Abstract
Background
To verify the influence of macrogeometry with healing chambers on the osseointegration of dental implants by analyzing implant stability quotient (ISQ) and evaluate the correlation between insertion torque and ISQ insertion with different macrogeometries.
Methods
In total, 26 implants were installed in the posterior mandible of eight patients with sufficient bone height for the installation of implants measuring 3.5 mm in diameter and 9.0 mm in length. The implants were categorized according to two types of macrogeometry: a test group (GT) with 13 conical implants with healing chambers and a control group (GC) with 13 conical implants with conventional threads. To insert the implants, a bone drilling protocol was used up to a diameter of 3 mm with the last helical bur. The insertion torque of the implants was evaluated, followed by the measurement of ISQ at 0 (T-0), 7 (T-7), 14 (T-14), 21 (T-21), 28 (T-28), and 42 (T-42) days.
Results
The mean insertion torque was 43 Ncm in both groups, without a significant difference. Moreover, no significant difference in the ISQ values was found between the groups at different time points (p > 0.05), except at T-7 (GT = 69.87±1.89 and GC = 66.48±4.49; p = 0.01). Although there was no significant difference, ISQ median values were higher in the GT group than GC group at 28 days (GT = 67.98 and GC = 63.46; p = 0.05) and 42 days (GT = 66.12 and GC = 60.33; p = 0.09). No correlation was found between the insertion torque and ISQ insertion (p > 0.05).
Conclusion
Furthermore, implants with a 3.5 mm diameter macrogeometry, with or without healing chambers, inserted with a drilling protocol up to 3 mm in diameter of the last helical bur, led to a similar secondary stability, with no difference in ISQ values. Although, implants with healing chamber demonstrates ascending values in the graph of ISQ, having a trend of faster osseointegration than implants without healing chambers. Both macrogeometries provide a similar primary stability to implants.
Trial registration
This study was registered retrospectively in ReBec (brazilian registry of clinical trials) under the number RBR-96n5×69, on the date of 19/06/2023.
Similar content being viewed by others
Introduction
Osseointegration is currently defined as the contact established without the interposition of non-osseous tissue between the remodeled normal bone and an implant, implying sustained transfer and load distribution from the implant to and within the bone tissue [1]. In precursor implants, the time of osseointegration in the mandible was recommended to be 3 months, and in the maxilla, 6 months [2]. Over the years, there have been constant improvements in the geometry and surface of implants as an attempt to accelerate osseointegration [3, 4].
Previous studies have shown that less bone compression in the implant insertion bed results in less tissue trauma and, consequently, less intensity of the inflammatory process [5,6,7]. Over-drilling, when the diameter of the last drill used in the bed approaches the external diameter of the threads, can also contribute to the reduction of this inflammatory process by lower compression of the implant surface on the bone, resulting in lower insertion torque [6]. Thus, studies with healing chambers, different types of threads, and drilling techniques have been developed to evaluate secondary stability and analyze different degrees of bone compression for a better osseointegration in macrogeometries with less compressive behavior [8,9,10,11].
Although few studies have prioritized over-drilling protocols for lower bone compression and acceleration of secondary stability, others have shown rapid osseointegration with conventional drilling protocols in Straumann implants (Straumann – Basel, Switzerland) [12, 13]. This company advocates a drilling protocol for most of its implants, with the last helical bur approximately 0.6 mm smaller than the diameter of the implant to be inserted, such as the use of the last 3.5 mm bur to insert a regular 4.1 mm implant. This conventional drilling protocol provides osseointegration in approximately 4 to 6 weeks, with an insertion torque ranging from 30 to 60 Ncm for the Straumann (Straumann – Basel, Switzerland) system on Standard Plus, Bone Level, and Tissue Level implants [14, 15].
Surface treatments of implants with sandblasting and acid attack increase surface roughness and implant-bone contact, improve the quality of osseointegration, and reduce bone repair time, providing attraction and adhesion of osteoblasts [16]. Implants subjected to sandblasting and acid attack have demonstrated a high survival rate (99%), promoting osseointegration within 6 weeks [13, 17, 18].
Macrogeometric, microgeometric, and surgical protocols for bone bed preparation and implant insertion interfere with osseointegration [17, 19,20,21,22]. The Due Cone implant (Implacil de Bortoli, – São Paulo, SP, Brazil) is a conical implant manufactured from commercially pure grade IV titanium, has a progressive trapezoidal thread design and surface treatment with the blasting of titanium oxide microparticles (approximately 100 μm) with subsequent etching with maleic acid [23]. Good results for implants with this macro design and surface treatment have been reported, in addition to the occurrence of osseointegration within 6 weeks of insertion [3, 18, 21]. Additionally, these implants have shown similar results to implants from other brands, such as Straumann and Nobel Biocare (Goteborg, Sweden), in animal studies, regarding the percentage of bone in contact with the implant (BIC%) after 6 weeks of healing [3, 23].
The presence of healing chambers on the surface of dental implants raises the hypothesis of acceleration of traditional implant osseointegration, aiming at shorter prosthetic rehabilitation on the implant [8, 11]. The Due Cone implant underwent modification in its macrogeometry with healing chambers to increase the implant and bone contact area, favoring the idea and concept of “less bone compression” during implant insertion. Animal studies carried out with this implant system, comparing conventional macrogeometry and macrogeometry with healing chambers, showed favorable bone accumulation in the healing chambers and reduction of implant insertion torque without loss of primary stability [8,9,10].
