Abstract
Background
Health economic research is still facing significant problems regarding the standardization and international comparability of health care services. As a result, comparative effectiveness studies and cost-effectiveness analyses are often not comparable. This study is part of the PECUNIA project, which aimed to improve the comparability of economic evaluations by developing instruments for the internationally standardized measurement and valuation of health care services for mental disorders. The aim of this study was to identify internationally relevant services in the health and social care sectors relevant for health economic studies for mental disorders.
Methods
A systematic literature review on cost-of-illness studies and economic evaluations was conducted to identify relevant services, complemented by an additional grey literature search and a search of resource use measurement (RUM) questionnaires. A preliminary long-list of identified services was explored and reduced to a short-list by multiple consolidation rounds within the international research team and an external international expert survey in six European countries.
Results
After duplicate removal, the systematic search yielded 15,218 hits. From these 295 potential services could be identified. The grey literature search led to 368 and the RUM search to 36 additional potential services. The consolidation process resulted in a preliminary list of 186 health and social care services which underwent an external expert survey. A final consolidation step led to a basic list of 56 services grouped into residential care, daycare, outpatient care, information for care, accessibility to care, and self-help and voluntary care.
Conclusions
The initial literature searches led to an extensive number of potential service items for health and social care. Many of these items turned out to be procedures, interventions or providing professionals rather than services and were removed from further analysis. The resulting list was used as a basis for typological coding, the development of RUM questionnaires and corresponding unit costs for international mental health economic studies in the PECUNIA project.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
Health economic evaluations are an integral part of health technology assessments and can inform policymakers and facilitate decision-making processes about the costs and the effectiveness of different health interventions. Cost-effectiveness analyses (CEAs) take changes in costs and the effectiveness of two or more alternative interventions into account, and are consequently of particular importance for decision-making within and across countries. Therefore, the need for standardization of economic evaluations to enable proper decision-making and transferability of results has long been recognized in the health economics community [1]. However, the reporting standards do still differ substantially. Health economic research is still facing significant problems regarding the standardization and international comparability of the definitions of services [2, 3], the measurement of service utilization [4], and the monetary valuation of services [5,6,7]. There is a demand for comparable health service data to improve evidence-based decision-making in health policy. The health agencies of the European Union (EU) need commensurable descriptions of care to evaluate health equity and ensure mobility of health service users in the EU [2]. Currently, the comparison of services and their contents is difficult, even if they have identical names, due to terminological variability [8]. The definition of a service is not always clear and can differ substantially. Even the term ‘service’ itself can refer to a range of elements such as the provider, a combination of functions, programs, resources, the facility of service provision or an organizational unit [2]. A service may be organized differently on an international, federal, regional, or even communal level, and it can also be challenging to define the target population of a service. There is a recognized shortcoming of international agreement on classification systems. In particular, there are no uniform coding matrices for different settings, which may lead to biased results in health services research [9, 10].
Another problem for the comparability of health economic studies is the lack of standardized resource use measurement (RUM) instruments, which may lead to unnecessary fluctuations of economic evaluation data [4, 11]. This impedes the comparability, transferability, and applicability of these studies within and across countries [12, 13]. RUMs are considered an important method for measuring the resources used by health service users within economic evaluations. Nevertheless, existing RUMs are often country-specific [14] or population-specific [15]. Hence, there is a need for harmonized RUMs to improve the overall methodology of both cost-effectiveness and comparative effectiveness studies [11, 13] in terms of international comparability. According to Mayer et al. [16], the first step in a RUM development process is the identification of economically relevant items by means of a literature review.
Likewise, there is also a substantial degree of variation in the applied valuation methods in European health economic studies [17]. For example, the micro-costing method and the gross costing method not only differ in their complexity but also their resulting estimates [5]. This lack of standardization potentially complicates the comparability and transferability of economic evaluations. The general methodological credibility of monetary valuations is hence questionable, and economic evaluations may be less useful for decision-making [18]. The underlying reason is that the applied valuation method has a significant impact on the results [19].
The EU project “ProgrammE in Costing, resource use measurement and outcome valuation for Use in multi-sectoral National and International health economic evaluAtions” (PECUNIA) aims to overcome the problems described above by developing standardized multi-sectoral, multi-national and multi-person resource use measurement instruments, standardized unit costs, and outcome assessment tools to improve the methodology of economic evaluations in the European Union [13, 20,21,22,23,24]. The PECUNIA Consortium coordinated by the Medical University of Vienna consists of ten institutions situated in six European countries: Austria (AT), Germany (DE), Hungary (HU), the Netherlands (NL), Spain (ES), and the United Kingdom (UK) [25]. Three mental disorders: depression, schizophrenia and post-traumatic stress disorder (PTSD) were chosen as exemplary diseases due to their high disease burden and economic relevance. The project is exploring multiple economic sectors and domains, namely “health and social care” sectors, “education and (criminal) justice” sectors, “employment and productivity” domains, and “patient, family and informal care” domains.
