Abstract
Introduction
Recent international consensus statements advocate for the integration of Point-of-Care Ultrasound (PoCUS) into the global undergraduate medical curriculum. Some medical schools outside Saudi Arabia have already incorporated PoCUS into their undergraduate curricula to enhance anatomy, physiology and pathology instruction. However, there are no data on the potential role of PoCUS in the preclinical training of medical students in Saudi Arabia. Given constraints on resources for medical education, a formal needs assessment was conducted to evaluate the potential utility of PoCUS within the basic science curriculum at our institution.
Methods
All final year medical students at our institution were invited to complete a validated online survey. The questionnaire utilized a 5-point Likert scale to assess student perceptions of the potential for PoCUS to improve their understanding of basic sciences and their desire for its incorporation into the preclinical curriculum.
Results
A total of 229 students participated (response rate 76%; male 134/200; female 95/100). Our survey demonstrated good internal consistency (Cronbach’s alpha: learning basic sciences 0.81, need for curriculum integration 0.83). The vast agreed that learning PoCUS would enhance their understanding of anatomy (95%) and pathology (75%). While only 52% agreed that learning PoCUS would improve their understanding of physiology, a substantial majority (80%) agreed that all medical schools should incorporate PoCUS into their undergraduate curricula. Furthermore, 62% agreed that offering PoCUS training would make the medical school more attractive to prospective applicants. No significant differences were observed between the responses of male and female students. The results of a confirmatory factor analysis provide strong support for the hypothesized three-factor model. All factor loadings are significant (P < 0.001),
Conclusions
Medical students in Saudi Arabia perceive that PoCUS would be a valuable tool to learn anatomy and pathology, aligning with the recommendations of the consensus conference on PoCUS integration in undergraduate medical education organized by the World Interactive Network Focused on Critical Ultrasound (WINFOCUS) and the Society of Ultrasound in Medical Education (SUSME). Introducing PoCUS training into preclinical medical curricula may also enhance the attractiveness of medical schools to potential applicants.
Take home message
Aligning with Global Trends: Integrating PoCUS into Undergraduate Medical Education.
Our study adds to the growing momentum for Point-of-Care Ultrasound (PoCUS) training in medical education. Building upon the recent proposal for a global PoCUS curriculum by WINFOCUS and SUSME, our findings demonstrate that Saudi Arabian medical students perceive PoCUS as a valuable tool for enhancing their grasp of basic sciences. This strong student support reinforces the case for integrating PoCUS into pre-clinical medical curricula throughout Saudi Arabia. The survey instrument developed for this study (Appendix 1) is a valuable tool for universities worldwide, allowing them to conduct similar needs assessments tailored to their specific contexts and contribute to the global adoption of PoCUS education.
Similar content being viewed by others
Background
The COVID-19 pandemic dramatically accelerated the adoption of point-of-care ultrasound (PoCUS) in clinical practice. A substantial body of evidence supports its routine use across various specialties [1,2,3,4,5,6,7]. This growing recognition has led to a surge in demand for PoCUS training among clinical medical students, interns, and residents in several specialties worldwide [8,9,10,11,12,13,14,15,16]. Reflecting this interest, residency programs worldwide are incorporating PoCUS training into their curriculums [8,9,10,11,12,13,14,15,16].
The potential benefits of early exposure to PoCUS for preclinical medical students have garnered significant attention. Studies have reported that PoCUS can enhance the learning of anatomy, pathology and physiology [17,18,19]. Indeed, several medical schools in Europe and the United States of America (USA) have successfully integrated PoCUS into their preclinical curricula [20,21,22,23,24].
Global organizations like the World Interactive Network Focused on Critical Ultrasound (WINFOCUS) and the Society of Ultrasound in Medical Education (SUSME) advocate for the widespread implementation of PoCUS into medical education [21, 22, 25]. However, a recent WINFOCUS/SUSME consensus conference on ultrasound education for undergraduate medical students highlights a limitation. The 69 authors only represented 17 countries and the majority primarily represented North American settings. This reinforces the need for context-specific PoCUS curricula tailored to individual institutional resources and settings [20].
