Abstract
Background
Interprofessional assessment and management of health needs for older adults living at home can help prioritize community service resources and enhance health, yet there is a shortage of professionals with the necessary competencies. Therefore, support and training for healthcare professionals in community settings to assess older adults’ health with the aim of for health promotion are needed.
Aim
To identify and provide an overview of published papers describing approaches for training healthcare professionals in assessing physical, mental, and social health needs in older adults living at home.
Method
A systematic literature search of the Cinahl, Medline, Academic Search Ultimate, Scopus, Embase, and British Nursing Index databases was performed. We considered studies focusing on the training of healthcare professionals in assessing a single or multiple health needs of older adults aged 65 and above living at home. We considered studies published between 1990 – and March 2024. The review evaluated qualitative, quantitative, and mixed methods studies published in English-language peer-reviewed academic journals. A quality appraisal was conducted via the Mixed Methods Appraisal Tool (MMAT).
Results
Twenty-three studies focused on training healthcare professionals to assess health needs and plan care for older adults living at home were included. The majority of the included studies combined teacher-driven pedagogical approaches consisting of educational sessions, written materials or e-learning, and more participant-engaging pedagogical approaches such as knowledge exchange or various forms of interactive learning. Healthcare professionals were trained to detect and manage single and multiple health needs, and some studies additionally incorporated interprofessional collaboration. Healthcare professionals were satisfied with the training content and it increased their confidence and competencies in health needs assessment and care planning for older adults. Moreover, some studies have reported that training interventions foster the implementation of new and effective ways of working and lead to positive outcomes for older adults.
Conclusion
Healthcare professionals were satisfied with a combination of participant-engaging and teacher-driven pedagogical approaches used to train them in assessing health needs and planning care for older adults living at home. Such training can lead to enhanced assessment skills and facilitate improvements in practice and health promotion for older adults. Future research is recommended on interprofessional simulation training for conducting structured and comprehensive health needs assessments of older adults living at home, as well as on the implementation of such assessments and health-promoting interventions.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
The globally growing and diverse aging population will impact the sustainability of healthcare systems and the independent living of older adults. To support the health needs of older adults, the World Health Organization (WHO) underscores the necessity of effectively training the healthcare workforce [1, 2]. However, the complexity of health needs in older adults, coupled with an increased risk of frailty and adverse health outcomes, challenges the provision of tailored care [3]. Healthcare professionals in homecare settings are well-positioned to assess the health needs of home-living older adults [4, 5] and facilitate the interprofessional management of these needs within the community [5].
Health needs assessment should offer a comprehensive understanding of individuals’ physical, mental, and social health needs, and address the constantly changing needs with increasing age. The assessments aim to identify those who can benefit from healthcare services, such as health education, disease prevention, treatment, and rehabilitation [6]. The assessment can help set service priorities and allocate service resources effectively, guide clinical decision-making [7] and design targeted, health promoting interventions [4, 7,8,9] to prevent or delay frailty [10], enhance overall outcomes for those with complex health needs [11] and enable them to remain at home for as long as possible [12]. Given its importance, the task of health needs assessment, is becoming increasingly crucial in homecare settings [13]. However, there is a scarcity of adequately trained professionals proficient in conducting interprofessional health needs assessments [4, 5, 9, 14, 15], including depression [16], cognitive function [17], social needs [18], sensory function (i.e. hearing and vision) [19], geriatric healthcare [20, 21], and multidimensional frailty [22, 23]. Frailty, as a dynamic state, affects an individual who experiences losses in one or more domains of human functioning (physical, mental, social) that are caused by the influence of a range of variables, and which increase the risk of adverse outcomes [24].
A comprehensive understanding of how to train healthcare professionals in health needs assessment of the physical, mental, and social health needs of older adults living at home is crucial. This review understands training as “planned and systematic activities designed to promote the acquisition of the knowledge, skills, and attitudes” [25, p77]. Training can take place as “on-the-job training,” with practicing tasks with a mentor or receiving feedback, or through “off-the-job training,” in a classroom setting with lectures, discussions, and exercises [26]. It is essential to consistently update and expand knowledge and skills throughout healthcare professionals’ careers [27]. Mentorship and support are highly valued as pedagogical approaches [28]. Another approach is implementing interprofessional team-based training [29] focused on health needs assessment for older adults, which can be complemented by practical, supervised training with a mentor in real-world settings [9]. Interprofessional simulation training can support healthcare professionals developing communication and collaborative skills and improving patient outcomes [2]. Additionally, opportunities to share and exchange experiences and new learning with peers and seniors, along with tailored, role-focused teaching, are effective approaches training strategies in community healthcare [30]. Practical training through simulation, case studies, and role-playing influences skill development by creating experiences that promote individual understanding and learning [31] and it is based on Vygotsky’s sociocultural learning theory [32]. Tailored simulation training in use of systematic assessment tools enhanced nurses’ competencies to assess and treat complex symptoms among older adults in long-term care facilities [33].
Therefore, this scoping review aimed to identify and provide an overview of published papers describing approaches for training healthcare professionals in assessing physical, mental, and social health needs in older adults living at home. Three research questions guided the review: (1) what pedagogical approaches are used when training healthcare professionals to assess the health needs of older adults living at home, (2) what is the content and foci in the health needs assessment training provided in the studies, and (3) what are the outcomes of training reported by healthcare professionals and older adults living at home?
Methods
Scoping review design
This study followed the Joanna Briggs Institute (JBI) methodology [34] for conducting and reporting scoping reviews built on Arksey and O’Malley’s framework [35]: (1) Define and align the objectives (2) develop and align the inclusion criteria with the objectives (3) describe the planned approach to evidence searching, selection, data extraction, and presentation of the evidence (4) search for the evidence (5) select the evidence (6) extract the evidence (7) analyze the evidence (8) present the results (9) summarize the evidence in relation to the purpose of the review, draw conclusions and note the implications of the findings [36]. In addition, the PRISMA-ScR [37] was used as a checklist to report the scoping review data charting, data synthesis and presentation of the data (Additional file 1).
Selection of studies
To be eligible for inclusion in the review, the study had to focus on the training of healthcare professionals in assessing physical, mental and social health needs [24], specifically assessing frailty, physical function, depression, cognition, social health, and sensory function of older adults aged 65 and above living at home [38]. Healthcare professionals from diverse fields were included, whether engaging in one-to-one interactions where individual healthcare professionals work directly with patients or working collaboratively in interprofessional teams of members from different professional backgrounds [29]. The review included qualitative, quantitative, and mixed methods studies published in English-language peer-reviewed academic journals. The inclusion and exclusion criteria are specified in Table 1 below.
Search strategy
The authors and an experienced research librarian collaboratively developed the search strategy and search terms. The search strategy followed the recommendation of JBI [34]. In June 2022, a limited search of PubMed and CINAHL was conducted to identify relevant articles. To develop a more comprehensive search strategy, we subsequently analyzed the titles and abstracts of the retrieved papers, as well as the index terms used to describe the articles. A systematic literature search was performed on October 6, 2022, in the CINAHL (EBSCO), MEDLINE (EBSCO), Academic Search Ultimate (EBSCO), Scopus (Elsevier), Embase (OVID) and British Nursing Index (ProQuest) databases. The updated search was conducted on the 7th of March 2024. The search terms employed in the different databases to represent training healthcare professionals to assess health needs in older adults living at home are described in Table 2. We considered studies published between 1990 – and March 2024. Ultimately, the reference lists of all included studies were reviewed to identify any additional studies aligned with the scoping review’s aim.
Identification and selection of studies
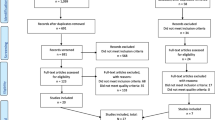
The search yielded a total of 2266 records. The study selection process is illustrated in Fig. 1 according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram [39]. The search results were uploaded into the citation management system EndNote, where duplicates were removed. A total of 1722 records remained for screening. We used the web application Rayyan [40] to screen studies for inclusion or exclusion. The screening involved all the authors working in pairs, independently assessing eligibility on the basis of the inclusion and exclusion criteria. Discrepancies were resolved through discussions until consensus by all authors in arranged meetings.
All the records were independently screened by the authors (BHL, DND, HKF, PD and MS), and 1452 records were excluded. Two hundred seventy abstracts were reviewed in blinded pairs, leading to the exclusion of 212 records. Next, the full texts of 58 studies were read. This process resulted in the exclusion of 38 studies whose reasons are provided in the flow chart. The remaining 20 studies were included in this review (Fig. 1).
The primary reason for exclusion was the lack of content related to training in health needs assessment (n = 13) or incorrect populations (n = 12). Eight studies were excluded because they focused on training for medical or bachelor’s degree students. Additionally, four publications were not peer-reviewed studies (n = 4).
BHL and MS independently screened the reference lists from the 20 included studies to identify additional eligible studies. After all the blinded titles were read, 28 titles of records were identified for abstract review. Following this, 22 titles were excluded, leaving 6 abstracts included in the full-text examination. The full-text reading further excluded four studies because they did not focus on training in health needs assessment. Finally, two studies [41, 42] were added to this scoping review, resulting in a total of 22 included studies.
An updated search was conducted on the 7th of March 2024, including publications from 2022 to 2024, following the procedure above. After removing duplicates, 173 titles and abstracts were screened for eligibility. The full texts of nine articles were read. Six studies were excluded because they did not include training for healthcare professionals. One had incorrect population, and the others were in a language other than English. This led to the inclusion of one new study [43], bringing the total number of included studies for the scoping review to 23.