The aim of this study was to identify services in the health and social care sectors that are relevant for the calculation of costs in economic evaluations from a societal perspective. According to the “whole systems approach”, the inclusion of the social care sector is pivotal in providing comprehensive mental health care. In particular, community-based social care interventions might be neglected in some healthcare systems, while they can have a significant impact on the course of a mental disorders [26]. Hence, social care services were also explicitly considered in this study to achieve a cross-sectoral broad perspective.
Methods
This study included two major steps: step I) a systematic and grey literature review for data identification, data extraction and the production of a preliminary listing of terms following initial consolidation steps (“preliminary service list”); step II) final consolidation step following external expert surveys in all six PECUNIA countries for the production of a “basic service list” used in all further steps in the PECUNIA project. These steps involved two working groups (A and B) as well as internal and external expert panels. The initial identification and consolidation steps included working group A from UKE (PH, AK, CD, HHK) and working group B from MUW (JS, CF, SM) supported by the relevant country-lead PECUNIA partners for country-specific tasks (internal expert panel: AT/MUW, DE/UKE, HU/CUB, NL/UM & EUR, ES/Psicost, UK/LSE & UnivBris). The external expert panel composed of 29 health and social service researchers, health economists, and planners from public agencies and other stakeholders in every participating country (AT: 7, DE: 3, HU: 4, NL: 5, ES: 6, UK: 4).
Step I was led by working group A and involved working group B as well as the internal expert panel. Step II was led by working group B and involved working group A, the internal expert panel and the external expert panel. The whole process and the activities performed by the working groups and the expert panels are shown in Fig. 1.
Step I – Identification and extraction
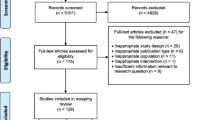
Firstly, working group A carried out a systematic review of the peer-reviewed literature to identify relevant services in mental health and social care. A systematic search strategy was applied including the use of indexed vocabulary (e.g. MeSH terms) and other keywords, combined with different Boolean operators and limits (details are shown Appendix 1). The structure of this systematic review was based on the PRISMA checklist. Information was gathered by screening of the databases PUBMED-Medline, PsycINFO, NHS EED, EconLit and Embase. One combined search was conducted for the health care and social care sectors. To identify relevant studies, we used a two-step approach. In the first step, titles and where necessary abstracts were screened to exclude studies that were distinct irrelevant. In the second step, all studies identified as possibly relevant in step one were obtained and screened for eligibility in full text.
Eligibility criteria were defined prior to the literature search. To identify relevant service items from a costing perspective, the systematic literature review included cost-of-illness studies and economic evaluations focusing on mental disorders. Publications in Dutch, English, German, Hungarian, and Spanish as per the involved countries from the previous ten years (search conducted in May 2018) were considered. Exclusion criteria included editorials, letters, case reports and reviews or cost-of-illness studies and cost-effectiveness analyses not focusing on mental disorders. Additionally, studies based on results already published elsewhere and abstracts without full-text availability were excluded. Working group A screened the methods and results sections of included studies to identify relevant service items, which were extracted into a MsExcel® file together with information on item definition (if available) and country of origin. In line with the more specific research focus of the PECUNIA project, the systematic literature search focused on services relevant for mental disorders. Although the PECUNIA project focusses on depression, schizophrenia and PTSD as exemplary diseases, we made no restrictions to specific diseases in this study for two reasons. On the one hand, we wanted to assure that we get a full picture of services relevant to mental disorders (i.e. although we choose three exemplary diseases to work with in the PECUNIA project, we developed further tools like a resource use questionnaire for mental disorders in general). On the other hand, it seemed impracticable to assign services to specific disorders, hence a full search for services was seen as the appropriate strategy.
Secondly, a manual search for additional key papers and national grey literature was performed by the internal expert panel in AT, DE, HU, NL, ES, and the UK. This focused on selected mental disorders including documents on care for depression, schizophrenia and PTSD, covering clinical guidelines, PhD-theses and publications by the government or major organizations in each of the six participating countries. No limit regarding the timeframe was set for the grey literature search, but only the most recent versions of e.g. clinical guidelines were included. To ensure a standardized approach, researchers were provided with identical search instructions and an extraction template for service items. The template asked researchers to name identified services used by persons with mental disorders together with a short description in English and national language and to provide information regarding disease, treatment setting as well as type of data source and references.
