Abstract
Background
Chronic systemic inflammation has been proposed as the underlying mechanism of pain chronicity in several pain conditions. In spite of the growing evidence supporting the role of systemic inflammatory markers as a diagnostic tool, their role has not been analyzed in a well-defined group of temporomandibular disorders (TMD) patients until now. This study aimed to investigate the association between various clinical features and comorbidity levels of TMD in relation to hematological markers and seek its association with long-term treatment response.
Methods
Clinical features and hematological indices including those for systemic inflammation were assessed in TMD patients (n = 154). Examinations were re-done after 6 months of conservative treatment. Patients were divided into pain improved and unimproved groups based on ≥ 2 numeric rating scale improvement in pain intensity at 6 months for final analysis.
Results
The portion of patients with low lymphocyte-to-monocyte ratio (p = 0.026), total protein (p = 0.014), hemoglobin (p = 0.040), and mean corpuscular hemoglobin concentration (p = 0.042) values showed significant differences according to prognosis groups. Low hemoglobin levels were significantly associated with unfavorable response to long-term treatment (β = 1.706, p = 0.018). High pre-treatment pain intensity (β=-0.682, p < 0.001) and low Graded Chronic Pain Scale (β = 1.620, p = 0.002) could predict significant pain improvement with long-term treatment.
Conclusions
Hematologic assessment could be considered in addition to clinical examination to better determine long-term prognosis in TMD patients.
Similar content being viewed by others
Background
Temporomandibular disorders (TMD) is a common form of orofacial pain involving the temporomandibular joints (TMJ) and masticatory muscles [1]. It is known to affect 6–12% of the adult population and is more common in women with a peak prevalence around the age of 20–40 years [2, 3]. According to a recent meta-analysis, the overall prevalence of TMD was reported to be somewhat higher as approximately 31% for adults/elderly and 11% for children/adolescents [4]. Conventional conservative treatments for TMD include education, physical therapy, medication, and intraoral appliance therapy while more recent attempts include temporomandibular joint disc regeneration or replacement using tissue engineering [5, 6]. TMD is known as a multifactorial disease with reported causes involving psychosocial aspects and systemic diseases [1, 2, 7]. While symptoms are mild and self-limiting in most patients, a chronic type of TMD may develop with persistent pain and a higher level of comorbidities including psychological, autonomic, and sleep disturbances [8, 9]. Due to the lack of full understanding involving its initiation and progression, the current diagnostic process for TMD is centered on verifying symptoms through patient interviews, muscle and joint palpations, and imaging of associated structures. This leads to symptomatic treatment rather than pathophysiology-driven therapy which also makes it difficult to predict prognosis [10].
Systemic inflammation may occur as a persistent, low-grade, long-lasting, and non-infective type. Exogenous factors which are also well-known confounders of TMD such as chronic stress, unhealthy habits or environmental changes along with endogenous stimuli could contribute to systemic inflammation [11]. Recently, systemic inflammation has been proposed as a causative factor of pain chronicity in several pain conditions such as fibromyalgia and complex regional pain syndrome [12, 13]. A few studies have also suggested the possibility of immune disturbance in TMD patients, although the results are limited due to their cross-sectional study design or small sample size [14, 15]. The critical role of systemic inflammation has been continuously investigated in major health conditions [16, 17]. However, the current literature on systemic inflammation in TMD as a more localized condition and with well-defined patient groups is extremely limited [18]. Active research to locate hematologic biomarkers of systemic inflammation that are closely related to disease activity and mortality has resulted in the investigation of representative markers including neutrophil-to-lymphocyte ratio (NLR), lymphocyte-to-monocyte ratio (LMR), platelet-to-lymphocyte ratio (PLR), and systemic immune-inflammation index (SII) [19,20,21,22,23]. In spite of the growing evidence supporting the possible role of systemic inflammatory markers as a diagnostic tool, their role has not been analyzed in a well-defined group of TMD patients until now.
Therefore, the aim of this study is to investigate the association between various clinical features and comorbidity levels of TMD in relation to hematologic markers of systemic inflammation and seek its association with long-term response to conventional treatment. And also, to explore the value of inflammatory biomarkers as possible diagnostic indices of TMD prognosis.
Materials and methods
Subjects
Consecutive patients who visited the Department of Orofacial Pain Clinic of Seoul National University Dental Hospital complaining of TMD related symptoms from March, 2013 to April, 2019 were studied. TMD was diagnosed following the research diagnostic criteria for TMD (RDC/TMD) [24, 25]. All physical examinations were done by a single experienced orofacial pain specialist who was calibrated by RDC/TMD consortium criteria (n = 607).