Search results, study selection and inclusion process [39]
Extraction and analysis of the data
In line with the updated JBI methodological guidelines for scoping reviews [34], we extracted and coded descriptive details from the 23 included records. The extraction table covered the publication year, country of origin, study purpose, research design, study population, context/setting, training intervention content and assessment tools, pedagogical approaches and training duration, and outcomes for healthcare professionals and older adults. A test was conducted to ensure that the coauthors were aligned in their understanding of what type of data to extract for the table. Feedback from the test guided essential refinements to the extraction table before the authors collaborated to extract and organize pertinent information. We applied a basic thematic analysis to code the data and identify, analyze, and interpret patterns, ultimately deriving themes that addressed our research questions [44, 45]. The analysis utilized NVivo 12 Pro software [46].
Quality appraisal
We performed a quality evaluation of the included studies via the Mixed Methods Appraisal Tool (MMAT) in blinded pairs. This tool is designed for a structured and standardized evaluation of methodological quality and risk of bias in systematic reviews that include qualitative, quantitative, and mixed methods studies [47]. Although quality evaluation is optional in a scoping review, it can provide valuable insights [48] and enhance the interpretability of the included studies [49].
All studies were evaluated according to five quality criteria specific to each research design (qualitative, quantitative descriptive, nonrandomized, randomized, and mixed methods studies). Each criterion received a response score of either “Yes,” indicating that the study met the quality criteria, or “No,” indicating that it did not meet the quality criteria or that it was unclear (see Table 4). It is discouraged to calculate an overall score. Any disagreements in scoring were resolved through discussion. The quality scores were not used to exclude articles from the review; instead, they were reported and discussed [49].
Results
In accordance with the JBI scoping review guidance [44], the extracted data are presented in a table format (Tables 3 and 5) and a narrative summary is provided to respond to the three research questions. Table 3 provides a description of the study characteristics, while Table 5 outlines overarching categories along with relevant extracted information [44].
Characteristics of the included studies
Table 3 shows that the 23 studies were published between 1990- and 2023. Eight studies were conducted in the United States [16, 42, 43, 50,51,52,53,54], three in Canada [55,56,57], three in Australia [58,59,60], three in the United Kingdom [41, 61, 62], and one each in Ireland [63], Italy [64], Brazil [65], France [66], Singapore [67], and Belgium [68].
Ten studies meticulously examined training interventions tailored for primary nurses [43, 50, 51, 54, 55, 60, 61, 63, 66, 68], one study specifically targeted the training of community health workers [65] and another presented an educational session tailored for case managers and agency supervisors [42]. The remaining studies indicated that training was provided to interprofessional teams or various distinct professions, such as nurses, physical therapists, occupational therapists, general practitioners, social workers and psychologists [16, 41, 52, 53, 56,57,58,59, 62, 64, 67]. The study participants were in home healthcare or primary/community care [16, 41, 43, 50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66, 68], community and social services [42, 64], mental health care [61], eldercare centers/daycare [67], residential settings [58, 59, 64], hospitals [53, 56], rehabilitation [56] and acute care [61].
Quality evaluation results
The quality appraisal procedure revealed variations in the quality of the 23 included studies. The detailed quality evaluation results for each study are presented in Table 4, and an overview of the methodological quality criteria is presented in Additional file 3.
Each study was evaluated on five criteria appropriate to its study design category. Overall, only one study, which was a mixed methods study, met al.l five quality criteria in the MMAT [62]. Additionally, one mixed methods study met four criteria [61], and another met three criteria [65]. The most common criterion that mixed methods studies failed to meet was 5.2: whether the different components of the study were effectively integrated to answer the research question. Among the quantitative randomized studies, one study met four quality criteria [50], whereas the other was of low quality, meeting only one criterion [59]. None of these studies met the quality criterion for proper randomization. In the quantitative nonrandomized studies, six met four criteria [41, 55, 56, 58, 64, 68], one met three [63], and one met only one criterion [16], indicating low quality. All studies met the criterion regarding whether the intervention was administered as intended. The most common criteria they failed to meet were 3.3: whether there were complete data and 3.4: whether confounders were accounted for in the study design and analysis. Among the descriptive studies, seven met four criteria [42, 43, 54, 57, 60, 66, 67], one met three criteria [53], and two met only one criterion [51, 52], demonstrating low quality.
The majority of these studies met the criterion regarding whether the measurements were appropriate. However, the criterion most studies did not meet (only one out of ten) was whether the risk of nonresponse bias was low. Notably, no qualitative methods studies were included in our scoping review.
Training interventions in assessment of older adults living at home
The next section presents a narrative overview of three major themes related to the three research questions. The themes concerned the training provided for healthcare professionals in assessing the physical, mental, and social health needs of older adults living at home: pedagogical approaches, content and foci of health needs assessment training for healthcare professionals and outcomes and evaluation of health needs assessment training for healthcare professionals and older adults living at home. The findings are summarized in Table 5 [44].
Pedagogical approaches
The included studies employed diverse pedagogical approaches to train healthcare professionals in assessing the health needs of older adults living at home. The spectrum of pedagogical approaches observed in the studies was categorized into teacher-driven and participant-engaging pedagogical approaches. Twenty-one studies [16, 42, 43, 50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65, 67, 68] combined teacher-driven and participant-engaging pedagogical approaches, reflecting a multifaceted training strategy. Mayall et al. [41] opted for a more singular pedagogical approach, exclusively relying on lecture-based education, whereas the training method used in the Piau et al. [66] study remained unspecified. The training interventions varied in duration, from one-hour sessions [68] to an ongoing training program spanning 21 months [57]. In two studies, the specific duration of the training interventions was not specified [53, 57]. The most common duration for training was 4–8 h [16, 43, 50, 52, 54, 56, 58, 59, 62, 67].
Teacher-driven pedagogical approaches
Almost all studies utilized teacher-driven pedagogical approaches, including educational sessions, written materials or e-learning [16, 41, 42, 50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65, 67, 68]. Educational sessions were evident in 14 studies [16, 41, 42, 50,51,52,53, 56,57,58,59, 62, 64, 65], providing healthcare professionals with information about relevant topics through lectures [16, 41, 42, 51, 62, 64, 65], slides [16, 64] and instructions [50, 52, 53], as well as demonstrations of the use of assessment tools [41, 42, 51, 56, 58, 59]. Additionally, Abbasi et al. [57] and Quijano et al. [42] offered ongoing sessions during the post training implementation period.
Written materials were provided to the participants in nine studies [16, 42, 50, 52, 54, 58, 59, 63, 64]. This included training manuals containing examples and case studies [58, 59], written documents about the training pack and the assessment forms [63], course textbooks and instruction manuals [64], educational materials including the program manual and articles [42], a CD-ROM (a data-disc for computer) containing written educational material [52] and toolkits derived from the educational material [16, 50, 54]. Brown et al. [54] reported that toolkits included key intervention components for seamless application of learned concepts [54]. Furthermore, some described follow-up emails to provide participants with information post training [50, 54].
E-learning as a preplaying online module or videoclip appeared in nine studies [16, 42, 43, 50, 53, 54, 61, 64, 68]. Naughton et al. [61] delivered prerecorded lectures [61], Landi et al. [64] used video recordings presenting real cases to test participants’ assessments- and decision-making skills, and Quinlan and Ryer [43] offered online modules on aging epidemiology, fall risk factors, and age-friendly health systems [43]. Participants watched video recordings portraying late-life depression [42, 53, 54], and patient interactions illustrating approaches to depression assessment [50, 54, 68] via standardized questions and follow-up questions [16]. Professional actors were used in three studies [16, 53, 68].
Participant-engaging pedagogical approaches
The majority of the included studies utilized participant-engaging pedagogical approaches involving knowledge exchange or various forms of interactive learning [16, 42, 43, 50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65, 67, 68].
Sixteen studies employed various forms of knowledge exchange such as discussion, questioning and coaching, between training participants and teachers [43, 51,52,53,54,55,56, 58,59,60,61, 63,64,65, 67, 68]. Peer-to-peer learning and dialog facilitated the exchange of knowledge and insights [65], which enriched the overall learning experience [61]. The participants were included in discussions following lectures [55], after watching scripted videos [53], and during patient case reviews [56, 67]. Additionally, three studies included both discussions and allowed participants questions [52, 54, 68]. Discussions allowed participants to delve into case management techniques [51], explore experiences related to assessing the health of older adults [54, 60, 64] and solve problems and discuss alternative strategies regarding depression screening [54]. A few studies have provided ongoing coaching in the post training phase to support healthcare professionals in applying newly acquired skills [42, 55, 57]. This included three months of feedback and support [42], mentorship for skill integration [57], and a six-month collaborative approach between resource staff and case managers involving home visits and clinical consultations [55].