Thirdly, as part of the grey literature search, working group A screened the content of RUM questionnaires from the DIRUM repository, RUM questionnaires identified in studies included in step I, and at a later stage the so-called “Core items for a standardized resource-use measure (ISRUM)” list from the UK [27]. Since the PECUNIA project aimed to develop a generic RUM questionnaire for use in economic evaluations, RUM screening was not limited to services specific for mental disorders only.
All identified items were added to a preliminary service list in an MsExcel® file which then underwent multiple consolidation steps. Working group A supported by working group B eliminated obvious duplicates and provided brief “working-definitions” for each remaining item. If not self-explanatory (e.g. “General Practitioner-contact”), these descriptions were either taken from the respective sources (systematic or grey literature search), or were newly developed based on an item-specific internet research. Descriptions were further face-validated by members of the internal expert panel before exploited in the external expert survey.
Step II – External expert survey and final revision
Working group B led the distribution of the consolidated preliminary service list as an MsExcel® based survey to the external expert panel in each of the six participating countries organized by the PECUNIA country leads. The survey was carried out between November 2018 and January 2019 and included questions on the clarity of definitions, the relevance and the economic impact of the identified items, and a request for any additional relevant missed services for the respective national health and social care sectors. Further details on the survey and resulting country reports can be found elsewhere [28].
The results of the expert survey were synthetized and consolidated jointly by working groups A and B with input from authors MGC and LSC for preparing a “basic service list” for all further work steps in the PECUNIA project. At this stage, eligible items from the ISRUM list [27] were added to the preliminary service list. Services were defined as follows [2, 10]:
“A ‘service’ is a micro-level functional system of care organization, defined as the smallest unit with own administrative structure available within the catchment area (micro-organization).”
Consequently, working groups A and B excluded all items that did not match this definition, in particular interventions (e.g. “cognitive behavioral therapy”), tests (e.g. “neuropsychological examination”) and professions (e.g. “GP assistant”). This step was necessary to reduce double counting and as a preparatory step for the DESDE coding (for details please see [29]) adapted to PECUNIA to define service-typologies for the development of internationally comparable units of analysis, harmonized resource use measurement, and corresponding reference unit costs for international (mental) health economic studies. Several of the resulting services were also merged into one single service due to similarity in terms of care activities and costs. For example, contacts with outpatient physicians and contacts with outpatient nurses were combined to one service “outpatient healthcare service” which was defined as a contact with an outpatient health care provider. On the other hand, some services were also split up, in particular if they were provided in more than one main branch of the DESDE coding-system. For example, “rehabilitation” may be provided as a residential or as an outpatient service resulting in two distinct services with distinctively different unit costs.
Results
Step I – Identification and extraction
The systematic literature review yielded 16,066 hits, of which 859 were removed as duplicates (Fig. 2). After adding 11 studies from other sources, titles and abstracts of 15,218 records were screened for relevancy according to the eligibility criteria and 966 publications were assessed in full-text. Of these, 587 publications were excluded for reasons (for references see Appendix 3), such as reporting no original cost data, or being a non-eligible study type. Hence, 379 studies (for references see Appendix 2) were included in the qualitative synthesis of relevant potential service items. In addition to the systematic literature search, the national grey literature searches yielded an additional 81 relevant publications and the search for RUM questionnaires yielded 11 instruments that were screened for further service items (for details see Appendix 4).
The total number of potential health and social care service items identified by the systematic literature search, the grey literature search and the RUM search is shown in Fig. 3. In this step, 699 items were identified. Whilst 95 of items identified in the systematic literature search, were published in international journals with English language, a considerable amount of 200 items were identified in publications from national sources. These items were translated into English language by the national partners together with the country-specific items identified in the grey literature search. Items were checked for duplicates, which were then excluded. The remaining 186 items constituted the preliminary service list used for the expert survey. The participating countries had the option to adjust the list to national specifics. For example, in Austria outpatient specialist services can be delivered in-hospital or out-of-hospital settings with distinctively different costs, hence both settings were asked as separate questions, which increased the number of items for the external expert survey in Austria.
Step II – External expert survey and final revision
Due to the very high number of services (n = 186) stemming from different areas of care (health or social care) and including rare or highly specialized services, responses were heterogeneous between experts. Often experts answered that they did not know how relevant items were regarding the intensity of their utilization. No additional items were added to the preliminary service list, nor were items deleted based on the expert survey.
Final revision of the preliminary service list based on the expert survey results by working groups A and B with input from authors MGC and LSC resulted in the “basic service list” consisting of 56 identified health and social care services (Table 1).
