Abstract
Background
Pain management is an important part of nursing care for children. The objective of this study was to systematically assess the impact of virtual reality (VR) technology on alleviating the pain and anxiety experienced by children during venipuncture procedures.
Methods
This study searched Pubmed, Web of Sciences, Scopus, The Cochrane Library, Cumulative Index of Nursing and Allied Health Literature (CINAHL), Embase, Medline, China National Knowledge Infrastructure (CNKI), Wanfang, Weipu and China biomedical databases on the randomized controlled trials (RCTs) of virtual reality technology for relieving pain and anxiety associated with venous puncture for children up to July 6, 2024. Risk of bias tool recommended by Cochrane library was used to evaluate the RCT quality. RevMan 5.3 software was used for statistical analysis.
Results
A total of 10 RCTs involving 874 children were included. 429 children received VR intervention during vein puncture. VR was beneficial to reduce the children’s self-reported pain scores [SMD=-0.48, 95% CI (− 0.61, − 0.35)], children’s caregivers reported needle-related pain level [SMD=-0.93, 95% CI (-1.45, − 0.42)], children’s self-reported anxiety scores [SMD=-0.45, 95% CI (− 0.65, − 0.25)], children’s caregivers reported needle-related anxiety level [SMD=-0.47, 95% CI (− 0.73, − 0.21)]. Egger regression tests indicated that there were no publication biases in the synthesized outcomes (all P > 0.05).
Conclusions
VR technology has been shown to effectively mitigate the pain and anxiety experienced by children during venipuncture. Despite the positive findings, more research is needed to better understand the role of VR in children undergoing venipuncture.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The International Association for the Study of Pain (IASP) [1] defines pain as an unpleasant feeling, emotional experience, or similar experience related to actual or potential tissue damage. The Joint Commission on Accreditation of Healthcare Organizations (JCAHO) has identified pain as the fifth vital sign after body temperature, pulse, respiration and blood pressure [2]. In clinical work, nursing puncture operations, such as intravenous infusion, injection, blood collection and vaccination, can cause patients, especially children, to feel pain, but nurses often do not pay enough attention to such pain [3]. Because children’s cognitive function is not yet mature, their pain threshold is lower than that of adults [4]. Especially during medical procedures that involve pain, children often encounter unpredictable and potentially distressing stimuli. These experiences can have significant adverse effects both in the short and long term. Immediate physiological responses may include an increased heart rate and elevated blood pressure. Psychologically, there can be a lasting impact, such as the development of fear and distrust towards medical and healthcare professionals. It is therefore essential to address these concerns to ensure the overall well-being and positive health outcomes for children in medical settings [5, 6]. For their caregivers, seeing children experience pain will also bring traumatic experience to parents, increase work pressure for pediatric nurses and easily lead to nurse patient conflicts. Furthermore, Children, due to their immature physical and mental development and relatively poor cognitive abilities, tend to experience anxiety more readily than adults when confronted with unfamiliar environments and strangers [7]. As high as 86.82% of pediatric patients have experienced severe fear and anxiety during venipuncture [8]. Consequently, effective management of pain and anxiety is a crucial component of the clinical nursing care provided during venipuncture in pediatric patients.
With the development of information technology, visual reality (VR) technology, as a new intervention method based on distraction, plays an important role in reducing patients’ pain [9]. VR technology provides a rich, multisensory experience by engaging multiple senses simultaneously. It presents a range of stimuli such as captivating visual images, three-dimensional (3D) spatial audio, and interactive tactile and olfactory feedback. This comprehensive sensory environment significantly enhances the user’s sense of immersion and engagement [10]. By strategically leveraging the finite cognitive resources of attention, the technology effectively redirects individuals’ focus from the “real world” to the captivating realm of the virtual. This transition moves the spotlight away from potentially harmful stimuli and towards more benign or even enjoyable events, consequently alleviating the burden of pain that individuals may be experiencing [11]. At present, VR technology has been widely used in cancer patients’ symptom management, post stroke rehabilitation training, chronic pain and other fields, and has achieved good results [12, 13], but the role of VR technology in children undergoing puncture operations remain unclear. In recent years, many studies [14,15,16] have explored the potential of virtual reality (VR) technology to mitigate pain symptoms in patients undergoing puncture operations. However, the sample sizes across these studies have varied significantly, leading to a range of findings. Given this context, the aim of this meta-analysis is to conduct a systematic evaluation of the effectiveness of VR technology in reducing pain and anxiety associated with venous puncture procedures in pediatric patients, to contribute valuable evidence to inform clinical nursing practices and enhance patient care.
