Abstract
Objective
The added value of systematic client feedback (SCF) to psychotherapy can be affected by patient perspectives, both in a positive and negative way, and is influenced by cultural factors as well. Current study explores patients’ perspectives on use and optimization of SCF in Dutch outpatient mental healthcare. Primary aim of present study is to generate implications for daily practice and optimize SCF implementation, particularly for the Netherlands.
Method
Four patients suffering from mild to moderate psychological disorders were in-depth interviewed on their perspective on the use of SCF, when the Partners for Change Outcome Management System (PCOMS, high frequent), the Outcome Questionnaire (OQ-45, low frequent) and the Mental Health Continuum Short Form (MHC-SF, low frequent) was added to treatment as usual in two Dutch outpatient mental healthcare centers offering brief psychological treatment. Interview topics were (a) SCF in general; (b) type of questionnaires; (c) frequency of use; (d) effect of SCF on therapy; and (e) perceived added value of SCF. A SCF expert team analyzed the data through reflexive Thematic Analysis.
Results
We identified three themes, all of which have two sub-themes: (a) Requirements to use SCF, with sub-themes (a1) Balance between effort to complete SCF and perceived validity, and (a2) Balance between used frequency and perceived validity; (b) Modifiers for test-taking attitude, with subthemes (b1) SCF as an embedded part of therapy, and (b2) Quality of Therapist-Client alignment; and (c) Effects on therapeutic process, with subthemes (c1) Focus on task and goals, and shared responsibility, and (c2) Effects on outcome and satisfaction.
Conclusions
Adding SCF to therapy can be perceived as helpful by patients in psychotherapy if two conditions are met: (1) Creating a right balance between effort and yield for SCF to be used at all; and (2) embedding SCF as an integral part of therapy, through therapist-client alignment. Throughout the progression of therapy, it might be useful to perceive SCF and therapy as communicating vessels; according to patients it is not only necessary to adjust therapy based on SCF, but also to adjust SCF based on the course of therapy.
Trial Registration
This trial was registered on September 30, 2015 in the Dutch Trial Register NTR5466. The Medical Ethics Committee of the University of Twente (Enschede) approved this study (registration number: K15-11, METC Twente).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Systematic Client Feedback (SCF), the regular monitoring of patients’ progress to optimize the course of psychotherapy, is nowadays an established method in mental healthcare [1]. In SCF, patients complete standardized questionnaires at regular intervals, and results are discussed during the session to assess whether the course of treatment requires adjustment. Possible underlying mechanisms of action of SCF are that it enhances patient-therapist communication and alliance, and focusses attention of the therapist, especially when the patient is not on track [2]. SCF is also known as Progress Feedback or Measurement Based Care, and several meta-analyses [1, 3] have demonstrated its potential to improve therapy outcome in terms of symptom reduction, wellbeing, or lowered drop-out rates. Despite this growing evidence for its added value, implementation of SCF is found to be challenging [4,5,6,7] with patient, therapist and organizational factors influencing its use and effect [8, 9].
In addition, SCF implementation is known to be influenced by cultural factors [10,11,12]. Strong heritage cultural identity was for instance found to be related to perceptions of potential harm of SCF use [10], and She et al. found differences in SCF use between Eastern and Western countries [11]. Douglas and colleagues [12] stated that within Western countries there are indications that optimal approaches when starting SCF implementation may vary from top-down, bottom-up, or a combination of bottom-up and top-down. Although the studies on cultural differences in SCF implementation are scarce, there are clear indications that a successful implementation strategy in one country is not automatically transferable to another country. Our study was designed to specifically examine patient factors on SCF within the Netherlands.
The specific influence of patient factors on the use and effect of SCF has been examined in several studies. Happel et al. [13] found that patients of mental health care services mainly want to use SCF as a means to have a joint conversation about recovery. This was also reported by Guthrie et al. [14], who underlined the importance of patients being included in the interpretation and use of SCF. In addition, Unsworth et al. [15] found that adding SCF to therapy can improve the client-therapist relationship.