During the revision process, we excluded 383 out of 439 items from the combined preliminary service list and the ISRUM list items. Most items were excluded because they were procedures rather than services (n = 209). Procedures were excluded to avoid double counting with services including these procedures. For example, diagnostic tests (e.g. “TSH-test”, “neuropsychological examination”, etc.) were excluded as procedures that are performed in the context of an “outpatient healthcare contact”, which is the service of interest included into the basic service list. Further 75 items were excluded because of similarity. This means that different items were combined to one service in the basic service list. For example, the service “outpatient health care contact” comprised all different types of outpatient physician specializations (e.g. GP, psychotherapist, neurologist, etc.). Finally, another 99 items were excluded for “other reasons”. These were predominantly items from the ISRUM list, that did not represent items related to health or social care at all. For example, questions regarding income losses or travel costs or items belonging to other service areas like the (criminal) justice sector or the educational sector.
We grouped identified services according to the main branches of the DESDE system: “residential care” (n = 17), “outpatient care” (n = 27), “day care” (n = 5), “information for care” (n = 2), “accessibility to care” (n = 3), and “self-help and voluntary care” (n = 2).
Overall, outpatient care was the largest group containing about half of all identified services (n = 27). Only 10 out of the 27 services were explicitly for persons with mental disorders. Most outpatient care services could roughly be assigned to either outpatient medical care, outpatient social care or outpatient vocational assistance. Among those services assigned to outpatient medical care, four services were for persons with mental disorders (“psychiatric drop-in center”, “psychiatric rehabilitation aftercare service”, “mental counselling center/advice center”, “psychological crisis resolution team”). A further four services for persons with mental disorders could be assigned to outpatient social care (“psychosocial crisis center”, “social care facility for mentally ill persons”, “social assistance for mentally ill persons”, “legal carer/guardian for mentally ill persons”) and two services could be assigned to outpatient vocational assistance (“protected / sheltered workshop for mentally ill persons” and “pre-vocational assessment service for mentally ill persons”).
Out of the 18 services located in residential care, eight services were referring to living facilities, of which three were explicitly for persons with mental disorders (“psychiatric residential home”, “assisted tenant group for mentally ill persons” and “sheltered housing for mentally ill persons”). The remaining 10 services in residential care were treatment-related in either hospitals or rehabilitation units, of which six were explicitly for persons with mental disorders (“acute psychiatric ward”, “psychiatric intensive care unit (PICU)”, “psychiatric long-term ward”, “Soteria house”, “non-addiction related psychiatric rehabilitation”, “addiction-related rehabilitation”).
Discussion
The objective of this study was to identify services relevant for persons with mental disorders in the health and social care sectors for economic analyses purposes. A provisional service list was compiled through systematic literature review and a grey literature search. Further data from existing RUM instruments were added. The preliminary service list resulting from these searches and several consolidation steps included 186 items, of which 56 were included in the final basic service list used for the development of the PECUNIA costing tools such as the PECUNIA Coding System [29], the PECUNIA RUM (Janssen LMMP, Evers I, Drost SMAA, Thorn RMWA, Hollingworth J, Noble W, et al: Involving respondents in the development process of the PECUNIA RUM instrument: Results of Think Aloud interviews, submitted) [30], the PECUNIA Reference Unit Costing (RUC) Templates [31] and the PECUNIA RUC Compendium [32, 33] https://www.pecunia-project.eu/tools).
The difference between the preliminary service list and the final basic service list resulted primarily from two reasons. First, we did not apply a specific definition of “service” when compiling the first preliminary service list. Instead, we collected all resource items related to health and social services use, in order to be as comprehensive as possible. As a result, the preliminary service list was a mix of not only services but also interventions, procedures or professions that had to be excluded subsequently. Second, for the further typology of services, the PECUNIA Consortium agreed to define a service according to the international DESDE classification system as adapted for the PECUNIA project. This allowed achieving a higher consolidation level where different items could be combined into one internationally harmonized service item for costing purposes. For example, the service “outpatient healthcare service” includes all types of outpatient physicians and non-physician healthcare providers.
This study allowed the realization of the magnitude of the problem when “words” are used to describe services for health economic research, because often “names” of services were prone to Babylonian confusion not allowing the comparison like with like. Whilst, for example, it was very clear for the national project partners and contact points what a simple service use like “mental hospital stay” meant in their respective country and/or region, a detailed analysis in terms of cost measurement for economic evaluations revealed that mental hospital stays may mean very different things in different countries. Affected dimensions were for example eligible target populations (regarding age group and gender, diagnosis, disease severity or functional impairment), treatments offered, average duration, setting (with and/or without overnight stay), and degree of specialization (mental ward versus closed mental ward). This problem has several implications. First, it points to a general limitation of comparisons of cost-of-illness studies and cost-effectiveness analyses when identically named services, do in fact not represent identical but rather similar compositions of utilized resources. Second, the description of services or utilized units in cost-of-illness studies and cost-effectiveness analysis can be questioned. Overall, studies rarely presented detailed descriptions of the units measured to calculate costs. We assume that this information is often regarded as unnecessary for evaluation purposes because the definition of services seems to be clear in the national context. While this might to be acceptable from a national perspective, it becomes a substantial problem, if one tries to compare the units of analysis internationally. However, if one tries to describe a service, the inherent question arises of how best to do this. Using words can introduce new problems by creating circular references. For these reasons, it was decided in the PECUNIA Consortium to use the DESDE coding system for the description of services.