Methods
We performed this meta-analysis in accordance to the preferred reporting items for systematic reviews and meta-analyses (PRISMA) statement [17].
Literature search
Two investigators searched Pubmed, Web of Science, Scopus, The Cochrane Library, Cumulative Index of Nursing and Allied Health Literature (CINAHL), Embase, Medline, China National Knowledge Infrastructure (CNKI), Wanfang, Weipu and China biomedical databases on the randomized controlled trials (RCTs) of virtual reality technology on relieving pain and anxiety related to venous puncture for children. The search time set in the databases was from the inception to July 6, 2024. The search strategy (supplementary file 1) of this meta-analysis was as follows: (“virtual reality” OR “digital technology” OR “VR” OR “immersi*” OR “distract*”) AND (“child” OR “pediatric” OR “children”) AND (“intramuscular injection” OR “vaccination” OR “venipuncture” OR “intravenous” OR “injection” OR “invasive procedure " OR “vascular access” OR “ blood draw” OR “port access” OR “needle–related procedurel” OR “subcutaneous injection” OR “intravenous cannulation” OR “intradermal injection” OR “intravenous line” OR “IV”). Besides, we had traced the references of the included RCTs and related reviews to avoid any missing literature. During the course of this study, the expertise and guidance of a librarian were actively sought to facilitate research and information gathering.
Inclusion and exclusion criteria
The inclusion criteria of this meta-analysis were as following: The study was RCT design; the study population were children aged 3–12 years who needed nursing puncture related procedures; The intervention group received virtual reality technology intervention during puncture related operation, while the control group received routine nursing intervention during puncture related operation; The primary outcome measure was the self-reported pain and anxiety score of the children, and the secondary outcome measure was the pain and anxiety score of the children reported by the primary caregiver. The pain and anxiety assessment tools mainly included Wong Baker Faces Pain Scale (WBFPS), Visual Analogue Scale (VAS), Revised Face Pain Scale (FPS-R), Children’s Fear Scale (CFS) and Facial Affective Scale (FAS). The scope of our review was restricted to publications documented in Chinese and English languages. In the process of compiling the literature, we meticulously excluded any studies that were found to be duplicates, as well as those deemed of low quality due to significant flaws in their research design or the presence of incomplete data.
Literature screening and data extraction.
Two researchers independently conducted the literature screening process, adhering strictly to the predefined inclusion and exclusion criteria. They initially reviewed the titles and abstracts of identified studies, followed by a full-text review to assess eligibility. The information was extracted from the selected literature. The screening results were then cross-verified to ensure consistency. Any discrepancies that arose between the two researchers were resolved through discussion to reach a consensus. The information extracted from this meta-analysis mainly included the first author, publication time, country, sample size, study population, age, gender, intervention measures, outcome indicators.
Quality evaluation
This meta-analysis employed the Risk of Bias Tool for RCTs, as recommended by the Cochrane Library, to assess the quality of the included literature [18]. The quality assessment tool encompasses several key domains: the method of random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, completeness of outcome data, selective reporting, and other potential sources of bias. Each domain was rated as having either a “high risk of bias,” a “low risk of bias,” or being “unclear.” The quality evaluation was conducted independently by two researchers. In instances where discrepancies arose, a third researcher was engaged to reach a consensus on the final evaluation. This rigorous approach ensures the reliability and integrity of the findings within the meta-analysis.