Exclusion criteria included those with other pain disorders within 6 months of study initiation, uncontrolled hypertension, hyperlipidemia, diabetes mellitus, musculoskeletal, psychiatric, rheumatologic and immune diseases, extended medication use within 2 months of study initiation, recent trauma history or orthognathic surgery, and presence of active inflammation or infection. Rheumatoid factor (RF) and/or antinuclear antibody (ANA) positive patients were referred to a rheumatologist and only included when not diagnosed with a definitive autoimmune and rheumatologic disease (n = 163). For longitudinal analysis, patients missing RDC/TMD axis II (n = 52) and 6 months follow-up data (n = 238) were also excluded. The final group subjected to analysis included 154 patients (mean age 30.2 ± 10.6 years).
All methods were performed in accordance with the Declaration of Helsinki and relevant guidelines. This work was approved by the Institutional Review Board of Seoul National University Dental Hospital (ERI19024). Waiver of additional informed consent was granted considering the retrospective nature of the study and no patient images were utilized in this study.
Assessment of temporomandibular disorders and related comorbidities
History taking of medical conditions and comorbidities was conducted along with a comprehensive intraoral examination. Degenerative joint disease of the TMJ was diagnosed based on plain radiographs when erosion of the cortical bone, osteophyte, and subcortical cyst formation was observed.
Clinical parameters including comfortable (CMO) and maximum mouth opening (MMO), pain on palpation of muscles (masticatory and cervical) and TMJ capsule area, and pain on mouth opening were examined. Subjective pain intensity was evaluated on a numeric rating scale (NRS, 0–10).
Psychological status and disability levels were evaluated with Symptom Checklist-90-Revision (SCL90R) [26] and RDC/TMD axis II questionnaires [27].
Hematologic assessment
Samples were taken from the antecubital vein at the first visit before treatment initiation. Complete blood cell counts with white blood cell (WBC) differential, red blood cell (RBC) indices, blood chemistry along with C-reactive protein (CRP), ANA (titers ≥ 1:40 considered positive), and RF were evaluated.
Inflammatory biomarkers including NLR (neutrophil/lymphocyte count), derived NLR (dNLR, absolute neutrophil/[white blood cell-absolute neutrophil count]), LMR (lymphocyte/monocyte count), PLR (platelet/lymphocyte count) and SII (platelet x [neutrophil /lymphocyte count]) were calculated [28, 29]. Cutoff values for NLR (male: 1.634, female 1.662), LMR (male: 5.048, female: 5.598), and PLR (male: 122.726, female: 142.759) were based on mean values from Koreans [30].
Assessment of long-term treatment response
Conservative treatment included control of contributing factors, self-exercise, occlusal stabilization splint, physical therapy (moist hot pack, ultrasound, electrical stimulation, and low-level laser), and medications including non-steroidal anti-inflammatory drugs. Patients were re-evaluated for CMO, MMO, pain on palpation of masticatory muscles and TMJ capsule, and pain intensity at 6 months from the first examination by the same clinician. For final analysis, patients were differentiated into pain improved and unimproved groups with ≥ 2 NRS improvement in pain intensity as criterion.
Statistical analysis
Normality of data was tested with Kolmogorov-Smirnov test and methods were selected accordingly. Differences between improved and unimproved groups were analyzed with student’s t-test or Mann-Whitney U test and chi-square test or Fisher’s exact test. Changes in clinical signs at 6 months were analyzed with Wilcoxon singed rank test and McNemar test. Logistic regression analysis was performed to evaluate baseline parameters affecting post-treatment pain improvement. Correlations of each dimension of TMD clinical and hematological parameters were analyzed by Spearman’s correlation coefficients. Receiver operating characteristic (ROC) curve and area under the curve (AUC) were analyzed to evaluate the power of pre-treatment hematological biomarkers in predicting post-treatment pain improvement. All statistical analyses were performed using SPSS 26.0 software (IBM, Chicago, IL, USA). Level of statistical significance was set at p < 0.05.
Results
Clinical characteristics according to prognosis groups
Baseline clinical characteristics
After 6 months of conservative treatment, 107 patients (69.5%) showed significant pain improvement (≥ 2 NRS improvement in pain intensity) and 47 (30.5%) did not.
As shown in Table 1, the pain improved group had a significantly higher pre-treatment pain intensity compared to the unimproved group based on both characteristic pain intensity (p = 0.034) and NRS scores on the initial visit (p < 0.001). Also, the pain improved group showed more pre-treatment functional disturbance as significantly smaller CMO values (p = 0.031) and more patients reporting pain on mouth opening (p = 0.011). There were no significant differences in baseline characteristics between the groups regarding confounders including age and gender, RDC/TMD axis I diagnoses, pain origin, and psychological conditions.
Changes in clinical signs with treatment
As shown in Table 2, all measured clinical and functional indices were significantly improved in the pain improved group with 6 months’ conservative treatment however, only the percentage of those with pain on masticatory muscle palpation significantly decreased in the unimproved group. Functional disturbance and pain persisted in this group.