Saudi Arabia presents a unique case study. While the potential benefits of early PoCUS exposure are evident, its integration into the preclinical medical curriculum remains absent. Several factors contribute to this gap. The Saudi Arabian healthcare system, like many others, faces resource constraints that necessitate careful consideration of educational priorities. A rapid expansion in the number of medical schools in Saudi Arabia from five in 1996 to 21 by 2008 has strained the existing infrastructure and the available qualified medical educators [26]. Additionally, the disparities in healthcare access between urban and rural areas, coupled with unique cultural and societal nuances, present further challenges. The use of English as the language of instruction also poses challenges for non-native English speakers.
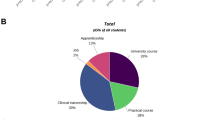
Our institution’s six-year medical program comprises three phases. The initial two-year preparatory phase focuses on foundational sciences and English language acquisition. The next two years integrate basic and clinical sciences through a problem-based learning approach, but without direct patient contact. The final two years are dedicated to clinical rotations.
Given the limited resources available for medical education, any proposal for its inclusion requires thorough needs assessment [9, 11]. A needs assessment is a systematic process of collecting and analyzing data to identify gaps between current practice and desired outcomes in medical education. While focus groups and interviews can be conducted, surveys are a common and efficient tool for needs assessments [27].
Previous research in Saudi Arabia indicates that while medical students [10] and interns [11] value PoCUS, initiating training in the internship year would be suboptimal [11]. Therefore, it is important to determine whether Saudi medical students perceive the preclinical use of PoCUS for basic science education as appropriate and necessary [28, 29].
This study addresses this knowledge gap by investigating:
Primary objective
To identify medical students’ perceptions of utilizing PoCUS for learning basic sciences.
Secondary objective
To explore medical students desire to incorporate PoCUS into the preclinical curriculum.
Understanding Saudi medical students’ perspectives is crucial for developing a locally relevant PoCUS curriculum. Moreover, the findings of this study may inform broader educational strategies and policies aimed at optimizing preclinical medical education within the region and beyond.
Methods
Ethical approval
The study was approved by the institutional review board (IRB) of King Abdulaziz Medical City, Riyadh (KAMC) and King Saud bin Abdulaziz University for Health Sciences (KSAU-HS) at the King Abdullah International Medical Research Center, Riyadh, Saudi Arabia.
Sample size calculation
To achieve a 5% margin of error with a 95% confidence level, a minimum sample size of 169 medical students was calculated assuming a 50% response distribution. This calculation considered the total population of 300 year-six medical students (200 male, 100 female).
Participants
Medical students at KSAU-HS are not currently exposed to PoCUS during their basic medical sciences education. While students may encounter PoCUS during their clinical rotations, the institution lacks a formal curriculum or training program specifically designed for PoCUS instruction.
To account for potential refusal to respond and achieve the target sample size of 169, all 300 year-six medical students (male 200, female 100) enrolled at our institution’s College of Medicine during the 2020–2021 academic year were invited to participate. An online survey link was sent to the medical students via email in January 2021. While email reminders were sent, no incentives were given and informed consent was obtained from all participants prior to survey completion.
Study and survey design
This cross-sectional survey investigated the potential benefits of incorporating point-of-care ultrasound (PoCUS) into basic science education at a large university for health sciences in Saudi Arabia. To develop a robust and relevant survey instrument, comprehensive literature search was conducted to evaluate the data demonstrating the relevance of PoCUS to learning anatomy, physiology and pathology [4,5,6,7,8, 12,13,14, 17, 20,21,22,23,24,25].
Informed by this review, two experts in survey design, medical education, PoCUS and medicine (RR and AH) collaboratively developed the questionnaire, which was structured into four sections: demographics, needs assessment, curriculum integration, and open-ended feedback.
The questionnaire comprised the following sections:
Demographics: This section collected basic data on participants’ age and sex.
Needs assessment: This section assessed students’ attitudes towards the potential use of PoCUS to learn basic preclinical sciences.
Curriculum integration: This section explored students’ perceptions of whether the College of Medicine should introduce PoCUS into the preclinical curriculum.
Open-ended feedback: This final section invited students to provide written comments on their attitudes towards using PoCUS in basic science education.