Statistical methods
EndNote 21 software was employed to efficiently manage data and references throughout the research process. This meta-analysis used RevMan 5.3 software for statistical analysis. If there was no heterogeneity among the results (P > 0.1, I2 < 50%), the fixed effect model was used for synthesized analysis. If there was heterogeneity (P ≤ 0.1, I2 > 50%), we used the random effect model to perform synthesized analysis. The outcome indicators analyzed in this meta-analysis were continuous variables, and the evaluation tools of each test indicator might be different, the standardized mean difference (SMD) was used as the effect indicator, and 95% confidence interval(95%CI) was calculated as the effect statistic. Sensitivity analyses was conducted on all outcomes after excluding studies with an uncertain or high risk of bias. Funnel plots and Egger regression test were used to evaluate the Publication bias of included RCTs. P < 0.05 indicated that the difference between groups was statistically significant.
Results
Study inclusion
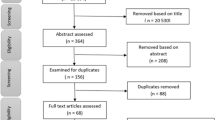
The initial search yielded a total of 715 pertinent articles. Upon the elimination of duplicates, 696 publications were subjected to initial screening. Following a review of the titles and abstracts, 643 articles were excluded, leaving 62 for further assessment through full-text evaluation. Adhering to the defined inclusion and exclusion criteria, a total of 10 RCTs [19,20,21,22,23,24,25,26,27,28], were ultimately included in this meta-analysis. The study selection process is visually depicted in Fig. 1.
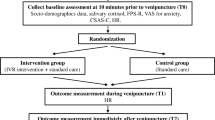
Characteristics of included RCTs
Of the included 10 RCTs [19,20,21,22,23,24,25,26,27,28], a total of 874 children involved, 429 children received VR intervention during vein puncture, 445 children received routine care during vein puncture. The included RCTs were conducted and reported from different countries. The characteristics of included RCTs are shown in Table 1.
Quality of included RCTs
The quality included in RCTs was generally good. All RCTs reported specific random grouping methods, and 4 studies [22,23,24, 28] did not report allocation hiding, which might cause researchers to report tendentiously. 6 studies [20, 21, 23, 24, 27, 28] reported no blind design. All studies clearly defined the inclusion and exclusion criteria, and described the gender, age and other baseline data of the two groups of children. The quality of included RCTs is shown in Figs. 2 and 3.
Synthesized outcomes
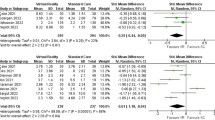
Children’s self-reported needle-related pain level All 10 studies [19,20,21,22,23,24,25,26,27,28] reported the self-reported pain scores for children. There was no heterogeneity among the studies (P = 0.06, I2 = 45%), and the fixed effect model was used for analysis. The results showed that VR technology was beneficial to reduce the children’s self-reported pain scores [SMD=-0.48, 95% CI (− 0.61, − 0.35), P < 0.001], as shown in Fig. 4a.
Children’s caregivers reported needle-related pain level 5 studies [20, 22, 24, 26, 27] reported the children’s caregivers reported pain scores for children. There was heterogeneity among the studies (P < 0.001, I2 = 86%), and the random effect model was used for analysis. The results showed that VR technology was beneficial to reduce the children’s caregivers reported needle-related pain level [SMD=-0.93, 95% CI (-1.45, − 0.42), P < 0.001], as shown in Fig. 4b.
Children’s self-reported needle-related anxiety level 4 studies [20, 21, 24, 28] reported the children’s self-reported needle-related anxiety level. There was no heterogeneity among the studies (P = 0.12, I2 = 49%), and the fixed effect model was used for analysis. The results showed that VR technology was beneficial to reduce the children’s self-reported anxiety scores [SMD=-0.45, 95% CI (− 0.65, − 0.25), P < 0.001], as shown in Fig. 5a.
Children’s caregivers reported needle-related anxiety level 2 studies [20, 24] reported the children’s caregivers reported needle-related anxiety level. There was no heterogeneity among the studies (P = 0.67, I2 = 0%), and the fixed effect model was used for analysis. The results showed that VR technology was beneficial to reduce the children’s caregivers reported needle-related anxiety level [SMD=-0.47, 95% CI (− 0.73, − 0.21), P < 0.001], as shown in Fig. 5b.