As expected, most of the identified services were located in residential and outpatient facilities. Hence, currently these types of services seem to play a pivotal role in mental healthcare provision in Europe. Conversely, services in the remaining segments of care (day care, accessibility to care, information to care, self-help and voluntary care) are very much underrepresented. This might change to some extent due to care transitions induced by the COVID-19 pandemic like increased use of video-consultations that outlast the end of the pandemic. Nevertheless, we identified a large number of services beyond “medical care” for example services providing protected living, assistance in different areas of daily living or the workplace.
Implications for future research
Our major learning concerns problems related to the use of language to describe health care services. Language turned out to be too vague and ambiguous to describe services in the international contexts. For this purpose, services were described using a taxonomical coding system in a next step. The question remains, how this problem should be addressed in further cost-of-illness studies and cost-effectiveness analyses. As already discussed, these studies rarely provided definitions of the items measured for cost calculation. Based on our findings this presents an underestimated source for inter-study heterogeneity. PECUNIA provides tools that can help to reduce this problem, but a certain amount of fuzziness will remain in international service comparisons, resulting from the between-country differences in the services themselves.
Future health services research should incorporate the analysis of vagueness and ambiguity of the terms, the production of international glossaries of terms after disambiguation of the identified terms, and dictionaries to translate the international terms into local terminology to improve semantic interoperability. In particular, cost-effectiveness and comparative effectiveness research should compare the same units of analysis and use a common vocabulary. This might increase the validity of multinational studies significantly, but healthcare provision can often also differ within a country on a regional or local level. Currently, the majority of studies compare solely the name of a service, but not the exact elements of the service such as the target group, type of care, activities, and type(s) and the number of professionals involved. The application of such a classification system is, therefore, particularly useful when developing new measurement instruments.
This study was used as a basis for the development of the PECUNIA RUM instrument. RUMs are important tools for measuring resource use in economic evaluations and their development process should follow a stepwise approach. A literature review should be conducted to identify economically and clinically relevant services for the specified disease area or target population. In addition, an expert survey may be conducted to evaluate the importance of the identified services and rank them accordingly. Existing RUMs can also be identified and analyzed regarding their content, structure and layout [12]. The results of this study reveal relevant services provided to health service users with mental disorders in the health and social care sector internationally, at least within the European context. This research was the first step in the process of the PECUNIA RUM development, i.e. the identification of economically relevant services for mental healthcare provision with a focus on Europe. The multinational PECUNIA RUM instrument is also harmonized with comparable reference unit costs (RUCs) in different countries, as it offers a catalogue of defined services that can be monetarily valued.
Strengths and limitations
We followed a highly standardized and structured study approach and incorporated expertise from multiple international health economic and health services working groups. Nevertheless, there are several limitations to this study. First, the systematic and the grey literature searches led to a varying amount of publications per country. Hence, some countries may be overrepresented, while others may be underrepresented. On the other hand, since we checked all services in national expert surveys, the basic service list should be comprehensive for the participating countries and for generic services but may miss some specific services in health and social care of non-participating countries.
Second, the inclusion of grey literature may have negatively influenced the systematic approach of this review due to the lacking preset search strategy. Hence, the reproducibility of the results is limited [34]. In this study, there was even further variability in the search approach, because different research strategies may have been used in the national-level grey literature searches despite the centrally provided search instructions and extraction templates for service items. On the other hand, the inclusion of grey literature can also be seen as an advantage, because it can complement the data of a systematic review and ultimately increase the level of evidence. Additionally, the incorporation of grey literature may counteract potential publications bias [34].
Third, since the more specific research questions and the resources of the PECUNIA project were focused on mental disorders, we were not able to search specifically for non-mental health services with the same intensity as for services for mental health. We restricted the identification of non-mental health services to a screening of existing RUM questionnaires and included all the most common RUMs so it should be highly unlikely that we missed essential generic health and social care services.
Fourth, we did not double-screen for identification of studies and service items in the systematic literature review by two independent reviewers. This incorporates risk of falsely included or excluded studies, but the risk of bias resulting from this limitation should be negligible for several reasons: 1) we included a very high number of 379 studies limiting the risk of bias from missing out further relevant studies; 2) several researchers from different countries were involved in all steps related to the processing of identified variables, thus limiting the risk of bias resulting from false inclusion of studies or service items; 3) since we did not calculate metrics using study results, we were not prone to risk of bias related to issues of statistical calculations.