Hematologic marker levels according to prognosis groups
As shown in Table 3, significantly more patients in the pain improved group had an abnormally low pre-treatment LMR value (p = 0.026). NLR, dNLR, PLR, and SII values were higher and LMR value was lower in the pain improved group although the difference was not statistically significant. Among red blood cell parameters, the pain improved group had a significantly higher hemoglobin (Hgb) concentration (p = 0.040) and more patients in the unimproved group had an abnormally low Hgb level (p = 0.046). Also, the mean corpuscular hemoglobin concentration (MCHC) was significantly higher in the improved group (p = 0.042). Significantly more patients in the pain unimproved group had an abnormally high protein concentration (p = 0.014).
Correlation between clinical characteristics and hematologic markers
RBC levels were significantly correlated with 6 months’ post-treatment CMO (r = 0.288, p < 0.001) and MMO (r = 0.257, p = 0.001) values. Hgb concentration was significantly correlated with 6 months’ post-treatment CMO (r = 0.240, p = 0.003) and MMO (r = 0.234, p = 0.003) values. Hematocrit was significantly correlated with 6 months’ post-treatment CMO (r = 0.261, p = 0.001) and MMO (r = 0.255, p = 0.001). Mean corpuscular volume (MCV) was significantly correlated with pain duration (r=-0.176, p = 0.030). Erythrocyte sedimentation rate (ESR) was significantly correlated with 6 months’ post-treatment CMO (r=-0.168, p = 0.038) and MMO (r=-0.160, p = 0.047).
Clinical and hematological parameters associated with refractory TMD pain
Logistic regression analysis was carried out with pre-treatment clinical and hematologic markers as independent variables and unimproved TMD pain as the dependent variable.
As shown in Table 4, high disability level of the Graded Chronic Pain Scale (GCPS) (β = 1.620, p = 0.002), and low pre-treatment pain intensity on NRS (β=-0.682, p < 0.001) was associated with long-term refractory TMD pain.
As shown in Table 5, abnormally low Hgb level (β = 1.706, p = 0.018) was associated with refractory TMD pain.
Effectiveness of pre-treatment hematologic markers in predicting long-term refractory TMD pain
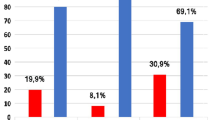
As shown in Table 6; Fig. 1, receiver operating characteristic (ROC) curve analyses showed that Hgb had sufficient predictive power to discriminate refractory TMD pain with a cutoff of 13.2 g/dL (area under the curve [AUC] = 0.604, p = 0.041).
Receiver operating characteristic (ROC) curves for long-term refractory TMD pain. The diagnostic ability was significant for hemoglobin concentration. AUC, area under the curve; NLR, neutrophil-to-lymphocyte ratio; dNLR, derived NLR ratio; LMR, lymphocyte-to-monocyte ratio; PLR, platelet-to-lymphocyte ratio; SII, systemic immune-inflammation index; Hgb, hemoglobin; ESR, erythrocyte sedimentation rate; CRP, C-reactive protein
Discussion
The results of this study showed that low Hgb levels were associated with long-term refractory TMD pain. Also, less patients had a low LMR value which is known to reflect an enhanced inflammatory status. Additionally, the total protein concentration reached abnormally high levels more frequently in refractory TMD patients. Such results point towards the possible involvement of systemic inflammation in TMD patients that do not respond well to conventional treatment.
This is the first study to investigate the relationship between clinical characteristics and hematological biomarkers of systemic inflammation such as NLR, dNLR, LMR, PLR, and SII in TMD patients. The growing interest in research to better understand disease states or predict prognosis with simple blood testing has led to the investigation of biomarkers involving nonspecific inflammation. And previous studies support the role of such indices in evaluating disease severity [16,17,18,19,20,21,22,23]. When TMD patients were grouped according to long-term treatment response, less patients in the unimproved group showed lower LMR values (p = 0.026) and the mean value was higher compared to the improved group although the difference did not reach statistical significance. Such a finding could be considered more significant since the applied cutoff value was based on data derived from Koreans and differentially applied according to gender. Studies show that mean values of hematologic markers of systemic inflammation including LMR, may differ according to ethnic group and gender hence, applying a cutoff value derived from other races could affect results [30]. However, this point was often not considered in other studies. Lower LMR values are known to reflect a higher degree of systemic inflammation and is frequently associated with poor prognosis. On the other hand, there is one research on breast cancer patients showing that low LMR has been reported as a predictive factor of favorable response [31]. In this aspect, the results of our study may appear contradictory to previous studies reporting a negative relationship between LMR and the level of postoperative pain [32]. Also, studies on rheumatoid arthritis investigating the relationship between pain levels and the same markers of systemic inflammation as in this study generally report that higher levels of inflammation are related to more pain [21]. Unfortunately, it is difficult to directly compare the results from such studies since most were of a cross-sectional design and smaller sample size which limits their validity to support a causal relationship. Since the decrease in pain intensity with TMD treatment was greater when the pre-treatment pain intensity was higher in our patients, it could be indirectly interpreted that the presence of nonspecific inflammation pre-treatment could be linked to higher pain intensity and better prognosis in terms of long-term pain improvement. From a different perspective, such a result could suggest that TMD with a larger inflammatory component responds more favorably to conventional treatment. Acute inflammation generally responds well to treatment in the majority of cases while, chronic pain is more often associated with low-grade inflammation [33]. The cutoff values of inflammatory indices used in this study were derived from healthy adults and data on values from specific disease groups is rare. This may have contributed to the failure of other hematologic markers of inflammation in reaching statistical significance and underlines the need to produce appropriate cutoff values that are associated with specific disease characteristics. Another point to consider is the cause of the change in inflammatory marker levels. Since those with active inflammation were excluded, it could be said that the inflammation present in the TMD patients is of a nonspecific nature which may have affected long-term treatment response. But still it is difficult to differentiate between systemic and local inflammation based on the indices investigated in this study.