Publication biases and sensitivity analyses
The funnel plots for synthesized outcomes are shown in Fig. 6. The dots were evenly distributed in the funnel plots, and Egger regression test results indicated there were no publication biases in the synthesized outcomes (all P > 0.05).
Sensitivity analyses, which evaluate the influence of one study on the overall risk estimate by removing study one by one, indicated that the overall risk estimate results were not substantially changed by any single RCT.
Discussions
At present, the pain management in children is usually inadequate, and the presence of pain may have a negative impact on children’s future pain response [29]. Previous studies [30,31,32] have pointed out that pain assessment should be carried out during admission, operation or invasive operation, department transfer, and disease development. The appropriate pain assessment scale should be selected before, during and after the puncture operation and the pain should be assessed accordingly [33]. It is necessary for pediatric nurses to provide comfortable care for foreseeable painful operations or diagnosis and treatment methods to minimize the adverse effects of pain on children [34, 35]. The results of this study have found that VR technology reduces the pain and anxiety of children undergoing vein puncture, which should be promoted in clinical nursing care of children.
At present, the mechanism of VR technology to alleviate pain is still under exploration. Relevant research [36] uses the attention theory or gate theory to explain, that is, the perception of pain requires attention. Effective engagement with VR can significantly divert the brain’s attentional resources, which are usually directed towards processing pain, thereby leading to a decrease in the perceived intensity of pain. In medical procedures like punctures, the strategic use of VR technology can encourage children to become deeply immersed in a captivating, engaging, and realistic digital environment. This is facilitated by multisensory stimulation that encompasses sight, sound, and touch. This stimulation not only piques the child’s interest but also serves to effectively reduce their awareness and sensitivity to pain, enhancing the overall comfort and ease of the procedure [37,38,39]. Previous researches [40, 41] have elucidated the neuroanatomical underpinnings of pain perception, demonstrating that exposure to painful stimuli is correlated with increased activity in pain matrix areas, such as the insula and thalamus. When patients undergo VR intervention, functional magnetic resonance imaging (fMRI) has revealed a significant reduction in the activity of these individual pain matrix areas—by more than 50%. This neuroimaging evidence aligns well with the subjective reports of decreased pain scores from patients who have received VR interventions. Additionally, several studies [40, 41] has highlighted the potential of virtual reality (VR) technology to enhance patients’ pain tolerance. This is achieved by mitigating the negative emotions associated with the experience and by shortening the duration it takes for patients to perceive pain. The immersive nature of VR serves as a distraction, effectively redirecting the patient’s attention away from the source of discomfort, thereby reducing the overall sensation of pain. This approach represents a promising avenue for improving the patient experience, particularly in pediatric populations where the management of pain and anxiety during medical procedures is of paramount importance. Therefore, the intervention of VR technology is of great significance to the management of puncture related pain in nursing care of children.
VR technology is helpful the pain management and care of children undergoing puncture operations. Untreated pain may lead to negative psychology in children, and severe pain may have a destructive impact on their future pain perception, so pain management is particularly important [42]. Previous study [43] has found that if children’s attention is focused on events other than nursing puncture operations, the pain signals transmitted to their brain will be reduced accordingly, and children will temporarily forget the pain they are experiencing. This study has demonstrated that VR technology can effectively alleviate the pain experienced by children during nursing punctures, as perceived from the viewpoints of both the children and their primary caregivers. Notably, children, being the direct subjects of pain perception, provide the most pertinent insights through their self-reported pain scores. However, it is important to recognize that their individual experiences of pain can vary significantly due to differences in age, cognitive abilities, and levels of understanding. Furthermore, the primary caregiver, who is well-acquainted with the child’s baseline condition and typical responses to pain, offers a valuable perspective when reporting on the child’s experience of pain. Their observations complement the child’s self-assessment and provide a more comprehensive understanding of the child’s pain and anxiety levels during the procedure. Overall, the study underscores the importance of considering multiple perspectives when evaluating the effectiveness of interventions like VR technology in pediatric pain management. By incorporating the viewpoints of both children and their caregivers, a more holistic and accurate assessment of the intervention’s impact can be achieved.