Conclusion
We found an extensive variety of services provided to persons with mental disorders in Europe. It became apparent that the distinction between a service and a procedure is not always clear-cut. Hence, these discrepancies in the conceptualization of a service potentially impede their comparability in economic evaluations. In this study, economically relevant services for mental health and social care were identified and organized according to the different “main types of care” of the DESDE classification system. As a result, a basic list of services for mental healthcare provision in Europe emerged. The resulting service list provided the basis for a typology coding system of services for internationally comparable units of analysis, the development of a harmonized RUM instruments, and corresponding reference unit costs for international mental health economic studies within the PECUNIA project [30,31,32,33] (https://www.pecunia-project.eu/tools).
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AT:
-
Austria
- DE:
-
Germany
- DESDE:
-
Description and evaluation of services and directories in Europe
- ES:
-
Spain
- HU:
-
Hungary
- ISRUM:
-
Core items for a standardized resource-use measure
- NL:
-
Netherlands
- RUM:
-
Resource use measurement (instrument)
- UK:
-
United Kingdom
References
Drummond M, Brandt A, Luce B, Rovira J. Standardizing methodologies for economic evaluation in health care. Practice, problems, and potential. Int J Technol Assess Health Care. 1993;9(1):26–36.
Salvador-Carulla L, Alvarez-Galvez J, Romero C, Gutierrez-Colosia MR, Weber G, McDaid D, et al. Evaluation of an integrated system for classification, assessment and comparison of services for long-term care in Europe: the eDESDE-LTC study. BMC Health Serv Res. 2013;13:218.
Montagni I, Salvador-Carulla L, McDaid D, Strassmayr C, Endel F, Naatanen P, et al. The REFINEMENT glossary of terms: an international terminology for mental health systems assessment. Adm Policy Ment Health. 2018;45(2):342–51.
Thorn JC, Coast J, Cohen D, Hollingworth W, Knapp M, Noble SM, et al. Resource-use measurement based on patient recall: issues and challenges for economic evaluation. Appl Health Econ Health Policy. 2013;11(3):155–61.
Barnett PG. An improved set of standards for finding cost for cost-effectiveness analysis. Med Care. 2009;47(7 Suppl 1):S82–8.
Jacobs JC, Barnett PG. Emergent challenges in determining costs for economic evaluations. Pharmacoeconomics. 2017;35(2):129–39.
Simon J. Health economic analysis of service provision. (Chapter 23/136). In: Geddes JR, Andreasen NC, Goodwin GM, editors. New Oxford textbook of psychiatry. 3rd ed. Oxford: Oxford University Press; 2020. p. 9780198713005.
Castelpietra G, Simon J, Gutierrez-Colosia MR, Rosenberg S, Salvador-Carulla L. Disambiguation of psychotherapy: a search for meaning. Br J Psychiatry. 2021;219(4):532–7.
Gutierrez-Colosia MR, Salvador-Carulla L, Salinas-Perez JA, Garcia-Alonso CR, Cid J, Salazzari D, et al. Standard comparison of local mental health care systems in eight European countries. Epidemiol Psychiatr Sci. 2019;28(2):210–23.
Salvador-Carulla L, Poole M, Gonzalez-Caballero JL, Romero C, Salinas JA, Lagares-Franco CM, et al. Development and usefulness of an instrument for the standard description and comparison of services for disabilities (DESDE). Acta Psychiatr Scand Suppl. 2006;432:19–28.
Noben CY, de Rijk A, Nijhuis F, Kottner J, Evers S. The exchangeability of self-reports and administrative health care resource use measurements: assessement of the methodological reporting quality. J Clin Epidemiol. 2016;74(93–106):e2.
Ridyard CH, Hughes DA, Team D. Development of a database of instruments for resource-use measurement: purpose, feasibility, and design. Value Health. 2012;15(5):650–5.
The PECUNIA Group. Vision & Mission. Available from: https://www.pecunia-project.eu/project/vision-and-mission.
Grupp H, Konig HH, Riedel-Heller S, Konnopka A. FIMPsy - Questionnaire for the assessment of medical and non medical resource utilisation in mental disorders: development and application. Psychiatr Prax. 2018;45(2):87–94.
Seidl H, Bowles D, Bock JO, Brettschneider C, Greiner W, Konig HH, et al. FIMA–questionnaire for health-related resource use in an elderly population: development and pilot study. Gesundheitswesen. 2015;77(1):46–52.