Hgb levels in those with refractory TMD pain were decreased in this study. Also, abnormally low Hgb level was associated with unfavorable treatment response based on logistic regression analysis. Hgb level may also be considered as an indicator of inflammatory conditions. Anemia of chronic disease is most commonly present in infectious, inflammatory or neoplastic diseases. Mediators of the inflammatory response are considered to be involved in the development of anemia [34]. Low Hgb levels were associated with higher disease activity, structural damage, and joint dysfunction in rheumatoid arthritis (RA) [35]. Also, Hgb reflected inflammatory status and disease activity in systemic lupus erythematosus, so could be used as a marker to predict treatment outcome [36]. The pathogenesis of anemia in chronic diseases involves abnormalities of iron absorption, release from macrophages, and dysfunction of cytokine networks, all of which can result in inadequate erythropoiesis [35]. It has been known that the production of cytokines in RA leads to a decrease in iron availability and plays a direct toxic effect on erythropoietin. In RA patients, the increased activation of inflammatory cells causing excessive cytokine production including tumor necrosis factor (TNF)-α, interleukin (IL)-1β, and IL-6 acts on erythropoietin progenitor cells, promoting hemolysis and causing subsequent reduction in the number of circulating red blood cells [35]. Inflammation could lead to the development of inflammatory anemia. Lower levels of Hgb are found in autoimmune hemolytic anemia which is accompanied by systemic inflammation [37]. Based on such studies reporting that increased levels of inflammatory cytokines could result in low levels of Hgb, this could indirectly suggest the possibility of increased inflammatory cytokine levels in our refractory TMD patients. A recent study found that TMD patients with high disability showed increased inflammatory cytokine levels including IL-β, -6, -10, and TNF-α [15]. Another study showed that IL-8 and IgG levels were significantly increased in the high disability TMD group [14]. Inflammation in the nervous system play significant roles in many chronic pain conditions. Certain cytokines/chemokines may directly activate nociceptive sensory neurons initiating and maintaining pathologic pain. Certain inflammatory cytokines are also involved in central sensitization and resulting hyperalgesia/allodynia [38].
Another finding of this study related to the low Hgb level of those with refractory TMD pain was the lower MCHC level in the unimproved group compared to the improved group. MCHC reflects the amount of hemoglobin responsible for oxygen transportation in the RBCs and is related to iron storage. A lower MCHC level was associated with poor prognosis in chronic heart disease patients and could be applied as a biomarker for evaluating the prognosis of chronic obstructive pulmonary disease, both which are accompanied by increased systemic inflammation [39].
In our study, more patients of the unimproved group showed abnormally increased total protein levels. Total protein levels increase in inflammatory states as chronic inflammation is associated with substantial changes in protein metabolism [40]. Whole body protein synthesis and breakdown is increased in inflammatory conditions such as inflammatory bowel disease [41]. Also, increased levels of total protein are found in other diseases including multiple myeloma which are known to have an inflammatory component in its pathogenesis [42]. A previous review reported that vitamin D deficiency and TMD were associated [43] while vitamin D has been implicated in the underlying mechanism of inflammation and insulin resistance [44]. Such literature additionally supports the role of sub-inflammation in TMD and the need to investigate the matter in relation to already known substance of TMD etiology including vitamins and hormones. However, the current existing literature on systemic inflammation in TMD is more focused on analyzing cytokine levels from venous blood [14, 15, 18] and future studies should include a wider range of systemic inflammatory indices to provide a comprehensive view on the issue.
As for clinical variables related to unfavorable TMD prognosis, lower pre-treatment pain intensity showed significant association. The higher the initial subjective pain level, the greater the long-term decrease with treatment. This result is in line with a study based on TMD showing that higher pain intensity and more widespread pain pre-treatment were significantly related to more pain improvement with treatment [45].