To enhance the questionnaire’s validity and reliability, a rigorous development process was employed. Initial content validity was established through expert review. Subsequently, following IRB approval, a pilot study involving five interns was conducted to assess clarity, comprehensiveness, and participant burden. The interns agreed that the content was appropriate, the questions were clear and no changes were required. The final questionnaire, presented in Appendix 1 was converted to an online format using Google Forms (Google, LLC, USA).
Study outcomes
Student perspectives on the utility of PoCUS for learning basic sciences (i.e., applicability) were assessed using a 5-point Likert scale (1 very poor, 2 poor, 3 fair, 4 good, 5 very good). Participants rated their agreement with statements regarding the potential incorporation of PoCUS into their medical school’s undergraduate curriculum on another 5-point Likert scale (1 strongly disagree, 2 disagree, 3 neutral, 4 agree, 5 strongly agree). Open-ended responses provided additional qualitative data on student perceptions of PoCUS.
Statistical analysis
All statistical analyses were performed using Excel (version 2016, Microsoft, USA) and R Studio (version 4.4.1 posit, USA). The data were analyzed using standard descriptive statistics. Each variable, including attitudes, applicability, competency, knowledge, and skills was evaluated independently. All responses were included in the final analysis, with data stratified by participant sex. Categorical data are presented as frequencies and percentages while interval data, derived from the Likert scales are presented as frequencies, percentages and means ± standard deviations (SD) as described previously [11, 29]. Likert scale data were assessed for internal consistency using Cronbach’s alpha. The responses of male and female medical students were compared using Chi-squared or McNemar tests for categorical data and Student’s t-test or analysis of variance (ANOVA) for interval data, as appropriate. To verify the construct validity of the survey instrument, a confirmatory factor analysis (CFA) was conducted using the R package lavaan [30]. A three-factor model was hypothesized, aligning with the study’s objectives and the literature. The factors were:
-
1.
Perceived Utility of PoCUS for Basic Science Learning: This factor assessed students’ beliefs about PoCUS’s potential to enhance understanding of foundational sciences (e.g., anatomy, physiology, and pathology).
-
2.
Perceived Utility of PoCUS for Regional Anatomy Learning: This factor focused on students’ perceptions of PoCUS’s role in learning specific anatomical regions.
-
3.
Attitudes Toward PoCUS Integration: This factor explored students’ attitudes towards incorporating PoCUS into the preclinical curriculum.
Results
Demographic information and response rates
A total of 229 medical students (mean age 23.8 ± SD 1.7 years) participated in the study, representing a response rate of 76.3% (Male 134, 67%; Female 95, 95%). The high response rate (RR) exceeded the minimum required to achieve the desired margin of error and confidence. Women’s RR (95%) were higher than men’s (67%). All participants answered all questions and all answers were included in the analyses.
Attitude towards using PoCUS to learn basic sciences
Table 1 summarizes medical students’ responses regarding the potential of PoCUS to enhance their understanding of various basic sciences. A vast majority of the sample (217, 94.8%) agreed or strongly agreed that learning PoCUS would increase their understanding of anatomy.
Significantly fewer students agreed that learning PoCUS would increase medical students’ understanding of pathology (171, 74.7%; P < 0.00001) or physiology (119, 52% P < 0.00001). The perceived benefit of PoCUS for learning physiology was significantly lower than both anatomy and pathology (p < 0.00001). There were no significant differences between the responses of male and female medical students (Fig. 1; P > 0.05).
Medical students’ attitudes towards the relevance of PoCUS to learning basic science, stratified by sex. Medical students’ attitudes towards the relevance of PoCUS to learning basic science stratified by sex. *Agreement with statements about whether learning PoCUS would improve understanding of basic sciences was rated on a 5-point Likert scale (1 strongly disagree, 2 disagree, 3 neutral, 4 agree, 5 strongly agree). Data are stratified by sex and presented as mean ± standard deviation. Abbreviations. COM, college of medicine; PoCUS, point-of-care ultrasound
Attitude towards using PoCUS to learn the anatomy of specific body parts
Table 2 summarizes medical student responses regarding the potential of PoCUS to enhance their understanding of the anatomy of specific body regions (head and neck, abdomen and pelvis). The internal consistency of the questions on attitudes towards using PoCUS to learn basic sciences and the anatomy of specific body parts was good (Cronbach’s alpha 0.81). The majority agreed or strongly agreed that learning PoCUS would increase medical students’ understanding of abdominal anatomy (215, 93.7%) and pelvic anatomy (210, 91.7%; P = 0.016). However, significantly fewer held the same belief regarding head and neck anatomy (165, 72.1%; P < 0.00001). There were no significant differences between the responses of male and female medical students (Fig. 2; P > 0.05).