Osstell (Integration Diagnostics AB, Göteborg, Sweden) measures the stability of the implant during certain periods of bone repair after its insertion. It allows the assessment of the stability of implants by resonance frequency assessment (RFA), which is generated by a magnetic pulse transmitted by a portable instrument that excites the SmartPeg. Thus, the implant stability quotient (ISQ) was obtained on a scale of 1 to 100.21 This assessment is widely used to analyze the implant stability and is related to the lateral stability of the implant, which depends on the rigidity of the connection between the implant surface and bone [22, 24,25,26,27].
This study aimed to evaluate the osseointegration and primary stability of two implant macrogeometries inserted in the mandible using a conventional drilling protocol. The analysis focused on the ISQ in the initial phases of bone healing and examined insertion torque and insertion ISQ, as well as the correlation between these measures. We hypothesized that the healing chambers could accelerate the process of osseointegration under the evaluated conditions by increasing the ISQ in a 42-day time period.
Materials and methods
Study design
This randomized clinical trial analyzed the insertion of 26 implants in the posterior region of the mandible of eight patients by comparing the ISQ values of two different types of implant macrogeometry. The patient recruitment period for this study began on April 7, 2022 and ended on June 2, 2022. The surgery to insert the implants was carried out in July 2022 with a follow-up of 42 days after the implant insertion surgery. Patients were categorized according to the type of implant macrogeometry: a test group (GT; with healing chambers; Maestro, Implacil de Bortoli, São Paulo, SP, Brazil) and a control group (GC; with conventional threads; Due Cone, Implacil de Bortoli, São Paulo, SP, Brazil). This study was approved by the Ethics and Research Committee of Pontifícia Universidade Católica do Paraná (PUCPR - number 5.338.876) and was retrospectively registered in ReBec (brazilian registry of clinical trials) under the number RBR-96n5 × 69. Informed consent was obtained from all individual participants included in the study. This study was conducted in accordance with CONSORT reporting guidelines [28].
Patient selection
Patients aged over 21 years that needed implants in the mandibular posterior region were selected. Patients assisted at the dental clinic of PUCPR were pre-selected based on the evaluation of panoramic radiographs. After pre-selection, patients who met the eligibility criteria were invited to a consultation with a clinical examination and referred to the radiology sector for cone-beam computed tomography and were included in the study. The sample was collected by convenience and after a sample power test was carried out to determine the significance of the sample.
The inclusion criteria were as follows:
-
patients with partially edentulous posterior mandible requiring one implant in each half-arch or two implants in each half-arch;
-
those with a minimum bone height of 11 mm and minimum bone thickness of 5 mm in the posterior region of the bilateral mandible evaluated using cone beam computed tomography; and.
-
those with sufficient prosthetic space for subsequent prosthetic rehabilitation.
The exclusion criteria were as follows:
-
Patients who require some type of bone reconstruction or advanced surgery to allow implant installation;
-
patients who did not agree to be part of the study;
-
patients with uncontrolled diabetes, with glycated hemoglobin (HbA1c) above 7.5%; [29]
-
smokers (> 10 cigarettes/day);
-
those using oral or injectable bisphosphonates;
-
immunodeficient patients.
-
patients who underwent radiotherapy in the head and neck region for less than 5 years before the beginning of the research;
-
patients with another systemic condition that contraindicated performing oral surgery or those who had conditions that could interfere with osseointegration.
Allocation randomization and blinding
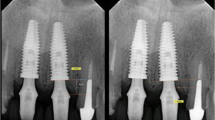
Each patient underwent surgery to install implants with healing chambers (Maestro) and conventional threads (Due Cone). All implants used were conical with a conical internal connection of size 3.5 × 9 mm. Randomization of the sites of each implant was performed by drawing lots with a sealed opaque envelope for each site of the mandible, thus creating a test group (GT) of Maestro implants and a control group (GC) of Due Cone implants. The patient and examiner who performed the clinical evaluations were blinded; however, it was not possible to blind the dentist who performed the procedure. The treatment allocation is shown in Fig. 1 and the macrogeometry of the implants used is shown in Fig. 2.
Intervention
Plans were made to perform the surgeries based on clinical evaluations and image analysis of cone-beam computed tomography scans. All biosafety procedures were adopted, and medications were prescribed before and after the surgery. One hour before the surgery, 2 g of cefadroxil was prescribed. To reduce pain and inflammation after the surgery, 100 mg of ketoprofen and 750 mg of paracetamol were prescribed for 3 days. Patients were instructed to use a mouthwash containing with 0.12% of chlorhexidine twice daily for 7 days.
Patients were anesthetized with 4% of articaine with 1:100.000 epinephrine (DFL, Rio de Janeiro, RJ, Brazil) using the inferior alveolar nerve block technique, complemented with the local infiltrative technique. A linear incision was made using a 15c scalpel blade in the bone crest. The detachment of the flap was performed with a Molt detacher, and the demarcation of the perforation site was started with the spear drill mounted on a 20:1 contra-angle until the desired height. Irrigation was performed with saline solution, and perforations were performed with the corresponding 2.0 conical burs and the 3.0 conical bur. Implants were installed 1 mm below the bone crest with a contra-angle to a torque of 35 Ncm and were finished with a surgical torque meter (Implacil de Bortoli, São Paulo, SP, Brazil) to verify the insertion torque.
All implants were installed using the Bortoli Implacil kit. A conventional drilling with a drill up to 3.0 mm was used, unlike the manufacturer’s recommendation, which recommends the last reamer of 3.5 mm, to test this drilling protocol on all implants of both groups. If the implant achieved a torque greater than 60 Ncm, it was removed, and a 3.5 mm drill of the drilling sequence was used so that the insertion torque was not high to prevent marginal bone loss at the sites. The insertion torque of each implant was checked, and a SmartPeg was installed directly on the implant to assess the primary stability by resonance frequency. Subsequently, a mini-abutment (Implacil de Bortoli, São Paulo, SP, Brazil) was installed with a torque of 20 Ncm with a prosthetic torque meter and specific wrench. The surgical procedure was completed with a 5.0 nylon suture thread.