Interactive training was employed in fifteen studies through skills training, role-playing, simulations, and hands-on training in real-world settings [16, 42, 43, 51, 52, 54, 55, 57,58,59,60, 62,63,64,65]. Skill training allows nurses to practice patient interviews and assessments and receive instructor feedback [54]. The participants practiced by assessing their colleagues’ health and responding to assessment [16, 51], with faculty staff offering assistance, encouragement, and feedback throughout [51]. Landi et al. [64] provided practice exercises followed by presentations, and Quinlan and Ryer [43] provided a virtual training session in motivational interviewing technique and assessment. Roleplay as a teaching strategy was used to address practical aspects of administering depression screening [50, 52, 60], and Butler and Quayle [63] incorporated case scenarios, roleplay, and practical skills training for assessing depression in older adults [63]. Simulation training was used to immerse participants in the experience of living with sight and hearing impairments performing everyday tasks such as filling out forms or managing medications using sight impairment spectacles. Training was followed by a debriefing session [62]. Hands-on training in the assessment of older adults’ health in real-world settings was conducted in ten studies [42, 51, 54, 55, 57,58,59,60, 64, 65]. Healthcare professionals gained clinical experience through assessments of home dwelling older adults [55, 58,59,60, 64, 65] and through participation in a rotational preceptorship for community health nurses. This enabled them to practice newly acquired assessment skills and collaborate in a real-life setting [51]. Additionally, two other studies emphasized practical training in communication with other professionals in real-world settings [58, 59], while Brown et al. [54] encouraged participants to practice assessments in a real-world setting between educational sessions.
Content and foci of health needs assessment training for health care professionals
All the included studies offered insights into the content and foci of health neesd assessment training interventions for healthcare professionals. The studies were divided into those aimed at training healthcare professionals to understand and assess either single or multiple physical, mental, and social health needs in older adults living at home. Additionally, some training sessions focused on interprofessional collaboration.
Single health need assessment training
The focus of twelve studies involved enhancing the skills of healthcare professionals in assessing, planning and conducting interventions for a specific, single health need in older adults, with each addressing either the assessment of mental or physical health [16, 41, 43, 52,53,54, 58,59,60, 62, 63, 68]. Two of these studies [43, 62] focused solely on physical health factor training. Smith et al. [62] emphasized training in assessing and detecting sight and hearing impairments without specifying whether any assessment tools were used [62]. Quinlan and Ryer [43] provided fall risk assessment training, which included the use of assessment tools to evaluate the physical function of older adults and to assess their home environments. The other ten studies [16, 41, 52,53,54, 58,59,60, 63, 68] focused on training to assess depression in older adults living at home. The training encompassed understanding and detecting the condition, and all of them included the use of assessment tools. Van Daele et al. [68] included skills such as actively listening to patients and motivating them to seek expert assistance when needed. Delaney et al. [16] incorporated skills in asking follow-up questions, and Mellor et al. [59] offered training in appropriate communication with older adults to identify masked, early signs of depression.
Multiple health needs assessment training
Eleven studies [42, 50, 51, 55,56,57, 61, 64,65,66,67] described training interventions for healthcare professionals aimed at assessing, planning, and conducting interventions for multiple health needs in older adults living at home. The training content ranged from learning to performing a holistic health assessment of older adults encompassing physical, mental, cognitive, and social factors [42, 51, 55,56,57, 61, 64, 66] to a more nuanced assessment of two or three of these factors [50, 65, 67]. All studies described the use of assessment tools or checklists. A holistic assessment and understanding of older adults’ health context and needs enables interventions to be tailored to their health and care needs, priorities, and levels of frailty [57]. Within the realm of holistic assessment, only two of these studies addressed alcohol and medication usage [55, 56], whereas two other studies focused on evaluating sensory status [57, 66]. For studies with more nuanced assessment training, three studies [42, 50, 67] primarily tailored their training to focus on depression assessment and intervention in older adults, but Quijano et al. [42] also included training in assessing general physical health status, social function, and cognitive function. Sin et al. [67] included dementia assessment and Bruce et al. [50] addressed factors that commonly complicate depression in homecare patients, such as health conditions, disability in activities of daily living, and cognitive function. The training included how to ask follow-up questions and observe nonverbal language [50]. Neto et al. [65] provided training for healthcare professionals in rural areas to screen for geriatric risk factors such as caregiver overburden, general health, social health, risk of falling, or difficulties in activities of daily living.
Interprofessional collaboration and communication skills in health needs assessment training
Beyond the focus on training for assessing the health needs of older adults, sixteen studies [42, 50,51,52,53,54,55, 57,58,59,60,61,62, 64, 65, 68] have incorporated training elements to increase interprofessional collaboration and communication skills among healthcare professionals. Health needs assessment training for interprofessional teams was evident in eight of the included studies [51, 55, 57,58,59, 61, 64, 65]. Two studies [58, 59] outlined an advanced session to teach skills for interacting with other healthcare providers, including general practitioners and mental health specialists, whereas Couser et al. [51] stressed the importance of effectively communicating the assessment results to physicians and other healthcare providers. Training in writing referrals was emphasized in ten studies [42, 50, 52,53,54, 58,59,60, 62, 68]. In addition, Stolee et al. [55] trained healthcare professionals in writing reports and making recommendations to the referring case manager. Only two studies [61, 65] included collaboration with family in their training programs. Naughton et al. [61] designed training programs to support healthcare professionals in navigating the complexities of collaboration with multidisciplinary teams, older adults, and their families. They also developed a network among nurses to facilitate the exchange of expertise, experience, and innovative ideas [61]. Neto et al. [65] aimed to increase the capacity of care workers to effectively collaborate with family caregivers and social services for dependent older adults in rural areas. Stolee et al. [55] provided training for case managers to extend this knowledge to their teams and strengthen connections with specialized geriatric services. Similarly, Abbasi et al. [57] emphasized team-based care delivery training, with active and holistic discussions among patients, caregivers, and interprofessional teams. Diverse skill sets within teams can effectively meet the holistic care needs of patients. In parallel, Piau et al. [66] focused on training nurses to collaborate with general practitioners to develop comprehensive care plans. Landi et al. [64] trained case managers who collaborated in supervised teams to assess older adults and present care plans. They watched videos of simulated team discussions to enhance their understanding of the assessment process and teamwork [64].
Evaluation and outcomes of health needs assessment training for healthcare professionals and older adults
All of the studies provided insight into the experiences or outcomes of healthcare professionals participating in the training interventions. This included their satisfaction and experiences with health needs assessment training, improved confidence and competencies in health assessment and care planning and shifts in work practices. Additionally, some studies have reported outcomes for older adults following health needs assessment training, such as appropriate referrals, tailored interventions, fall prevention, symptom reduction, and improved overall function. The evaluation of these outcomes relied to a small extent on models or frameworks, with only three studies incorporating them [43, 61, 62]. Smith et al. [62] utilized Kirkpatrick’s four-level training evaluation model to assess the relevance and impact of educational intervention. Naughton et al. [61] adopted Alvarez et al.’s (2004) framework of an integral model of training evaluation and effectiveness. Quinlan and Ryer [43] presented their findings following the Revised Standards for Quality Improvement Reporting Excellence (SQUIRE) framework.
Healthcare professionals’ satisfaction and experiences with assessment training
Ten studies provided insights into healthcare professionals’ experiences with participating in training interventions [16, 41, 43, 54,55,56, 60,61,62, 65], where most of the participants expressed satisfaction with both the content and format of the courses. The participants in Brymer, Cormack and Spezowka [56] expressed a high level of satisfaction with the presenter’s content, pacing, and format, and in Mayall et al. [41], the training met the participants’ needs and expectations. The participants in Naughton et al. [61] particularly valued the peer-to-peer learning aspect, whereas Smith et al. [62] emphasized the effectiveness of simulations. Neto et al. [65] rated classroom sessions and supervised home visits very positively and found them useful. Furthermore, participants in four of the studies [16, 60, 61, 65] offered suggestions to enhance the number of educational sessions. They suggested allocating more time for training [16, 65], a greater focus on skills training [60, 61], additional training in managing complex and technically challenging issues [65] and incorporating more time for case studies and discussions [16].
Improved confidence and competence in health assessment and care planning
Improvements in assessment competencies following training interventions among healthcare professionals were reported in nineteen studies [16, 41, 42, 51, 52, 54,55,56,57,58,59,60, 62,63,64,65,66,67,68]. Among these, nine studies explicitly reported increased confidence among healthcare professionals in assessing older adults’ health needs [16, 41, 54, 55, 58, 59, 63, 67, 68]. The health need sassessment and use of assessment tools or checklists led to the identification of health needs. Quinlan and Ryer [43] noted that without screening in a fall prevention program, the identification of fall risk among older adults would be missed. Piau et al. [66] noted that a high proportion of assessments effectively identified frailty and suggested interventions and referrals. One comment was that they “were previously skirting around the problem, now asked about mental health directly” [61, p. 33]. Naughton et al. [61] reported that performing a comprehensive geriatric assessment helped when raising issues with general practitioners because they were talking about their language. Nunn, Annells and Sims [60] acknowledged the use of Geriatric Depression Screening (GDS) tool raised awareness of depression. A total of 62.5% felt that the GDS helped identify depression that might otherwise be overlooked, but some questioned its universal usefulness [60]. Abbasi et al. [57] reported that having an evaluation framework helped healthcare professionals guide meaningful measures [57]. Conversely, some participants also expressed that they relied more on observation than direct questions when assessing depression [54]. According to Landi et al. [64], careful assessments is deemed essential for effective care planning, and Stolee et al. [55] emphasize the critical role of assessment training in identifying health needs and equitably distributing community service resources. Two studies reported one year of retention of knowledge and skills without the inclusion of a refresher course [54, 62].
