Abstract
Background
Non-adherence to recommended therapy remains a challenge to achieving optimal clinical outcome with resultant economic implications.
Objective
To evaluate the effect of a pharmacist-led intervention on treatment non-adherence and direct costs of management among patients with type 2 diabetes (T2D).
Method
A quasi-experimental study among 201-patients with T2D recruited from two-tertiary healthcare facilities in southwestern Nigeria using semi-structured interview. Patients were assigned into control (HbA1c < 7%, n = 95) and intervention (HbA1c ≥ 7%, n = 106) groups. Baseline questionnaire comprised modified 4-item Medication Adherence Questions (MAQ), Perceived Dietary Adherence Questionnaire (PDAQ) and International Physical Activity Questionnaire, to assess participants’ adherence to medications, diet and physical activity, respectively. Post-baseline, participants were followed-up for 6-month with patient-specific educational intervention provided to resolve adherence discrepancies in the intervention group only, while control group continued to receive usual care. Subsequently, direct costs of management for 6-month pre-baseline and 6-month post-baseline were estimated for both groups. Data were summarized using descriptive statistics. Chi-square, McNemar and paired t-test were used to evaluate categorical and continuous variables at p < 0.05.
Results
Mean age was 62.9 ± 11.6 years, and 160(79.6%) were females. Glycated haemoglobin (HbA1c) was 6.1 ± 0.6% (baseline) and 6.1 ± 0.8% at 6-month post-baseline (p = 0.094) for control group, and 8.7 ± 1.5% (baseline) versus 7.8 ± 2.0% (6-month), p < 0.001, for the intervention. Post-baseline, response to MAQ items 1 (p = 0.017) and 2 (p < 0.001) improved significantly for the intervention. PDAQ score increased significantly from 51.8 ± 8.8 at baseline to 56.5 ± 3.9 at 6-month (p < 0.001) for intervention, and from 56.3 ± 4.0 to 56.5 ± 3.9 (p = 0.094) for the control group. Physical activity increased from 775.2 ± 700.5 Metabolic Equivalent Task (MET) to 829.3 ± 695.5MET(p < 0.001) and from 901.4 ± 743.5MET to 911.7 ± 752.6MET (p = 0.327) for intervention and control groups, respectively. Direct costs of management per patient increased from USD 327.3 ± 114.4 to USD 333.0 ± 118.4 (p = 0.449) for the intervention, while it decreased from USD 290.1 ± 116.97 to USD289.1 ± 120.0 (p = 0.89) for control group, at baseline and 6-month post-baseline, respectively.
Conclusion
Pharmacist-led intervention enhanced adherence to recommended medications, diet and physical activity among the intervention patients, with a corresponding significant improvement in glycaemic outcome and an insignificant increase in direct costs of management. There is a need for active engagement of pharmacists in management of patients with diabetes in clinical practice.
Trial registration
ClinicalTrials.gov identifier: NCT04712916. Retrospectively-registered.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Diabetes is one of the common non-communicable diseases worldwide [1]. The World Health Organisation (WHO) has reported that the prevalence of diabetes is rapidly increasing in low- and middle-income countries (LMICs) [2]. In Africa, 14.7 million adults are estimated to have diabetes, with Nigeria having the largest number of people with diabetes in Africa [3, 4]. The WHO estimates that about 1.7 million people are living with diabetes in Nigeria, which is expected to increase to 4.8 million by the year 2030 [4,5,6]. About one-quarter to one-third of all hospitalisation in medical (nonsurgical) wards in Nigeria have been linked to diabetes and its associated complications [7, 8]. Generally, in Nigeria, patients with diabetes either in ambulatory or institutionalised care typically make out-of-pocket payment for all their treatment expenses. There is no subsidy provision for the general populace as at present. However, few employees from organised private sector or government-owned public institutions, who might have enrolled under the National Health Insurance Scheme (NHIS) are required to pay only 10% of the total costs of treatment covering mostly the prescribed medications and laboratory investigations. In addition, both the secondary and tertiary care facilities are usually involved in treatment and care for diabetes patients, but comprehensiveness of management received by the patients may relatively differ between the two tiers, especially in relation to the diverse medical specialties and higher number of medical consultants in the tertiary hospitals.
In many LMICs including Nigeria, patients with diabetes faced varying challenges, ranging from lack of access to adequate medical facilities, socio-economic problems, to experience of fluctuating magnitude of disease complications [9, 10]. However, the goal of management for diabetes requires optimal adherence to recommended therapies, in order to achieve optimal clinical outcomes, and subsequently a reduced healthcare cost [11, 12]. In many developed and developing countries, it is estimated that about 50 to 60% of patients with chronic diseases including diabetes are non-adherent to prescribed therapies [13,14,15]. Specifically, in most developing countries, poor adherence to prescribed therapies among ambulatory patients with diabetes is a growing concern for healthcare providers and patients [15,16,17], partly because of its adverse consequences on therapeutic outcomes [18,19,20]. Non-adherence is especially high among patients with chronic diseases including diabetes mellitus largely because they require long-term and sometimes complex treatment regimen to control symptoms and prevent complications [17, 21]. However, suboptimal adherence to prescribed diabetes medications has been reported to account for 30 to 50% of treatment failure and worsen treatment outcomes with the attendant complications [9, 10]. Previous studies have also reported that patients with diabetes who are non-adherent had both statistically and clinically worse outcomes than their adherent counterparts [22, 23]. In addition, poor glycaemic control among patients with diabetes is associated with reduced treatment benefits, as well as increased financial burden on both patients and the society [24,25,26]. The challenge of treatment non-adherence among these patients may perhaps be averted if patients are adequately counseled on the necessity for optimal commitment to prescribed therapies, while non-adherent behaviours appropriately resolved [27,28,29,30]. Studies in many developed countries have reported improvement in medication adherence and clinical outcomes in pharmacist-conducted medication management among patients with diabetes [29, 31,32,33]. Also, it has been shown that a high level of medication adherence is associated with lower disease-related medical costs [12, 34]. The more patients adhered to therapy, the better the achievement of good clinical outcome, and the less is the length of hospitalisation and costs of management [12, 35,36,37].
Although, studies in some developed countries have related poor glycaemic control to higher healthcare costs [36,37,38]. Also, there had been studies conducted in LMICs including Nigeria to explore medication adherence and glycaemia among ambulatory patients with diabetes [17, 14, 25, 39], and a few on adherence to physical activity and dietary recommendations [40, 41]. However, none of these studies from developing countries comprehensively explore the interplay between treatment adherence, clinical outcomes and associated costs of management among patients with type 2 diabetes. This study therefore employed validated tools to evaluate therapy adherence and patient-specific reasons for non-adherence among ambulatory patients with type 2 diabetes in two tertiary hospitals, who had good glycaemia (HbA1c < 7%; control group) and those with poor glycaemia (HbA1c ≥ 7%; intervention group). We also evaluated the effect of pharmacist-led educational intervention in resolving identified adherence discrepancies on medications, diet and physical activity among patients in the intervention group only. Direct costs of management including transportation, consultation, medications and laboratory investigations for 6-month pre-baseline and 6-month post-baseline were subsequently estimated for both groups.
Method
Study site
University College Hospital (UCH) Ibadan, Oyo State and Federal Medical Centre (FMC) Abeokuta, Ogun State. The UCH is a 900-bed teaching hospital and is affiliated with University of Ibadan, Oyo state, Nigeria. The FMC is a 350-bed hospital and serves as a teaching hospital for BABCOCK University in Ogun state, Nigeria.