On the other hand, high disability level based on GCPS was significantly associated with long-term refractory TMD pain. GCPS reflects not only the intensity of pain but also the level of disturbance in daily activities that the patient perceives to have. Interference in activities is also caused by common comorbidities of TMD such as psychological and sleep disturbances in addition to the pain intensity itself [15, 46]. Depression is a well-known contributing factor of chronic TMD as is primary sleep disorders such as obstructive sleep apnea and insomnia [47,48,49].
There are several limitations of this study to be considered. First, this study was a single-center study of a retrospective nature. Although known confounders of both TMD and hematologic markers were controlled, this was based on information from medical records and additional verification of systemic conditions was not carried out. Exclusion of subjects based on the presence of certain systemic conditions including other pain disorders was done by medical history taking through a structured interview and this could have resulted in the inclusion of certain data which was inappropriate for analysis. Secondly, hematologic information was not collected at the long-term follow-up point limiting the direct analysis between clinical and hematologic values after 6-months’ treatment. Future studies should involve collection of both data sets to allow a more precise establishment of their interrelationship. However, the aim of this study was to tentatively evaluate the possibility of hematologic indices as prognostic parameters and the longitudinal aspect of our study fulfills such an objective. Thirdly, patient diagnosis of this study followed the RDC/TMD since DC/TMD had not yet been implemented in the clinic during the designated study period. Results based on the more recent DC/TMD diagnosis could differ and future studies should apply the most recent diagnostic criteria for up-to-date information [50]. Fourthly, there may be statistical bias since a large number of patients were excluded from the parent population due to the lack of long-term follow-up data. Finally, our study did not produce results based on different gender and age groups although both factors were matched when comparing the groups. Also, all data was from Koreans so the results may not universally apply to other ethnic groups. The hematologic biomarkers investigated in this study are known to be affected by various factors including age, gender, race, and adverse health habits so, future studies should be designed to consider such conditions as well-designed prospective research to further validate the role of inflammatory biomarkers in the diagnosis of TMD.
In conclusion, high LMR values were observed in refractory TMD patients. Also, low Hgb and high total protein levels were associated with poor long-term prognosis in TMD with conventional treatment. Such results could indicate the possible role of nonspecific inflammation in chronic TMD pathogenesis. Their validity for clinical usage should be further evaluated in addition to clinical factors such as pain intensity and GCPS in TMD.
Data availability
The raw data supporting this study are not in the public domain but are available upon reasonable request from the corresponding author.
Abbreviations
- TMD:
-
Temporomandibular disorders
- TMJ:
-
Temporomandibular joints
- NLR:
-
Neutrophil-to-lymphocyte ratio
- LMR:
-
Lymphocyte-to-monocyte ratio
- PLR:
-
Platelet-to-lymphocyte ratio
- SII:
-
Systemic immune-inflammation index
- RDC/TMD:
-
Research diagnostic criteria for TMD
- RF:
-
Rheumatoid factor
- ANA:
-
Antinuclear antibody
- CMO:
-
Comfortable mouth opening
- MMO:
-
Maximum mouth opening
- NRS:
-
Numeric rating scale
- WBC:
-
White blood cell
- RBC:
-
Red blood cell
- Hgb:
-
Hemoglobin
- MCHC:
-
Mean corpuscular hemoglobin concentration
- MCV:
-
Mean corpuscular volume
- CRP:
-
C-reactive protein
- ESR:
-
Erythrocyte sedimentation rate
- ROC:
-
Receiver operating characteristic
- AUC:
-
Area under the curve
- GCPS:
-
Graded chronic pain scale
- TNF:
-
Tumor necrosis factor
- IL:
-
Interleukin
References
McNeill C, Mohl ND, Rugh JD, Tanaka TT. Temporomandibular disorders: diagnosis, management, education, and research. J Am Dent Assoc. 1990;120(3). https://doi.org/10.14219/jada.archive.1990.0049.
Yap AU, Cao Y, Zhang MJ, Lei J, Fu KY. Number and type of temporomandibular disorder symptoms: their associations with psychological distress and oral health-related quality of life. Oral Surg Oral Med Oral Pathol Oral Radiol. 2021;132(3):288–96. https://doi.org/10.1016/j.oooo.2021.04.059.
Liu F, Steinkeler A. Epidemiology, diagnosis, and treatment of temporomandibular disorders. Dent Clin North Am. 2013;57(3):465–79. https://doi.org/10.1016/j.cden.2013.04.006.
Valesan LF, Da-Cas CD, Réus JC, Denardin ACS, Garanhani RR, Bonotto D, Januzzi E, de Souza BDM. Prevalence of temporomandibular joint disorders: a systematic review and meta-analysis. Clin Oral Investig. 2021;25(2):441–53. https://doi.org/10.1007/s00784-020-03710-w.