Twenty studies documented a better understanding of appropriate interventions and referrals [16, 41, 42, 50,51,52,53, 55, 57,58,59,60,61,62,63,64,65,66,67,68]. According to Delaney et al. [16], 50% of the participants noted that a key aspect they learned was understanding the significance of the assessment results and the corresponding interventions [16]. The participants in the study by Neto et al. [65] demonstrated significantly improved capacity in responding to the health and care needs of older adults. The participant reported increased confidence in making referrals and consulting resources [51], increased knowledge about managing depression, making referrals, and accessing available local services [41] and enhanced self-efficacy in providing care for older adults [16, 58]. Nunn, Annells and Sims [60] reported that 50% of participants felt prepared to address older adults’ depression after training. Smith et al. [62] observed increased referral practices and improved ability to advise patients about sensory services, whereas Mellor et al. [59] noted a slight increase over time in specialist referrals, and senior staff reported increased confidence in interacting with health specialists.
Shift in healthcare professionals’ work practices after assessment training
The training intervention resulted in either a change or potential for change in work practices in ten studies [16, 42, 43, 52, 53, 55, 57, 62,63,64]. Butler and Quayle [63] reported that prior to receiving training, nurses did not utilize any formal assessment measures to screen for depression in older adults. However, following training, some nurses continue to use screening measures for depression in their clinical practice [63]. Similarly, case managers in Stolee et al. [55] stated that the major change in their assessment practice was greater consistency in the use of assessment tools. Smith et al. [62] reported a shift in practice toward incorporating more detailed information about patients’ impairments and implementing supportive strategies, and in Marcus et al. [53], communication of depression screening results to patients, physicians, or mental health specialists became a standard protocol.
Landi et al. [64] reported that training was proven feasible and may be implemented on a broader scale, and Luptak et al. [52] outlined an implementation period of the ADAPT—Assuring Depression Assessment and Proactive Treatment protocol for depression care in rural healthcare—with the potential to achieve the outlined goals in various clinical settings [52]. Delaney et al. [16] reported that project participants were interested in implementing the program in their homecare setting and developed a train-the-trainer model. Abbasi et al. [57] provided results and experiences regarding the Seniors Community Hub (SCH) through the ADKAR (awareness, desire, knowledge, ability, reinforcement) evaluation framework to assist others interested in implementing a similar integrated care model [57]. Quinlan and Ryer [43] stated that fall assessment practices are currently implemented and continuous; similarly, Quijano et al. [42] reported that depression interventions continue to be offered by participating agency offices. On the other hand, Butler and Quayle [63] noted the challenge of implementing assessment tools due to competing demands such as holidays, working part-time or being too busy, and Sin et al. [67] outlined one participant with difficulties in applying new knowledge owing to manpower shortages and constraints in time and space.
Outcomes for older adults following the health needs assessment training
Seven studies [42, 43, 50, 53, 57, 66, 68] detailed outcomes for older adults following health needs assessment training for healthcare professionals. These outcomes included appropriate referrals, tailored interventions, fall prevention, symptom reduction, and improved overall function. Bruce et al. [50] highlighted that depressed older adults in the intervention group were more likely to receive appropriate referrals for mental health evaluation [50], aligning with findings where a minimal intervention significantly increased the detection of depression and further referrals to general practitioners [68]. The findings in two studies demonstrated that patients were referred to tailored resources designed to address their identified problems [53, 57]. Furthermore, Quijano et al. [42] revealed that older adults’ awareness of seeking help and the significance of physical activity for maintaining health improved. Quinlan and Ryer [43] stated that after providing care plans to 83 older adults, most implemented fall prevention strategies during a two-week follow-up call with 29 older adults, with only one fall reported. Piau et al. [66] identified the main causes of frailty and reported effective intervention recommendations and referrals [66]. Most physicians in Stolee et al. [55] reported better general function for older adults due to comprehensive geriatric assessment. Findings in two studies [42, 57] documented reductions in depression severity at the follow-up assessment due to appropriate referrals and interventions [42, 57], and significantly more older adults felt better and experienced pain reduction, followed by increased activity [42]. Additionally, Abbasi et al. [57] reported a slight improvement in health-related quality of life, including mobility, usual activities, pain/discomfort, and anxiety and depression, suggesting enhanced function [57].
Discussion
This scoping review provides insights into training interventions for healthcare professionals assessing the physical, mental, and social health needs of older adults living at home. The analysis of 23 studies revealed that nearly all training interventions used a multifaceted training strategy combining teacher-driven and participant-engaging pedagogical approaches to teach healthcare professionals theoretical and practical knowledge. Health needs assessment training focuses on the skills needed to conduct single or multiple health needs assessments in older adults. Interprofessional collaboration was an essential part of most training interventions. Multiple studies noted that participants were satisfied with the training content and had increased confidence and competencies in health needs assessment and care planning. Studies have also reported a shift in work practices for health care professionals and some included results have shown improved health outcomes for older adults.
Our study revealed that most of the included studies blended the use of teacher-driven and participant-engaging pedagogical approaches [16, 42, 43, 50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65, 67, 68]. These approaches provide participants with confidence and competencies in health needs assessment [16, 41, 42, 51, 52, 54,55,56,57,58,59,60, 62,63,64,65,66,67,68]. Skilled healthcare professionals are crucial in facilitating the implementation of health assessments for older adults [69]. Lectures can be highly effective for learning, especially when they stimulate thinking and active engagement. Their effectiveness depends on the lecturer’s skill and can be improved by incorporating learner feedback, performance results, self-reflection, and peer feedback [70]. Another way to improve lecture quality is by including interactive elements such as practical skill training, following John Dewey’s “learning by doing” philosophy [32]. In our review, we identified fifteen studies that utilized participant-engaging approaches such as skills training, role-playing, simulations, hands-on training in real-world settings [16, 42, 43, 51, 52, 54, 55, 57,58,59,60, 62,63,64,65], and sixteen studies employed discussion, questioning and coaching [43, 51,52,53,54,55,56, 58,59,60,61, 63,64,65, 67, 68]. The integration of teacher-driven sessions, interactive training, and knowledge exchange resembles simulation training, which typically includes briefing, simulation exercises, and debriefing phases. These phases allow participants to reflect, enhance their learning, and deepen their educational experience [71]. Debriefing is a valuable tool for reflecting on and discussing experiences in training and real-world settings. This helps individuals and teams identify strengths, areas for improvement, and lessons learned, thereby enhancing learning and future performance [72]. However, effective debriefing relies on facilitators with strong skills to maximize learning outcomes [73].
The WHO advocates interprofessional simulation training to enhance healthcare professionals’ competencies and improve patient outcomes [2]. Even if several studies combined teacher-driven approaches, interactive training and knowledge exchange, our review included only one study utilizing simulation training [62]. Health needs assessment training for interprofessional teams was evident in eight of the studies included in our review [51, 55, 57,58,59, 61, 64, 65]. Such training has been proven to provide valuable insights into the health of older adults, leading to improved care delivery [74, 75], improved patient outcomes [76] and reduced hospitalization [74]. It can improve conflict management skills and team functioning [76] and play a critical role in equitably distributing community service resources [55]. Interprofessional simulation training is an engaging method for training clinical skills, procedures, teamwork, and communication in a safe, realistic environment [77]. It promotes critical thinking, reflection [78], and effective learning [79] enhancing the application of knowledge in clinical practice [80]. The use of participant engaging pedagogical approaches aligns with the sociocultural view of training, which emphasizes active engagement and collaboration in the learning process. It enables knowledge exchange and reflection, and participants can integrate their experiences with new information, internalize it, and construct new knowledge [32, 81]. Practical training such as simulations, can push participants out of their comfort zones, foster collaborative learning and enrich the educational experience [82]. However, to achieve optimal learning, it is crucial to balance skill development with an appropriate level of challenge as learners acquire new concepts. At the same time, temporary support from more experienced learners should be available. This balance is known as the zone of proximal development, which represents the space between a learner’s current skill level and their potential skill level with guidance. Tasks within this zone promote growth [83].
Our review reports a distinction in training content with a focus on assessing single versus multiple health needs in older adults. Ten studies [16, 41, 52,53,54, 58,59,60, 63, 68] focused solely on assessing depression. There is a strong correlation between late-life depression and reduced quality of life, as well as comorbidities such as physical illness, disability [58, 84] and physical frailty [85, 86]. However, single health need assessment training may inadvertently lead to the overlooking of broader health needs among older adults. A multiple health assessment of older adults is recommended [7], as it can serve as the foundation for developing holistic interventions to enhance overall health [10, 12, 87,88,89], promote health [90], foster positive health behaviors [91], and reduce frailty [92, 93]. Our review included eight studies [42, 51, 55,56,57, 61, 64, 66] providing training in physical, cognitive, mental, and social health needs assessment, alongside care planning on the basis of these assessments. Research indicates that both healthcare professionals and frail older adults participating in an interdisciplinary care approach were satisfied with the improved structure of care and appreciated the emphasis on health promotion [94]. On the other hand, a comprehensive health needs assessment is a multifaceted and complex intervention, with uncertainties surrounding its effectiveness and underlying mechanisms [95]. Some research findings indicate that there is no conclusive evidence that it reduces disability, prevents functional decline [96], impacts mortality, or supports independent living in older adults [97]. These results underscore the complexity and challenges in conducting and implementing comprehensive health needs assessments and tailoring interventions to promote health in older adults.