Study design
A quasi-experimental study among T2D patients recruited from the two hospitals using questionnaire-guided semi-structured interview. At baseline, participants with HbA1c ≥7% (poor glycaemia) were assigned into intervention group, while those with HbA1c < 7% (good glycaemia) were considered as control group. Post-baseline, patient-specific pharmacist-led educational intervention was provided for participants in the intervention group only, to resolve adherence discrepancies in medications, diet and physical activity. The control group continued to receive usual care. At the end of 6-month post-baseline, the same questionnaire used for baseline interview was re-administered to participants in both groups to ascertain the extent of change in the measured variables at baseline. In this study, the direct costs of management defined as the sum of transport fare, consultation fee, as well as costs of medications and laboratory investigations were calculated 6-month pre-baseline and 6-month post-baseline for individual patient. The 6-month pre-baseline costs of management was estimated using key parameters garnered retrospectively from individual patient’s case note. This included date and number of clinics attended within 6-month prior to the baseline enrolment, details of prescribed medications comprising dosage form, drug name, dosage strength, frequency and duration of use, as well as diabetes-specific laboratory investigations. Total cost of transport fare was estimated by multiplying the number of clinics attended within the period by the prevailing transport cost, as indicated by each patient. The National Union of Road Transport Workers (NURTW) recommended fare for commercial/public vehicles was used as a guide. Patients were courteously asked about the rate of transport fare to the hospital during the prospective baseline interaction, while the amount/cost indicated was used to multiply the number of clinics attended within the 6-month pre-baseline. Consultation fee was calculated using the hospital’s approved fee which remained relatively stable in both hospitals within the period. Cost of medications was calculated using the price value of each medication from each hospital pharmacy unit, taking into consideration the daily dosage and duration of therapy. Also, the cost of laboratory investigations was estimated using the approved price from each hospital laboratory. Similar information was garnered and the same procedure followed to estimate the direct costs of management for the 6-month post-baseline.
Study population
Adult T2D patients attending the endocrinology out-patient clinic of each hospital.
Inclusion and exclusion criteria
Adult out-patients with primary diagnosis of T2D, who must have also been on antidiabetes medications for at least 6-month prior to the commencement of the study. Patients with Type 1 diabetes, gestational diabetes and T2D who declined participation were excluded.
Sample size determination
Average of 25 patients with T2D regularly attended the weekly medical out-patient endocrinology clinic of each hospital. This gave a total of 100 patients per month in each hospital, which translated to an estimated population of 600 T2D per hospital for the 6-month study period. However, information obtained from the medical record unit of each hospital indicated that a maximum of 2 to 6 months clinic appointment is usually given to T2D in UCH, and a maximum of 3 months appointment in FMC, depending on the extent of glycaemic control. Based on this information, and considering the regular attendees of 100 T2D patients per month in each hospital, a total of 700 T2D (400 in UCH, and 300 in FMC) was considered as estimated population to guide the calculation of sample size. Thus, using the estimated population, at 95% confidence level and 5% margin of error, the Raosoft® sample size calculator [https://www.raosoft.com/samplesize.html] gave a value of 248. However, addition of 10% attrition rate gave a target sample size of 272.8 (rounded off to 273) to guide enrolment of participants.
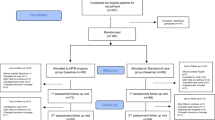
Sampling and recruitment procedure
On every diabetes clinic day of each hospital, the principal investigator first checked and screened the medical records/case notes of T2D attendees for eligibility. Eligible case notes were consecutively selected and individual patient’s hospital number was used as identification tag/code. On each clinic, eligible patients were called by their respective hospital number which is always written on each patient’s small hospital appointment card. This was done to identify the precise location of each patient while waiting for their turn of physician consultation. Subsequently, patients were approached individually to introduce the study, as well as informed them of the purpose and procedures for involvement in the study. These were clearly explained to individual patient generally in English, and specifically in the local language (Yoruba). The informed consent form as approved by the Institution Review Board (IRB) was given to individual patient to read, while clarifications were made when necessary. Elderly patients were assisted by caregivers who accompanied them to the hospital. The instrument and informed consent form were translated into Yoruba, the predominant local language of participants, while back-translation was subsequently done to ensure response consistency. Patients were individually asked to indicate their intention to participate in the study by appending written signature or thumbprint in the appropriate space provided on the informed consent form. This approach was consistently followed and assured throughout the recruitment period at baseline. Patients were assured of their anonymity and confidentiality of response and were also told that their participation in the study is voluntary. Only the eligible patients who gave voluntary informed consent were enrolled, while those who declined participation were excluded from the study. At baseline, 273 patients were approached, while 227 (83.2%) consented to partake from both hospitals within the study period. Questionnaire was administered to consented participants and diabetes-specific clinical parameters, precisely HbA1c and blood pressure (BP) were also assessed. Each participant had individualised baseline, while intervention continued for patients in the intervention group by the principal investigator. Once the 6-month duration of involvement in the study is completed, then individual participation was considered terminated. At the end of 6-month follow-up period, a total of 201 (88.5%) patients completed the study from both hospitals and were those considered for data analysis. This comprised 95 patients with good glycaemia (HbA1c < 7%; control group) and 106 patients with poor glycaemia (HbA1c ≥7%; intervention group) using the ADA target for diabetes control [42]. Twenty-six (11.5%) participants were lost to follow-up including 11 patients from control group and 15 in the intervention group. Detail of participants’ enrolment is shown in the CONSORT flow diagram/chart (Fig. 1).
Finger pin-prick blood assay of glycated haemoglobin (HbA1c) was done using point-of-care kit, while BP measurements using Omron® digital monitor were taken on two separate occasions at few minutes interval and the average value was recorded. Patients’ BP and HbA1c were also rechecked after 6-month of interaction to assess the extent of change in the diabetes-specific clinical parameters.
Data collection instrument
The baseline questionnaire comprised sections A to F. Section A captured demographic data, including monthly income and mode of medical bill payment. Section B contained modified International Physical Activity Questionnaire short-form (IPAQ-SF) [43], with individual physical activity calculated as metabolic equivalent task (MET) per week [44]. Section C consisted of modified Perceived Dietary Adherence Questionnaire (PDAQ) developed by Assad et al [45] to measure patients’ perception of dietary adherence. For these items, higher scores reflected higher level of adherence [45]. In this study, participants were classified as adherent to dietary recommendations if they score 51 (80%) and above out of the 63 maximum obtainable score, while those who scored less than 51 (80%) were classified as dietary non-adherent. Section D contained modified 4-item Medication Adherence Questions (MAQ). A ‘No’ response to all the 4-item MAQ was considered as optimal (100%) commitment to prescribed medication(s), while a ‘Yes’ response to any of the 4-item questions suggested suboptimal (< 100%) commitment to medication-taking [15, 46, 47]. Section E contained open-ended questions which explored reason(s) for non-adherence to medications, physical activity and dietary recommendations. Section F contained components of educational intervention to resolve adherence discrepancies identified in the response to question-items in MAQ, IPAQ-SF and PDAQ among patients in the intervention group. Where necessary, at least one or two clinic appointments were rescheduled to follow-up the participants in the intervention group. The 6-month post-baseline evaluation employed the same question-items in sections B, C, D and E to re-assessed participants in both control and intervention groups, with a view to ascertain the possible change in adherence status to recommended medications, diet and physical activity.
