as examiners using instruments of uniform specifications. Kappa consistency test was performed for the examiners in advance (Kappa = 0.65), and the subsequent examiners were consistent.
The subjects were randomly divided into experimental group and control group according to the random number table, with 12 subjects in each group. The experimental and control groups were denoted as E1 and C1 at baseline, and E2 and C2 at final visit, respectively. The examiners did not know the grouping of subjects, and did not participate in index recording and koumiss distribution.
Day 1-Day 28, a 2500mL package of pasteurized sealed koumiss was opened every day, divided into 12 150mL food-grade measuring cups with LIDS, and distributed to subjects in the experimental group at a uniform time and place, and they were instructed to drink koumiss as slowly as possible on the spot. Due to the unique taste of koumiss, the control group at the same time took blank treatment. During the intervention period, subjects were asked not to perform any oral procedures, maintain their oral hygiene habits, and refrain from taking antibiotics or additional probiotics.
Each weekend, the experimental group will conduct additional questionnaire survey on the adverse reactions of drinking koumiss.
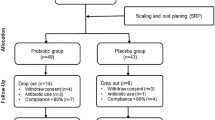
Day 29 All subjects were recalled for clinical examination consistent with baseline examination and supragingival plaque collection. The flow chart was shown in Fig. 1.
7 days before the beginning of the experiment, all subjects were enrolled for a unified dental examination according to the inclusion and exclusion criteria, and given a thorough upper gingival scaling by a professional dentist to remove plaque, stains and calculus. Day 0 recalled the subjects, rechecked the experimental admission criteria. The subjects were randomly divided into experimental group and control group with 12 subjects in each group. Day 1-Day 28, koumiss was distributed to subjects in the experimental group at a uniform time and place. Day 29 All subjects were recalled for clinical examination consistent with baseline examination and supragingival plaque collection.
Sample collection
Sterile cotton swabs were used to wipe the buccal, lingual and occludal surfaces of the upper and lower mandibular posterior teeth on both sides until all the supringival plaque observed by naked eyes were collected[8]. The cotton swabs were cut off and stored in 1.5 ml centrifuge tube with 0.5mlPBS buffer, respectively, and stored in the laboratory at -80℃ refrigerator within 2 h.
Genomic DNA extraction
The sample was thawed from − 80℃ in advance, the cotton swab tip was removed, centrifuged at 15000r/min at 4℃ for 5 min, and the supernatant was discarded. DNA was extracted from both cotton swab and precipitate by CTAB method. Total genomic DNA samples were extracted using the OMEGA Soil DNA Kit (M5635-02) (Omega Bio-Tek, Norcross, GA, USA), following the manufacturer’s instructions, and stored at -20 °C prior to further analysis. The quantity and quality of extracted DNAs were measured using a NanoDrop NC2000 spectrophotometer (Thermo Fisher Scientific, Waltham, MA, USA) and agarose gel electrophoresis, respectively [23].
Amplification of 16 S rRNA gene and sequencing
Using standard primers ACTCCTACGGGAGGCAGCA/ GGACTACHVGGGTWTCTAAT, hypervariable regions (V3-V4) of 16 S rRNA gene were amplified for each sample. In short, the sample was uniformly diluted to 20ng/ul. Amplification system (25μL) includes 5× Reaction buffer 5μL, 5×GC buffer 5μL, dNTP (2.5 mm) 2μL, Forwardprimer (10 μm) 1μL, Reverseprimer (10 μm) 1μL, DNA Template 2μL, ddH2O 8.75μL and Q5 DNA Polymerase 0.25μL. Amplification parameters were set as initial denaturation 98℃ 2 min, denaturation 98℃ 15s, rolling at 55℃ 30s, Extension 72℃ 30s, Final Extension 72℃ 5 min, 10 ℃ while held 25 to 30 cycles. The construction of the high-throughput sequencing library and sequencing tasks based on Illumina NovaseqPE250 platform were completed by Paiseno Biotechnology Co., LTD. (Shanghai, China).