Assessment of primary and secondary stability
Primary stability was evaluated by the insertion torque values of each implant, and compared to their implant stability quotient (ISQ) values with the Ostell instrument (Integration Diagnostics AB, Göteborg, Sweden), both directly on the implant and on the mini-abutment installed. The ISQ assessment in the post-implant installation period was performed on the mini-abutment to facilitate this assessment and avoid overloading the healing implant [30]. At the time of implant installation, the ISQ assessment can be performed directly on the implant without damaging it [31].
The RFA test was performed at the time of implant installation directly on the implant, on the mini-abutment on the day of installation, and on the same mini-abutment after 7, 14, 21, 28, and 42 days. RFA produces an ISQ that ranges from 1 to 100; a higher ISQ value indicates a greater clinical rigidity. At each measurement visit, SmartPeg was installed on the mini-abutment with a torque of 10 Ncm, and the measurements were repeated. The ISQ was measured by the same independent examiner in four different positions (mesial, distal, lingual, and buccal) perpendicular to the SmartPeg (Fig. 3). The mean values were considered as the value of primary or secondary stability when measured on the day of implant installation or during follow-up, respectively. Measurements were performed independently, evaluating one implant at a time, the examiner blinded of the group, and SmartPegs were individualized for each implant.
In all follow-up consultations, clinical evaluations were performed to investigate the edema and signs of infection, and the patient was enquired about the presence of postoperative pain and discomfort.
Statistical analysis
Data were analyzed using a statistical program (SPSS 25.0, IBM Statistics, New York, NY, USA). The Shapiro–Wilk test showed a non-normal data distribution. The correlation between the insertion torque and ISQ at the time of implant placement was analyzed using Spearman’s non-parametric test. The non-parametric Mann–Whitney U test was used to assess the differences between the groups, and the Friedman test was used to assess the difference between the ISQ results in the samples at different times. The sample power test was performed to determine the significance of the sample. Tests were performed at a significance level of 5%.
Results
In total, 26 implants were placed in the posterior region of the mandible in eight patients (women, 7; man, 1) aged between 38 and 69 years. All implant insertion sites were randomized, resulting in 13 implants in the GC group and 13 implants in the CT group evaluated.
In the analysis between groups at different evaluation times, there was a statistically significant difference at T-7, with higher ISQ values for the GT (p = 0.01; Table 1). Although there was no significant difference in the other times, ISQ median values were higher in the GT group than GC group at 28 days (GT = 67.98 and GC = 63.46; p = 0.05) and 42 days (GT = 66.12 and GC = 60.33; p = 0.09). Table 1 shows the mean values, standard deviation, median, and interquartile range of insertion torque, ISQ on the implant at T-0, and ISQ on mini-abutment at all times points.
No statistically significant correlation was found between the insertion torque and ISQ at the time of installation (p > 0.05) (Table 2).
In the Friedman test, there was a significant difference in terms of the ISQ results at different time points, both for the total sample (p = 0.004) and the samples of the GT (p = 0.035) and GC (p = 0.043), showing higher values over time.
A sample power of 77.2% was obtained for ISQ values at T-7 (p = 0.01), confirming the statistical power of this sample for this time point.
Figure 4 presents a graph with Q1, Q2 (median), Q3, and minimum and maximum ISQ values on the mini-abutment at different time points.
Discussion
Implant characteristics have been improved to achieve ideal secondary stability in a short period of time [32, 33]. Already well documented in the literature and widely known by clinicians, Straumann implants have rapid osseointegration, and Both GT implants (Maestro Implants) with trapezoidal threads and Straumann implants with conventional threads present with low insertion torque or locking [10]. The same is evaluated by a torquemeter: the low torque of the test implants can be conferred by the healing chambers, while the low torque of the Straumann control implants can be verified by the type and shape of the threads. Despite the mechanical torque being low in both types of implants, the secondary stability performance is comparable, with ISQ results close to 70 at 28 and 42 days, indicating a good stability value closer to 70. In the present study, the values of ISQ in the GT at 28 and 42 days were 68; These values were close to the ISQ values of 70 presented in the group of implants with the same characteristics installed in the rabbit tibiae [10].
The primary stability of the implant must be obtained to achieve the desired bone healing, with new bone formation around the implant and its maturation without the formation of connective tissue [34]. For this, the implant needs to remain static in the bone, respecting its primary stability [35]. However, the high insertion torque can impair the optimal healing of the implant in the bone tissue by osseointegration, and the development of implants with smoother threads and smaller lengths and depths of chambers between the threads is increasingly widespread [36]. Thus, a final consensus advocates an ideal insertion torque value between 30 and 50 Ncm, and torques above this value may impair the osseointegration [37]. In our study, the mean insertion torque was approximately 40–45 Ncm, which is within the recommended value. Previous studies have indicated the excellent performance of the Straumann SLA implant, both in its reduced osseointegration time and the amount of newly formed bone in close contact with the implant [17, 18, 38]. In addition to the surface treatment, this characteristic may also be due to the low value of insertion torque due to the softer and less compressive threads, in addition to the low length of chambers between the implant threads. Implants with healing chambers (Maestro implants) showed higher ISQ and BIC% (bone-implant contact) values than those with Straumann implants 28 days after their insertion in rabbit tibias [10]. These values in animals show a similarity between the Straumann and Implacil Maestro implants with healing chambers.