Medical students’ attitudes towards the relevance of PoCUS to learning the anatomy of various regions of the body, stratified by sex. Medical students’ attitudes towards the relevance of PoCUS to learning the anatomy of various regions of the body stratified by sex. *Agreement with statements about whether learning PoCUS would improve understanding of the anatomy of various regions of the body was rated on a Likert scale (1 strongly disagree, 2 disagree, 3 neutral, 4 agree, 5 strongly agree). Data are stratified by sex and presented as mean ± standard deviation. Abbreviations. COM, college of medicine; PoCUS, point-of-care ultrasound
Perceived benefits of integration of PoCUS training into the preclinical curriculum
The internal consistency for these questions was good (Cronbach’s alpha 0.84). As shown in Table 3, a substantial majority of participants (182, 79.5%) agreed or strongly agreed that all medical schools should incorporate PoCUS into their undergraduate curricula. Many students (143, 62.4%) also perceived that the medical school setting of the current study would attract more applicants if it offered PoCUS training. There were no significant differences between the responses of male and female medical students (Fig. 3; p > 0.05).
Medical students’ attitudes towards whether medical schools should teach PoCUS, stratified by sex. Medical students’ attitudes towards whether the College of Medicine should teach PoCUS stratified by sex. *Agreement with statements about whether learning PoCUS would improve understanding of basic sciences was rated on a Likert scale (1 strongly disagree, 2 disagree, 3 neutral, 4 agree, 5 strongly agree). Data are stratified by sex and presented as mean and standard deviation. Abbreviations. COM, college of medicine; PoCUS, point-of-care ultrasound
Confirmatory factor analysis
The results of the CFA analysis presented in Appendix Tables 1 and 2 provide strong support for the hypothesized three-factor model. All factor loadings are significant (P < 0.001), indicating appropriate grouping of the variables into their respective factors. The model fit indices are generally good, suggesting a satisfactory fit between the model and the data. Overall, the CFA results provide evidence for the validity and reliability of the measurement model, supporting the use of these factors in further research and analysis.
Free text comments
Three participants provided free text comments, which are listed below with corrected spelling and grammar.
“More courses should be added to increase medical students’ knowledge”.
“I wish a radiology course was organized to cover all aspects of imaging especially ultrasound. A consolidated two weeks radiology course could massively boost our radiology skills and understanding.”
“Thank you for your valuable questionnaire. I would love to improve if there is any way I can learn please let me know. Thank you.”
These comments align with the findings of the quantitative data analysis, offering valuable insights into these students’ perspectives on their undergraduate medical education and the potential benefits of integrating PoCUS into the curriculum.
Discussion
Our findings underscore the strong belief among medical students in the potential benefits of PoCUS for enhancing their understanding of anatomy (95%) and pathology (75%). Furthermore, a substantial majority (80%) agreed or strongly agreed that PoCUS should be integrated into undergraduate medical curricula in Saudi Arabia. Our observations align with the constructivist learning theory, which suggests that active, hands-on learning experiences can facilitate deeper understanding and retention of complex concepts [31]. Furthermore, the specific free text comments requesting additional courses and a focus on ultrasound suggest a genuine interest and perceived need for PoCUS training among the participants.
While the intuitive advantage of using real-time imaging to visualize anatomy is clear, fewer participants perceived a similar benefit for physiology. Nevertheless, the overall student body recognized the potential value of incorporating PoCUS into preclinical curricula. Despite these positive student perceptions, at the end of the first quarter of the 21st Century, the integration of PoCUS into preclinical medical education remains largely absent in the Middle East and is limited to only a few universities worldwide [20,21,22,23,24].
At our institution, and many others throughout Saudi Arabia; male and female medical students are taught in separate branches of the College of Medicine. Both groups expressed the belief that learning PoCUS could improve their understanding of basic sciences. This observation has significant implications for medical education in Saudi Arabia, highlighting the need for a standardized approach to PoCUS training that is applicable to all medical students.