Bioinformatic analysis of sequencing data
The expanded Human Oral Microbiome Database (eHOMD) was used for bioinformatic analysis. Initial screening was performed on the original off-board data of high-throughput sequencing based on sequence quality while retest the problem samples. Perform sequence denoising or OTU clustering according to QIIME2 DADA2 analysis process. According to the distribution of ASV/OTU in different samples, evaluate the α diversity level of each sample. At the ASV/OTU level, the distance matrix of each sample was calculated, and the differences in β diversity and significance among different groups were measured. At the level of taxonomic composition, we further measure the diversity of species abundance composition among different groups and try to find marker species.
Statistical analysis of clinical indicators
Data composed of oral clinical indicators, including baseline data and final data, were tested for normality and homogeneity of variance. Independent sample T test was used to statistically analyze the baseline level difference between the experimental group and the control group and the level difference between the experimental group and the control group. Paired sample T test was used to statistically analyze the level difference of the experimental group and the control group before and after the trial, respectively. Software SPSS 25.0 was used.
Collection, sequencing and statistics of the koumiss sample
Koumiss samples were collected from the unsealed sour mare’s milk within 28 days of intervention. An additional 5 ml of sour mare’s milk was collected into a sterile centrifugal tube every day and stored at 4℃. After the intervention was completed, they were fully mixed, and 10 ml was extracted from them, which were sent together with the supringival plaque samples for nucleic acid extraction and 16 S rRNA high-throughput sequencing. The specific steps were the same as above. And the dominant species were counted at phylum and genus levels.
Result
Baseline characteristics
Twenty-four eligible subjects (10 males and 14 females, aged 19 to 22 years) were enrolled from 01/09/2023 to 30/09/2023. On Day 0 (baseline), gender, age distribution, oral clinical parameters and microbial parameters were similar between the two groups (Table 1), all without significant difference (P > 0.05). None of the subjects were lost to follow-up.
Result of 16 S high-throughput sequencing
Koumiss sample
There were 92,466 sequences obtained by analyzing the sample of koumiss. The DADA2 method was used for analysis, and 56,880 sequences were obtained through sequence quality control, denoising, linking and chimera removal. The length of sequence distribution ranged from 404 bp to 432 bp, with an average of 427 bp. The ASV value was 409 in total. One kingdom, 7 phyla, 16 classes, 29 orders, 44 families, 64 genus and 58 species were identified from the sample of koumiss. Abundant probiotics beneficial to gingival health were found in koumiss. Lactobacillus accounted for the highest proportion of microorganisms in the koumiss sample, reaching 76.67%. Previous double-blind randomized placebo-controlled pilot studies have shown that oral administration of Lactobacillus reuteri-containing lozenges is clinically and microbiologically effective in the treatment of chronic periodontal diseases, including gingivitis [24, 25]. The protective effects of Lactobacillus against gingivitis are mainly related to direct inhibition of pathogens, competitive inhibition of pathogen attachment, antibacterial biofilm, and direct or indirect attenuation of immune inflammatory responses [26]. The second genus is Roseomonas, with 9.59%, and studies have shown that it has a therapeutic effect in regulating the skin microbiota and exhibits a possible anti-inflammatory effect [27, 28]. This property may be helpful in the treatment of gingivitis, but there are no studies on the oral microbiota and further research is needed. In addition, there are many other probiotics that may be beneficial for gingival health. For example, Lactococcus, which accounts for 2.12%, has shown in previous studies that its whey bioconversion products can reduce inflammation-related cytokines, increase antioxidant stress markers [29]. It can also produce nisin, which prevents oral biofilm formation and disrupts pre-formed 24- and 48-hour biofilms, reducing the level of pathogens in biofilms and promoting plaque diversity levels closer to “health” level [30]. Bifidobacterium, which accounts for 0.09%, has similar effects to Lactobacillus, an auxiliary effect on the treatment of gingivitis, significantly reducing the levels of pathogens and pro-inflammatory cytokines [31, 32].
Supragingival plaque samples
Sequence processing analysis
A total of 48 samples were analyzed, resulting in 4,345,611 sequences, with an average of 90,534 sequences per sample. The DADA2 method was used for analysis, and 2,491,993 sequences were obtained after sequence quality control, denoising, linking and chimera removal, with an average of 51,917 sequences per sample. The length of sequence distribution ranged from 48 bp to 437 bp, with an average of 423 bp. A total of 7522 ASV values were calculated, and the average ASV value of each sample was 157.