In this study, the healing chambers on the surface of the implant in the GT provided an increase in the contact area between the implant and the bone while reducing the insertion torque and bone necrosis around the implant [8, 9]. This characteristic tends to increase the BIC area, reducing the time of secondary stability of the implant and consequently reducing the healing time of the implant in the bone, allowing an opening of the implant to perform the definitive prosthesis in less time [8, 9]. In the present study, it was not possible to assess the BIC% value because it was a human study; Although there is no statistically significant difference between the ISQ of both groups tested in our study, the mean and median values of ISQ in GT for 28 and 42 days are higher, which may indicate an acceleration trend of osseointegration and a possibility of earlier prosthetic loading in implants with healing chambers.
Some in vitro studies show that the primary stability of implants with and without healing chambers is similar because the insertion ISQ of these implants is similar, although the insertion torque is lower in implants with healing chambers [39,40,41]. Animal studies show higher ISQ and BIC% values in the group of implants with healing chambers than in implants without chambers, after a period of 4 weeks [8, 9, 11]. Our study showed no difference in insertion ISQ between the groups, corroborating the literature confirming good primary stability of the tested implants, in addition to also showing good secondary stability.
In the present study, a conventional drilling protocol was used with the last helical drill cutter 0.5 mm smaller than the inserted implant diameter for both groups, but when the implant was inserted with a higher torque, above 60 Ncm, the implant was removed, and an optional 3.5 mm diameter drill was used so that the insertion torque was not high. The values of both insertion torque and insertion ISQ were very close between the groups, which may be due to the standardization that we obtained in our study. To improve the primary stability, especially in more medullary bone, such as type IV bone [42], under-drilling performed with drills with a 0.6 to 1.5 mm difference in implant diameter can increase implant locking, especially in those with a low insertion torque due to the macrogeometry and presence of a more medullary bone [7, 40, 43,44,45]. In implants with macrogeometry that confers a high locking, sub-drilling in more cortical bone (types I and II) [42] is not recommended because the insertion torque becomes higher with a greater probability of bone necrosis in the bed and results in greater marginal bone loss [7, 46]. The greater compression may occur due to the thread geometry of the implant, having a greater compression with more aggressive threads for greater locking [47]. When there is an excessive compression of the implant in the bone due to the high insertion torque of the implant, forces are transmitted to the adjacent bone, which may cause irreversible damage and reach a maximum threshold with plastic deformation, microcracks, and even necrosis [48]. Greater damage tends to occur mainly in the cortical bone, which does not have a good blood supply and is more easily reabsorbed by necrosis [49].
The manufacturer of the implants used in this research recommended the use of drills up to 3.5 mm for the insertion of implants of 3.5 mm in diameter (types I and II) in the mandible region. This protocol favors decompression of the implant walls in the bone bed, thereby reducing the implant insertion torque [8,9,10,11, 39, 40]. This study did not follow the manufacturer’s recommendation because we used a conventional drilling protocol in which the last reamer is 0.5 mm smaller in diameter than the diameter of the installed implant. This protocol is widely recommended by several implant manufacturers, including Straumann implants, which mostly have a drilling protocol with the last helical reamer in a 3.5 mm diameter for regular implants of 4.1 mm in diameter, providing rapid osseointegration [14, 15, 50]. The Straumann Tapered Effect and Bone Level implants are self-tapping implants, different from the Straumann Standard Plus implant. These self-threading implants, with the same conventional drilling protocol (last drill 3.5 mm for implants of 4.1 mm in diameter), have a higher insertion torque than Standard Plus implants; however, they have similar osseointegration from 4 to 6 weeks, resulting in an ISQ above 70 in this period [50]. Herein, we aimed to adopt a conventional drilling protocol to test whether the macrogeometry influences the secondary stability in these conditions, similar to most systems because the risk of loss of insertion torque in implants installed with over-drilling (last drill similar to the diameter of the implant) can be considerable. Thus, in our study, we obtained an insertion torque pattern of 43 Ncm in both groups, with no difference between the values of both insertion ISQ and ISQ in subsequent evaluations, which may have been influenced by the established drilling protocol.
Surface treatment also influences the primary and secondary stability of the implant [16, 20, 21, 51]. The implants in the groups GT and GC underwent surface treatment using blasting titanium oxide microparticles (≅ 100 μm), and were washed ultrasonically with alkaline solution and distilled water and submitted to the application of maleic acid, resulting in roughness of Ra = 0.56 ± 0.10 μm. In vitro studies carried out with the same implant tested in our study with healing chambers revealed higher values for implant removal torque and a higher bone fraction occupancy rate (BAFO%) in implants with healing chambers with treated surfaces than in implants with a machined surface [9]. Traditional implants with surface treatment provide better performance and a shorter time to reach secondary stability, with greater bone production on their surface, when compared to implants without surface treatment [52,53,54]. The implant used in this study has a roughness of Ra = 0.56 ± 0.10 μm; however, one study found a greater differentiation and recruitment of osteoblasts on surfaces with medium roughness, around 1–2 μm of roughness [55]. Therefore, improving the surface treatment and presence of healing chambers is recommended for better secondary stability.
In the present study, the ISQ values in the GT group were < 70, despite being close to this value. In ideal values for the load on the implant, the Osstell manufacturer recommends ISQ values of ≥ 70 [56]. Therefore, based on the results of the present study, it may be imprudent to indicate load application with the installation of a definitive prosthesis in the period of 42 days for implants tested in the mandible with a conventional drilling protocol. However, the implants in the GT tended to have a shorter osseointegration time than the implants in the GC group, probably not requiring an osseointegration time of 90 days in the mandible.