The results of this study have shown that VR technology can alleviate puncture related anxiety of children. A recent study [44] has shown that compared with the control group, the anxiety scores of children with anxiety disorder who received VR intervention are significantly lower. Some studies [45,46,47] have shown that high anxiety levels may worsen individual pain experience, lead to lower pain threshold, and further stimulate children’s pain response and anxiety symptoms. VR technology enables children to maintain a sense of pleasure, achieve a state of physical and mental relaxation, and eliminate anxiety through visual images and auditory stimulation [48,49,50]. By obstructing the child’s view of the clinical environment, the VR devices can mitigate the fear and anxiety that children may experience due to the unfamiliar and often intimidating surroundings. Additionally, VR headsets effectively block out adverse auditory stimuli from the environment, such as the sounds of medical equipment or procedures, which can be distressing for young patients [51, 52]. Therefore, VR intervention effectively alleviates the anxiety of children caused by nursing puncture operations.
The limitations of this study are worth considering. First of all. Given the rapid evolution of VR technology, the pertinence of findings from Gold in the year of 2006 [23] is questionable, particularly in light of the significant technological advancements that have occurred since then. The VR equipment type, intervention content, basic diseases of children and nursing puncture received are different, which may increase the heterogeneity of combined results. Secondly, this meta-analysis only includes Chinese and English reported literature, there may be articles published in other language that could not be included for analysis. Thirdly, we do not have information or data regarding that if the children have exposure to venipuncture prior to this event, this can significantly influence the pain level and other outcomes of children, more studies on this issue in the future are needed. Fourthly, different research tools for anxiety and pain assessment may have different effects on the results of meta-analysis. Even if we chose MD for data synthesis, there was still a potential risk of bias. Finally, it is noteworthy that the safety of VR interventions has not been explicitly reported in the studies reviewed. Consequently, there is a clear need for future research to delve into both the application effects and the safety profile of VR technology within the context of clinical venipuncture nursing. This should be approached through large-scale, high-quality studies that can provide more definitive insights into the potential benefits and risks associated with VR use in this setting.
Conclusions
In summary, VR technology has demonstrated the potential to effectively alleviate the pain and anxiety associated with pediatric venipuncture procedures. It is recommended that future research include a comprehensive safety report on VR interventions to ensure patient well-being. Future studies could benefit from incorporating a broader range of evaluation metrics, such as heart rate, blood pressure, respiration rate, and patient satisfaction surveys. These indicators can provide a more holistic assessment of the intervention’s impact. Besides, there is a pressing need for more high-quality, multicenter, and large-sample studies to further evaluate the clinical utility and efficacy of VR technology in pediatric nursing. Such research endeavors will be instrumental in establishing evidence-based guidelines for VR use, ensuring that this promising tool is employed in a manner that is both safe and maximally effective in managing pain and anxiety during pediatric venipuncture procedures.
Data availability
All data generated or analyzed during this study are included in this published article.
Abbreviations
- CINAHL:
-
Nursing and Allied Health Literature
- CNKI:
-
China National Knowledge Infrastructurek
- RCTs:
-
Randomized controlled trials
- PRISMA:
-
Preferred reporting items for systematic reviews and meta-analyses
- WBFPS:
-
Wong Baker Faces Pain Scale
- VAS:
-
Visual Analogue Scale
- FPS-R:
-
Revised Face Pain Scale
- CFS:
-
Children’s Fear Scale
- FAS:
-
Facial Affective Scale
- SMD:
-
Standardized mean difference
- CI:
-
Confidence interval
References
Raja SN, Carr DB, Cohen M, Finnerup NB, Flor H, Gibson S, Keefe FJ, Mogil JS, Ringkamp M, Sluka KA, et al. The revised International Association for the study of Pain definition of pain: concepts, challenges, and compromises. Pain. 2020;161(9):1976–82.
Merboth MK, Barnason S. Managing pain: the fifth vital sign. Nurs Clin North Am. 2000;35(2):375–83.