The Coronavirus Disease 2019 pandemic brought the benefits of PoCUS clearly into focus, demonstrating its utility in various clinical settings. It is not surprising that medical students were aware that PoCUS could improve their understanding of pathology and advocated for its curricular integration. While the primary application of PoCUS lies in clinical settings, its integration into the pre-clinical curriculum can offer significant benefits. By using PoCUS in simulated clinical scenarios and basic science courses, students can:
Enhance Visual Learning: PoCUS provides a visual and interactive approach to learning anatomy and physiology, making abstract concepts more tangible [17,18,19].
Develop Clinical Reasoning Skills: Early exposure to PoCUS can help students develop clinical reasoning skills by interpreting ultrasound images and making diagnostic decisions [17,18,19].
Given the strong student interest and the potential educational benefits, we propose integrating PoCUS into both the preclinical and clinical phases of the medical curriculum.
Pre-clinical Phase:
Basic Science Integration: PoCUS can be integrated into specific courses, such as anatomy and physiology, to visualize anatomical structures and physiological processes in real-time.
Simulated Learning Environments: PoCUS can be used in simulated clinical scenarios to enhance the learning of anatomy, physiology, and pathology.
Clinical Phase:
Point-of-Care Ultrasound: PoCUS can be used at the bedside to diagnose and manage various clinical conditions.
Procedural Skills Training: PoCUS can be used to guide procedures such as phlebotomy, peripheral line placement and arterial puncture.
While the traditional definition of PoCUS emphasizes its use at the point of care, its application in simulated environments can provide controlled setting for students to practice and develop essential skills while learning basic sciences. By integrating PoCUS into both pre-clinical and clinical settings, we can equip future clinicians with the knowledge and skills necessary to effectively utilize this valuable tool.
To realize this potential locally, medical schools must develop tailored PoCUS curricula and training programs to improve educational outcomes and attract prospective students,
Globally, these findings should encourage medical schools to standardize the inclusion of innovative teaching tools like PoCUS. Students’ perception that the use of this tool may improve their understanding of anatomy and specific body parts suggests that similar curricula could be beneficial across diverse educational systems. By aligning training with emerging technologies, institutions may better prepare future physicians for contemporary healthcare challenges.
Development of a curriculum and training program for basic sciences
While general guidelines exist [20,21,22,23,24,25], a localized approach is essential. Establishing expert panels to define clear objectives and learning outcomes within the context of each institution’s resources.
While guided by the recommendations of the WINFOCUS/SUSME consensus conference [25], the curriculum must adhere to some fundamental principles [9, 25, 32]:
-
1.
Curriculum design: The curricula must be easily teachable, learnable and sustainable within the institution’s resources and environment [9, 25, 32].
-
2.
Clear indications: The use of PoCUS should be guided by clear objectives to achieve defined goals (e.g., visualizing the internal jugular vein to enhance understanding of anatomy) [25].
-
3.
Scope of practice and privileges: Scopes of practice and institutional privileges must be defined [9, 32]. Students must fully understand the limitations of PoCUS [9, 32].
-
4.
Integration without compromise: PoCUS training should not detract from students’ core learning of basic sciences.
Implementation of a curriculum and training program for PoCUS
Successful integration of PoCUS into preclinical curricula requires dedicated faculty sonography champions who can ensure regular didactic sessions, access to appropriate equipment, and most importantly, hands-on training [9, 32].
Faculty must possess sufficient theoretical, clinical, and practical PoCUS knowledge and skills [9, 32]. Comprehensive training, accreditation, and institutional credentialing are essential for faculty to effectively train and evaluate students [9, 32].
Institutional support must prioritize faculty development, establish the infrastructure for ongoing quality assurance processes and provide systems for the secure archiving of ultrasound images [9, 33]. This will require the support of fully certified sonographers and radiologists in the radiology department.
Implementing a PoCUS curriculum clearly demands significant resources and organizational commitment. To facilitate this and ensure that important aspects are not overlooked quality metrics for medical education must be used [13].
Our findings align with previous research demonstrating the value of PoCUS for medical students and trainees [10, 11, 16]. However, this study contributes novel evidence of strong student interest in PoCUS within the Saudi Arabian context, where its integration remains notably absent. This disparity underscores the urgent need for institutional curricula development.