Validation and pre-test of questionnaire
The questionnaire was assessed for content validity by an endocrinologist in UCH and three pharmacists in the academia who were knowledgeable about diabetes mellitus. A pre-test was done among twenty-five randomly selected T2D patients in UCH who were subsequently excluded from the main study. Patients for the pre-test were chosen from UCH alone largely in consideration of a relatively high patronage of patients with diabetes when compared to FMC. Specifically, the adapted IPAQ-SF [43] and PDAQ [45] scales were further re-evaluated/validated among the pre-test participants, in order to ensure reproducibility of the item-statements in the scales, as well as its effective use among the Nigerian patients. Feedback from the pre-test led to modifications in the instrument including some questions on physical activity which were rephrased as open-ended questions. In addition, some food items in the PDAQ that are not native food of the studied population were replaced with their indigenous food with similar calorie in accordance with official recommendations [48, 49]. However, these changes did not affect the scoring and the validity of the scales. Internal consistency of the question-items in PDAQ and MAQ was subsequently determined using Cronbach alpha test with values of 0.87 and 0.76, respectively.
Educational intervention provided for participants in the intervention group
The face-to-face patient-specific educational intervention for participants in intervention group was provided by the principal investigator in the endocrinology clinic of each hospital. The intervention largely focused on clarification of medication doses, time of use, side effects as well as measure(s) to overcome some of the identified challenges including missed doses, types and kinds of foods, calorie intake, appropriate time of medication use in relation to meal, salt restriction, spacing of meal time and storage of food especially fruits. Prioritising tolerable physical activity was also emphasized. The educational intervention provided for patients in the intervention group was largely verbal, but was supplemented by a purposely designed educational resource material given to the intervention patients at the baseline recruitment stage, as a form of guidance for dietary recommendations and physical activity. The resource material basically contained the necessary tips on preferable types of food, fruits and vegetables, as well as the most useful forms of physical activity for patients with diabetes, such as brisk walking. The rescheduled appointment(s) of at least once or twice for participants in the intervention group within the 6-month post-baseline follow-up, allowed for reinforcement of the importance of positive adherence behaviours to achieve better therapeutic outcome. It also helped in ascertaining the extent of uptake of counselling tips/advice on the knowledge gaps identified during the baseline interaction. This approach was consistently maintained for patients in the intervention group, while those in the control group continued to receive usual care. Participants’ response to different sections of the questionnaire at baseline and within the 6-month follow-up was captured and documented in the coded questionnaire for individual patient. The intervention was provided by the principal investigator based on previous professional practice experience and clinical knowledge in diabetes management, while other co-investigators monitored the study progress and the intervention process. This was in a bid to ascertain strict compliance with the study protocol, while ensuring immediate and consistent entering of data as collected. Also, the intervention was carried out following the Template for Intervention Description and Replication (TIDER) checklist [50].
Data analysis
Data were entered into SPSS (version 23), with descriptive and inferential statistics employed for analysis. Paired t-test was used to evaluate the extent of change in continuous variables, especially the clinical parameters, IPAQ, PDAQ and cost variables at baseline and 6-month post-baseline. McNemar test was used to assess for significant change in the response to MAQ items at baseline and 6-month post-baseline. Chi-square (χ2) was used to test for association between categorical variables (gender, age, educational qualifications) and baseline glycaemia, as well as adherence status at p < 0.05.
Results
Demographic and clinical characteristics of participants
Table 1 shows the demographic and clinical characteristics of participants. There were more females (160; 79.6%) compared to males (41; 20.4%). Mean age was 62.9 ± 11.6 years, and average monthly income was USD 189.3 ± 253.6 (Table 1). The mean HbA1c for the control group at baseline and at 6-month were 6.1 ± 0.6% and 6.1 ± 0.8%, respectively, while the mean HbA1c for the intervention group were 8.7 ± 1.5% and 7.8 ± 2.0% at baseline and 6-month post-baseline, respectively. Associations between demographic characteristics and baseline HbA1c values for participants in both groups are: gender (χ2 = 11.381; p = 0.001), age (χ2 = 5.72; p = 0.125), and educational qualification (χ2 = 2.781; p = 0.427). Also, relationship between demographic variables and baseline medication adherence of participants included age (χ2 = 3.554; p = 0.169), gender (χ2 = 0.486; p = 0.486) and educational qualification (χ2 = 4.155; p = 0.245).
Participants’ response to MAQ, PDAQ and IPAQ at baseline and 6-month post-baseline
Overall, at baseline, 65 (68.4%) of patients in the control and 45 (42.5%) in the intervention responded ‘No’ to all the 4-items in MAQ scale, indicating optimal (100%) commitment to medication-taking as prescribed. However, at the end of 6-month post-baseline, 75 (78.9%) of the patients in the control and 80 (75.5%) in the intervention had optimal commitment to their medication(s). Detail of participants’ response to MAQ is shown in Table 2. Evaluation of PDAQ scale indicated that, at baseline, 84 (88.4%) in the control and 67 (63.2%) in the intervention had score ≥ 51 (i.e. dietary adherent), while at 6-month post-baseline, 87 (91.6%) in the control and 95 (89.6%) in the intervention were dietary adherent (Table 3). The IPAQ evaluation showed that, a total of 59 (62.1%) and 64 (60.1%) patients in the control and intervention groups, respectively had ≥600MET physical activity per week at baseline (i.e. adherence to recommended minimum physical activity). Whereas, 66 (69.5%) in the control and 76 (71.7%) in the intervention were adherent to recommended physical activity at 6-month post-baseline (Table 3).
Clinical outcomes and adherence parameters evaluated at baseline and 6-month post-baseline
In the intervention group, there was a significant reduction in the HbA1c from 8.7 ± 1.5% at baseline to 7.8 ± 2.0% at 6-month (p < 0.001). The systolic blood pressure reduced from 136.9 ± 20.7 mmHg at baseline to 131.0 ± 19.9 mmHg at 6-month (p = 0.002). In addition, there was a significant improvement in the average weekly physical activity from 775.2 ± 700.5MET at baseline to 829.3 ± 695.5MET at 6-month (p < 0.001) and a significant increase in adherence to dietary recommendations from 51.8 ± 8.8 at baseline to 56.4 ± 4.3 at 6-month (p < 0.001) Table 3.
In the control group, there was no significant change in the HbA1c value at baseline (6.1 ± 0.6%) and at 6-month post-baseline (6.1 ± 0.8%), p = 0.094, but a significant reduction in systolic blood pressure from 129.3 ± 18.2 mmHg (baseline) to 125.3 ± 15.9 mmHg (6-month post-baseline), p = 0.004. Also, there was insignificant increase in adherence to dietary recommendations (56.3 ± 4.0 to 56.5 ± 3.9; p = 0.094), as well as the weekly physical activity (901.4 ± 743.5 to 911.7 ± 752.6MET; p = 0.327), Table 3.