Mayer S, Paulus ATG, Laszewska A, Simon J, Drost R, Ruwaard D, et al. Health-related resource-use measurement instruments for intersectoral costs and benefits in the education and criminal justice sectors. Pharmacoeconomics. 2017;35(9):895–908.
van Lier LI, Bosmans JE, van Hout HPJ, Mokkink LB, van den Hout WB, de Wit GA, et al. Consensus-based cross-European recommendations for the identification, measurement and valuation of costs in health economic evaluations: a European Delphi study. Eur J Health Econ. 2018;19(7):993–1008.
Mayer S, Kiss N, Laszewska A, Simon J. Costing evidence for health care decision-making in Austria: a systematic review. PLoS One. 2017;12(8):e0183116.
Mayer S, Fischer C, Zechmeister-Koss I, Ostermann H, Simon J. Are unit costs the same? A case study comparing different valuation methods for unit cost calculation of general practitioner consultations. Value Health. 2020;23(9):1142–8.
Simon J. Multi-sectoral costs and benefits in health economic evaluations across Europe: The PECUNIA project. J Ment Health Policy Econ. 2019;22:1–40.
The PECUNIA Group. PECUNIA - ProgrammE in Costing, resource use measurement and outcome valuation for Use in multi-sectoral National and International health economic evaluAtions. Available from: http://www.pecunia-project.eu/.
Simon J. on behalf of the PECUNIA Consortium. Assessing the costs and outcomes of healthcare. EU Research (Spring 2021). 2021.
Simon JK, A Brodszky, V. Evers, S. Roijen, L. Serrano-Pérez, P. Salvador-Carulla, L. Park, A.L. Hollingworth, W. (Pharmaco)economic evaluations for mental health related services: the PECUNIA project. Eur J Public Health. 2020(30). https://doi.org/10.1093/eurpub/ckaa166.574.
Laszewska A, Helter TM, Nagel A, Peric N, Simon J. Patient-reported outcome measures suitable for quality of life/well-being assessment in multisectoral, multinational and multiperson mental health economic evaluations. Evid Based Ment Health. 2022;25(2):85–92.
The PECUNIA Group. Available from: https://www.pecunia-project.eu/about/consortium.
Rosen A, Gill NS, Salvador-Carulla L. The future of community psychiatry and community mental health services. Curr Opin Psychiatry. 2020;33(4):375–90.
Thorn JC, Brookes ST, Ridyard C, Riley R, Hughes DA, Wordsworth S, et al. Core items for a standardized resource use measure: expert delphi consensus survey. Value Health. 2018;21(6):640–9.
Fischer C, Mayer S, Peric N, Simon J, Group P. Establishing a comprehensive list of mental health-related services and resource use items in Austria: a national-level, cross-sectoral country report for the PECUNIA project. PLoS One. 2022;17(1):e0262091.
Gutierrez-Colosia MRH, P. Simon, J. Konnopka, A. Fischer, C. Mayer, S. Brodszky, V. Hakkaart-van Roijen, L. Evers, S. Park, A. König, H.-H. Hollingworth, W. Salinas-Pérez J. A. the PECUNIA Group and Salvador-Carulla L. Magnitude of terminological bias in international health services research: a disambiguation analysis in mental health. Epidemiol Psychiatr Sci. 2022;31:e59, 1–7. https://doi.org/10.1017/S2045796022000403.
PECUNIA Group. PECUNIA Resource Use Measurement Instrument (PECUNIA RUM) (Version 1.0/2021). https://doi.org/10.5281/zenodo.5036942. https://www.pecunia-projecteu/tools/rum-instrument. 2021.
PECUNIA Group. PECUNIA Reference Unit Cost Templates (PECUNIA RUC Templates) (Version 1.0/2021). https://doi.org/10.5281/zenodo.5037573. https://www.pecunia-projecteu/tools/ruc-templates. 2021.
PECUNIA Group. PECUNIA Reference Unit Cost Compendium (PECUNIA RUC Compendium) (Version 1.0/2021). https://doi.org/10.5281/zenodo.5040068. https://www.pecunia-projecteu/tools/ruc-compendium. 2021.
Mayer S, Berger M, Konnopka A, Brodszky V, Evers S, Hakkaart-van Roijen L, et al. In search for comparability: the PECUNIA reference unit costs for health and social care services in Europe. Int J Environ Res Public Health. 2022;19(6):3500.
Mahood Q, Van Eerd D, Irvin E. Searching for grey literature for systematic reviews: challenges and benefits. Res Synth Methods. 2014;5(3):221–34.
Funding
Open Access funding enabled and organized by Projekt DEAL. This project has received funding from the European Union’s Horizon 2020 research and innovation programme under grant agreement No 779292. The funding body had no influence on the design of the study and collection, analysis, and interpretation of data or the writing the manuscript.