As for the limitations, despite being a prospective and randomized clinical study with a higher level of scientific evidence than a cohort study, since the researcher controls the actions and clinical follow-up, it was difficult to obtain a larger sample of patients due to recruitment and selection criteria eligibility, and specific time to follow the entire sample [57]. A sample with less than 30 participants is able to estimate data characterized by a population when specific statistical tests are applied according to their distinction of normality; however, in a larger sample, the statistical differences become more evident as the discrepancies of some values that do not follow the general average do not have much influence [58, 59]. In addition, we tested implants with a different drilling protocol than that recommended by the manufacturer. This may have influenced the results obtained, as studies of animals with the drilling protocol recommended by the manufacturer showed a significant difference between ISQ after 28 days, between implants with and without healing chambers [8,9,10]. Regarding the demographics of the patient sample, we believe that there was no interference in the results, since we kept the sample very similar with the eligibility criteria, since all patients were healthy, without any different health conditions, did not take continuous medication and did not have any type of addiction. Regarding clinical characteristics, we matched the position of the implant in the posterior region of the mandible, all having antagonists in the maxilla. With these similar characteristics, we believe that these factors did not interfere in the result. Although most studies test the ISQ for up to 45 days, it would be prudent to have future studies that test this value for a longer period to evaluate the pattern of bone healing over time to ensure that this pattern is ascending and that it does not decrease in values as it could affect the time of prosthetic implementation and prosthetic functionality. Therefore, it is recommended to develop future randomized clinical trials with implants that have decompression chambers compared to the same type of implant without them, inserted with the drilling protocol recommended by the manufacturer, to assess whether this device can influence the acceleration and quality of osseointegration, seeking to define an ideal prosthetic loading time protocol for these implants inserted in the mandible and maxilla.
Conclusion
Regarding secondary stability, no difference was observed between the implants tested with the two macrogeometries, inserted with a conventional drilling protocol, and evaluated for a period of 42 days. Therefore, the healing chambers did not influence the implant stability quotient (ISQ) values, providing secondary stability similar to that of the group without healing chambers.
Implants with and without healing chambers, inserted using a conventional drilling protocol, did not show different values for insertion torque and insertion ISQ, and there was no correlation between these values.
Although there is no significant difference between the groups, healing chambers may tend to accelerate osseointegration of implants, being feasible to apply prosthetic loading earlier than implants without healing chambers. Though, more clinical studies should be carried out to verify the secondary stability of these implants inserted both with the drilling protocol recommended by the manufacturer and with the conventional drilling protocol.
Data availability
All data generated or analysed during this study are included in this published article.
References
Albrektsson T, Chrcanovic B, Jacobsson M, Wennerberg A. Osseointegration of implants: a biological and clinical overview. JSM Dent Surg. 2017;2(3).
Adell R, Eriksson B, Lekholm U, Brånemark P-I, Jemt T. A long-term follow-up study of osseointegrated implants in the treatment of totally edentulous jaws. Internat J Oral Maxillofac Implants. 1990;5(4). PMID: 2094653.
Marao HF, Jimbo R, Neiva R, Gil LF, Bowers M, Bonfante EA et al. Cortical and Trabecular Bone Healing Patterns and Quantification for Three Different Dental Implant Systems. Int J Oral Maxillofac Implants. 2017;32(3):585 – 92. https://doi.org/10.11607/jomi.4856 PMID: 27835707.
de Pimentel Lopes GJ, Leite FC, Pontes AE, Sakakura CE, Junior EM. Comparison of the Primary and Secondary Stability of Implants with Anodized Surfaces and Implants Treated by Acids: A Split-Mouth Randomized Controlled Clinical Trial. Int J Oral Maxillofac Implants. 2016;31(1):186 – 90. https://doi.org/10.11607/jomi.4212 PMID: 26800177.
Campos FE, Gomes JB, Marin C, Teixeira HS, Suzuki M, Witek L et al. Effect of drilling dimension on implant placement torque and early osseointegration stages: an experimental study in dogs. J Oral Maxillofac Surg. 2012;70(1):e43-50. https://doi.org/10.1016/j.joms.2011.08.006 PMID: 22182660.
Jimbo R, Tovar N, Anchieta R, Machado L, Marin C, Teixeira H et al. The combined effects of undersized drilling and implant macrogeometry on bone healing around dental implants: an experimental study. Int J Oral Maxillofac Surg. 2014;43(10):1269-75. https://doi.org/10.1016/j.ijom.2014.03.017 PMID: 24794761.
Antonacci D, Del Fabbro M, Bollero P, Stocchero M, Jinno Y, Canullo L. Clinical effects of conventional and underprepared drilling preparation of the implant site based on bone density: A systematic review and meta-regression. J Prosthodont Res. 2022. https://doi.org/10.2186/jpr.JPR_D_21_00275 PMID: 35321991.
Gehrke SA, Aramburu JJ, Perez-Diaz L, do Prado TD, Dedavid BA, Mazon P et al. Can changes in implant macrogeometry accelerate the osseointegration process? An in vivo experimental biomechanical and histological evaluations. PLoS One. 2020;15(5):e0233304. https://doi.org/10.1371/journal.pone.0233304 PMID: 32407416.
Gehrke SA, Aramburú Júnior J, Pérez-Díaz L, Treichel TLE, Dedavid BA, De Aza PN, et al. New Implant Macrogeometry to improve and accelerate the Osseointegration: an in vivo experimental study. Appl Sci. 2019;9(15). https://doi.org/10.3390/app9153181.