Diversity analysis
Previous studies have shown that patients with periodontal diseases (including gingivitis) have a higher diversity and biomass of microbial communities, along with an increased proportion of Gram-negative and anaerobic bacteria in the gingival microbial population [34,35,36,37]. In our findings, by α-diversity analysis (Fig. 2A) and β-diversity analysis (Fig. 2B), we obtained the results that after the intervention, the diversity of the microbial community in the experimental group increased with statistically significant differences, and there was no significant change in the control group. This is contrary to the previous research findings, but the possible reason is analyzed as follows. After the intervention, compared with the control group, the Gram-positive bacteria in the experimental group increased by relatively + 749.44% (p = 0.038), and the Gram-negative bacteria decreased by relatively − 883.88% (p = 0.009). And after the intervention, compared with the control group, the aerobic and facultative anaerobic bacteria in the experimental group increased by relatively + 164.40% (p = 0.356), and the obligate anaerobic bacteria decreased by relatively − 292.73% (p = 0.106). These indicates that in this study, the increased diversity of the experimental group was mainly derived from Gram-positive bacteria, aerobic and facultative anaerobic bacteria, while the proportion of Gram-negative bacteria and anaerobic bacteria decreased. These are healthy changes for gingival microecological stability, consistent with previous studies [34,35,36,37].
Diversity analysis. A. α-diversity index: Chao1 and Observed Species index are selected to represent richness, Shannon and Simpson index to represent diversity, and Faith’s PD index to represent evolution-based diversity. Pielou’s Evenness index was used to characterize evenness, and Good’s Coverage index was used to characterize coverage. B. Non-metric multidimensional scaling (NMDS) analysis(left), group difference analysis(right): the distance algorithm chosen was weighted_unifrac
Bacterial community analysis
Figure 3(A, B) showed the dominant bacteria (top 20) of supragingival plaque before and after intervention at the phylum and genus level by using the relative abundance structure. At the phylum level, the top 5 microorganisms with the highest abundance ratio are Bacillota, Pseudomonadota, Actinomycetota, Fusobacteriota, and Bacteroidota. Regarding Bacillota, the previous literature is controversial. S. Huang at al. and A. L. Griffen at al. observed a higher proportion of Firmicutes around the gingival tissue in healthy individuals [36, 38], and L. Abusleme at al. observed Bacillota in patients with periodontal diseases (including gingivitis) was significantly increased [34]. In this experiment, we measured a relative decrease (-252.45%) of Bacillota in the experimental group (p < 0.05) compared to the control group. On the basis of previous studies about the difference between gingival microbes in healthy people and patients with gingivitis or periodontitis, we found that after the intervention, the experimental group had a relative decrease in gingival disease-related bacteria Fusobacteriota (-64.45%, p > 0.05), and a relative increase in gingival health-related bacteria Pseudomonadota (+ 2.85%, p > 0.05) and Actinomycetota (+ 406.14%, p < 0.05). In addition, in the experimental group, some gingival disease-related microorganisms Bacteroidota, Spirochaetota, Synergistota, and Chloroflexota increased after the intervention compared with the control group [34,35,36]. But considering that the increase of these microorganisms is not large, and they are not absolute pathogenic bacteria in the progression of gingival disease, it may be normal fluctuations of oral flora changes.
At the genus level, the top 10 microorganisms with the highest abundance ratio were Neisseria, Streptococcus, Haemophilus, Veillonella, Actinomyces, Corynebacterium, Fusobacterium, Leptotrichia, Rothia, Prevotella. Observed a higher amount in healthy people than in patients with gingival disease, the bacteria relatively increased in the experimental group are Rothia (+ 49.95%, p < 0.05), Corynebacterium (+ 687.71%, p < 0.01) and Actinomyces (+ 565.17%, p < 0.05) [35]. These changes suggest that Zeger therapy can promote the development of gingival flora closer to a healthy environment. Associated with gingival disease, the bacteria relatively decreased in the experimental group are Porphyromonas (-149.26%, p > 0.05), Fusobacterium (-116.45%, p > 0.05) and Veillonella (-390.04%, p < 0.05). Among them, Porphyromonas and Fusobacterium are considered as the main pathogenic bacteria of periodontal diseases (including gingivitis) [35]. Although their statistical significances are not obvious, their obvious clinical significances call for a larger sample size and further study. In addition, it is interesting to note that although outside the top10, Saccharibacteria (TM7) was significantly relatively higher (+ 442.18%) in the experimental group (p < 0.05) compared with the control group. Previously, its role in oral health and disease was thought to be unknown [39], and it has tended to be considered as a potential pathogen of periodontal diseases. But a recent study has shown that, contrary to the suspected pathogenic role, TM7 protects the host from bacterial-induced inflammatory damage [40]. Therefore, the changes in gingival microbiome caused by Zeger therapy are beneficial for gingival health.