Our review revealed that almost all [16, 41,42,43, 50,51,52,53,54,55,56,57,58,59,60,61, 63,64,65,66,67,68] health needs assessment training programs included the use of assessment tools or checklists, leading to the identification of health needs. Only one of these studies reported that participants relied more on observation than on direct questioning when assessing depression [54]. Additionally, another study found that healthcare professionals using assessment tools felt that this approach led to asking overly personal and intrusive questions without first establishing trust or explaining the purpose of the assessment [98]. On the other hand, some older adults reported that using assessment tools made it difficult to discuss issues outside the predefined domains of the comprehensive health needs assessment [99]. Research indicates that current assessment practices heavily rely on professional judgment and intuition, and healthcare professionals in community settings often lack adequate knowledge and training regarding the health needs assessment of older adults [22, 100]. This can be seen as problematic because these professionals are ideally positioned to assess older adults early in their health trajectories [105]. Proper assessment in these settings can facilitate the early recognition of functional decline [101, 102] and vulnerability, enable timely intervention to mitigate frailty’s adverse effects [105], and support effective care planning [64]. Even if several healthcare professionals have endorsed the integration of frailty assessment tools into primary care [22], they need a simple, efficient assessment tool [105] that empowers them to identify older adults’ health needs [9, 88, 103, 104]. This is particularly critical due to the essential role that assessments play in equitably distributing community service resources [105]. As such, this review underscores the importance of educating healthcare professionals in community care to effectively assess the physical, mental, and social health needs of older adults. Furthermore, understanding the learning process of healthcare professionals [78], evaluating the effects of training [106], and establishing evidence-based standards for skills training are crucial for high-quality teaching [107]. Additionally, further research is necessary to assess the feasibility, effectiveness, and acceptability of interprofessional interventions targeting multiple health needs aimed at health promotion [90] and experiences using comprehensive health assessment tools [108].
Methodological considerations
This review included studies employing various methods to obtain comprehensive insights into training healthcare professionals in assessing the health needs of older adults living at home [47]. We utilized a validated mixed-methods appraisal tool to assess the quality of the included studies [47, 49]. We did not include reporting on screening questions regarding the clarity of the research question or whether the collected data addressed the research questions, as our review focused exclusively on empirical studies. Additionally, we chose not to calculate an overall score from the ratings of each criterion, as this practice is discouraged. We provide an overview of each study’s quality by presenting the ratings of each criterion [49]. Our findings revealed that only one study met all the quality criteria, fifteen studies met four criteria, three studies met three criteria, and four studies met only one criterion. High-quality studies employ rigorous and robust methods, leading to reliable and valid findings [109]. While most studies met 3–4 quality criteria, they provide a relatively strong evidence base and offer valuable insights, although some concerns remain. Several studies did not meet the quality criteria for nonresponse bias or complete outcome data. It is crucial to describe and evaluate a low response rate for its potential impact, as this can limit the generalizability of findings [110]. Many studies also failed to account for confounders in their design and analysis. Confounding factors may bias results by distorting the interpretation of findings [49], masking actual associations or creating false associations, potentially leading to incorrect conclusions [111]. The randomization of study subjects and rigorous statistical analyses can mitigate the impact of confounding variables [112]. Nonetheless, conducting a quality assessment increases awareness of these biases and limitations, thereby enhancing our confidence in the study findings.
Strengths and limitations
Our scoping review has several limitations. Initially, our search strategy involved the use of six databases and various relevant search terms related to training healthcare professionals in assessing the health needs of older adults. We excluded gray literature to focus on mapping existing published research and identifying any research gaps. The search was conducted by an experienced librarian. Despite our efforts to comprehensively map the research literature, we may have overlooked some studies. Second, our exclusion criteria, which encompassed, for example, general practitioners, students, and institutional settings, restricted the scope of the study. Additionally, we focused on health needs assessment, excluding studies that assessed the environment, an important factor in enabling older adults to stay at home as long as possible. However, based on the findings and limitations of the included studies, we believe our review provides valuable insights into the research context. These findings can inform future research, practice, policymaking, and the development of training programs for healthcare professionals in community settings to assess older adults’ health needs.
Conclusion
Healthcare professionals require training in assessing physical, mental, and social health needs in older adults living at home to ensure tailored interventions that enhance their health and independence. Our study revealed that healthcare professionals were satisfied with the combination of participant-engaging and teacher-driven pedagogical approaches when training in physical, mental, and social health needs assessment. Such training is beneficial and strengthens healthcare professionals’ confidence and competency in assessment and care planning for older adults living at home. Additionally, some studies reported that following health needs assessment training, there was a shift in work practices and improved health outcomes for older adults. We suggest that health needs assessment training programs are valuable for improving health and care for older adults living at home and contribute to increased sustainability in healthcare.
Furthermore, we propose additional research on interprofessional simulation training for the structured assessment of multiple health needs in older adults, ensuring comprehensive coverage of all significant health issues in these assessments. We also recommend research on the implementation of such assessments and health promoting interventions.
Data availability
No datasets were generated or analysed during the current study.
References
Avallone M, Perweiler E, Pacetti S. Using the 4Ms framework to teach geriatric competencies in a community clinical experience. Nurs Forum [Internet]. 2021; 56(1):[83 – 8 pp.]. https://doi.org/10.1111/nuf.12511
World Health Organization W. Transforming and scaling up health professionals’ education and training. World Health Organization guidelines 2013. Geneva: World Health Organization; 2013. p. 122.
World Health Organization W. Ageing and health Geneva: World Health Organization, WHO. 2022 [ https://www.who.int/news-room/fact-sheets/detail/ageing-and-health
Thiyagarajan JA, Araujo de Carvalho I, Peña-Rosas JP, Chadha S, Mariotti SP, Dua T et al. Redesigning care for older people to preserve physical and mental capacity: WHO guidelines on community-level interventions in integrated care. PLoS Med [Internet]. 2019; 16(10):[e1002948-e pp.]. https://doi.org/10.1371/journal.pmed.1002948
World Health Organization W. Integrated care for older people (ICOPE): Guidance for person-centred assessment and pathways in primary care Geneva. World Health Organization,;; 2019. (WHO/FWC/ALC/19.1).
Wright J, Williams R, Wilkinson JR. Development and importance of health needs assessment. Bmj [Internet]. 1998; 316(7140):[1310-3 pp.]. https://doi.org/10.1136/bmj.316.7140.1310
Ravaghi H, Guisset A-L, Elfeky S, Nasir N, Khani S, Ahmadnezhad E, Abdi Z. A scoping review of community health needs and assets assessment: concepts, rationale, tools and uses. BMC Health Services Research [Internet]. 2023; 23(1):[44 p.]. https://doi.org/10.1186/s12913-022-08983-3
Karlsson S, Ridbäck A, Brobeck E, Norell Pejner M. Health Promotion Practices in Nursing for Elderly Persons in Municipal Home Care: An Integrative Literature Review. Home Health Care Management & Practice [Internet]. 2020; 32(1):[53–61 pp.]. https://doi.org/10.1177/1084822319863308
Schain A, Rees C, Medina C, Eyler R, Glenney S, Rodko E et al. Reducing Risks for Older Adults With an Interprofessional Community-Academic Partnership: A Case Study. Home Healthc Now [Internet]. 2018; 36(6):[362-8 pp.]. https://doi.org/10.1097/nhh.0000000000000696
van Assen MALM, Helmink JHM, Gobbens RJJ. Associations between lifestyle factors and multidimensional frailty: a cross-sectional study among community-dwelling older people. BMC Geriatrics [Internet]. 2022; 22(1):[1–13 pp.]. https://doi.org/10.1186/s12877-021-02704-x