This added value of SCF for patients was found by Hoy [16] as well, who concluded that the use of SCF not only facilitated the conversation between patient and therapist, but also increased patients’ self-awareness. Wolpert [17] on the other hand warned of the potential iatrogenic damage of poorly implemented SCF. Wolpert and colleagues [18] additionally found that patients feared that SCF would put too much emphasis on technique at the expense of building a working relationship.
Solstad et al. [19] conducted a systematic review of patients’ experiences in the use of SCF. They found four meta-themes in which SCF was perceived as either helpful or hindering: (1) SCF can induce suspicion towards the therapists; (2) Used questionnaires are often too limited or symptom-oriented, not sufficiently corresponding with what patients regard as valuable outcomes; (3) SCF can lead to increased patient empowerment, and (4) SCF can increase collaboration between patient and therapist.
These four themes described by Solstad et al. [19] seem highly relevant, and are also found in later research. The enhanced empowerment in the form of heightened self-awareness and improved collaboration was for instance found by Hovland et al. [20]. In addition, Moltu et al. [21] found that the increased collaboration between patient and therapist was perceived as important not only for patients but also for therapists. This effect of increased collaboration has also been found in group therapy [22] where it strengthened the working alliance.
In summary, previous studies in patients’ perspectives in the use of SCF on the one hand found that adding SCF to treatment as usual can improve collaboration and patient empowerment, but on the other hand can induce suspicion towards therapists or hinder therapy when the used questionnaire is not perceived as a valuable outcome parameter. Although previous studies have painted a clear picture of important themes that play a role in patients’ use of SCF, they have provided little concrete insight into the practical implications that would improve the use of SCF for patients. In addition, SCF implementation is affected by cultural factors and varies per setting and country. Consequently, actionable insights will vary per setting and country as well.
Current study aimed to generate actionable outcomes that can be used as tools to optimize the added value of SCF for patients in Dutch outpatient mental healthcare. We have therefore chosen to have the patient perspective on adding high and low frequent SCF to their therapy analyzed by a team of SCF experts familiar with its use in the Netherlands. By thus organizing the analysis into shared meaningful themes, we expected to be able to formulate clear implications for daily practice. We used reflexive Thematic Analysis (rTA) as described by Braun and Clarke [23,24,25] and further elaborated by Byrne [26] as qualitative method, as it is specifically intended for such profound subjective analysis and designed to generate actionable outcomes for a specific target group.
Instead of aiming for high generalizability, we strived for actionable insights for daily practice of SCF use in the Netherlands. Our main goal was to investigate the conditions that patients consider helpful or necessary to successfully use SCF in Dutch mental healthcare. By distilling important central themes in using SCF from a patient’s point of view, we thus aimed to generate implications for daily practice and optimize its implementation. Our secondary goal was to investigate to what extent themes found in interviews with Dutch patients correspond to the four general meta-themes found by Solstad et al. [19].
Method
Recruitment
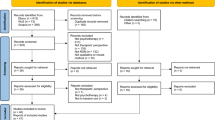
Patients were recruited from two centers of Mindfit, an outpatient mental health organization in the Netherlands with over 30 centers across the country. These centers are offering brief psychological treatment added with high and low frequent SCF. Their therapeutic approach is based on (positive) cognitive behavioral therapy [27] and solution focused therapy [28].
Recruitment was carried out with the help of therapists who regularly added SCF to treatment as usual. First posters with information about the interviews were hung in the participating centers. If patients were interested in participating in the interviews, they could express this to their own therapist and were then asked if they agreed to be contacted by the lead researcher for an individual interview.