Gehrke SA, Junior JA, Eirles Treichel TL, Dedavid BA. Biomechanical and histological evaluation of four different implant macrogeometries in the early osseointegration process: An in vivo animal study. J Mech Behav Biomed Mater. 2022;125:104935. https://doi.org/10.1016/j.jmbbm.2021.104935 PMID: 34736028.
Gehrke SA, Tumedei M, Aramburu Junior J, Treichel TLE, Kolerman R, Lepore S et al. Histological and Histomorphometrical Evaluation of a New Implant Macrogeometry. A Sheep Study. Int J Environ Res Public Health. 2020;17(10). https://doi.org/10.3390/ijerph17103477 PMID: 32429405.
Sayin Ozel G, Inan O, Secilmis Acar A, Alniacik Iyidogan G, Dolanmaz D, Yildirim G. Stability of dental implants with sandblasted and acid-etched (SLA) and modified (SLActive) surfaces during the osseointegration period. J Dent Res Dent Clin Dent Prospects. 2021;15(4):226 – 31. https://doi.org/10.34172/joddd.2021.037 PMID: 35070174.
Cochran DL, Buser D, Ten Bruggenkate CM, Weingart D, Taylor TM, Bernard JP et al. The use of reduced healing times on ITI® implants with a sandblasted and acid-etched (SLA) surface: Early results from clinical trials on ITI® SLA implants. Clin Oral Implants Res. 2002;13(2):144–153. https://doi.org/10.1034/j.1600-0501.2002.130204.x PMID: 11952734.
Markovic A, Calvo-Guirado JL, Lazic Z, Gomez-Moreno G, Calasan D, Guardia J et al. Evaluation of primary stability of self-tapping and non-self-tapping dental implants. A 12-week clinical study. Clin Implant Dent Relat Res. 2013;15(3):341-9. https://doi.org/10.1111/j.1708-8208.2011.00415.x PMID: 22171668.
Stavropoulos A, Cochran D, Obrecht M, Pippenger BE, Dard M. Effect of Osteotomy Preparation on Osseointegration of Immediately Loaded, Tapered Dental Implants. Adv Dent Res. 2016;28(1):34–41. https://doi.org/10.1177/0022034515624446 PMID: 26927486.
Rupp F, Liang L, Geis-Gerstorfer J, Scheideler L, Hüttig F. Surface characteristics of dental implants: A review. Dent Mater. 2018;34(1):40–57. https://doi.org/10.1016/j.dental.2017.09.007 PMID: 29029850.
Körmöczi K, Komlós G, Papócsi P, Horváth F, Joób-Fancsaly Á. The early loading of different surface-modified implants: a randomized clinical trial. BMC Oral Health. 2021;21(1):1–8. https://doi.org/10.1186/s12903-021-01498-z PMID: 33902551.
Hao CP, Cao NJ, Zhu YH, Wang W. The osseointegration and stability of dental implants with different surface treatments in animal models: a network meta-analysis. Sci Rep. 2021;11(1):13849. https://doi.org/10.1038/s41598-021-93307-4 PMID: 34226607.
Albrektsson T, Zarb GA. Current interpretations of the osseointegrated response: clinical significance. Int J Prost. 1993;6. PMID: 8329101.
Buser D, Broggini N, Wieland M, Schenk RK, Denzer AJ, Cochran DL et al. Enhanced bone apposition to a chemically modified SLA titanium surface. J Dent Res. 2004;83(7):529 – 33. https://doi.org/10.1177/154405910408300704 PMID: 15218041.
Dos Santos MV, Elias CN, Cavalcanti Lima JH. The effects of superficial roughness and design on the primary stability of dental implants. Clin Implant Dent Relat Res. 2011;13(3):215 – 23. https://doi.org/10.1111/j.1708-8208.2009.00202.x PMID: 19744197.
Monje A, Ravida A, Wang HL, Helms JA, Brunski JB. Relationship Between Primary/Mechanical and Secondary/Biological Implant Stability. Int J Oral Maxillofac Implants. 2019;34:s7-s23. https://doi.org/10.11607/jomi.19suppl.g1 PMID: 31116830.
Benalcazar Jalkh EB, Parra M, Torroni A, Nayak VV, Tovar N, Castellano A et al. Effect of supplemental acid-etching on the early stages of osseointegration: A preclinical model. J Mech Behav Biomed Mater. 2021;122:104682. https://doi.org/10.1016/j.jmbbm.2021.104682 PMID: 34311324.
Pattijn V, Van Lierde C, Van der Perre G, Naert I, Vander Sloten J. The resonance frequencies and mode shapes of dental implants: Rigid body behaviour versus bending behaviour. A numerical approach. J Biomech. 2006;39(5):939–947. https://doi.org/10.1016/j.jbiomech.2005.01.035 PMID: 16488232.
Bechara S, Kubilius R, Veronesi G, Pires JT, Shibli JA, Mangano FG. Short (6-mm) dental implants versus sinus floor elevation and placement of longer (≥ 10‐mm) dental implants: a randomized controlled trial with a 3‐year follow‐up. Clinl Oral Implant Res. 2017;28(9):1097 – 107. https://doi.org/10.1111/clr.12923 PMID: 27402427.
Kim SJ, Ribeiro ALVL, Atlas AM, Saleh N, Royal J, Radvar M et al. Resonance frequency analysis as a predictor of early implant failure in the partially edentulous posterior maxilla following immediate nonfunctional loading or delayed loading with single unit restorations. Clin Oral Implant Res. 2015;26(2):183 – 90. https://doi.org/10.1111/clr.12310 PMID: 24325547.