Figure 3C used a phylogenetic tree plot to show the position of each ASV/OTU in the evolutionary tree and the evolutionary distance between each other, and reflected their composition, abundance, taxonomy and other information through heat maps and bar charts.
Bacterial difference analysis in the experimental group before and after intervention
Based on the above analysis, it was concluded that the experimental group had significant changes in the supragingival plaque habitat before and after intervention, while the control group did not. Therefore, we further conducted species difference analysis on the experimental group and tried to find marker species.
Species difference analysis in the experimental group before and after intervention. A. Difference test boxplot (phylum, top 20). B. Venn diagram (the frequency of occurrence = 1). C. Heat map (genus, top 20). D. Difference test boxplot of Gram-positive bacteria (genus, top 20). E. Difference test boxplot of Gram-negative bacteria (genus, top 20)
Statistical differences in relative species composition at phylum(A) and genus (D, E) levels were tested before and after treatment in the experimental group using the difference test boxplot in Fig. 4.
Figure 4B shows that E1 and E2 have 13 common ASV/OTU by using Venn diagram, E1 has 17 exclusive species, and E2 has 11 accordingly.
In order to further compare the differences in species composition between the experimental groups before and after intervention, and to display the species abundance distribution trend of each sample, the heat map was used for species composition analysis in Fig. 4C. Heat maps are made using abundance data from the top 20 genera with average abundance. It was found that the abundance of Leptotrichia, Cardiobacterium, Selenomonas, Prevotella, Saccharibacteria_(TM7)_[G-1], Corynebacterium, Actinomyces, Rothia, Aggregatibacter, Capnocytophaga, Peptidiphaga and other genera increased after intervention, while Fusobacterium, Porphyromonas, Streptococcus, Haemophilus, Anaerococcus, Neisseria, Lautropia, Veillonella, Lactobacillus and other genera decreased after intervention.
Results of clinical indicators
δE and δC are based on the paired sample T test, except that the changes in PD in the control group before and after intervention were clinically significant (95% CI, -0.63 to -0.11; p < 0.01), there were no significant differences in other indexes. Based on independent sample T test, δE-δC showed no significant difference in the four clinical indicators between the two groups. However, we found that GI, PI and GBI showed a trend of increasing after intervention in both groups, while PD showed a trend of decreasing (Table 2).
Discussion
Koumiss, renowned for its extensive historical usage, harbors a plethora of advantageous constituents including abundant polyunsaturated fatty acids, small-molecule amino acids, lactose, lactic acid, and a profusion of probiotics. These beneficial components engage in interactions with the oral microenvironment, thereby inducing alterations in the composition of the oral microbiota. Such modifications hold promise for potentially enhancing the oral health of patients with gingivitis. These interactions manifest through diverse mechanisms, with some mediated by the molecular constituents of koumiss, others involving molecules possessing antibacterial properties, and yet others serving as substrates for the metabolism of beneficial microorganisms. Moreover, the probiotics present in koumiss may facilitate certain functions, thereby modulating the microenvironment of the oral microbiota. Recent research has revealed that TM7, utilizing the arginine deiminase system (ADS), metabolizes arginine to produce adenosine triphosphate (ATP), thereby conferring protection against acid stress to both TM7 and its host bacteria. Acid stress arises commonly in the human oral cavity due to bacterial carbohydrate metabolism. Within the oral cavity, TM7 engages in a symbiotic association with Actinomyces, wherein Actinomyces deficient in ADS may benefit from enhanced survival conditions through symbiotic interaction with TM7 [41]. Notably, koumiss is known to be abundant in small-molecule amino acids, and our investigations have demonstrated a significant elevation in the abundance of both TM7 and Actinomyces following koumiss consumption. Consequently, TM7 utilizes small-molecule arginine present in koumiss to foster a symbiotic relationship with Actinomyces, thus ameliorating the oral gingival microbial milieu and reinstating microbial homeostasis. This intriguing phenomenon warrants further investigation to validate its potential implications.