We aimed for a small number of in-depth interviews instead of a large number of short interviews, because we intended to generate actionable insights for SCF implementation for clinical practice in Dutch mental healthcare. In the first recruitment round, carried out in the second quartile of 2016, two patients registered for the interviews. After these first interviews were conducted, it emerged that both patients were predominantly positive about SCF use. We then decided to hold a second recruitment round to ensure that we would get a sufficiently diverse picture of patient perspectives in line with the findings of Solstad et al. [19]. In this second round of recruitment, carried out in the third quartile of 2017, two patients again registered, one with a more or less positive attitude and one with an ambivalent attitude towards SCF use. This seemed to sufficiently correspond with perspectives that emerged from previous studies and based on this preliminary analysis was concluded that the recruitment phase could be terminated.
All interested patients agreed to be contacted, had experience with the use of high and low frequent SCF, and continued to participate. All participating patients were given pseudonyms to secure anonymity and signed an informed consent prior to the interview. They were allowed to withdraw their consent to record, transcribe or use their data during or after the interview. None of the patients withdrew their consent.
Patients
We recruited four patients, three women and one man, with an age between 22 and 47 years (M = 32.5, SD = 12.56). All patients were referred to psychological treatment by their general practitioner. The inclusion criteria were that patients were: (a) at least 18 years old; (b) suffered from mild to moderate psychological disorders; (c) mastered Dutch as their first or second language; and (d) were receiving treatment as usual added with SCF. All patients participated in a larger study [29] approved by the Medical Ethics Committee of the University of Twente (K15-11, METC Twente).
Data Collection
The in-depth interviews were the primary source for analyses. The conversations with the patients were conducted on the basis of a semi-structured interview based on a Dutch study of Boeschen Hospers [30] in patients’ experiences of SCF use, and on the themes found by Solstad et al. [19].
All interviews were conducted in-person by the lead researcher. Interviews were not time-limited, and patients could return for a second round of interviewing if desired. Interviews were concluded when the interviewee stated that they had nothing further to add. No patient used a second round of interviewing, and interviews lasted 42 min on average (range 33–51). All data were anonymized and then transcribed by a professional transcription agency. The lead researcher then reinspected the transcribed data and adjusted them where necessary by listening to the recordings.
SCF-tools
Low frequency SCF was already implemented at the participating centers as part of standard measurement. In our study high frequent SCF was added to low frequent SCF. The interviews focused on patients’ experiences with SCF in general, as well as the questionnaires used. Three SCF-tools were used in this study; the Partners for Change Outcome Management System (PCOMS; high frequent), the Outcome Questionnaire (OQ-45; low frequent) and the Mental Health Continuum Short Form (MHC-SF; low frequent). All three questionnaires were discussed in terms of content, length and used frequency.
PCOMS [31, 32] is a feedback system using two brief, four-item visual analogue scales, the Outcome Rating Scale (ORS) and the Session Rating Scale (SRS). PCOMS was used as a high frequent SCF-tool, to be used at every therapy session. In PCOMS, the ORS is administered at the beginning of each session, measuring intrapersonal, interpersonal, social, and overall wellbeing. The SRS is administered at the end of each session, measuring the affective bond, topics and goals, approach or method, and the overall working alliance. The ORS- and SRS-score and progress or decline from previous scores are discussed immediately and are used for improvement in upcoming therapy sessions. Miller et al. [31] examined the psychometric properties of the ORS, finding a high internal consistency, test-retest reliability and sensitivity to change. Duncan at al. [32] tested the psychometric properties of the SRS, finding similar validity and reliability as longer alliance measures.
The Dutch version of the MHC-SF [33, 34] was used as low frequent SCF tool, with a minimum of two times (at the begin and the end of therapy) and a maximum of four times (at the beginning, after 5 weeks, after 13 weeks, and at the end of therapy). It contains 14 items and taps the domains of emotional, psychological and social wellbeing. The total sum score is the overall experienced positive mental health. An item of the MHC-SF is “How often have you felt that you have contributed something important to society?”, and its psychometric properties were empirically tested by Lamers and colleagues [34] finding high internal reliability and moderate test-retest reliability.