Reason(s) for treatment non-adherence among participants
Fifty-one (53.7%) in the control and 104 (98.1%) in the intervention gave one or combination of reasons for medication non-adherence. Financial constraints [control (25; 49.0%), intervention (48; 46.1%)] and forgetfulness [control (16; 31.3%), intervention (36; 34.6%)] were mostly cited as major reason(s) for medication non-adherence (Table 4). Also, the reason(s) for non-adherence to dietary recommendations in different combination included: knowledge deficit of the importance of recommended diet for diabetes management [control (3; 18.8%), intervention (23; 38.3%)], financial constraints [control (3; 18.8%), intervention (11; 18.3%)], difficulty in accessing recommended diet [control (5; 31.3%), intervention (4; 6.7%)], lack of means of preservation e.g. refrigerator [control (5; 31.3%), intervention (14; 23.3%)], and inability to resist dietary desires [control (0; 0.0%), intervention (8; 13.3%)]. For the physical activity non-adherence, the reason(s) largely cited included: tiredness/discomfort [control (13; 36.1%), intervention (14; 33.3%)], lack of time/busy schedule [control (9; 25.0%), intervention (14; 33.3%)], unwillingness [control (8; 22.2%), intervention (8; 19.0%)] and illness [control (6; 16.7%), intervention (6; 14.3%)].
Financial capacity and medical bill payment mechanism among participants
Of the 106 participants in the intervention group, 42 (39.6%) paid for medical bill by self via out-of-pocket (OOP), 34 (32.1%) had their caregivers responsible for paying OOP and 12 (11.3%) paid through co-OOP of caregivers with patients, while enrollees of National Health Insurance Scheme (NHIS) who usually pay 10% of their medical bill accounted for 11 (10.4%). Seven (6.6%) gave no response. In the control group, 44 (46.3%) paid medical bill by self OOP, 25 (26.3%) had it paid OOP by their caregivers, 14 (14.7%) co-OOP with caregivers, while 12 (12.6%) were NHIS enrollees.
Change in direct costs of management for participants in the control and intervention groups
There was a significant decrease in mean costs per patient for consultation and transportation at 6-month post-baseline for both groups (Table 5). In the intervention group, the mean cost per patient for antidiabetes medications increased from an average of USD 117.3 ± 61.9 pre-baseline to USD 127.3 ± 66.2 at 6-month post-baseline (p = 0.025), while mean cost per patient for laboratory investigations decreased from USD 87.8 ± 28.1 to USD 82.3 ± 16.1 (p = 0.035). Overall, the mean direct costs of management per patient increased from USD 327.3 ± 114.4 (pre-baseline) to USD 333.0 ± 118.4 (6-month post-baseline), p = 0.449, in the intervention group. However, in the control group, the mean direct costs of management per patient decreased from USD 290.1 ± 117.0 (pre-baseline) to 289.1 ± 120.0 at 6-month post-baseline (p = 0.89), Table 5.
Discussion
In this study, we evaluated treatment adherence and patient-specific reason(s) for non-adherence among patients classified as good glycaemia (control group) and poor glycaemia (intervention group). This coupled with educational intervention provided for patients in the intervention group during a 6-month follow-up, while direct costs of management were subsequently estimated for both groups. Our study however showed a significant increase in the number of patients in the intervention group with optimal commitment to medication-taking at the end of 6-month post-baseline, compared to the control cohort. This may perhaps suggest that consistent verification of patients’ understanding and knowledge about a medical condition and its treatment during patient-provider’s encounter could be a key educational strategy to reveal the information gaps of patients [28]. Previous studies have also reported educational intervention to be most effective in resolving knowledge-related medication non-adherence behaviour [28, 51, 52]. In addition, our study reveals improvement in glycaemia in the intervention cohort, which may partly be linked to improved adherence to recommended therapies in the cohort compared to the control group. Though, the average HbA1c value in our study is above the American Diabetes Association (ADA) recommended target of < 7.0% [42], however, significant reduction (0.9%) in the average HbA1c from 8.7 ± 1.5% (baseline) to 7.8 ± 2.0% (6-month post-baseline) in the intervention group is consistent with previous studies in most developed and some developing countries [30, 32, 33]. Kiel et al in an observational prospective study to demonstrate the pharmacist’s impact on clinical outcomes in a diabetes disease management program showed an HbA1c reduction of 1.6% [53]. In addition, Chen et al reported a decrease of 0.83% in mean HbA1c in the intervention group during a randomised controlled trial on pharmaceutical care of elderly patients with poorly controlled T2D [38]. Also, Odegard et al in a randomised pharmacist’s intervention among poorly controlled diabetes mellitus reported a significant reduction in HbA1c from 10.2 to 8.7% after 6 months and 8.2% after 12 months [54]. It is also noteworthy to mention that, there is a corresponding increase in the proportion of patients in intervention group with good glycaemia at the end of 6-month post-baseline (66.7%) compared to 47.3% at baseline. Previous studies have indicated a strong correlation between increased therapy adherence and better glycaemic control among patients with T2D, with a possible reduction in the risk of diabetes complications, morbidity and mortality [28, 55, 56]. Also, the United Kingdom Prospective Diabetes Study Group has proved that for every 1% reduction in HbA1c, there is a 21% drop in the risk for any diabetes-related adverse events or complications, and a 21% reduction in deaths related to diabetes [57, 58]. The positive clinical outcome in the intervention group may therefore be indirectly linked to a consequent reduction in the risk of microvascular adverse events among the intervention patients. Thus, there may be the need for pharmacists, especially in LMICs to take cognizance of this study findings, by actively involved in holistic patient-centred adherence counseling for patients with diabetes in particular and chronic diseases in general, in a bid to ensure improved glycaemic outcome. This may become necessary if taking into consideration the inadequacies of the current process of adherence enhancement by physician alone [59, 60], where the information provided by physician about medication(s) might be insufficient for the patient, partly due to physician’s time constraints and high number of patients to attend to during clinic visits [60,61,62]. Pharmacists having direct contact with patients during filling and refilling of prescriptions have a better ability to detect potential or actual adherence problems, and having confirmed the existence of a non-adherence problem, intervene to resolve the actual problem(s) while preventing the development of potential ones [63].
Asides the reduction in glycaemic outcome among participants in the intervention group, we observed a significant increase of 8.5% in the mean cost per patient for antidiabetes medication(s) from USD 117.3 ± 61.9 to USD 127.3 ± 66.2, and a 6.1% increase in mean costs per patient for total medications. While the direct costs of management per patient changed from USD 327.3 ± 114.4 to 333.0 ± 118.4, indicating a 1.7% increase. However, in the control group, the mean cost per patient for antidiabetes medications decreased by 1.7%, while the total direct costs of management per patient decreased by 0.3%. Overall, the average direct costs of management for the intervention patients was USD 37.2 (11.4%) higher than that for patients in the control group. This seems consistent with Chen et al which reported the mean cost per patient of USD 44.10 in the intervention and USD 4.35 in the control group, representing an increase of USD 39.73 in cost per patient [38]. Sokol et al [64] and Roebuck et al [65] have reported that greater adherence to medication(s) for chronic condition is associated with higher medication costs but lower non-medical costs. It has also been shown that costs of care was significantly associated with glycaemic control [66, 67]. Mata-Cases et al [37] in their study reported that patients with diabetes who had poor glycaemic control (HbA1c > 7%) had increased costs of €448.0 per patient per year compared to those with good control (HbA1c ≤7%). The two main variables reported to cause the increase in costs in their study were medications and hospitalisation [37]. In our study, the increase in costs per patient for total medications in the intervention group may be partly attributed to poor clinical outcomes, which may necessitate aggressive management with therapy intensification for the cohort. Treatment intensification may include add-on medication(s) and sometimes brand substitution which may be relatively expensive than the generic equivalent, thereby contributing to higher costs of management [68,69,70]. Notwithstanding, healthcare providers including pharmacists may need to take up active role in educating patients on diabetes-specific treatment goals, as well as involving them in the treatment plans/decision geared towards achieving and maintaining target glycaemic outcome. This patient-centred approach to care may invariably lead to better outcome, with a possible reduction in the development of diabetes complications and by extension the costs of management.