In koumiss, probiotics have the capacity to effectively colonize and proliferate within the bacterial milieu, leading to the depletion of nutrients crucial for the growth of pathogenic bacteria. Moreover, these probiotics produce antimicrobial substances, such as acetic acid and lactic acid, which exhibit inhibitory effects specifically against Gram-negative bacteria. On the host front, probiotics in koumiss can modulate host responses by down-regulating pathways associated with tissue damage, such as reversing epithelial damage induced by inflammation through the up-regulation of structural proteins. Additionally, they may up-regulate pathways that suppress pathogen growth or virulence [16]. For instance, koumiss has been shown to stimulate the secretion of the anti-inflammatory cytokine IL-10, thereby exerting anti-inflammatory and immunomodulatory effects [6, 7]. Furthermore, Lactobacillus helveticus NS8, a constituent of koumiss, significantly inhibits the activation of NF-κB, upregulates IL-10, downregulates IL-17-producing T cells, and promotes the proliferation of beneficial commensal microorganisms while inhibiting harmful microorganisms, thereby preserving microbial balance and health [42]. However, while these mechanisms have been extensively investigated in the gut, their specific effects within the oral cavity remain understudied. Therefore, further research is warranted to elucidate the intricate mechanisms underlying the therapeutic efficacy of koumiss for promoting gingival health.
High diversity in the oral microbiome is often indicative of a dysbiotic community. Interestingly, our findings reveal that while koumiss treatment has the potential to improve gingival health, it also increases oral microbiome diversity. According to Abusleme et al.‘s study on the gingival microbiome in healthy individuals, gingivitis patients, and periodontitis patients, oral microbial diversity is higher in gingivitis patients compared to healthy individuals, but lower in periodontitis patients than in gingivitis patients [35]. This suggests that the diversity of the oral microbiome does not strictly correlate with the progression and severity of periodontal disease. This raises the question: although increased oral microbiome diversity can reflect ecological changes and is often viewed as an indicator of dysbiosis, could it be that, in certain cases (such as gingivitis patients), an appropriate range of increase is not necessarily detrimental and may prevent the progression of periodontal disease? This does not contradict the idea that increased diversity in the oral microbiome of healthy individuals indicates dysbiosis; it merely represents a different context. For healthy individuals, an increase in bacterial abundance is unfavorable. However, for gingivitis patients with pre-existing microbial imbalance, a moderate elevation in bacterial abundance may potentially prevent the progression to periodontitis. Our results indicate that most of the microbes contributing to the increased diversity are beneficial oral bacteria. Given that the gingival microbiome of periodontitis patients is widely dominated by pathogenic bacteria, the heightened diversity resulting from koumiss consumption may mitigate the predominance of these harmful bacterial species.
Periodontal diseases, including gingivitis, arise from an imbalance in the commensal oral microbiota, triggering the host’s immune response and resulting in inflammation and tissue damage [13, 33]. The diverse microenvironments within the oral cavity harbor unique microbial communities governed by intricate signaling pathways, as well as host and environmental factors [15]. Considering the ability of Zeger therapy to modulate gingival microbial diversity, it is conceivable that it could also confer benefits in addressing other oral microbial imbalance-related conditions, such as caries, halitosis, and oral mucosal diseases. However, this study is constrained by the limited sample size, which may compromise the certainty of our findings. Furthermore, no significant differences were observed in our clinical parameters before and after the intervention in either the experimental or control groups, except for periodontal probing depth (PD) in the control group (p < 0.01). This discrepancy may be attributed to the mild gingival inflammation exhibited by our target population of gingivitis patients, which may not manifest significant changes in clinical parameters over the short-term duration of 1–28 days. Although we utilized 16 S high-throughput sequencing of the microbiota to enhance sensitivity and accuracy, enabling the detection of rapid changes in oral microbiota associated with gingival health, further investigation is warranted to elucidate the long-term effects of koumiss consumption on gingival health over an extended period, such as several years.