Zhang Y, Yan F, Li S, Wang Y, Ma Y. Effectiveness of animal-assisted therapy on pain in children: a systematic review and meta-analysis. Int J Nurs Sci. 2021;8(1):30–7.
Andersson V, Bergman S, Henoch I, Simonsson H, Ahlberg K. Pain and pain management in children and adolescents receiving hospital care: a cross-sectional study from Sweden. BMC Pediatr. 2022;22(1):252.
Whitley GA, Hemingway P, Law GR, Siriwardena AN. Improving ambulance care for children suffering acute pain: a qualitative interview study. BMC Emerg Med. 2022;22(1):96.
Payson A, Pulido A, San Martin S, Garlesky C, Garcia E, Reyes C, Reyes M, Leyenaar J. Inequities in Pain Assessment and Care of Hospitalized Children with Limited English proficiency. Hosp Pediatr. 2022;12(6):561–8.
Xu M, Mao B, Zhang X. The effect of strengthening nurse-patient communication skills on improving the success rate of emergency infusion puncture. China Health. 2022;25(3):10–4.
Shen L, Su Y. Effect of humanized nursing model intervention on painless puncture compliance and stress response in children with intravenous infusion. Women’s Children’s Health Guide. 2022;15(2):1–3.
Perez Torres TDCB, Morente Sanchez JA, Escobar Castellanos L, Escobar Fernandez M, Gonzalez Sanchez L, Rodriguez Fernandez MI. [Reducing the pain in invasive procedures during paediatric hospital admissions: fiction, reality or virtual reality?]. Pediatr (Engl Ed). 2019;91(2):80–7.
Addab S, Hamdy R, Thorstad K, Le May S, Tsimicalis A. Use of virtual reality in managing paediatric procedural pain and anxiety: an integrative literature review. J Clin Nurs. 2022;31(21–22):3032–59.
Spiegel B, Fuller G, Lopez M, Dupuy T, Noah B, Howard A, Albert M, Tashjian V, Lam R, Ahn J, et al. Virtual reality for management of pain in hospitalized patients: a randomized comparative effectiveness trial. PLoS ONE. 2019;14(8):e0219115.
Xiang H, Shen J, Wheeler KK, Patterson J, Lever K, Armstrong M, Shi J, Thakkar RK, Groner JI, Noffsinger D, et al. Efficacy of smartphone active and Passive virtual reality distraction vs Standard Care on burn Pain among Pediatric patients: a Randomized Clinical Trial. JAMA Netw Open. 2021;4(6):e2112082.
Bergomi P, Scudeller L, Pintaldi S, Dal Molin A. Efficacy of non-pharmacological methods of Pain Management in Children undergoing venipuncture in a Pediatric Outpatient Clinic: a Randomized Controlled Trial of Audiovisual Distraction and External Cold and Vibration. J Pediatr Nurs. 2018;42:e66–72.
Wang L, Zhang Y, He Y, Tang L, Zhao J. Preliminary construction of virtual reality system of jugular vein puncture based on SOFA. China Med Equip. 2018;33(2):6–9.
Yu Q, Feng L. Application of virtual reality technology combined with early local infiltration anesthesia in PICC catheterization of school-age children. Nurs Res. 2023;37(5):918–21.
Tao M, Zhu H, Wu C. Application of virtual reality technology in patients with P ICC catheterization in hematology department. Qilu J Nurs. 2021;27(18):2–6.
Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. 2021;372:n160.
Sterne JAC, Savovic J, Page MJ, Elbers RG, Blencowe NS, Boutron I, Cates CJ, Cheng HY, Corbett MS, Eldridge SM, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898.
Aydin AI, Ozyazicioglu N. Using a virtual reality headset to decrease Pain Felt during a Venipuncture Procedure in Children. J Perianesth Nurs. 2019;34(6):1215–21.
Chen YJ, Cheng SF, Lee PC, Lai CH, Hou IC, Chen CW. Distraction using virtual reality for children during intravenous injections in an emergency department: a randomised trial. J Clin Nurs. 2020;29(3–4):503–10.