While the study was conducted in Saudi Arabia, the findings may have broader implications for medical education worldwide. The implementation of a curriculum for ultrasound education of undergraduate medical students in Saudi Arabia may potentially be influenced by previous experience with PoCUS in other nations. The potential for international standardization of preclinical PoCUS training is suggested by the similarity between our findings and those reported for American students, interns, and residents [16].
Limitations and strengths
By employing a rigorous survey methodology, including the development of a validated questionnaire following a systematic literature review, the use of a representative sample and CFA, the needs assessment conducted in this study gathered comprehensive data on medical students’ perceptions of PoCUS and their expectations for its integration into the curriculum. Thus, this study provides a robust foundation for understanding the need for PoCUS education in our Saudi Arabian context.
The study surveyed final year medical students in the middle of the scholastic year. Thus, these students had completed their pre-clinical training in basic sciences. Although the curriculum at KSAU-HS currently does not include PoCUS, the students should have had some informal exposure to PoCUS during their clinical training. This informal exposure to PoCUS during clinical rotations, may have influenced the students’ perceptions of its utility in preclinical education. While, this strengthens the generalizability of our findings regarding the potential role of PoCUS in basic science education within our institution. However, it must be acknowledged that many medical students [10] and interns [11], in Saudi Arabia believe that PoCUS is applicable to clinical settings, which may have influenced their perspectives on its preclinical utility.
Although the response rate exceeded the desired threshold, the external validity of the findings may be limited. It was performed in final year medical students in one college of medicine in Riyadh, Saudi Arabia. However, the college attracts students from across the country, increasing the likelihood that the sample represents the broader population of medical students in Saudi Arabia. Future longitudinal studies could explore the long-term impact of PoCUS integration on student outcomes. Additionally, comparative studies across different educational settings would enhance our understanding of optimal implementation strategies.
Addition to literature
The current study provides evidence that medical students, training in Saudi Arabia, perceive that PoCUS may be applicable to learning basic sciences. However, PoCUS training is currently absent from undergraduate medical education in Saudi Arabia. This gap could be addressed by incorporating PoCUS into basic science curricula. However, this will require formal supervision, governance, and accreditation frameworks for students and their trainers.
Our findings are of significant value to institutions considering the development of PoCUS training programs for preclinical medical students. The survey instrument used in the present study (Appendix 1) can also be used by other institutions to conduct similar needs assessments for their own unique contexts.
Conclusions
A WINFOCUS/SUSME international consensus conference recently proposed a global curriculum for the use of PoCUS in undergraduate medical education [25]. However, their recommendations may not be feasible or applicable universally due to contextual variations. The present study demonstrates that both male and female medical students in Saudi Arabia believe that PoCUS can improve their understanding of basic sciences. Colleges of Medicine throughout Saudi Arabia should consider incorporating PoCUS into their preclinical curricula. Universities worldwide can adapt the survey instrument developed by the authors (Appendix 1) to perform similar needs assessments tailored to their institutions’ specific settings.
Data availability
The datasets generated and/or analysed during the current study are not publicly available because the institutional sponsor of the study (King Abdullah International Medical Research Center, Riyadh, Saudi Arabia) does not currently have a formal data sharing policy in place. The institution does not have a dedicated data repository or process for broader data sharing at this time. However, the authors have included the survey instrument used in the study (Appendix 1) to allow other researchers to replicate the study design and collect their own data within their specific institutional contexts. Furthermore, upon reasonable request the corresponding author will request approval from the Study’s sponsor to release anonymized data.
Abbreviations
- KAMC:
-
King Abdulaziz Medical City
- KAIMRC:
-
King Abdullah International Medical Research Center
- PoCUS:
-
Point-of-care ultrasound
- RR:
-
Response rate
- SD:
-
Standard deviation
- SUSME:
-
Society of Ultrasound in Medical Education
- WINFOCUS:
-
World Interactive Network Focused on Critical Ultrasound
References
Conlon TW, Nishisaki A, Singh Y, Bhombal S, De Luca D, Kessler DO, et al. Moving Beyond the Stethoscope: Diagnostic Point-of-Care Ultrasound in Pediatric Practice. Pediatrics. 2019;144:e20191402.