Conclusion
Zeger therapy increasing microbial diversity, mainly attributable to increasing proportion of Gram-positive bacteria and decreasing of Gram-negative bacteria, thought to be beneficial for gingival health while improved no significant change in clinical parameters. It also promotes gingival health-related microbes increasing (Rothia, Corynebacterium, Actinomyces, Saccharibacteria_TM7, etc.) and gingival disease-related microbes decreasing (Porphyromonas, Fusobacterium, Veillonella, etc.).
Data availability
The datasets generated and/or analysed during the current study are available in the BioProject database (ID: PRJNA1145633), http://www.ncbi.nlm.nih.gov/bioproject/1145633.
References
Rakhmanova A, Wang T, Xing G, Ma L, Hong Y, Lu Y, et al. Isolation and identification of microorganisms in Kazakhstan Koumiss and their application in preparing cow-milk koumiss. J Dairy Sci. 2021;104(1):151–66.
Malacarne M, Martuzzi F, Summer A, Mariani P. Protein and fat composition of mare’s milk: some nutritional remarks with reference to human and cow’s milk. Int Dairy J. 2002;12(11):869–77.
Xia Y, Yu J, Miao W, Shuang Q. A UPLC-Q-TOF-MS-based metabolomics approach for the evaluation of fermented mare’s milk to koumiss. Food Chem. 2020;320:126619.
Kwok LY, Wang L, Zhang J, Guo Z, Zhang H. A pilot study on the effect of Lactobacillus casei Zhang on intestinal microbiota parameters in Chinese subjects of different age. Benef Microbes. 2014;5(3):295–304.
Pan DD, Zeng XQ, Yan YT. Characterisation of Lactobacillus fermentum SM-7 isolated from koumiss, a potential probiotic bacterium with cholesterol-lowering effects. J Sci Food Agric. 2011;91(3):512–8.
Li Q, Zhang C, Xilin T, Ji M, Meng X, Zhao Y, et al. Effects of Koumiss on intestinal immune modulation in immunosuppressed rats. Front Nutr. 2022;9:765499.
Rong J, Zheng H, Liu M, Hu X, Wang T, Zhang X, et al. Probiotic and anti-inflammatory attributes of an isolate Lactobacillus helveticus NS8 from Mongolian fermented koumiss. BMC Microbiol. 2015;15:196.
Wang J, Zhang H, Chen X, Chen Y, Menghebilige, Bao Q. Selection of potential probiotic lactobacilli for cholesterol-lowering properties and their effect on cholesterol metabolism in rats fed a high-lipid diet. J Dairy Sci. 2012;95(4):1645–54.
Wang Y, Li Y, Xie J, Zhang Y, Wang J, Sun X, et al. Protective effects of probiotic Lactobacillus casei Zhang against endotoxin- and d-galactosamine-induced liver injury in rats via anti-oxidative and anti-inflammatory capacities. Int Immunopharmacol. 2013;15(1):30–7.
Zhao ZW, Pan DD, Wu Z, Sun YY, Guo YX, Zeng XQ. Antialcoholic liver activity of whey fermented by Lactobacillus casei isolated from koumiss. J Dairy Sci. 2014;97(7):4062–71.
Chen MX, Zhong YJ, Dong QQ, Wong HM, Wen YF. Global, regional, and national burden of severe periodontitis, 1990–2019: an analysis of the global burden of disease study 2019. J Clin Periodontol. 2021;48(9):1165–88.
Eke PI, Dye BA, Wei L, Slade GD, Thornton-Evans GO, Borgnakke WS, et al. Update on prevalence of periodontitis in adults in the United States: NHANES 2009 to 2012. J Periodontol. 2015;86(5):611–22.
Kinane DF, Stathopoulou PG, Papapanou PN. Periodontal diseases. Nat Reviews Disease Primers. 2017;3:17038.