Kennedy MA, Hatchell KE, DiMilia PR, Kelly SM, Blunt HB, Bagley PJ et al. Community health worker interventions for older adults with complex health needs: A systematic review. Journal of the American Geriatrics Society [Internet]. 2021; 69(6):[1670-82 pp.]. https://doi.org/10.1111/jgs.17078
de Carvalho IA, Epping-Jordan J, Pot AM, Kelley E, Toro N, Thiyagarajan JA, Beard JR. Organizing integrated health-care services to meet older people’s needs. Bull World Health Organ [Internet]. 2017; 95(11):[756 – 63 pp.]. https://doi.org/10.2471/BLT.16.187617
Rusli KDB, Tan AJQ, Ong SF, Speed S, Lau Y, Liaw SY. Home-based nursing care competencies: A scoping review. Journal of Clinical Nursing [Internet]. 2023; 32(9–10):[1723-37 pp.]. https://doi.org/10.1111/jocn.16169
World Health Organization W. Integrated care for older people (ICOPE) Geneva: World Health Organization, WHO. 2024 [ https://www.who.int/teams/maternal-newborn-child-adolescent-health-and-ageing/ageing-and-health/integrated-care-for-older-people-icope
Adhikari P. Geriatric health care in India -Unmet needs and the way forward. Archives of Medicine and Health Sciences [Internet]. 2017; 5:[112 p.]. https://doi.org/10.4103/2321-4848.208215
Delaney C, Fortinsky RH, Doonan L, Grimes RLW, Terra-Lee P, Rosenberg S, Bruce ML. Depression Screening and Interventions for Older Home Health Care Patients: Program Design and Training Outcomes for a Train-the-Trainer Model. Home Health Care Management & Practice [Internet]. 2011 2011/12/01; 23(6):[435 – 45 pp.]. https://doi.org/10.1177/1084822311405459
Briskie Semeniuk P, Bier N, Couture M, Vachon B, Belchior P. Perceived knowledge needs of occupational therapists for evaluating seniors with cognitive impairments. Physical & Occupational Therapy in Geriatrics [Internet]. 2023; 41(4):[515 – 37 pp.]. https://doi.org/10.1080/02703181.2023.2180566
Galvez-Hernandez P, González-de Paz L, Muntaner C. Primary care-based interventions addressing social isolation and loneliness in older people: a scoping review. BMJ Open [Internet]. 2022; 12(2):[e057729-e pp.]. https://doi.org/10.1136/bmjopen-2021-057729
Mathisen TS, Eilertsen G, Ormstad H, Falkenberg HK. Barriers and facilitators to the implementation of a structured visual assessment after stroke in municipal health care services. BMC Health Services Research. 2021;21(1):497. https://doi.org/10.1186/s12913-021-06467-4
Li S, Zhang J, Liu Y, Wang A-P, Qiu G. Survey of the demand for care services for older people and the training needs of their care workers: a cross-sectional study in Northeast China. BMC Nurs [Internet]. 2022; 21(1):[25- pp.]. https://doi.org/10.1186/s12912-022-00809-1
Fulmer T, Reuben DB, Auerbach J, Fick DM, Galambos C, Johnson KS, Actualizing Better Health And Health Care For Older Adults. Health Affairs [Internet]. 2021; 40(2):[219 – 25 pp.]. https://doi.org/10.1377/hlthaff.2020.01470
Kennedy F, Galvin R, Horgan NF. Managing frailty in an Irish primary care setting: A qualitative study of perspectives of healthcare professionals and frail older patients. Journal of Frailty, Sarcopenia & Falls [Internet]. 2021; 6(1):[1–8 pp.]. https://doi.org/10.22540/JFSF-06-001
Frost R, Robinson K, Gordon AL, Caldeira de Melo R, Villas Boas PJF, Azevedo PS et al. Identifying and Managing Frailty: A Survey of UK Healthcare Professionals. Journal of Applied Gerontology [Internet]. 2023; 43(4):[402 – 12 pp.]. https://doi.org/10.1177/07334648231206321
Gobbens RJ, Luijkx KG, Wijnen-Sponselee MT, Schols JM. Toward a conceptual definition of frail community dwelling older people. Nursing Outlook [Internet]. 20102010/03/01/; 58(2):[76–86 pp.]. https://doi.org/10.1016/j.outlook.2009.09.005
Salas E, Tannenbaum SI, Kraiger K, Smith-Jentsch KA. The Science of Training and Development in Organizations:What Matters in Practice. Psychological Science in the Public Interest [Internet]. 2012; 13(2):[74–101 pp.]. https://doi.org/10.1177/1529100612436661
Armstrong M, Taylor S. Armstrong’s handbook of human resource management practice: A guide to the theory and practice of people management. Kogan Page; 2023.
World Health Organization W. Building a skilled health workforce World Health Organization, Europe: World Health Organization, WHO. 2024. https://www.who.int/europe/activities/building-a-skilled-health-workforce
Ganann R, Weeres A, Lam A, Chung H, Valaitis R. Optimization of home care nurses in Canada: A scoping review. Health & Social Care in the Community [Internet]. 2019; 27(5):[e604-e21 pp.]. https://doi.org/10.1111/hsc.12797
Reeves S, Lewin S, Espin S, Zwarenstein M. Interprofessional teamwork for health and social care. Wiley; 2011.
Cunningham N, Cowie J, Watchman K, Methven K. Understanding the training and education needs of homecare workers supporting people with dementia and cancer: A systematic review of reviews. Dementia (London) [Internet]. 2020; 19(8):[2780 – 803 pp.]. https://doi.org/10.1177/1471301219859781
Kolb DA. Experiential learning: Experience as the source of learning and development. Second edition ed. Upper Saddle River, New Jersey Pearson Education, Inc.; 2015.
Säljö R, Moen S. Læring og kulturelle redskaper: om læreprosesser og den kollektive hukommelsen. Oslo: Cappelen akademisk forl.; 2006.
Myrvang T, Rokstad AMM. Simulering og ferdighetstrening kombinert med bruk av systematiske verktøy i sykehjem – en kvalitativ studie av sykepleieres erfaringer. Nordisk sygeplejeforskning [Internet]. 2022; 12(2):[1–14 pp.]. https://doi.org/10.18261/nsf.12.2.1
Peters M, Godfrey C, McInerney P, Munn Z, Tricco A, Khalil H. In: E A, Munn Z, editors. Chapter 11: scoping reviews. JBI Manual for Evidence Synthesis: JBI; 2020.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. International journal of social research methodology [Internet]. 2005; 8(1):[19–32 pp.]. https://doi.org/10.1080/1364557032000119616
Peters MDJ, Marnie C, Tricco AC, Pollock D, Munn Z, Alexander L, et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Synthesis [Internet]. 2020;18(10):2119. 26 pp.].
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Annals of internal medicine [Internet]. 2018; 169(7):[467 – 73 pp.]. https://www.acpjournals.org/doi/full/https://doi.org/10.7326/M18-0850
Singh S, Bajorek B. Defining ‘elderly’ in clinical practice guidelines for pharmacotherapy. Pharm Pract (Granada) [Internet]. 2014; 12(4):[489 p.]. https://doi.org/10.4321/s1886-36552014000400007
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ [Internet]. 2009; 339(7716):[332-6 pp.]. https://doi.org/10.1136/bmj.b2535
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Systematic reviews [Internet]. 2016; 5(1):1–10 pp.]. https://springerlink.fh-diploma.de/article/https://doi.org/10.1186/s13643-016-0384-4
Mayall E, Oathamshaw S, Lovell K, Pusey H. Development and piloting of a multidisciplinary training course for detecting and managing depression in the older person. Journal of Psychiatric and Mental Health Nursing [Internet]. 2004; 11(2):[165 – 71 pp.]. https://doi.org/10.1111/j.1365-2850.2003.00702.x
Quijano LM, Stanley MA, Petersen NJ, Casado BL, Steinberg EH, Cully JA, Wilson NL. Healthy IDEAS:A Depression Intervention Delivered by Community-Based Case Managers Serving Older Adults. Journal of Applied Gerontology [Internet]. 2007; 26(2):[139 – 56 pp.]. https://doi.org/10.1177/0733464807299354
Quinlan S, Ryer S. Implementing a Fall Prevention Initiative in Nurse-Facilitated Annual Wellness Visits: A Quality Improvement Project. Journal of Nursing Care Quality [Internet]. 2023; 38(3):[243 – 50 pp.]. https://doi.org/10.1097/NCQ.0000000000000690
Pollock D, Peters MDJ, Khalil H, McInerney P, Alexander L, Tricco AC et al. Recommendations for the extraction, analysis, and presentation of results in scoping reviews. JBI Evidence Synthesis [Internet]. 2023; 21(3):[520 – 32 pp.]. https://doi.org/10.11124/jbies-22-00123
Braun V, Clarke V. Thematic analysis: a practical guide. Los Angeles, California: SAGE; 2022.
Phillips M, Lu J. A quick look at NVivo. Journal of Electronic Resources Librarianship [Internet]. 2018 2018/04/03; 30(2):[104-6 pp.]. https://doi.org/10.1080/1941126X.2018.1465535
Pace R, Pluye P, Bartlett G, Macaulay AC, Salsberg J, Jagosh J, Seller R. Testing the reliability and efficiency of the pilot Mixed Methods Appraisal Tool (MMAT) for systematic mixed studies review. Int J Nurs Stud [Internet]. 2012; 49(1):[47–53 pp.]. https://doi.org/10.1016/j.ijnurstu.2011.07.002
Kazi MR, Chowdhury N, Chowdhury M, Turin TC. Conducting comprehensive scoping reviews to systematically capture the landscape of a subject matter. Population Medicine [Internet]. 2021; 3(December):[1–9 pp.]. https://doi.org/10.18332/popmed/143831
Hong QN, Pluye P, Fàbregues S, Bartlett G, Boardman F, Cargo M et al. Mixed methods appraisal tool (MMAT), version 2018. Registration of copyright [Internet]. 2018; 1148552(10).
Bruce ML, Brown EL, Raue PJ, Mlodzianowski AE, Meyers BS, Leon AC et al. A randomized trial of depression assessment intervention in home health care. J Am Geriatr Soc [Internet]. 2007; 55(11):[1793 – 800 pp.].
Couser S, Moehrlin BA, Deitrich C, Hess L. Expanding community health nursing roles to meet health-care needs of frail elderly. An adult learning model. J Community Health Nurs [Internet]. 1990;7(1):3–13. pp.].
Luptak M, Kaas MJ, Artz M, McCarthy T, Project ADAPT. A program to assess depression and provide proactive treatment in rural areas. Gerontologist [Internet]. 2008; 48(4):[542-8 pp.]. https://doi.org/10.1093/geront/48.4.542
Marcus P, Kennedy GJ, Wetherbee C, Korenblatt J, Dorta H, Lantz MS. Training professional home care staff to help reduce depression in elderly home care recipients. Clin Geriatr [Internet]. 2006; 14(7):[13 – 6 pp.].