Weekes KJ, Lam P, Kim C, Johnstone B. Characterization of temporomandibular joint articular disc progenitor cell clones. Eur Cell Mater. 2023;45:1–13. https://doi.org/10.22203/eCM.v045a01.
Helgeland E, Shanbhag S, Pedersen TO, Mustafa K, Rosén A. Scaffold-based Temporomandibular Joint tissue regeneration in Experimental Animal models: a systematic review. Tissue Eng Part B Rev. 2018;24(4):300–16. https://doi.org/10.1089/ten.TEB.2017.0429.
Covert L, Mater HV, Hechler BL. Comprehensive Management of Rheumatic diseases affecting the Temporomandibular Joint. Diagnostics (Basel). 2021;11(3):409. https://doi.org/10.3390/diagnostics11030409.
Scrivani SJ, Keith DA, Kaban LB. Temporomandibular disorders. N Engl J Med. 2008;359(25):2693–705. https://doi.org/10.1056/NEJMra0802472.
List T, Jensen RH. Temporomandibular disorders: old ideas and new concepts. Cephalalgia. 2017;37(7):692–704. https://doi.org/10.1177/0333102416686302.
Schiffman E, Ohrbach R. Executive summary of the Diagnostic Criteria for Temporomandibular disorders for clinical and research applications. J Am Dent Assoc. 2016;147(6):438–45. https://doi.org/10.1016/j.adaj.2016.01.007.
Zhou WBS, Meng J, Zhang J. Does low grade systemic inflammation have a role in chronic pain? Front Mol Neurosci. 2021;14:785214. https://doi.org/10.3389/fnmol.2021.785214.
Bäckryd E, Tanum L, Lind AL, Larsson A, Gordh T. Evidence of both systemic inflammation and neuroinflammation in fibromyalgia patients, as assessed by a multiplex protein panel applied to the cerebrospinal fluid and to plasma. J Pain Res. 2017;10:515–25. https://doi.org/10.2147/JPR.S128508. Published 2017 Mar 3.
Linnman C, Becerra L, Borsook D. Inflaming the brain: CRPS a model disease to understand neuroimmune interactions in chronic pain. J Neuroimmune Pharmacol. 2013;8(3):547–63. https://doi.org/10.1007/s11481-012-9422-8.
Son C, Park YK, Park JW. Long-term evaluation of temporomandibular disorders in association with cytokine and autoantibody status in young women. Cytokine. 2021;144:155551. https://doi.org/10.1016/j.cyto.2021.155551.
Park JW, Chung JW. Inflammatory cytokines and sleep disturbance in patients with Temporomandibular disorders. J Oral Facial Pain Headache. 2016;30(1):27–33. https://doi.org/10.11607/ofph.1367.
Gasparyan AY, Ayvazyan L, Mukanova U, Yessirkepov M, Kitas GD. The platelet-to-lymphocyte ratio as an inflammatory marker in Rheumatic diseases. Ann Lab Med. 2019;39(4):345–57. https://doi.org/10.3343/alm.2019.39.4.345.
Kumarasamy C, Sabarimurugan S, Madurantakam RM, Lakhotiya K, Samiappan S, Baxi S, Nachimuthu R, Gothandam KM, Jayaraj R. Prognostic significance of blood inflammatory biomarkers NLR, PLR, and LMR in cancer-A protocol for systematic review and meta-analysis. Med (Baltim). 2019;98(24):e14834. https://doi.org/10.1097/MD.0000000000014834.
Lerman SF, Mun CJ, Hunt CA, Kunatharaju S, Buenaver LF, Finan PH, Campbell CM, Phillips J, Fernandez-Mendoza J, Haythornthwaite JA, Smith MT. Insomnia with objective short sleep duration in women with temporomandibular joint disorder: quantitative sensory testing, inflammation and clinical pain profiles. Sleep Med. 2022;90:26–35. https://doi.org/10.1016/j.sleep.2022.01.004.
Mariani P, Russo D, Maisto M, Troiano G, Caponio VCA, Annunziata M, Laino L. Pre-treatment neutrophil-to-lymphocyte ratio is an independent prognostic factor in head and neck squamous cell carcinoma: Meta-analysis and trial sequential analysis. J Oral Pathol Med. 2022;51(1):39–51. https://doi.org/10.1111/jop.13264.
Mandaliya H, Jones M, Oldmeadow C, Nordman II. Prognostic biomarkers in stage IV non-small cell lung cancer (NSCLC): neutrophil to lymphocyte ratio (NLR), lymphocyte to monocyte ratio (LMR), platelet to lymphocyte ratio (PLR) and advanced lung cancer inflammation index (ALI). Transl Lung Cancer Res. 2019;8(6):886–94. https://doi.org/10.21037/tlcr.2019.11.16.