Curtis MA, Diaz PI, Van Dyke TE. The role of the microbiota in periodontal disease. Periodontol 2000. 2020;83(1):14–25.
Lamont RJ, Koo H, Hajishengallis G. The oral microbiota: dynamic communities and host interactions. Nat Rev Microbiol. 2018;16(12):745–59.
Scannapieco FA, Gershovich E. The prevention of periodontal disease—an overview. Periodontol 2000. 2020;84(1):9–13.
Bustamante M, Oomah BD, Mosi-Roa Y, Rubilar M, Burgos-Díaz C. Probiotics as an adjunct therapy for the treatment of halitosis, dental caries and periodontitis. Probiotics Antimicrob Proteins. 2020;12(2):325–34.
Gheisary Z, Mahmood R, Harri Shivanantham A, Liu J, Lieffers JRL, Papagerakis P, et al. The clinical, microbiological, and immunological effects of probiotic supplementation on prevention and treatment of periodontal diseases: a systematic review and meta-analysis. Nutrients. 2022;14(5):1036.
Gruner D, Paris S, Schwendicke F. Probiotics for managing caries and periodontitis: systematic review and meta-analysis. J Dent. 2016;48:16–25.
Matsubara VH, Bandara HM, Ishikawa KH, Mayer MP, Samaranayake LP. The role of probiotic bacteria in managing periodontal disease: a systematic review. Expert Rev Anti Infect Ther. 2016;14(7):643–55.
Vivekananda MR, Vandana KL, Bhat KG. Effect of the probiotic Lactobacilli reuteri (Prodentis) in the management of periodontal disease: a preliminary randomized clinical trial. J oral Microbiol. 2010;2.
Kuru BE, Laleman I, Yalnızoğlu T, Kuru L, Teughels W. The influence of a bifidobacterium animalis probiotic on gingival health: a randomized controlled clinical trial. J Periodontol. 2017;88(11):1115–23.
Kim CS, Cha L, Sim M, Jung S, Chun WY, Baik HW et al. Probiotic supplementation improves cognitive function and mood with changes in gut microbiota in community-dwelling older adults: a randomized, double-blind, placebo-controlled, multicenter trial. The journals of gerontology Series A, Biological sciences and medical sciences. 2021;76(1):32–40.
Teughels W, Durukan A, Ozcelik O, Pauwels M, Quirynen M, Haytac MC. Clinical and microbiological effects of Lactobacillus reuteri probiotics in the treatment of chronic periodontitis: a randomized placebo-controlled study. J Clin Periodontol. 2013;40(11):1025–35.
Grusovin MG, Bossini S, Calza S, Cappa V, Garzetti G, Scotti E, et al. Clinical efficacy of Lactobacillus reuteri-containing lozenges in the supportive therapy of generalized periodontitis stage III and IV, grade C: 1-year results of a double-blind randomized placebo-controlled pilot study. Clin Oral Invest. 2020;24(6):2015–24.
Wang J, Liu Y, Wang W, Ma J, Zhang M, Lu X, et al. The rationale and potential for using Lactobacillus in the management of periodontitis. J Microbiol. 2022;60(4):355–63.
Myles IA, Castillo CR, Barbian KD, Kanakabandi K, Virtaneva K, Fitzmeyer E et al. Therapeutic responses to Roseomonas mucosa in atopic dermatitis may involve lipid-mediated TNF-related epithelial repair. Sci Transl Med. 2020;12(560).
Myles IA, Earland NJ, Anderson ED, Moore IN, Kieh MD, Williams KW et al. First-in-human topical microbiome transplantation with Roseomonas mucosa for atopic dermatitis. JCI Insight. 2018;3(9).
Park E, Ha J, Lim S, Kim G, Yoon Y. Development of postbiotics by whey bioconversion with Enterococcus faecalis M157 KACC81148BP and Lactococcus lactis CAU2013 KACC81152BP for treating periodontal disease and improving gut health. J Dairy Sci. 2021;104(12):12321–31.
Radaic A, Ye C, Parks B, Gao L, Kuraji R, Malone E, et al. Modulation of pathogenic oral biofilms towards health with nisin probiotic. J oral Microbiol. 2020;12(1):1809302.