Brown EL, Raue PJ, Roos BA, Sheeran T, Bruce ML. Training nursing staff to recognize depression in home healthcare. J Am Geriatr Soc [Internet]. 2010; 58(1):[122-8 pp.]. https://doi.org/10.1111/j.1532-5415.2009.02626.x
Stolee P, Patterson ML, Wiancko DC, Esbaugh J, Arcese ZA, Vinke AM et al. An enhanced role in comprehensive geriatric assessment for community-nurse case managers. Can J Aging [Internet]. 2003; 22(2):[177 – 84 pp.].
Brymer C, Cormack C, Spezowka K. Improving the care of the elderly in a rural county through education. Gerontology & Geriatrics Education [Internet]. 1998; 19(1):[55–64 pp.]. https://doi.org/10.1300/j021v19n01_05
Abbasi M, Khera S, Dabravolskaj J, Chevalier B, Parker K. The seniors’ community hub: An integrated model of care for the identification and management of frailty in primary care. Geriatrics (Switzerland) [Internet]. 2021; 6(1):[1–15 pp.]. https://doi.org/10.3390/geriatrics6010018
McCabe MP, Russo S, Mellor D, Davison TE, George K. Effectiveness of a training program for carers to recognize depression among older people. International Journal of Geriatric Psychiatry [Internet]. 2008; 23(12):[1290-6 pp.]. https://doi.org/10.1002/gps.2067
Mellor D, Kiehne M, McCabe MP, Davison TE, Karantzas G, George K. An evaluation of the beyondblue Depression Training Program for aged care workers. International Psychogeriatrics [Internet]. 2010; 22(6):[927 – 37 pp.]. https://doi.org/10.1017/S1041610210000153
Nunn R, Annells M, Sims J. Screening for depression in older district nursing clients: feasibility study. British Journal of Community Nursing [Internet]. 2007; 12(3):[108 – 14 pp.]. https://doi.org/10.12968/bjcn.2007.12.3.23037
Naughton C, Hayes N, Zahran Z, Norton C, Lee G, Fitzpatrick JM et al. The development of the Older Person’s Nurse Fellowship: Education concept to delivery. Nurse Education Today [Internet]. 2016; 44:[1–7 pp.]. https://doi.org/10.1016/j.nedt.2016.04.022
Smith A, Shepherd A, Macaden L, Macleod KL. Raising awareness of sensory impairment among community nurses: a brief intervention in a remote island setting. Rural & Remote Health [Internet]. 2018 08; 18(3):[4548 p.]. https://doi.org/10.22605/RRH4548
Butler M, Quayle E. Training primary care nurses in late-life depression: knowledge, attitude and practice changes. International Journal of Older People Nursing [Internet]. 2007 2023-10-26; 2(1):[25–35 pp.]. https://doi.org/10.1111/j.1748-3743.2007.00054.x
Landi F, Sgadari A, Cipriani L, Castellani M, Pahor M, Carbonin PU, Bernabei R. A simple program to train case managers in community elderly care. Aging Clinical and Experimental Research [Internet]. 1996; 8(3):[211-8 pp.]. https://doi.org/10.1007/bf03339679
Neto JBF, de Moraes GLA, de Souza Aredes J, Giacomin KC, de Melo LP, Sempe L, Lloyd-Sherlock P. Building the capacity of community health workers to support health and social care for dependent older people in Latin America: a pilot study in Fortaleza, Brazil. BMC Geriatrics [Internet]. 2021 10 02; 21(1):[526 p.]. https://doi.org/10.1186/s12877-021-02477-3
Piau A, Sourdet S, Toulza O, Bernon C, Tavassoli N, Nourhashemi F. Frailty Management in Community-Dwelling Older Adults: Initial Results of a Trained Nurses Program. Journal of the American Medical Directors Association [Internet]. 2019; 20(5):[642-3 pp.]. https://doi.org/10.1016/j.jamda.2018.11.011
Sin GL, Yeo D, Koh HJ, Lee J, Ng LL. Training eldercare workers in mental healthcare. Singapore Med J [Internet]. 2018 01; 59(1):[28–32 pp.]. https://doi.org/10.11622/smedj.2017052
Van Daele T, Vansteenwegen D, Hermans D, Van den Bergh O, Van Audenhove C. Home nurses and patient depression. Attitudes, competences and the effects of a minimal intervention. Journal of Advanced Nursing (John Wiley & Sons, Inc) [Internet]. 2015; 71(1):[126 – 35 pp.]. https://doi.org/10.1111/jan.12476
King AII, Boyd ML, Dagley L, Raphael DL. Implementation of a gerontology nurse specialist role in primary health care: Health professional and older adult perspectives. J Clin Nurs [Internet]. 2018; 27(3–4):[807 – 18 pp.]. https://doi.org/10.1111/jocn.14110
Di Leonardi BC. Tips for facilitating learning: the lecture deserves some respect. J Contin Educ Nurs [Internet]. 2007 Jul-Aug; 38(4):[154 – 61; quiz 62 – 3, 75 pp.]. https://doi.org/10.3928/00220124-20070701-09
Dieckmann P. Using Simulations for Education, Training and Research. Pabst Science; 2009.
Tannenbaum SI, Cerasoli CP. Do Team and Individual Debriefs Enhance Performance? A Meta-Analysis. Human Factors [Internet]. 2013; 55(1):[231 – 45 pp.]. https://doi.org/10.1177/0018720812448394
Tannenbaum SI, Greilich PE. The debrief imperative: building teaming competencies and team effectiveness. BMJ Quality & Safety [Internet]. 2023; 32(3):[125-8 pp.]. https://doi.org/10.1136/bmjqs-2022-015259
Montano AR, Shellman J, Malcolm M. Outcomes From an Interprofessional Geriatric Outreach and Training Program. Innov Aging [Internet]. 2022; 6(6):[igac044 p.]. https://doi.org/10.1093/geroni/igac044
Ostertag S, Bosic-Reiniger J, Migliaccio C, Zins R. Promoting Older Adult Health with Interprofessional Education through Community Based Health Screening. Int J Environ Res Public Health [Internet]. 2022; 19(11). https://doi.org/10.3390/ijerph19116513
Park MK, Taylor JA, Biernot J, Martin DJ, The Virtual Geriatric Assessment Interdisciplinary Team Project.: Interprofessional Geriatric Training Against the Backdrop of COVID-19. Journal of Applied Gerontology [Internet]. 2024; 0(0):[07334648241234496 p.]. https://doi.org/10.1177/07334648241234496
Decker S, Sportsman S, Puetz L, Billings L. The Evolution of Simulation and Its Contribution to Competency. The Journal of Continuing Education in Nursing [Internet]. 2008; 39(2):[74–80 pp.]. Available from: https://doi.org/10.3928/00220124-20080201-06
Rutherford-Hemming T. Simulation Methodology in Nursing Education and Adult Learning Theory. Adult Learning [Internet]. 2012; 23(3):[129 – 37 pp.]. https://doi.org/10.1177/1045159512452848
Husebø SE, O’Regan S, Nestel D. Reflective practice and its role in simulation. Clinical Simulation in Nursing [Internet]. 2015; 11(8):[368 – 75 pp.]. https://doi-org.ezproxy.uis.no/https://doi.org/10.1016/j.ecns.2015.04.005
Acosta DJ, Rinfret A, Plant J, Hsu AT. Using Patient Simulation to Promote Best Practices in Fall Prevention and Postfall Assessment in Nursing Homes. Journal of Nursing Care Quality [Internet]. 2022; 37(2):[117 – 22 pp.]. https://doi.org/10.1097/NCQ.0000000000000599
Vygotskij LS, Roster MT, Bielenberg T-J, Skodvin A, Kozulin A. Tenkning og tale. Oslo: Gyldendal akademisk; 2001.
Owen L, Steel A, Goffe K, Pleming J, Sampson EL. A multidisciplinary simulation programme to improve advance care planning skills and engagement across primary and secondary care. Clinical Medicine. 2022; 22(1):[51 – 7 pp.]. https://doi.org/10.7861/clinmed.2021-0240
Vygotskij LS, Cole MG, John-Steiner V, Scribner S, Souberman E. Mind in society: the development of higher psychological processes. Cambridge, Mass: Harvard University Press; 1978.