Longjohn M, Wan J, Joshi V, Pershad J. Point-of-care echocardiography by pediatric emergency physicians. Pediatr Emerg Care. 2011;27:693–6.
Marin JR, Dean AJ, Bilker WB, Panebianco NL, Brown NJ, Alpern ER. Emergency ultrasound-assisted examination of skin and soft tissue infections in the pediatric emergency department. Acad Emerg Med. 2013;20:545–53.
Pomero F, Dentali F, Borretta V, Bonzini M, Melchio R, Douketis JD, et al. Accuracy of emergency physician-performed ultrasonography in the diagnosis of deep-vein thrombosis: a systematic review and meta-analysis. Thromb Haemost. 2013;109:137–45.
Koratala A, Bhattacharya D, Kazory A. Point of care renal ultrasonography for the busy nephrologist: A pictorial review. World J Nephrol. 2019;8:44–58.
Olson APJ, Trappey B, Wagner M, Newman M, Nixon LJ, Schnobrich D. Point-of-care ultrasonography improves the diagnosis of splenomegaly in hospitalized patients. Crit Ultrasound J. 2015;7:13.
Rajendram R, Hussain A, Mahmood N, Kharal M. Feasibility of using a handheld ultrasound device to detect and characterize shunt and deep vein thrombosis in patients with COVID-19: An observational study. Ultrasound J. 2020;12:49.
Rajendram R, Souleymane M, Mahmood N, Kharal M, AlQahtani M. Point-of-care diagnostic lung ultrasound is highly applicable to the practice of medicine in Saudi Arabia but the current skills gap limits its use. Ann Thorac Med. 2021;16:266–73.
Souleymane M, Rajendram R, Mahmood N, Ghazi AMT, Kharal YMS, Hussain A. A survey demonstrating that the procedural experience of residents in internal medicine, critical care and emergency medicine is poor: training in ultrasound is required to rectify this. Ultrasound J. 2021;13:20.
Rajendram R, Alrasheed AO, Boqaeid AA, Alkharashi FK, Qasim SS, Hussain A. Training medical students in physical examination and point-of-care ultrasound: An assessment of the needs and barriers to acquiring skills in point-of-care ultrasound. J Family Community Med. 2022;29:62–70.
Jarwan W, Alshamrani AA, Alghamdi A, Mahmood N, Kharal YM, Rajendram R, et al. Point-of-Care Ultrasound Training: An Assessment of Interns ’ Needs and Barriers to Training. Cureus. 2020;12:e11209.
Ma IWY, Steinmetz P, Weerdenburg K, Woo MY, Olszynski P, Heslop CL, et al. The Canadian Medical Student Ultrasound Curriculum: A Statement From the Canadian Ultrasound Consensus for Undergraduate Medical Education Group. J Ultrasound Med. 2020;39:1279–87.
Ambasta A, Balan M, Mayette M, Goffi A, Mulvagh S, Buchanan B, et al. Education Indicators for Internal Medicine Point-of-Care Ultrasound: a Consensus Report from the Canadian Internal Medicine Ultrasound (CIMUS) Group. J Gen Intern Med. 2019;34:2123–9.
Jamil SF, Rajendram R. Training pediatric residents in point-of-care ultrasound: An assessment of the needs and barriers to acquire the skill. Int J Pediatr Adolesc Med. 2022;9:49–55.
Rajendram R, Souleymane M, Mahmood N, Sambas R, Kharal YMS. Measurement of the Applicability of Abdominal Point-of-Care Ultrasound to the Practice of Medicine in Saudi Arabia and the Current Skill Gaps. PoCUS J. 2021;6:36–41.
Koratala A, Segal MS, Kazory A. Integrating Point-of-Care Ultrasonography Into Nephrology Fellowship Training: A Model Curriculum. Am J kidney diseases: official J Natl Kidney Foundation. 2019;74:1–5.
Tarique U, Tang B, Singh M, Kulasegaram KM, Ailon J. Ultrasound Curricula in Undergraduate Medical Education: A Scoping Review. J Ultrasound Med. 2018;37:69–82.
So S, Patel RM, Orebaugh SL. Ultrasound imaging in medical student education: Impact on learning anatomy and physical diagnosis. Anat Sci Educ. 2017;10:176–89.