Invernici MM, Salvador SL, Silva PHF, Soares MSM, Casarin R, Palioto DB, et al. Effects of Bifidobacterium probiotic on the treatment of chronic periodontitis: a randomized clinical trial. J Clin Periodontol. 2018;45(10):1198–210.
Oliveira LF, Salvador SL, Silva PH, Furlaneto FA, Figueiredo L, Casarin R, et al. Benefits of Bifidobacterium animalis subsp. lactis probiotic in experimental periodontitis. J Periodontol. 2017;88(2):197–208.
Murakami S, Mealey BL, Mariotti A, Chapple ILC. Dental plaque-induced gingival conditions. J Periodontol. 2018;89(Suppl 1):S17–27.
Abusleme L, Dupuy AK, Dutzan N, Silva N, Burleson JA, Strausbaugh LD, et al. The subgingival microbiome in health and periodontitis and its relationship with community biomass and inflammation. ISME J. 2013;7(5):1016–25.
Abusleme L, Hoare A, Hong BY, Diaz PI. Microbial signatures of health, gingivitis, and periodontitis. Periodontol 2000. 2021;86(1):57–78.
Griffen AL, Beall CJ, Campbell JH, Firestone ND, Kumar PS, Yang ZK, et al. Distinct and complex bacterial profiles in human periodontitis and health revealed by 16S pyrosequencing. ISME J. 2012;6(6):1176–85.
Shi B, Chang M, Martin J, Mitreva M, Lux R, Klokkevold P, et al. Dynamic changes in the subgingival microbiome and their potential for diagnosis and prognosis of periodontitis. mBio. 2015;6(1):e01926–14.
Huang S, Li R, Zeng X, He T, Zhao H, Chang A, et al. Predictive modeling of gingivitis severity and susceptibility via oral microbiota. ISME J. 2014;8(9):1768–80.
Bor B, Bedree JK, Shi W, McLean JS, He X. Saccharibacteria (TM7) in the human oral microbiome. J Dent Res. 2019;98(5):500–9.
Chipashvili O, Utter DR, Bedree JK, Ma Y, Schulte F, Mascarin G, et al. Episymbiotic Saccharibacteria suppresses gingival inflammation and bone loss in mice through host bacterial modulation. Cell Host Microbe. 2021;29(11):1649–e627.
Yu G, Phillips S, Gail MH, et al. The effect of cigarette smoking on the oral and nasal microbiota. Microbiome. 2017;5(1):3.
Rong J, Liu S, Hu C, Liu C. Single probiotic supplement suppresses colitis-associated colorectal tumorigenesis by modulating inflammatory development and microbial homeostasis. J Gastroenterol Hepatol. 2019;34(7):1182–92.
Acknowledgements
The authors would like to acknowledge the assistance of Shihai Yin, the Dentist of the Shihai Dental Clinic and retired professor of the West China Hospital of Stomatology, along with all the dentists and volunteers who agreed to participate in this study for their assistance with data collection. The authors would also like to acknowledge the assistance of Lei Lei, associate professor of the Department of Preventive Dentistry, West China Hospital of Stomatology, Sichuan University, for her valuable suggestions for our thesis.
Funding
This research was funded by Science and Technology Project of Sichuan Province, China, No.2021YJ0229.
Author information
Authors and Affiliations
Contributions
Conceptualization, methodology, project administration, investigation, validation, formal analysis, data curation, resources and writing—original draft preparation, XC and YZ; investigation, validation, resources and visualization, KX and ML; supervision, funding acquisition, project administration, writing—review and editing, WY; All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the volunteers to publish this paper. The clinical trial was approved by the Medical Ethics Committee of West China Hospital of Stomatology, Sichuan University, batch No. WCHSIRB-D-2021-428. Before patient registration began, the prospective clinical trial was registered in www.clinicaltrials.gov public repository in China under the registration number ChiCTR2200060555 on 04/06/2022.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Chen, X., Zhao, Y., Xue, K. et al. Microbiological and clinical effects of probiotic-related Zeger therapy on gingival health: a randomized controlled clinical trial. BMC Oral Health 24, 1086 (2024). https://doi.org/10.1186/s12903-024-04846-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12903-024-04846-x