The most common reasons for medication non-adherence among patients in both groups were forgetfulness and financial constraints. Forgetfulness has been identified as a major reason for non-adherence in previous studies [17, 28, 71]. Lack of financial coping mechanism has also been found to be an adherence barrier among patients with chronic illness [72, 73]. Patients who paid for their medication(s) out-of-pocket are more likely to adopt different costs-containment coping strategies such as erratic or irregular filling of prescriptions or taking less frequent doses to make the medication(s) last longer [73,74,75]. In addition, the topmost reason for dietary non-adherence among the cohorts was lack of knowledge on the importance of recommended diets for diabetes management. This is despite the fact that dietary management is an integral aspect of T2D management to achieve optimal glycaemic control [76]. Thus, in our study, identification of barriers to dietary adherence and the subsequent resolution of patient-specific dietary knowledge gaps in the intervention cohort, mostly helped in enhancing dietary self-care behaviour necessary to ensure optimal glycaemic outcome. Reduction in HbA1c value has been reported to be associated with ingestion of lower carbohydrate and low saturated fat diet in patients with diabetes [76,77,78,79]. Consumption of low glycaemic index carbohydrate and low cholesterol-containing diets are core dietary information consistently emphasized for the intervention patients. In addition, there is an increased number of patients in the intervention group with good response on adherence to physical activity at the end of 6-month post-baseline. This may perhaps be linked to increased awareness of positive impact of exercise on glycaemic control, as well as other health-related benefits of prescribed form of exercise. Educational intervention has been reported to improve patients’ participation in physical activity by changing their physical activity behaviour [80, 81]. However, tiredness and busy schedule were the most reported barriers to engagement in regular physical activity among the intervention patents, while unwillingness was most cited in the control group. Pati et al has reported unwillingness as one of the major barriers to increased participation in physical activity practice [82].
Despite the fact that our study findings serve as a useful evidence-based information to further reiterate the necessity for pharmacists’ active contribution in collaborative care of patients with diabetes generally. This study however, has the following limitations. The self-report nature of the tools used for data collection may be associated with some inherent bias such as recall bias, when patients may over- or under-report some of the information provided. Also, we employed quasi-experimental approach in which participants were solely assigned into control and intervention groups based on their respective glycated haemoglobin value. Thus, the possibility of the difference in baseline characteristics of participants affecting the eventual outcomes may not be totally ruled out. As a result, selection and channeling bias [83, 84] might be a concern in our study, since participants were not subjected to standard randomisation techniques that will assure equal chance of being allocated to either of the studied groups. Nevertheless, evaluation of association between the participants’ demographic characteristics and baseline HbA1c value, as well as medication adherence status indicated no statistically significant difference. Moreover, the scope and design of our study to categorize patients into ‘good’ and ‘poor’ glycaemia necessitate the use of quasi-experimental concept. Another limitation of our study may be linked to the recruitment of participants, as well as provision of intervention in the endocrinology clinic of the hospitals, which may perhaps have impacted on the emotion or psyche of some studied participants. Thus, the possibility of response bias may not be completely excluded. Nevertheless, the proactive and patient-centred measures adopted in our study including the courteous patient approach and consistent use of non-judgmental interacting skills during encounters might have assisted in boosting the morale of participants to provide an honest opinion/response. Also, the likelihood of selective outcome reporting and analysis bias may still be a concern, especially when the investigator serves as both the data collector and evaluator. This concern was partly allayed considering the adopted approach where the co-investigators are continuously monitoring the study progress and the intervention process to ensure strict compliance with the study protocol, while ensuring immediate and consistent entering of data as collected at each study site, with no propensity for conflicting data. In addition, the principal investigator, at intervals, always present the update on the data collected, where challenges encountered are highlighted and possible resolution proffered. Furthermore, in our study, the retrospective estimation of 6-month pre-baseline direct costs of management using the prevailing costs at the time of the study may not give a concise reflection of the pre-baseline cost value, on account of the time lag. Nevertheless, all the aforementioned limitations may need to be carefully considered, when interpreting the findings of our study, while caution should be exercised in making a widespread generalisation.
Conclusion
Pharmacist-led intervention enhanced adherence to recommended medications, diet and physical activity among the poorly-controlled type-2-diabetes, with a corresponding significant improvement in glycaemic outcome and an insignificant increase in associated direct costs of management. This further underscores a need for proactive engagement of pharmacists in collaborative management of patients with type 2 diabetes, especially in respect to treatment adherence enhancement to achieve positive clinical outcomes.
Availability of data and materials
The data sets used and/or analysed during the current study are available from the corresponding author on request.
Abbreviations
- T2D:
-
Type 2 diabetes mellitus
- HbA1c:
-
Glycated haemoglobin
- MAQ:
-
Medication Adherence Questions
- PDAQ:
-
Perceived Dietary Adherence Questionnaire
- IPAQ:
-
International Physical Activity Questionnaire
- MET:
-
Metabolic Equivalent Task
- UCH:
-
University College Hospital
- FMC:
-
Federal Medical Centre
- USD:
-
United States of America Dollar
- UKPDS:
-
United Kingdom Prospective Diabetes Study
- NHIS:
-
National Health Insurance Scheme
- NURTW:
-
National Union of Road Transport Workers
- ADA:
-
American Diabetes Association
- CONSORT:
-
Consolidated Standards of Reporting Trials
- IRB:
-
Institution Review Board
- WHO:
-
World Health Organisation
- NREC:
-
National Research and Ethic Committee
- LMICs:
-
Low and Middle Income Countries
References
Arumugam G, Manjula P, Paari N. A review: anti diabetic medicinal plants used for diabetes mellitus. J Acute Dis. 2013;2(3):196–200. https://doi.org/10.1016/S2221-6189(13)60126-2.
World Health Organisation (WHO) 2020. https://www.who.int/news-room/fact-sheets/detail/diabetes. Accessed 26 June 2020.
Zimmet P. The burden of type 2 diabetes: are we doing enough? Diabet Metab. 2003;29(4):659–81. https://doi.org/10.1016/S1262-3636(03)72783-9.
Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes. Estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27(5):1047–53. https://doi.org/10.2337/diacare.27.5.1047.
Chinenye S, Uloko AE, Ogbera AO, Ofoegbu EN, Fasanmade AO, Fasanmade AA, et al. Profile of Nigerians with diabetes mellitus- Diabcare Nigeria study group (2008): results of multicentre study. Indian J Endocrinol Metab. 2012;16(4):558–64. https://doi.org/10.4103/2230-8210.98011.
World Health Organization (WHO). Diabetes Action Now Booklet: an initiative of the World Health Organization and International Diabetes Federation. WHO Publication 2004:4. Geneva, Switzerland. http://www.who.int/diabetes/booklet. Access 20 March 2020.