Nelson BP, Hojsak J, Dei Rossi E, Karani R, Narula J. Seeing Is Believing: Evaluating a Point-of-Care Ultrasound Curriculum for 1st-Year Medical Students. Teach Learn Med. 2017;29:85–92.
Prosch H, Radzina M, Dietrich CF, Nielsen MB, Baumann S, Ewertsen C, et al. Ultrasound Curricula of Student Education in Europe: Summary of the Experience. Ultrasound Int Open. 2020;6:E25–33.
Cantisani V, Dietrich CF, Badea R, Dudea S, Prosch H, Cerezo E, et al. EFSUMB Statement on Medical Student Education in Ultrasound [long version]. Ultrasound Int Open. 2016;2:E2–7.
Dietrich CF, Hoffmann B, Abramowicz J, Badea R, Braden B, Cantisani V, et al. Medical Student Ultrasound Education: A WFUMB Position Paper, Part I. Ultrasound Med Biol. 2019;45:271–81.
Siegel-Richman Y, Kendall J. Establishing an Ultrasound Curriculum in Undergraduate Medical Education: How Much Time Does It Take? J Ultrasound Med. 2018;37:569–76.
Stone-McLean J, Metcalfe B, Sheppard G, Murphy J, Black H, McCarthy H, et al. Developing an Undergraduate Ultrasound Curriculum: A Needs Assessment. Cureus. 2017;9:e1720.
Hoppmann RA, Mladenovic J, Melniker L, Badea R, Blaivas M, Montorfano M et al. International consensus conference recommendations on ultrasound education for undergraduate medical students. Ultrasound Journal. 2022;14:1–32.
Telmesani A, Zaini RG, Ghazi HO. Medical education in Saudi Arabia: a review of recent developments and future challenges. East Mediterranean Health J. 2011;17:703–7.
Myers P. GP learning needs assessments. Br J Gen Pract. 1999;49:303–7.
Kern D, Thomas P, Hughes M. Curriculum Development for Medical Education. A Six-Step Approach. Johns Hopkins University; 2009.
Watson K, Lam A, Arishenkoff S, Halman S, Gibson NE, Yu J, et al. Point of care ultrasound training for internal medicine: A Canadian multi-centre learner needs assessment study. BMC Med Educ. 2018;18:1–8.
Rosseel Y. lavaan: An R Package for Structural Equation Modeling. J Stat Softw. 2012;48:1–36.
Yachou Y, Samson O, Lasvergnas O. Prospective comparative study on enhancing geometrical mental representation and anatomical learning in medical students through modeling clay as an assessment tool. Anat Sci Educ. 2024;17:779–95.
Hussain A, Ma IWY. Internal Medicine Point of Care Ultrasound in the 21st Century: A FoCUS on the Middle East. J Saudi Heart Association. 2020;32:479–82.
Wong J, Montague S, Wallace P, Negishi K, Liteplo A, Ringrose J, et al. Barriers to learning and using point-of-care ultrasound: a survey of practicing internists in six North American institutions. Ultrasound J. 2020;12:19.
Acknowledgements
Not applicable.
Funding
None.
Author information
Authors and Affiliations
Contributions
RR conceptualised the study. All authors were involved in literature searches and the study design. RR, and AH designed the questionnaire for the survey. AOA, SSQ, AAB and FKA collected the data. RR performed the statistical analysis. All authors were involved in the interpretation of the data. RR prepared the initial draft of the manuscript. All authors critically revised the scientific content of the manuscript, reviewed the manuscript and approved the final version of the manuscript for publication.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This prospective, observational study was approved by the institutional review board (IRB) of the King Abdullah International Medical Research Center, Riyadh, Arabia (Reference RC19/213/R). Informed consent was obtained from all participants. All experiments were performed in accordance with relevant ethical guidelines and regulations including the Declaration of Helsinki.
Consent for publication
No identifiable data from individual subjects is included in this paper.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Rajendram, R., Alrasheed, A.O., Boqaeid, A.A. et al. Investigating medical students’ perceptions of point-of-care ultrasound integration into preclinical education. BMC Med Educ 24, 1513 (2024). https://doi.org/10.1186/s12909-024-06501-z
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1186/s12909-024-06501-z