Chandrashekara S, Mukhtar Ahmad M, Renuka P, Anupama KR, Renuka K. Characterization of neutrophil-to-lymphocyte ratio as a measure of inflammation in rheumatoid arthritis. Int J Rheum Dis. 2017;20(10):1457–67. https://doi.org/10.1111/1756-185X.13157.
Erre GL, Paliogiannis P, Castagna F, Mangoni AA, Carru C, Passiu G, Zinellu A. Meta-analysis of neutrophil-to-lymphocyte and platelet-to-lymphocyte ratio in rheumatoid arthritis. Eur J Clin Invest. 2019;49(1):e13037. https://doi.org/10.1111/eci.13037.
Zhang Y, Meng Y, Chen M, Baral K, Fu Y, Yang Y, Cao L, Zhao M. Correlation between the systemic immune-inflammation indicator (SII) and serum ferritin in US adults: a cross-sectional study based on NHANES 2015–2018. Ann Med. 2023;55(2):2275148. https://doi.org/10.1080/07853890.2023.2275148.
Dworkin SF, LeResche L. Research diagnostic criteria for temporomandibular disorders: review, criteria, examinations and specifications, critique. J Craniomandib Disord. 1992;6(4):301–55.
Sohn BJ, Park MW, Park JW, Chung SC, Chung JW. Reliability of the Korean version of research diagnostic criteria for temporomandibular disorders (RDC/TMD). J Oral Med Pain. 2008;33(4):323–38.
Derogatis LR, Cleary PA. Confirmation of the dimensional structure of the SCL-90: a study in construct validation. J Clin Psychol. 1977;33(4):981–9.
Dworkin SF, Sherman J, Mancl L, Ohrbach R, LeResche L, Truelove E. Reliability, validity, and clinical utility of the research diagnostic criteria for Temporomandibular disorders Axis II scales: depression, non-specific physical symptoms, and graded chronic pain. J Orofac Pain. 2002;16(3):207–20.
Proctor MJ, McMillan DC, Morrison DS, Fletcher CD, Horgan PG, Clarke SJ. A derived neutrophil to lymphocyte ratio predicts survival in patients with cancer. Br J Cancer. 2012;107(4):695–9. https://doi.org/10.1038/bjc.2012.292.
Somay E, Yilmaz B. High pretreatment systemic immune-inflammation index values are associated with diminished short-term success after temporomandibular joint arthrocentesis procedure. BMC Oral Health. 2021;21(1):531. Published 2021 Oct 15. https://doi.org/10.1186/s12903-021-01899-0
Lee JS, Kim NY, Na SH, Youn YH, Shin CS. Reference values of neutrophil-lymphocyte ratio, lymphocyte-monocyte ratio, platelet-lymphocyte ratio, and mean platelet volume in healthy adults in South Korea. Med (Baltim). 2018;97(26):e11138. https://doi.org/10.1097/MD.0000000000011138.
Peng Y, Chen R, Qu F, Ye Y, Fu Y, Tang Z, Wang Y, Zong B, Yu H, Luo F, Liu S. Low pretreatment lymphocyte/monocyte ratio is associated with the better efficacy of neoadjuvant chemotherapy in breast cancer patients. Cancer Biol Ther. 2020;21(2):189–96. https://doi.org/10.1080/15384047.2019.1680057.
Yuan C, Wang Z, Zhu G, Wang C, Ma X, Wang X. Preoperative lymphocyte-to-monocyte ratio can indicate the outcomes in Repair of I-III Degree Injury of lateral ankle ligament. Biomed Res Int. 2022;2022:6234561. https://doi.org/10.1155/2022/6234561. Published 2022 Apr 19.
Lasselin J, Kemani MK, Kanstrup M, Olsson GL, Axelsson J, Andreasson A, Lekander M, Wicksell RK. Low-grade inflammation may moderate the effect of behavioral treatment for chronic pain in adults. J Behav Med. 2016;39(5):916–24. https://doi.org/10.1007/s10865-016-9769-z.
John M, Hoernig S, Doehner W, Okonko DD, Witt C, Anker SD. Anemia and inflammation in COPD. Chest. 2005;127(3):825–9. https://doi.org/10.1378/chest.127.3.825.
Chen YF, Xu SQ, Xu YC, Li WJ, Chen KM, Cai J, Li M. Inflammatory anemia may be an indicator for predicting disease activity and structural damage in Chinese patients with rheumatoid arthritis. Clin Rheumatol. 2020;39(6):1737–45. https://doi.org/10.1007/s10067-019-04873-y.
Yu H, Jiang L, Yao L, Gan C, Han X, Liu R, Su N. Predictive value of the neutrophil-to-lymphocyte ratio and hemoglobin in systemic lupus erythematosus. Exp Ther Med. 2018;16(2):1547–53. https://doi.org/10.3892/etm.2018.6309.