The Dutch version of the Outcome Questionnaire (OQ-45; [35, 36] was also used as low frequent SCF tool, with a minimum of two times (at the begin and the end of therapy) and a maximum of four times (at the beginning, after 5 weeks, after 13 weeks, and at the end of therapy). The OQ-45 is measuring patients’ wellbeing and psychiatric symptoms. It uses a five-point scale ranging from 0 (never) to 4 (almost always) on three subscales: Symptom Distress, Interpersonal Relationships, and Social Role and contains 45 items. The total score ranges from 0 to 180. Examples of the OQ-45 are “I tire quickly”, or “I feel lonely”. The Dutch translation of the OQ-45 was examined by De Jong et al. [36], finding similar reliability and validity as the original OQ-45. Based on their findings De Jong et al. added a fourth scale to the OQ-45, called the Anxiety and Somatic Distress scale.
In summary, PCOMS was used in this study as a relatively short SCF-tool at high frequency, the MHC-SF as a medium length SCF-tool at low frequency, and the OQ-45 as relatively long SCF-tool at low frequency.
Methodological Approach
Reflexive Thematic Analysis (rTA; [23,24,25]) was used for the qualitative analysis by a Dutch team of SCF experts. Thematic analysis in general can be seen as an appropriate method for understanding a range of experiences across a data set [37]. rTA can be seen as an artful interpretive way of thematic analysis [38] and can be particularly useful to generate actionable outcomes [39].
To interpret our data, we used a constructionist epistemological approach. In this approach criteria for themes to be noteworthy are that they must be both recurring and meaningful. In line with this approach, we used an experiential orientation to data comprehension, aiming to highlight meaningfulness as described by the participating patients and acknowledge their subjectivity. Aligned with this constructionist and experiential strategy, we adopted an inductive, data driven approach instead of a deductive, theory driven approach. Finally, our coding strategy focused on latent coding instead of semantic coding, aiming to identify underlying assumptions and ideas.
Patients were interviewed on their perspective on the use of SCF, when it was added to treatment as usual. Interview topics were their views on: (a) SCF in general; (b) used questionnaires; (c) used frequency; (d) effect of SCF on therapy; and (e) perceived added value of SCF. The interview protocol is available in supplemental material (appendix A). The standards for reporting qualitative research as formulated by O’Brian and colleagues [40] were used to compile the manuscript.
Researchers
BB is a clinical psychologist and psychotherapist with 26 years of experience as a therapist. He is trained in several SCF methods, is an experienced SCF user and has conducted research on the added value of SCF in the past 15 years. He is also a senior lecturer and researcher at the University of Groningen. EdG is a psychologist and an experienced researcher, and coordinator of the implementation of Meaningful Outcomes, Value Based Health Care, Routine Outcome Monitoring (ROM) and Patient Satisfaction at Dimence, an in- and outpatient mental healthcare institute with around 3000 employees in the Netherlands. KdJ is a psychologist and assistant professor at Leiden University. Her research focuses on understanding differences in treatment outcomes between institutions, therapists and patients, as well as developing and testing interventions that improve outcomes in mainstream clinical practice. KdJ has two lines of research: personalized mental health care and therapist differences. Within the second line she also researches interventions that help therapists to provide more effective care, such as SCF, deliberate practice and training therapeutic skills. JdK is a clinical psychologist and psychotherapist and endowed professor at the University of Groningen to advance education and research on the treatment of complex grief. The last 10 years he has also been conducting SCF research together with the other members of this group.
Analysis
The analytical process consisted of the six phases of reflexive Thematic Analysis as proposed by Braun and Clarke [23]. The first phase, familiarization with the data, was done by the lead researcher, who also conducted the interviews. After the interviews had been transcribed, all recordings were listened to again and any incompleteness was corrected if necessary.
The first iteration of the second phase, coding of the data, was done by the lead researcher as well. In total 151 excerpts were coded in this phase. The second iteration was done by the lead researcher and EdG merging duplications and overlapping encodings, reducing the number of encodings to 80.