Nelson JC, Clary CM, Leon AC, Schneider LS. Symptoms of Late-Life Depression: Frequency and Change During Treatment. The American Journal of Geriatric Psychiatry [Internet]. 2005 Jun 2005; 13(6):[520-6 pp.]. http://ezproxy.uis.no/login?url=https://www-proquest-com.ezproxy.uis.no/scholarly-journals/symptoms-late-life-depression-frequency-change/docview/195983951/se-2
Mulasso A, Roppolo M, Giannotta F, Rabaglietti E. Associations of frailty and psychosocial factors with autonomy in daily activities: a cross-sectional study in Italian community-dwelling older adults. Clinical Interventions in Aging [Internet]. 2016 2023-11-22; 11:[37–45 pp.]. https://doi.org/10.2147/CIA.S95162
Oyon J, Serra-Prat M, Ferrer M, Llinares A, Pastor N, Limón E et al. Psychosocial factors associated with frailty in the community-dwelling aged population with depression. A cross-sectional study. Atención Primaria [Internet]. 2021 2021/05/01/; 53(5):[102048 p.]. https://doi.org/10.1016/j.aprim.2021.102048
Agredano RS, Masclans JG, Guix-Comellas EM, Fraile VM, Sarria-Guerrero JA, Pola MS, Fabrellas N. Older Adults With Complex Chronic Conditions Who Receive Care at Home: The Importance of Primary Care Assessment. Journal of gerontological nursing [Internet]. 2021; 47(11):[31 – 8 pp.]. https://doi.org/10.3928/00989134-20211013-02
Seematter-Bagnoud L, Büla C. Brief assessments and screening for geriatric conditions in older primary care patients: a pragmatic approach. Public Health Rev [Internet]. 2018; 39:[8 p.]. https://doi.org/10.1186/s40985-018-0086-7
Piccoliori G, Gerolimon E, Abholz HH. Geriatric assessment in general practice using a screening instrument: is it worth the effort? Results of a South Tyrol Study. Age Ageing [Internet]. 2008; 37(6):[647 – 52 pp.]. https://doi.org/10.1093/ageing/afn161
Prince MJ, Acosta D, Guerra M, Huang Y, Jacob KS, Jimenez-Velazquez IZ et al. Intrinsic capacity and its associations with incident dependence and mortality in 10/66 Dementia Research Group studies in Latin America, India, and China: A population-based cohort study. PLoS Med [Internet]. 2021; 18(9):[e1003097-e pp.]. https://doi.org/10.1371/journal.pmed.1003097
Seah B, Kowitlawakul Y, Jiang Y, Ang E, Chokkanathan S, Wang W. A review on healthy ageing interventions addressing physical, mental and social health of independent community-dwelling older adults. Geriatric Nursing [Internet]. 2019; 40(1):[37–50 pp.]. https://doi.org/10.1016/j.gerinurse.2018.06.002
Macdonald SHF, Travers J, Éidín Ní S, Bailey J, Romero-Ortuno R, Keyes M et al. Primary care interventions to address physical frailty among community-dwelling adults aged 60 years or older: A meta-analysis. PLoS One [Internet]. 2020; 15(2). https://doi.org/10.1371/journal.pone.0228821
Li C-M, Chen C-Y, Li C-Y, Wang W-D, Wu S-C. The effectiveness of a comprehensive geriatric assessment intervention program for frailty in community-dwelling older people: a randomized, controlled trial. Archives of Gerontology and Geriatrics [Internet]. 2010; 50:[S39-S42 pp.]. https://doi.org/10.1016/S0167-4943(10)70011-X
Metzelthin SF, Daniëls R, van Rossum E, Cox K, Habets H, de Witte LP, Kempen GIJM. A nurse-led interdisciplinary primary care approach to prevent disability among community-dwelling frail older people: A large-scale process evaluation. Int J Nurs Stud [Internet]. 2013; 50(9):[1184-96 pp.]. https://doi.org/10.1016/j.ijnurstu.2012.12.016
Fox ST, Janda M, Hubbard R. Understanding how comprehensive geriatric assessment works: the importance of varied methodological approaches. Aging Clinical and Experimental Research [Internet]. 2023 2023/02/01; 35(2):[417 – 23 pp.]. https://doi.org/10.1007/s40520-022-02305-7
Metzelthin SF, van Rossum E, de Witte LP, Ambergen AW, Hobma SO, Sipers W, Kempen GIJM. Effectiveness of interdisciplinary primary care approach to reduce disability in community dwelling frail older people: cluster randomised controlled trial. BMJ [Internet]. 2013; 347(7926):[12- pp.]. https://doi.org/10.1136/bmj.f5264
Mayo-Wilson E, Grant S, Burton J, Parsons A, Underhill K, Montgomery P. Preventive home visits for mortality, morbidity, and institutionalization in older adults: a systematic review and meta-analysis. PLoS One [Internet]. 2014 PMC3951196]; 9(3):[e89257 p.]. https://doi.org/10.1371/journal.pone.0089257
Lagerin A. District nurses’ experiences of preventive home visits to 75-year-olds in Stockholm: a qualitative study. Primary Health Care Research & Development (Cambridge University Press / UK) [Internet]. 2016; 17(5):[464 – 78 pp.]. https://doi.org/10.1017/S1463423615000560
Rietkerk W, Smit MF, Wynia K, Slaets JPJ, Zuidema SU, Gerritsen DL. Explaining experiences of community-dwelling older adults with a pro-active comprehensive geriatric assessment program - a thorough evaluation by interviews. BMC Geriatr [Internet]. 2019; 19(1):[12 p.]. https://doi.org/10.1186/s12877-018-1025-7
Papadopoulou C, Barrie J, Andrew M, Martin JC, Birt A, Raymond Duffy FJ, Hendry A. Perceptions, practices and educational needs of community nurses to manage frailty. Br J Community Nurs [Internet]. 2021; 26(3):[136 – 42 pp.]. https://doi.org/10.12968/bjcn.2021.26.3.136
Lang D, Hoey C, O’Shea D, Whitty H. National Frailty Education Programme Report: the fundamentals of Frailty. Republic of Ireland: Health Service Executive; 2023.
Donoghue OA, O’Shea M, McGarrigle CA, Lang D, Hoey C, Whitty H et al. Translating frailty assessment methodologies and research-based evidence to clinical education and practice. Journal of Aging & Social Policy [Internet]. 2022; 34(4):[537 – 51 pp.]. https://doi-org.ezproxy.uis.no/10.1080/08959420.2020.1777825
Obbia P, Graham C, Duffy FJR, Gobbens RJJ. Preventing frailty in older people: An exploration of primary care professionals’ experiences. Int J Older People Nurs [Internet]. 2020; 15(2):[e12297 p.]. https://doi.org/10.1111/opn.12297
Hoogendijk EO, Afilalo J, Ensrud KE, Kowal P, Onder G, Fried LP. Frailty: implications for clinical practice and public health. Lancet [Internet]. 2019; 394(10206):[1365-75 pp.]. https://doi.org/10.1016/S0140-6736(19)31786-6
Carroll C, Sworn K, Booth A, Tsuchiya A, Maden M, Rosenberg M. Equity in healthcare access and service coverage for older people: a scoping review of the conceptual literature. Integr Healthc J [Internet]. 2022; 4(1):[e000092 p.]. https://doi.org/10.1136/ihj-2021-000092
Dieckmann P. The unexpected and the non-fitting - considering the edges of simulation as social practice. Adv Simul (Lond) [Internet]. 2020; 5(1):[2- pp.]. https://doi.org/10.1186/s41077-020-0120-y
Reierson IA, Ravik M, Blomberg K, Bjork IT, Boelenius K, Stenholt BV, Husebo SE. Comparing didactic approaches for practical skills learning in Scandinavian nursing simulation centres: A qualitative comparative study. J Adv Nurs [Internet]. 2024. https://doi.org/10.1111/jan.16150
Stoop A, Lette M, van Gils PF, Nijpels G, Baan CA, de Bruin SR. Comprehensive geriatric assessments in integrated care programs for older people living at home: A scoping review. Health Soc Care Community [Internet]. 2019; 27(5):[e549-e66 pp.]. https://doi.org/10.1111/hsc.12793
Ahmed I, Ishtiaq S. Reliability and validity: Importance in Medical Research. J Pak Med Assoc [Internet]. 2021; 71(10):[2401-6 pp.]. https://doi.org/10.47391/jpma.06-861
Mölenberg FJM, de Vries C, Burdorf A, van Lenthe FJ. A framework for exploring non-response patterns over time in health surveys. BMC Medical Research Methodology [Internet]. 2021 2021/02/18; 21(1):[37 p.]. https://doi.org/10.1186/s12874-021-01221-0
Skelly AC, Dettori JR, Brodt ED. Assessing bias: the importance of considering confounding. Evid Based Spine Care J [Internet]. 2012; 3(1):[9–12 pp.]. https://doi.org/10.1055/s-0031-1298595
Pourhoseingholi MA, Baghestani AR, Vahedi M. How to control confounding effects by statistical analysis. Gastroenterol Hepatol Bed Bench [Internet] 2012 Spring; 5(2):79–83 pp.].
Acknowledgements
The authors express gratitude to librarian Kari Hølland, Division of Research, Stavanger University Library for performing the systematic literature searches.
Funding
This article stems from the research project “More good days at home - Advancing health promoting practices in municipal healthcare services for older recipients of homecare” (HEIME), specifically related to Work Package 3, “Simulation and training for health needs assessment in home-living older adults”. HEIME is funded by the Research Council of Norway (grant 320622), University of Southeastern-Norway, University of Stavanger, Stavanger, Horten, Porsgrunn and Nome municipality (2021–2025). Dr. Grethe Eilertsen is the project director. Drs. Siri Tønnessen, Anette Hansen and Professor Marianne Storm are the principal researchers and work package leaders.
Open access funding provided by University of Stavanger & Stavanger University Hospital
Author information
Authors and Affiliations
Contributions
All authors (BHL, DND, HKF, PD and MS) contributed to the design and development of the study, research questions, and literature search. BHL conducted the literature search in collaboration with MS and research librarian. All authors participated in the screening and quality assessment processes. Data analysis and manuscript writing and preparation was led by BHL in collaboration with MS. All authors were involved in reading, commenting and reviewing the text, and approving the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This scoping review article does not contain any studies with human participants performed by any of the authors.
Consent for publication
Not applicable.
Conflict of interest
None declared.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Larsen, B.H., Dyrstad, D.N., Falkenberg, H.K. et al. Training healthcare professionals in assessment of health needs in older adults living at home: a scoping review. BMC Med Educ 24, 1019 (2024). https://doi.org/10.1186/s12909-024-06014-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12909-024-06014-9