Author information
Authors and Affiliations
Consortia
Contributions
PH has contributed to the analysis and interpretation of data and wrote the first draft of the manuscript. MGC has contributed to the study design, the grey literature searches, the analysis and interpretation of data and substantially revised the manuscript. CD contributed to the systematic literature searches and prepared data analysis. HHK contributed to the study design and revised the manuscript. JS contributed to the study design, the analysis and interpretation of data and substantially revised the manuscript. CF contributed to the grey literature searches and revised the manuscript. SM contributed to the grey literature searches and revised the manuscript. LSC contributed to the study design, the analysis and interpretation of data and substantially revised the manuscript. VB contributed to the grey literature searches and revised the manuscript. LHR contributed to the grey literature searches, the analysis and interpretation of data and revised the manuscript. SE contributed to the grey literature searches, the analysis and interpretation of data and revised the manuscript. ALP contributed to the grey literature searches and revised the manuscript. WH contributed to the grey literature searches and revised the manuscript. AK contributed to the study design, the analysis and interpretation of data and finalized the manuscript.
All authors read and approved the final manuscript.
PECUNIA Group
This manuscript was written on behalf of the PECUNIA Group. Members of the PECUNIA Group are (in alphabetical order for each country-partner):
Medical University of Vienna d: PI: Judit Simon; team members (in alphabetical order): Michael Berger, Claudia Fischer, Agata Łaszewska, Susanne Mayer, Nataša Peri´c; University Medical Center Hamburg-Eppendorf a: PI: Hans-Helmut König; team members (in alphabetical order): Christian Brettschneider, Marie Christine Duval, Paul Hinck, Johanna Katharina Hohls, Alexander Konnopka, Louisa-Kristin Muntendorf; Corvinus University of Budapest h: PI: Valentin Brodszky; team members: László Gulácsi; Maastricht University k: PI: Silvia M.A.A. Evers; team members (in alphabetical order): Ruben M.W.A. Drost, Luca M.M. Janssen, Aggie T.G. Paulus, Irina Pokhilenko; Erasmus University Rotterdam I, j: PI: Leona Hakkaart-van Roijen; team members (in alphabetical order): Kimberley Hubens, Ayesha Sajjad; Servicio de Evaluación del Canario de la Salud p: PI:Pedro Serrano-Aguilar; PSICOST Scientific Association c: PI: Luis Salvador-Carulla; team members (in alphabetical order): Nerea Almeda, Pilar Campoy-Muñoz, Carlos R. García-Alonso, Mencía R. Gutiérrez-Colosía, Cristina Romero-López-Alberca; team members (in alphabetical order): Lidia García-Pérez, Renata Linertová, Lilisbeth Perestelo-Pérez, Cristina Valcárcel-Nazco; London School of Economics and Political Science m: PI: A-La Park; University of Bristol n: PI: William Hollingworth; team members (in alphabetical order): Sian Noble, Joanna Thorn.
a Department of Health Economics and Health Services Research, University Medical Center Hamburg-Eppendorf (UKE), Hamburg, Germany.
c Scientific Association PSICOST, Seville, Spain.
d Department of Health Economics, Center for Public Health, Medical University of Vienna (MUW), Vienna, Austria.
h Department of Health Economics, Corvinus University of Budapest (CUB), Budapest, Hungary.
i Institute for Medical Technology Assessment, Erasmus University Rotterdam (EUR), Burgemeester Oudlaan 50, PO Box 1738, 3000 Rotterdam, DR, Netherlands.
j Health Technology Assessment, Erasmus School of Health Policy and Management, Erasmus University Rotterdam (EUR), Burgemeester Oudlaan 50, PO Box 1738, 3000 Rotterdam, DR, Netherlands.
k Department of Health Services Research, Care and Public Health Research Institute (CAPHRI), Faculty of Health, Medicine and Life Sciences (FHML), Maastricht University (UM), Maastricht, the Netherlands.
m Care Policy and Evaluation Centre (CPEC), Department of Health Policy, London School of Economics and Political Science (LSE), London, UK.
n Health Economics Bristol, Department of Population Health Sciences, Bristol Medical School (UnivBris), Bristol, UK.
p Servicio de Evaluación del Canario de la Salud (SESCS), El Chorrillo, Tenerife (Spain).
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Appendix 1. Systematic search concept. Appendix 2. Included publications from systematic literature review. Appendix 3. Excluded publications from systematic literature review. Appendix 4. Identified and screened resource use questionnaires.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Hinck, P., Gutierrez-Colosía, M., Duval, C. et al. The identification of economically relevant health and social care services for mental disorders in the PECUNIA project. BMC Health Serv Res 23, 1045 (2023). https://doi.org/10.1186/s12913-023-09944-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-023-09944-0