The lead researcher and EdG also conducted the third phase, generating initial themes, which consisted of three iterations. After the initial iteration of themes, it became clear that different themes were related to three different implementation phases; the start-up phase, the executive phase and the final phase of therapy. Thus, in the second and third iteration, six subthemes were formulated that seemed to be related to three overarching themes. The first overarching theme contained the necessary conditions for using SCF at all. The second theme involved building trust and careful collaboration around the use of SCF as an embedded part of therapy. The last overarching theme contained the effects of SCF on outcomes.
Reviewing and developing of themes, the fourth phase, was done by the entire SCF expert team in four rounds of adjustment. In this phase, the codes of the initial subtheme ‘compulsory use of SCF’ were grouped under the initial subtheme ‘embedded part of the therapy’. In addition, the initial overarching theme ‘the effects of SCF on outcomes’ was split into two preliminary sub-themes ‘effect on working relationship’ and ‘effect on outcomes’.
The SCF expert team conducted the fifth phase as well; refining, defining and naming themes, in two rounds of adjustment. In this phase, we formulated fully developed substantive themes and subthemes in consensus. The final report was produced by the entire team, all authors of this manuscript.
Results
Analyzing the data, we identified three themes: (1) Requirements to use SCF; (2) Modifiers for test-taking attitude; and (3) Effects on therapeutic process. These three themes are corresponding with the start-up phase, the executive phase and the final phase of therapy. All main themes had two subthemes. The themes seem to influence each other and their relationship is illustrated in Fig. 1.
The extent to which the requirements for the use of SCF are met, seems strongly related to the test taking attitude once SCF is used. All participants indicated that clear explanations are necessary to clarify the relevance of the questionnaires. This influence also goes the other way; the extent to which a positive test-taking attitude is formed seems related to the conditions imposed on the use of SCF as well. Some participants also indicated that after experiencing the added value of a specific questionnaire, they were more motivated to complete the questionnaire the next time. However, this relationship seems somewhat weaker because negotiating the conditions takes place in the early stages and the test-taking attitude gradually takes shape as the treatment progresses. The extent to which the conditions for the use of SCF are met combined with the extent to which a positive test-taking attitude is formed seem to be related to the effect on the therapeutic process. Each of the main themes and underlying subthemes are described in detail in the following sections, including illustrating quotes to clarify core meanings of the different subthemes.
Requirements to use SCF
As indicated above, three different SCF-tools were used by the participants; a relatively short SCF-tool that was used at high frequency, a medium SCF-tool that was used at low frequency, and a relatively long SCF-tool that was also used at low frequency. The interviews showed that the extent to which a patient is willing to use and complete a SCF-tool is related to the frequency in which it is used, the length of the tool and the complexity of the questions on the one hand, and its perceived validity on the other hand.
Balance between effort it takes to complete SCF and perceived validity
Participants indicated that the relatively short questionnaire did not provide very detailed information, but was very user-friendly. Participants also indicated that the advantage of the longer questionnaires was that you dive deeper into a problem and thus gain more insight into what is going on.
Regarding the relatively longer questionnaires, it was also indicated that it was quite a lot of work, that not all questions were relevant and that using these longer SCF-tools should also yield something. One participant was also disturbed by questions that came back in a slightly different form and made a plea for computer adaptive testing:
There’s a lot of repetition in it. And then I think, I have just filled that in too. [ ] There were for instance a lot of questions about whether you drink or do drugs. Look, if that doesn’t apply to you, then that question will still come up every time. Yes, that was asked three times. If you already say no to the first one, then I think it is unnecessary to fill in the other two [ ] if it has been modified slightly. So if, for example, you can immediately declare alcohol and drugs, no, and all those questions below that will disappear. Then I think it’s a good questionnaire.