Dumoulin S, Bouchard S, Ellis J, Lavoie KL, Vezina MP, Charbonneau P, Tardif J, Hajjar A. A Randomized Controlled Trial on the use of virtual reality for needle-related procedures in children and adolescents in the Emergency Department. Games Health J. 2019;8(4):285–93.
Erdogan B, Aytekin Ozdemir A. The Effect of three different methods on Venipuncture Pain and anxiety in children: distraction cards, virtual reality, and Buzzy(R) (Randomized Controlled Trial). J Pediatr Nurs. 2021;58:e54–62.
Gold JI, Kim SH, Kant AJ, Joseph MH, Rizzo AS. Effectiveness of virtual reality for pediatric pain distraction during i.v. placement. Cyberpsychol Behav. 2006;9(2):207–12.
Gold JI, Mahrer NE. Is virtual reality Ready for Prime Time in the Medical Space? A Randomized Control Trial of Pediatric virtual reality for Acute Procedural Pain Management. J Pediatr Psychol. 2018;43(3):266–75.
Hsu MF, Whu YW, Lin IC, Liu CY, Lai FC, Liu PC, Chen CW. Effectiveness of virtual reality interactive play for children during Intravenous Placement: a Randomized Controlled Trial. Asian Nurs Res (Korean Soc Nurs Sci). 2022;16(2):87–93.
Koc Ozkan T, Polat F. The effect of virtual reality and Kaleidoscope on Pain and anxiety levels during venipuncture in children. J Perianesth Nurs. 2019;35(2):206–11.
Ozalp Gerceker G, Ayar D, Ozdemir EZ, Bektas M. Effects of virtual reality on pain, fear and anxiety during blood draw in children aged 5–12 years old: a randomised controlled study. J Clin Nurs. 2020;29(7–8):1151–61.
Piskorz J, Czub M. Effectiveness of a virtual reality intervention to minimize pediatric stress and pain intensity during venipuncture. J Spec Pediatr Nurs 2018, 23(1).
Gerceker GO, Bektas M, Aydinok Y, Oren H, Ellidokuz H, Olgun N. The effect of virtual reality on pain, fear, and anxiety during access of a port with huber needle in pediatric hematology-oncology patients: Randomized controlled trial. Eur J Oncol Nurs. 2021;50:101886.
Fuller C, Huang H, Thienprayoon R. Managing Pain and Discomfort in Children with Cancer. Curr Oncol Rep. 2022;24(8):961–73.
Drake-Brockman TFE, Smallbone HE, Sommerfield D, von Ungern-Sternberg BS. Remote after-care using smartphones: a feasibility study of monitoring children’s pain with automated SMS messaging. Paediatr Anaesth. 2022;32(8):954–60.
Dugan MQ, Delgado JR, De Souza E, Anderson TA. Pediatric chronic post-surgical pain prevalence, pain scores, and quality-of-life: results of an exploratory patient survey at a single-center tertiary care children’s hospital. J Anesth. 2022;36(5):606–11.
Lee HN, Bae W, Park JW, Jung JY, Hwang S, Kim DK, Kwak YH. Virtual reality environment using a dome screen for procedural pain in young children during intravenous placement: a pilot randomized controlled trial. PLoS ONE. 2021;16(8):e0256489.
Bak J, Zarzycka D, Mazur A. Coping with pain: Polish versions of the Pain Coping Questionnaire for both children and parents. Pain Manag. 2022;12(4):487–97.
Fang Y, Silin Z, Li J. The application of clown care in the venipuncture of preschool children. J Nurs. 2022;37(6):3–6.
Bannister K, Sachau J, Baron R, Dickenson AH. Neuropathic Pain: mechanism-based therapeutics. Annu Rev Pharmacol Toxicol. 2020;60:257–74.
Smith KL, Wang Y, Colloca L. Impact of virtual reality technology on Pain and anxiety in Pediatric burn patients: a systematic review and Meta-analysis. Front Virtual Real 2022, 2.