Norton MR. The Influence of Low Insertion Torque on Primary Stability, Implant Survival, and Maintenance of Marginal Bone Levels: A Closed-Cohort Prospective Study. Intl J Oral Maxillofac Implant. 2017;32. https://doi.org/10.11607/jomi.5889 PMID: 28708918.
Schulz KF, Altman DG, Moher D, Group C. CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. Int J Surg. 2011;9(8):672-7. https://doi.org/10.4103/0976-500X.72352 PMID: 21350618.
Promsudthi A, Pimapansri S, Deerochanawong C, Kanchanavasita W. The effect of periodontal therapy on uncontrolled type 2 diabetes mellitus in older subjects. Oral Dis. 2005;11(5):293-8. https://doi.org/10.1111/j.1601-0825.2005.01119.x PMID: 16120115.
Bergamo ETP, Zahoui A, Barrera RB, Huwais S, Coelho PG, Karateew ED et al. Osseodensification effect on implants primary and secondary stability: Multicenter controlled clinical trial. Clin Implant Dent Relat Res. 2021;23(3):317 – 28. https://doi.org/10.1111/cid.13007 PMID: 34047046.
da Rocha Ferreira JJ, Machado LFM. Insertion Torque Value and Implant Stability Quotient: Separate Evaluation and Correlation for Different Clinical Parameters. Int J Oral Maxillofac Implants. 2022;37(4):812 – 22. https://doi.org/10.11607/jomi.9346 PMID: 35904839.
Steiner C, Karl M, Steiner D, Meyer B. Observational study on primary and secondary stability of two current bone level implant designs. Quintessence Int. 2021;0(0):0. https://doi.org/10.3290/j.qi.a45605 PMID: 33491395.
Albrektsson T, Wennerberg A. On osseointegration in relation to implant surfaces. Clin Implant Dent Relat Res. 2019;21:4–7. https://doi.org/10.1111/cid.12742 PMID: 30816639.
Lioubavina-Hack N, Lang NP, Karring T. Significance of primary stability for osseointegration of dental implants. Clin Oral Implants Res. 2006;17(3):244 – 50. https://doi.org/10.1111/j.1600-0501.2005.01201.x PMID: 16672018.
Javed F, Ahmed HB, Crespi R, Romanos GE. Role of primary stability for successful osseointegration of dental implants: Factors of influence and evaluation. Interv Med Appl Sci. 2013;5(4):162-7. https://doi.org/10.1556/IMAS.5.2013.4.3 PMID: 24381734.
Li MJ, Kung PC, Chang YW, Tsou NT. Healing Pattern Analysis for Dental Implants Using the Mechano-Regulatory Tissue Differentiation Model. Int J Mol Sci. 2020;21(23). https://doi.org/10.3390/ijms21239205 PMID: 33276683.
Greenstein G, Cavallaro J. Implant Insertion Torque: Its Role in Achieving Primary Stability of Restorable Dental Implants. Compendium of Continuing Education in Dentistry (Jamesburg, NJ: 1995). 2017;38(2):88–95; quiz 6. PMID: 28156122.
Nevins M, Parma-Benfenati S, Quinti F, Galletti P, Sava C, Sava C et al. Clinical and Histologic Evaluations of SLA Dental Implants. Int J Periodontics Restorative Dent. 2017;37(2):175 – 81. https://doi.org/10.11607/prd.3131 PMID: 28196156.
Gehrke SA, Perez-Diaz L, Mazon P, De Aza PN. Biomechanical Effects of a New Macrogeometry Design of Dental Implants: An In Vitro Experimental Analysis. J Funct Biomater. 2019;10(4). https://doi.org/10.3390/jfb10040047 PMID: 31731451.
Gehrke SA, Scarano A, de Lima JHC, Bianchini MA, Dedavid BA, De Aza PN. Effects of the Healing Chambers in Implant Macrogeometry Design in a Low-Density Bone Using Conventional and Undersized Drilling. J Int Soc Prev Community Dent. 2021;11(4):437 – 47. https://doi.org/10.4103/jispcd.JISPCD_96_21 PMID: 34430506.
Haseeb SA, Rajendra K, Manual L, Kochhar AS, Dubey D, Dang GS. Comparative evaluation of Implant Stability, insertion Torque, and Implant Macrogeometry in different bone densities using resonance frequency analysis. J Contemp Dent Pract. 2021;22(6):665–8. PMID: 34393124.
Oliveira MR, Goncalves A, Gabrielli MAC, de Andrade CR, Vieira EH, Pereira-Filho VA. Evaluation of Alveolar Bone Quality: Correlation Between Histomorphometric Analysis and Lekholm and Zarb Classification. J Craniofac Surg. 2021;32(6):2114-8. https://doi.org/10.1097/SCS.0000000000007405 PMID: 33405451.
de Carvalho Formiga M, Gehrke AF, De Bortoli JP, Gehrke SA. Can the design of the instruments used for undersized osteotomies influence the initial stability of implants installed in low-density bone? An in vitro pilot study. PLoS One. 2021;16(10):e0257985. https://doi.org/10.1371/journal.pone.0257985 PMID: 34618848.
Mello-Machado RC, Sartoretto SC, Granjeiro JM, Calasans-Maia JA, de Uzeda M, Mourao C et al. Osseodensification enables bone healing chambers with improved low-density bone site primary stability: an in vivo study. Sci Rep. 2021;11(1):15436. https://doi.org/10.1038/s41598-021-94886-y PMID: 34326400.