Balance between used frequency and perceived validity
The combination of long and short SCF-tools was seen as helpful, when the short tools were used frequently and the longer tools occasionally to ask more specifically about different problems. Participants stated that the longer SCF-tools should best be used at the beginning and at the end of therapy, and in longer treatments, for example every three months:
I would have [the longer questionnaires] administered at the beginning and the end anyway and then… Yes, I think it depends a bit on how long your treatment lasts. Yes, if you are only here for three months and you receive such a questionnaire ten times, that is too much. But I think I would do it an average of three times. Once at the beginning and the end and once in the middle. But suppose you are here for a year, then I would do it more often. Once a quarter for instance, something like that.
Modifiers for test-taking attitude
The test-taking attitude seemed to be mainly related to the extent to which therapist and patient collaborated on the one hand, and by the extent to which SCF was an embedded part of the treatment on the other hand.
Quality of therapist-client alignment
All participants reported that the building of trust is important in successfully using SCF. Trust can be improved through an equal approach and a solidly built collaboration. It is important that the information obtained is handled carefully in a joint conversation to determine how to make the results meaningful. One participant stated:
You must have great confidence in the person treating you, because he or she is immediately watching. So it’s, … the questions are very personal. And then you really have to have confidence in your practitioner. And then, then it works very well. If you don’t trust your practitioner, well, I guess you’re going to fill it in based on what the practitioner would like to see. [ ] And my therapist understood what I meant, where my problem was and worked on it. So that’s what I mean by trust. [ ] It also seems that you then expect the other person to handle the information carefully.
SCF as an embedded part of therapy
The participants indicated that a thorough explanation about the content and use of the SCF-tools is necessary before the start. Specific instructions about the necessity and added value of negative feedback was also considered important. In addition, patients recommended the practitioner to actively structure the treatment and make SCF an embedded part of the therapy. One of the participants, who also used online therapy tools, stated:
If you provide blended treatment, both face-to-face therapy sessions and internet therapy, and you also have completed SCF-tools, then it is important that you discuss the online tools and SCF in the face-to-face sessions. This will make it more lively and a coherent whole. By doing so, you show your involvement as a practitioner as well.
Effects on therapeutic process
With regard to the effect of SCF on the therapeutic process, two different sub-themes could be distinguished; one that focused more on the course of the treatment, and one that focused more on the end result.
Focus on task and goals, and shared responsibility
The participants stated that using SCF helped them realize that they were not just having a conversation with their therapist, but that they also needed to focus on the tasks and goals of the therapy. In particular, the short questionnaires used at high frequency contributed to this. One of the participants stated:
Completing and discussing the ORS together at the start leads to a shared responsibility for the quality of the session. The SRS is a great way to make adjustments afterwards if, despite discussing the ORS, the session did not go entirely as desired.
Effect on outcome and satisfaction
Finally, most of the participants indicated that the use of SCF led to more satisfaction with the treatment and the outcome. Completing the longer questionnaires in particular confirmed improvement and growth when therapy was completed. They also stated that the graphical representation helped to compare feeling and ‘fact’:
Yes, those [questionnaires] were discussed and then you could also see it in a graph. Then you could also see how, how, plus and minus what you had in it, so to speak. It is, yes, it is confrontational. If you think: I don’t feel so good today, and you see on the screen that you actually feel better [compared to earlier], that’s it… It’s good for yourself, and the same goes for the other way around.
One participant however, who did not improve sufficiently during therapy, indicated that it was confronting to see this reflected in the questionnaires. The lack of progress shown in the questionnaires made it clear that a different, more intensive form of treatment was needed elsewhere. On the one hand, the participant felt that a different form of treatment was needed, but on the other hand, also wanted to stay with the current therapist. However, when they looked at the SCF, it became clear that the latter was not appropriate.
Besides the relative homogeneity found in the answers and themes, we also found an important difference between the participants, namely their level of computer skills. These skills varied from moderate to expert, which appeared to influence how they experienced the user-friendliness of administration. This difference in skills seemed to particularly affect the theme ‘Requirements to use SCF’ because participants with lower computer skills found it more difficult to complete the online questionnaires.