Fattizzo B, Barcellini W. Autoimmune hemolytic anemia: causes and consequences. Expert Rev Clin Immunol. 2022;18(7):731–45. https://doi.org/10.1080/1744666X.2022.2089115.
Zhang JM, An J. Cytokines, inflammation, and pain. Int Anesthesiol Clin. 2007;45(2):27–37. https://doi.org/10.1097/AIA.0b013e318034194e.
Sato K, Inoue S, Ishibashi Y, Ota T, Murano H, Furuyama K, Yang S, Machida H, Nakano H, Sato M, Nemoto T, Nishiwaki M, Yamauchi K, Igarashi A, Watanabe M. Association between low mean corpuscular hemoglobin and prognosis in patients with exacerbation of chronic obstructive pulmonary disease. Respir Investig. 2021;59(4):498–504. https://doi.org/10.1016/j.resinv.2021.01.006.
Mercier S, Breuillé D, Mosoni L, Obled C, Patureau Mirand P. Chronic inflammation alters protein metabolism in several organs of adult rats. J Nutr. 2002;132(7):1921–8. https://doi.org/10.1093/jn/132.7.1921.
Powell-Tuck J, Garlick PJ, Lennard-Jones JE, Waterlow JC. Rates of whole body protein synthesis and breakdown increase with the severity of inflammatory bowel disease. Gut. 1984;25(5):460–4. https://doi.org/10.1136/gut.25.5.460.
Morrison T, Booth RA, Hauff K, Berardi P, Visram A. Laboratory assessment of multiple myeloma. Adv Clin Chem. 2019;89:1–58. https://doi.org/10.1016/bs.acc.2018.12.001.
Ferrillo M, Lippi L, Giudice A, Calafiore D, Paolucci T, Renò F, Migliario M, Fortunato L, Invernizzi M, de Sire A. Temporomandibular disorders and vitamin D deficiency: what is the linkage between these conditions? A systematic review. J Clin Med. 2022;11:6231. https://doi.org/10.3390/jcm11216231.
Garbossa SG, Folli F, Vitamin D. Sub-inflammation and insulin resistance. A window on a potential role for the interaction between bone and glucose metabolism. Rev Endocr Metab Disord. 2017;18:243–58. https://doi.org/10.1007/s11154-017-9423-2.
Jo JH, Son C, Chung JW, Park JW. Presence of widespread pain predicts comorbidities and treatment response in temporomandibular disorders patients. Oral Dis. 2022;28(6):1682–96. https://doi.org/10.1111/odi.13987.
Yatani H, Studts J, Cordova M, Carlson CR, Okeson JP. Comparison of sleep quality and clinical and psychologic characteristics in patients with temporomandibular disorders. J Orofac Pain. 2002;16(3):221–8.
Cao Y, Yap AU, Lei J, Zhang MJ, Fu KY. Subtypes of acute and chronic temporomandibular disorders: their relation to psychological and sleep impairments. Oral Dis. 2021;27(6):1498–506. https://doi.org/10.1111/odi.13692.
Alvaro PK, Roberts RM, Harris JK. A systematic review assessing bidirectionality between sleep disturbances, anxiety, and Depression. Sleep. 2013;36(7):1059–68. https://doi.org/10.5665/sleep.2810. Published 2013 Jul 1.
Andrews JG, Oei TP. The roles of depression and anxiety in the understanding and treatment of Obstructive Sleep Apnea Syndrome. Clin Psychol Rev. 2004;24(8):1031–49. https://doi.org/10.1016/j.cpr.2004.08.002.
Osiewicz M, Ciapała B, Bolt K, Kołodziej P, Więckiewicz M, Ohrbach R. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD): Polish assessment instruments. Dent Med Probl. 2024;61(1):5–8. https://doi.org/10.17219/dmp/181149. PMID: 38270283.
Acknowledgements
Not applicable.
Funding
No funding related to this study.
Author information
Authors and Affiliations
Contributions
I Cho- Data curation; Formal analysis; Visualization; Validation; Writing-original draft.JH Jo- Formal analysis; Validation; Writing-review & editing.JW Park- Conceptualization; Methodology; Investigation; Data curation; Validation; Resources; Supervision; Project administration; Writing-original draft; Writing-review & editing.All authors approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All methods were performed in accordance with the Declaration of Helsinki and relevant guidelines and regulations. This work was approved by the Institutional Review Board of Seoul National University Dental Hospital (ERI19024). All subjects signed an informed consent form on their first visit approving the usage of their medical records for academic purpose. The need for obtaining further informed consent was waived by the Institutional Review Board based on the retrospective nature of the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cho, IS., Jo, J.H. & Park, J.W. Hematological biomarkers of systemic inflammation in predicting long-term treatment response of temporomandibular disorders. BMC Oral Health 24, 1097 (2024). https://doi.org/10.1186/s12903-024-04862-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12903-024-04862-x