Unachukwu CN, Uchenna DI, Young EE. Mortality among diabetes in patients in Port Harcourt Nigeria. Afr J Endocrinol Metabol. 2008;7(1):1–4.
Aguocha BU, Ukpabi JO, Onyeonoro UU, Njoku P, Ukegbu AU. Pattern of diabetic mortality in a tertiary health facility in south eastern Nigeria. Afr J Diabetes Med. 2013;21:1–3.
Godman B, Basu D, Pillay Y, Mwita JC, Rwegerera GM, Anand Paramadhas BD, et al. Review of ongoing activities and challenges to improve the care of patients with type 2 diabetes across Africa and the implications for the future. Front Pharmacol. 2020;11:108. https://doi.org/10.3389/fphar.2020.00108.
Fasamade OA, Dagogo-Jack S. Diabetes Care in Nigeria. Ann Global Health. 2016;81(6):81(6). https://doi.org/10.1016/j.aogh.2015.12.012.
Luga AO, McGuire MJ. Adherence and health care costs. Risk Manag Healthc Policy. 2014;7:35–44.
Cutler RL, Fernandez-Llimos F, Frommer M, Benrimoj C, Garcia-Cardenas V. Economic impact of medication non-adherence by disease groups: a systematic review. BMJ Open. 2018;8(1):e016982. https://doi.org/10.1136/bmjopen-2017-016982.
Napolitano F, Napolitano P, Angelillo IF. Collaborative working group. Medication adherence among patients with chronic conditions in Italy. Eur J Pub Health. 2016;26(1):48–52. https://doi.org/10.1093/eurpub/ckv147.
Hamine S, Gerth-Guyette E, Faulx D, Green BB, Ginsburg AS. Impact of mHealth chronic disease management on treatment adherence and patient outcomes: a systematic review. J Med Internet Res. 2015;17(2):e52. https://doi.org/10.2196/jmir.3951.
Adisa R, Fakeye TO, Fasanmade A. Medication adherence among ambulatory patients with type 2 diabetes in a tertiary healthcare setting in southwestern Nigeria. Pharm Pract. 2011;9(2):72–81. https://doi.org/10.4321/S1886-36552011000200003.
Demoz GT, Wahdey S, Bahrey D, Kahsay H, Woldu G, Niriayo YL, et al. Predictors of poor adherence to antidiabetic therapy in patients with type 2 diabetes: a cross-sectional study insight from Ethiopia. Diabetol Metab Syndr. 2020;12(1):62. https://doi.org/10.1186/s13098-020-00567-7.
Gelaw BK, Mohammed A, Tegegne GT, Defersha AD, Fromsa M, Tadesse E, et al. Non-adherence and contributing factors among ambulatory patients with anti diabetic medications in Adama referral hospital. Adv Pharmacoepidemiol Drug Saf. 2014;3(04):169. https://doi.org/10.4172/2167-1052.1000169.
Jackevicius CA, Li P, Tu J. Prevalence, predictors and outcomes of primary non-adherence after acute myocardial infarction. Circulation. 2008;117(8):1028–36. https://doi.org/10.1161/CIRCULATIONAHA.107.706820.
Ho MP, Bryson CL, Rumsfeld JS. Medication adherence: its importance in cardiovascular outcomes. Circulation. 2009;119(23):3028–5. https://doi.org/10.1161/CIRCULATIONAHA.108.768986.
Ho PM, Tsai TT, Maddox TM, Power JD, Carroll NM, Jackevicius C, et al. Delays in filling clopidogrel prescription after hospital discharge and adverse outcomes after drug-eluting stent implantation. Implications for transitions of care. Circulation. 2010;3(3):261–6. https://doi.org/10.1161/CIRCOUTCOMES.109.902031.
Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353(5):487–97. https://doi.org/10.1056/NEJMra050100.
Pladevall M, Williams LK, Potts LA, Divine G, Xi H, Elston LJ. Clinical outcomes and adherence to medications measured by claims data in patients with diabetes. Diabetes Care. 2004;27(12):2800–5. https://doi.org/10.2337/diacare.27.12.2800.
Walker E, Molitch M, Kramer M, Kahn S, Ma Y, Edelstein S, et al. Adherence to preventive medications: predictors and outcomes in the diabetes prevention program. Diabetes Care. 2006;29(9):1997–2002. https://doi.org/10.2337/dc06-0454.
Banerji MA, Dunn JD. Impact of glycemic control on healthcare resource utilization and costs of type 2 diabetes: current and future pharmacologic approaches to improving outcomes. Am Health Drug Benefits. 2013;6(7):382–92.
Kamuhabwa A, Charles E. Predictors of poor glycemic control in type 2 diabetic patients attending public hospitals in Dar Es Salaam. Drug Healthc Patient Saf. 2014;6:155–65. https://doi.org/10.2147/DHPS.S68786.
Nasseh K, Frazee SG, Visaria J, Vlahiotis A, Tian Y. Cost of medication nonadherence associated with diabetes, hypertension, and dyslipidemia. Am J Pharm Benefits. 2012;4(2):e41–7.
Martin LR, Williams SL, Haskard KB, Dimatteo MR. The challenge of patient adherence. Ther Clin Risk Manag. 2005;1(3):189–99.
Adisa R, Fakeye TO. Treatment non-adherence among patients with poorly controlled type 2 diabetes in ambulatory care settings in southwestern Nigeria. Afr Health Sci. 2014;14(1):1–10. https://doi.org/10.4314/ahs.v14i1.2.
Odegard PS, Capoccia K. Medication taking and diabetes: a systematic review of the literature. Diabet Educator. 2007;33(6):1014–29. https://doi.org/10.1177/0145721707308407.
Lim PC, Lim K, Embee ZC, Hassali MA, Thiagarajan A, Khan TM. Study investigating the impact of pharmacist involvement on the outcomes of diabetes medication therapy adherence program Malaysia. Pak J Pharm Sci. 2016;29(2):595–601.
Leguelinel-Blache G, Dubois F, Bouvet S, Roux-Marson C, Arnaud F, Castelli C, et al. Improving Patientʼs primary medication adherence: the value of pharmaceutical counseling. Medicine (Baltimore). 2015;94(41):e1805. https://doi.org/10.1097/MD.0000000000001805.
Jeong S, Lee M, Ji E. Effect of pharmaceutical care interventions on glycemic control in patients with diabetes: a systematic review and meta-analysis. Ther Clin Risk Manag. 2018;14:1813–29. https://doi.org/10.2147/TCRM.S169748.
Pousinho S, Morgado M, Plácido AI, Roque F, Falcão A, Alves G. Clinical pharmacists´ interventions in the management of type 2 diabetes mellitus: a systematic review. Pharm Pract. 2020;18(3):2000. https://doi.org/10.18549/PharmPract.2020.3.2000.
Dalton K, Byrne S. Role of the pharmacist in reducing healthcare costs: current insights. Integr Pharm Res Pract. 2017;25(6):37–46. https://doi.org/10.2147/IPRP.S108047.
Coto JA, Yehle KS, Foli KJ. The relationship between uncontrolled Glycemia and the cost of hospitalization. Clin Nurse Spec. 2014;8(5):283–7. https://doi.org/10.1097/NUR.0000000000000071.
Shetty S, Secnik K, Oglesby AK. Relationship of glycemic control to total diabetes-related costs for managed care health plan members with type 2 diabetes. J Manag Care Pharm. 2005;11(7):559–64. https://doi.org/10.18553/jmcp.2005.11.7.559.