Li T, Fu Y, Yang Y, Zhou YE. Control effect of virtual reality technology on procedural pain in children’s wound: a meta-analysis. Med (Baltim). 2022;101(40):e30961.
Liu KY, Ninan SJ, Laitman BM, Goldrich DY, Iloreta AM, Londino AV. 3rd: virtual reality as distraction analgesia and Anxiolysis for Pediatric Otolaryngology procedures. Laryngoscope. 2021;131(5):E1714–21.
Lee SY, Cha JY, Yoo JW, Nazareno M, Cho YS, Joo SY, Seo CH. Effect of the application of virtual reality on Pain Reduction and Cerebral Blood Flow in Robot-assisted gait training in burn patients. J Clin Med 2022, 11(13).
Kardon A, Murray RS, Khalid M, Colloca L, Simard JM, Badjatia N, Murthi SB, Morris NA. Pain Control and Anxiolysis after Subarachnoid Hemorrhage using immersive virtual reality: a Case Report. Neurohospitalist. 2022;12(3):563–6.
Suleman SK, Atrushi A, Enskar K. Effectiveness of art-based distraction on reducing pediatric patients’ pain and anxiety during venipuncture: a randomized controlled trial. Complement Ther Clin Pract. 2022;48:101597.
Jinyumei, Yangyang H, Caihong W. Summary of the best evidence for pain management of children’s peripheral venous puncture. J Nurse Train. 2022;37(17):6–9.
Xiaole Z, Genzhen Y. Application of children’s medical counseling in venipuncture of children with chronic kidney disease. J Nurs Adm Manag. 2021;15(5):11–4.
Gold JI, Belmont KA, Thomas DA. The neurobiology of virtual reality pain attenuation. Cyberpsychol Behav. 2007;10(4):536–44.
Moore DJ, Keogh E, Eccleston C. The effect of threat on attentional interruption by pain. Pain. 2013;154(1):82–8.
Pourmand A, Davis S, Marchak A, Whiteside T, Sikka N. Virtual reality as a clinical Tool for Pain Management. Curr Pain Headache Rep. 2018;22(8):53.
Guenther M, Gorlich D, Bernhardt F, Pogatzki-Zahn E, Dasch B, Krueger J, Lenz P. Virtual reality reduces pain in palliative care-A feasibility trial. BMC Palliat Care. 2022;21(1):169.
Diaz-Rodriguez M, Alcantara-Rubio L, Aguilar-Garcia D, Perez-Munoz C, Carretero-Bravo J, Puertas-Cristobal E. The Effect of Play on Pain and anxiety in children in the field of nursing: a systematic review. J Pediatr Nurs. 2021;61:15–22.
de la Cruz Herrera M, Fuster-Casanovas A, Miro Catalina Q, Cigarran Mensa M, Alcantara Pinillos P, Vilanova Guitart I, Grau Carrion S, Vidal-Alaball J. Use of virtual reality in the reduction of Pain after the administration of vaccines among children in Primary Care centers: protocol for a Randomized Clinical Trial. JMIR Res Protoc. 2022;11(4):e35910.
Kaya M, Karaman Ozlu Z. The effect of virtual reality on pain, anxiety, and fear during burn dressing in children: a randomized controlled study. Burns 2022.
Wang Q, Xu S, Guo B, Xu Y, Lu W. Virtual reality as an adjunctive non-pharmacological therapy to reduce pain in school-aged children with burn wounds. J Burn Care Res 2022.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
Q W, R S designed research; Q W, R S, Y L, D C conducted research; Q W, R S, Y L analyzed data; Q W, D C wrote the first draft of manuscript; D C had primary responsibility for final content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
In this study, all methods were performed in accordance with the relevant guidelines and regulations. Ethics approval and consent to participate are not necessary since our study is a meta-analysis.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it.The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wei, Q., Sun, R., Liang, Y. et al. Virtual reality technology reduces the pain and anxiety of children undergoing vein puncture: a meta-analysis. BMC Nurs 23, 541 (2024). https://doi.org/10.1186/s12912-024-02184-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12912-024-02184-5