Lemos BF, Lopez-Jarana P, Falcao C, Rios-Carrasco B, Gil J, Rios-Santos JV et al. Effects of Different Undersizing Site Preparations on Implant Stability. Int J Environ Res Public Health. 2020;17(23). https://doi.org/10.3390/ijerph17238965 PMID: 33276529.
Bashutski JD, D’Silva NJ, Wang HL. Implant compression necrosis: current understanding and case report. J Periodontol. 2009;80(4):700-4. https://doi.org/10.1902/jop.2009.080581 PMID: 19335092.
Alemayehu DB, Jeng YR. Three-Dimensional Finite Element Investigation into Effects of Implant Thread Design and Loading Rate on Stress Distribution in Dental Implants and Anisotropic Bone. Materials (Basel). 2021;14(22). https://doi.org/10.3390/ma14226974 PMID: 34832374.
Winwood K, Zioupos P, Currey J, Cotton JR, Taylor M. The importance of the elastic and plastic components of strain in tensile and compressive fatigue of human cortical bone in relation to orthopaedic biomechanics. J Musculoskelet Neuronal Interact. 2006;6(2):134. PMID: 16849822.
Gholami H, Mericske-Stern R, Jöhren P, Enkling N. Bone Resorption around Self-Tapping Implants in Bone Density Type I-II: 3-Years Results of a Prospective Clinical Study. Int J Dent Oral Health. 2020;6(3). PMID: 16849822.
Toyoshima T, Tanaka H, Ayukawa Y, Howashi M, Masuzaki T, Kiyosue T et al. Primary Stability of a Hybrid Implant Compared with Tapered and Cylindrical Implants in an Ex Vivo Model. Clin Implant Dent Relat Res. 2015;17(5):950-6. https://doi.org/10.1111/cid.12205 PMID: 24506148.
Ogle OE. Implant surface material, design, and osseointegration. Dental Clinics. 2015;59(2):505 – 20. https://doi.org/10.1016/j.cden.2014.12.003 PMID: 25835806.
Marinho VC, Celletti R, Bracchetti G, Petrone G, Minkin C, Piattelli A. Sandblasted and acid-etched dental implants: a histologic study in rats. Int J Oral Maxillofac Implant. 2003;18(1). PMID: 12608672.
Grassi S, Piattelli A, Ferrari DS, Figueiredo LC, Feres M, Iezzi G et al. Histologic evaluation of human bone integration on machined and sandblasted acid-etched titanium surfaces in type IV bone. J Oral Implantol. 2007;33(1):8–12. https://doi.org/10.1563/0-791.1 PMID: 17410906.
Grassi S, Piattelli A, de Figueiredo LC, Feres M, de Melo L, Iezzi G et al. Histologic evaluation of early human bone response to different implant surfaces. J Periodontol. 2006;77(10):1736-43. https://doi.org/10.1902/jop.2006.050325 PMID: 17032118.
Andrukhov O, Huber R, Shi B, Berner S, Rausch-Fan X, Moritz A et al. Proliferation, behavior, and differentiation of osteoblasts on surfaces of different microroughness. Dent Mater. 2016;32(11):1374-84. https://doi.org/10.1016/j.dental.2016.08.217 PMID: 27637551.
Huang H, Wu G, Hunziker E. The clinical significance of implant stability quotient (ISQ) measurements: A literature review. J Oral Biol Craniofac Res. 2020;10(4):629 – 38. https://doi.org/10.1016/j.jobcr.2020.07.004 PMID: 32983857.
Arieta-Miranda JM, Ruiz-Yasuda CC, Perez Vargas LF, Torres Ricse DA, Diaz SP, Arieta YC et al. New Pyramid Proposal for the Levels of Scientific Evidence According to SIGN. Plast Reconstr Surg. 2022;149(4):841e-3e. https://doi.org/10.1097/PRS.0000000000008946 PMID: 35231000.
Rohrig B, du Prel JB, Wachtlin D, Kwiecien R, Blettner M. Sample size calculation in clinical trials: part 13 of a series on evaluation of scientific publications. Dtsch Arztebl Int. 2010;107(31–32):552-6. https://doi.org/10.3238/arztebl.2010.0552 PMID: 20827353.
Huang P, Woolson RF, O’Brien PC. A rank-based sample size method for multiple outcomes in clinical trials. Stat Med. 2008;27(16):3084 – 104. https://doi.org/10.1002/sim.3182 PMID: 18189338.
Acknowledgements
The authors greatly for Implacil De Bortoli Produtos Odontológicos Ltda by the material preparation and support.
Funding
This research received no external funding.
Author information
Authors and Affiliations
Contributions
Conceptualization, P.T.R.S., R.M. and G.F.F.G.; Statistical analysis, S.A.I.; Formal analysis, P.T.R.S.; Methodology, P.T.R.S., R.M, F.A.O.S.S, N.F.M, B.E.S.A.F.M.; Project administration, L.R.A-A. and E.A.R.R.; Resources, R.M.; Supervision, L.R.A-A. and E.A.R.R.; Writing—original draft, P.T.R.S.; Writing—review & editing, R.M., L.R.A-A, E.M.S. and E.A.R.R.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethics and Research Committee of Pontifícia Universidade Católica do Paraná (PUCPR - number 5.338.876) and was registered in ReBec (brazilian registry of clinical trials) under the number RBR-96n5 × 69. Written informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
da Rosa de Souza, P.T., Manfro, R., de Salles Santos, F.A.O. et al. Analysis of osseointegration of implants with macrogeometries with healing chambers: a randomized clinical trial. BMC Oral Health 24, 1114 (2024). https://doi.org/10.1186/s12903-024-04857-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12903-024-04857-8