Mata-Cases M, Casajuana M, Franch-Nadal J, Casellas A, Castell C, Vinagre I, et al. Direct medical costs attributable to type 2 diabetes mellitus: a population-based study in Catalonia. Spain Eur J Health Econ. 2016;17(8):1001–10. https://doi.org/10.1007/s10198-015-0742-5.
Chen JH, Ou HT, Lin TC, Lai EC, Kao YH. Pharmaceutical care of elderly patients with poorly controlled type 2 diabetes mellitus: a randomized controlled trial. Int J Clin Pharm. 2016;38(1):88–95. https://doi.org/10.1007/s11096-015-0210-4.
Adisa R, Fakeye TO. Effects of number and type of antidiabetes medications on adherence and glycaemia of ambulatory type 2 diabetes patients in southwestern Nigeria. Pharm Pract. 2013;11(3):156–65. https://doi.org/10.4321/S1886-36552013000300006.
Ayele AA, Emiru YK, Tiruneh SA, Ayele BA, Gebremariam AD, Tegegn HG. Level of adherence to dietary recommendations and barriers among type 2 diabetic patients: a cross-sectional study in an Ethiopian hospital. Clin Diabetes Endocrinol. 2018;4(1):21. https://doi.org/10.1186/s40842-018-0070-7.
Mohammed AS, Adem F, Tadiwos Y, Woldekidan NA, Degu A. Level of adherence to the dietary recommendation and glycemic control among patients with type 2 diabetes mellitus in eastern Ethiopia: a cross-sectional study. Diabetes Metab Syndr Obes. 2020;13:2605–12. https://doi.org/10.2147/DMSO.S256738.
American Diabetes Association (2018). Glycemic Targets: Standards of medical Care in Diabetes 2018. Diabetes Care 2018; 41(Suppl 1):S55-S64.
International Physical Activity Questionnaire - Short Form - PLoS https://doi.org/10.2165/11531930-000000000-. 00000. Page 2. Short Last 7 Days Self-Administered version of the IPAQ. Revised August 2002 https://journals.plos.org/plosone/article/file?type=supplementary&id=info:doi/. Accessed 23 June 2019.
International Physical Activity Questionnaire - Short Form http://www.ipaq.ki.se Accessed 21 May 2019.
Asaad G, Sadegian M, Lau R, Xu Y, Soria-Contreras DC, Bell RC, et al. The reliability and validity of the perceived dietary adherence questionnaire for people with type 2 diabetes. Nutrients. 2015;7(7):5484–96. https://doi.org/10.3390/nu7075231.
Gonzalez JS, Schneider HE, Wexler DJ, Psaros C, Delahanty LM, Cagliero E, et al. Validity of medication adherence self-reports in adults with type 2 diabetes. Diabetes Care. 2013;36(4):831–7. https://doi.org/10.2337/dc12-0410.
Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24(1):67–74. https://doi.org/10.1097/00005650-198601000-00007.
Evert AB, Boucher JL, Cypress M, Dunbar SA, Franz MJ, Mayer-Davis EJ, et al. Nutrition therapy recommendations for the Management of Adults with diabetes. Diabetes Care. 2013;36(11):3821–42. https://doi.org/10.2337/dc13-2042.
Atkinson FS, Foster-Powell K, Brand-Miller JC. International tables of glycemic index and glycemic load values: 2008. Diabetes Care. 2008;31(12):2281–3. https://doi.org/10.2337/dc08-1239.
Hoffmann TC., Glasziou PP, Milne R, Perera R, Moher D, Altman DG, Barbour V, Macdonald H, Johnston M, Lamb SE, Dixon-Woods M, McCulloch P, Wyatt JC, Chan AW, Michie S. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ. 2014; 7:348:g1687. doi: https://doi.org/10.1136/bmj.g1687.
Muñoz EB, Dorado MF, Guerrero JE, Martínez FM. The effect of an educational intervention to improve patient antibiotic adherence during dispensing in a community pharmacy. Aten Primaria. 2014;46(7):367–75. https://doi.org/10.1016/j.aprim.2013.12.003.
Muira KW, Venturaa A, Stinnetta SS, Enfiedjian A, Allinghama RR, Lee PP. The influence of health literacy level on an educational intervention to improve glaucoma medication adherence. Patient Educ Couns. 2012;87(2):160–4. https://doi.org/10.1016/j.pec.2011.09.009.
Kiel PJ, McCord AD. Pharmacist impact on clinical outcomes in a diabetes disease management program via collaborative practice. Ann Pharmacother. 2005;39(11):1828–32. https://doi.org/10.1345/aph.1G356.
Odegard PS, Goo A, Hummel J, Williams KL, Gray SL. Caring for poorly controlled diabetes mellitus: a randomized pharmacist intervention. Ann Pharmacother. 2005;39(3):433–40. https://doi.org/10.1345/aph.1E438.
Chung WW, Chua SS, Lai PSM, Chan SP. Effects of a pharmaceutical care model on medication adherence and glycemic control of people with type 2 diabetes. Patient Prefer Adherence. 2014;8:1185–94. https://doi.org/10.2147/PPA.S66619.
Presley B, Groot W, Pavlova M. Pharmacy-led interventions to improve medication adherence among adults with diabetes: a systematic review and meta-analysis. Res Social Adm Pharm. 2019;15(9):1057–67. https://doi.org/10.1016/j.sapharm.2018.09.021.
United Kingdom Prospective Diabetes Study Group (UKPDS). Association of glycemia with macro-vascular and microvascular complications of type 2 diabetes (UKPDS 35). Prospective observational study. BMJ 2000; 321(7258):405–412.
United Kingdom Prospective Diabetes Study Group (UKPDS). Intensive blood glucose control with sulfonylurea or insulin compared with conventional treatment and risk of complication in patients with type 2 diabetes. UKPDS 33. Lancet. 1998;352(9131):837–8. https://doi.org/10.1016/S0140-6736(98)07019-6.
Barry CA, Stevenson FA, Britten N, Barber N, Bradley CP. 2001. Giving voice to the lifeworld. More humane, more effective medical care? A qualitative study of doctor-patient communication in general practice. Soc Sci and Med. 2001;53(4):487–505. https://doi.org/10.1016/S0277-9536(00)00351-8.
Barber N. Ensuring patient’s satisfaction with information about their medicines. Qual Health Care. 2001;10(3):130–1. https://doi.org/10.1136/qhc.0100130.
Collier IA, Baker DM. Implementation of a pharmacist-supervised outpatient diabetes treatment clinic. Am J Health Syst Pharm. 2014;71(1):27–36. https://doi.org/10.2146/ajhp130200.
Newby KL, Dobesh PP, Ashen D. Eds. 2011. Key strategies to maximize adherence to secondary prevention therapies for coronary artery disease. Mediscape education @ 2011 Mediscape, LLC. Http://www.CME@medscape.net. Access 20 June 2020.
Hepler CD, Strand LM. Opportunities and responsibilities in pharmaceutical care. Am J Hosp Pharm. 1990;47(3):533–43.
Sokol MC, McGuigan KA, Verbrugge RR, Epstein RS. Impact of medication adherence on hospitalization risk and healthcare cost. Med Care. 2005;43(6):521–30. https://doi.org/10.1097/01.mlr.0000163641.86870.af.