Discussion
In this study several Dutch patients interviews on the use of SCF were analyzed through reflexive Thematic Analysis by an SCF expert team, to generate implications for daily practice and optimize its implementation in the Netherlands. Three themes could be identified, all of which have two sub-themes.
The first theme is related to the start of therapy and describes requirements to use SCF. In this phase it seems important that the therapist and patient find a balance between effort to complete SCF in terms of complexity, length and frequency, and the perceived validity of the used SCF system. Longer, complex questionnaires are preferably used at low frequency and shorter simpler questionnaires at high frequency.
After this first start-up phase, modifiers for test-taking attitude can be distinguished, with SCF as an embedded part of therapy on the one hand, and the quality of Therapist-Client alignment on the other. If these two phases are completed successfully, the chance seems to increase that SCF has positive effects on the therapeutic process and improve outcome and satisfaction.
The results found are in line with the two helping meta-themes of SCF found by Solstad et al. [18]; SCF led to increased patient empowerment, and increased collaboration between patient and therapist. The participating patients stated that SCF led to an increased focus on task, goals, and to an increased awareness of shared responsibility.
Our results are also aligned with one of the hindering meta-theme found by Solstad et al. [18] reporting that SCF is not always sufficiently corresponding with what patients regard as valuable outcomes. Our participants endorsed that questionnaires should sufficiently correspond with what they regard as valuable outcomes and added that this partly depends on the length, complexity and frequency of the questionnaire used.
Contrary to the findings of Solstad and colleagues, SCF did not induce suspicion towards therapists in our study. This may be related to the fact that in our study feedback generally led to an improvement in treatment outcome [7]. On the other hand, the participants indicated that SCF does not automatically have added value. Thus, when the requirements are insufficiently met, and the test taking attitude is poor, it will probably have a negative effect, as described by Wolpert [16].
Finally, we found that SCF can also be confronting, especially if no progress can be observed. It forces to change the course of treatment, or sometimes even the treatment setting, even if the working alliance is satisfactory. In this way, SCF can help to close unhelpful treatments in time and lead the way to a more helpful form of therapy.
Implications
This study provides evidence that SCF does not automatically lead to improvement in Dutch mental healthcare and that an ongoing process of therapist-client alignment seems required. This starts with the preparation, in which frequency, length, user friendliness and complexity of the questionnaires used must be balanced with their perceived added value. This alignment seems best continued through an solidly built collaboration to determine how to ensure that SCF becomes a meaningful embedded part of the therapy. Throughout the progression of therapy, it seems necessary to keep discussing SCF and adjust it if necessary. In other words, SCF and therapy are communicating vessels. It is not only necessary to adjust therapy based on SCF, but it is also necessary to adjust SCF based on the course of therapy.
This ‘communicating vessels-approach’ is not common practice in SCF use neither in the Netherlands nor in other countries. Most often the questionnaires are used in a fixed frequency of completion, determined at the outset of therapy. Treatment will be adjusted in the further course based on SCF, but not the other way around. However, the patients in this study make a clear plea for the possibility of adjusting not only treatment, but also type and frequency of questionnaires. This may be related to cultural aspects. The Netherlands is known for its neo-corporate ‘Polder Model’ in which it is very common to negotiate together on all kinds of areas, and this model is deeply anchored in the culture [41].
In addition, the desire to adjust the use of SCF during the course of treatment may also be related to the added predicted value of SCF. In the study of Bovendeerd et al. [7] the added value of SCF was mainly found at the beginning of therapy, over 76% of the added improvement was achieved in the first three months. If SCF is continued with the same intensity after these three months, the efforts will remain the same, but the benefits will decrease. If that is the case, it seems logical to adjust the intensity as well.
Limitations
The current study combined the perspective of a limited number of patients in Dutch mental healthcare when high and low frequent SCF was added to their therapy with the perspective of a Dutch team of SCF experts using reflexive Thematic Analysis (rTA) as described by Braun and Clarke [24]. This method is specifically designed for profound subjective analysis concerning a specific topic, in this case SCF implementation in the Netherlands. This subjectivity is a strength on the one hand, because it can lead to profound interpretations and useful practical implications. This subjectivity is also its limitation, another team of experts might come to different conclusions.