Roebuck CM, Liberman JN, Gemmill-Toyama M, Brennan TA. Medication Adherence Leads to Lower Health Care Use and Costs Despite Increased Drug Spending. Health Aff. (Millwood). 2011;30(1):91–9.
Afroz AA, Chowdhury HA, Shahjahan M, Hafez MD, Hassan N, Ali L. Association of good glycemic control and cost of diabetes care: experience from a tertiary care hospital in Bangladesh. Diabetes Res Clin Pract. 2016;120:142–8. https://doi.org/10.1016/j.diabres.2016.07.030.
Mata-Cases M, Rodríguez-Sánchez B, Mauricio D, Real J, Vlacho B, Franch-Nadal J, et al. The association between poor glycemic control and health care costs in people with diabetes: a population-based study. Diabetes Care. 2020;43(4):751–8. https://doi.org/10.2337/dc19-0573.
Meddings J, Kerr EA, Heisler M, Hofer TP. Physician assessments of medication adherence and decisions to intensify medications for patients with uncontrolled blood pressure: still no better than a coin toss. BMC Health Serv Res. 2012;12(1):270. https://doi.org/10.1186/1472-6963-12-270.
Knapp M, King D, Pugner K, Lapuerta P. Non-adherence to antipsychotic medication regimens: associations with resource use and costs. Br J Psychiatry. 2004;184(6):509–16. https://doi.org/10.1192/bjp.184.6.509.
Gray A, Raikou M, McGuire A, Fenn P, Stevens R, Cull C, Stratton I, Adler A, Holman R Turner R, On behalf of the United Kingdom Prospective Diabetes Study Group. Cost effectiveness of an intensive blood glucose control policy in patients with type 2 diabetes: economic analysis alongside randomised controlled trial (UKPDS 41). United Kingdom Prospective Diabetes Study Group. BMJ (Clinical Research ed.). 2000; 320(7246):1373–1378.
Meinema JG, van Dijk N, Beune EJ, Jaarsma DA, van Weert HC, Haafkens JA. Determinants of adherence to treatment in hypertensive patients of African descent and the role of culturally appropriate education. PLoS One. 2015;10(8):e0133560. https://doi.org/10.1371/journal.pone.0133560.
Jiang C, Ma J, Zhang X, Luo W. Measuring financial protection for health in families with chronic conditions in rural China. BMC Public Health. 2012;12(1):988. https://doi.org/10.1186/1471-2458-12-988.
Murphy A, McGowan C, McKee M, Suhrcke M, Hanson K. Coping with healthcare costs for chronic illness in low-income and middle-income countries: a systematic literature review. BMJ Glob Health. 2019;4(4):e001475. https://doi.org/10.1136/bmjgh-2019-001475.
Gupta S, McColl MA, Guilcher SJ, Smith K. Cost-related nonadherence to prescription medications in Canada: a scoping review. Patient Prefer Adherence. 2018;12:1699–715. https://doi.org/10.2147/PPA.S170417.
Khera R, Valero-Elizondo J, Das SR, Virani SS, Kash BA, de Lemos JA, et al. Cost-related medication nonadherence in adults with atherosclerotic cardiovascular disease in the United States, 2013 to 2017. Circulation. 2019;140(25):2067–75. https://doi.org/10.1161/CIRCULATIONAHA.119.041974.
Haimoto H, Sasakabe T, Wakai K, Umegaki H. Effects of a low-carbohydrate diet on glycemic control in outpatients with severe type 2 diabetes. Nutr Metab (Lond) 2009; 6:21. https://doi.org/10.1186/1743-7075-6-21.
Sami W, Ansari T, Butt NS, Ab Hamid MR. Type 2 diabetes mellitus: link between diet, HbA1c and complications. AMJ. 2016;9(9):346–56. https://doi.org/10.4066/AMJ.2016.2708.
Wallin A, Giuseppe D, Orsini N, Patel PS, Forouhi NG, Wolk A. Fish consumption, dietary long-chain n-3 fatty acids, and risk of type 2 diabetes systematic review and meta-analysis of prospective studies. Diabetes Care. 2012;35(4):918–29. https://doi.org/10.2337/dc11-1631.
Shadman Z, Khoshniat M, Poorsoltan N, Akhoundan M, Omidvar M, Larijani B, et al. Association of high carbohydrate versus high fat diet with glycated hemoglobin in high calorie consuming type 2 diabetics. J Diabetes Metab Disord. 2013;12(1):27. https://doi.org/10.1186/2251-6581-12-27.
Sigal RJ, Armstrong MJ, Bacon SL, Boulé NG, Dasgupta K, Kenny GP, et al. Physical activity and diabetes. Canadian J Diabetes. 2018;42(1):S54–63. https://doi.org/10.1016/j.jcjd.2017.10.008.
Çolak TK, Acar G, Dereli EE, Özgül B, Demirbüken İ, Alkaç Ç, et al. Association between the physical activity level and the quality of life of patients with type 2 diabetes mellitus. J Phys Thera Sci. 2016;28(1):142–7. https://doi.org/10.1589/jpts.28.142.
Pati S, Lobo E, Pati S, Desaraju S, Mahapatra P. Type 2 diabetes and physical activity: barriers and enablers to diabetes control in eastern India. Prim Health Care Res Dev. 2019;20(e44):1–6. https://doi.org/10.1017/S1463423619000689.
Schweizer ML, Braun BI, Milstone AM. Research methods in healthcare epidemiology and antimicrobial stewardship – quasi-experimental designs. Infect Control Hosp Epidemiol. 2016;37(10):1135–40. https://doi.org/10.1017/ice.2016.117.
Handley MA, Lyles CR, McCulloch C, Cattamanchi A. Selecting and improving quasi-experimental designs in effectiveness and implementation research. Ann Rev Public Health. 2018;39(1):5–25. https://doi.org/10.1146/annurev-publhealth-040617-014128.
Acknowledgements
The authors acknowledge the staff of record department and the medical out-patients clinic of University College Hospital, Ibadan and Federal Medical Centre Abeokuta for their support during data collection. We also appreciate the participants for their time.
Funding
No fund was received from any organisation or institution for the purpose of this research.
Author information
Authors and Affiliations
Contributions
AEI designed the study, collected the data, conduct the statistical analysis and developed the manuscript. WOE was involved in the designing of the study, monitored the study progress and intervention process and draft of the manuscript. RA was involved in the designing of the study, monitored the study progress and intervention process, conduct the statistical analysis, developed the manuscript as well as correction of the manuscript.
All the authors read and approved the final submission.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval for the study was obtained from the University of Ibadan/University College Hospital Ethics Review Committee with approval number NHREC/05/01/2008a and Federal Medical Centre, Abeokuta (NREC/06/21/2010–2015) Ethics Review Committee. Verbal and written informed consent in accordance with the approved study protocol by the Ethics committee, was obtained from each participant after explaining the objectives and procedure of the study to the participants individually. The information in the informed consent form was explicitly read and explained to individual participant on every clinic day before the commencement of the interview. Only the consented participants within the study period were enrolled.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ipingbemi, A.E., Erhun, W.O. & Adisa, R. Pharmacist-led intervention in treatment non-adherence and associated direct costs of management among ambulatory patients with type 2 diabetes in southwestern Nigeria. BMC Health Serv Res 21, 1000 (2021). https://doi.org/10.1186/s12913-021-06979-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-021-06979-z