Regarding the reflexivity of this research team as formulated by O’Brian and colleagues [40], there is a consciously chosen overlap between the researchers’ characteristics and the interviewed patients. We chose to combine the perspective of Dutch patients in outpatient mental healthcare with the perspective of a team of Dutch SCF experts, and used reflexive thematic analysis to generate themes and actionable insights for clinical practice. This profound subjective approach optimizes an in-depth analysis concerning implementing SCF in Dutch outpatient mental healthcare. This approach might simultaneously lead to limited transferability, especially for SCF implementation in other countries.
Conclusion
Adding SCF to therapy was perceived as helpful by Dutch patients in psychotherapy if two conditions were met; (1) Creating a right balance between effort and yield for SCF to be used at all, and (2) embedding SCF as an integral part of therapy, through therapist-client alignment. Throughout the course of therapy, it might be useful to perceive SCF and therapy as communicating vessels: therapy must be adjusted based on SCF, and SCF use must be adjusted based on the course of therapy. If these conditions are met, it will probably improve the working alliance, therapy outcome and treatment satisfaction.
Data availability
The data that support the findings of this study are available from the corresponding author, BB, upon reasonable request.
Abbreviations
- MHC-SF:
-
Mental Health Continuum Short Form
- OQ-45:
-
Outcome Questionnaire
- ORS:
-
Outcome Rating Scale
- PCOMS:
-
Partners for Change Outcome Management System
- rTA:
-
reflexive Thematic Analysis
- SCF:
-
Systematic Client Feedback
- SRS:
-
Session Rating Scale
References
de Jong K, Conijn JM, Gallagher RAV, Reshetnikova AS, Heij M, Lutz MC. Using progress feedback to improve outcomes and reduce drop-out, treatment duration, and deterioration: a multilevel meta-analysis. Clin Psychol Rev. 2021;85:102002. https://doi.org/10.1016/j.cpr.2021.102002.
de Jong K, Douglas S, Wolpert M, Delgadillo J, Aas B, Bovendeerd B, Carlier I, Compare A, Edbrooke-Childs J, Janse P, Lutz W, Moltu C, Nordberg S, Poulsen S, Rubel JA, Schiepek G, Schilling VNLS, van Sonsbeek M, Barkham M. Using Progress Feedback to Enhance Treatment outcomes: a narrative review. Adm Policy Ment Health. 2024. https://doi.org/10.1007/s10488-024-01381-3. https://doi.org/10.1007/s10488-024-01381-3. Advance online publication.
Lambert MJ, Whipple JL, Kleinstäuber M. Collecting and delivering progress feedback: a meta-analysis of routine outcome monitoring. Psychother (Chic). 2018;55(4):520–37. https://doi.org/10.1037/pst0000167.
Bickman L, Douglas SR, De Andrade AR, et al. Implementing a measurement feedback system: a tale of two sites. Adm Policy Ment Health. 2016;43(3):410–25. https://doi.org/10.1007/s10488-015-0647-8.
Brattland H, Koksvik JM, Burkeland O, et al. The effects of routine outcome monitoring (ROM) on therapy outcomes in the course of an implementation process: a randomized clinical trial. J Couns Psychol. 2018;65(5):641–52. https://doi.org/10.1037/cou0000286.
Lewis CC, Boyd M, Puspitasari A, et al. Implementing measurement-based care in behavioral health: a review. JAMA Psychiatry. 2019;76(3):324–35. https://doi.org/10.1001/jamapsychiatry.2018.3329.
Bovendeerd B, De Jong K, De Groot E, Moerbeek M, De Keijser J. Enhancing the effect of psychotherapy through systematic client feedback in outpatient mental healthcare: a cluster randomized trial. Psychother Res. 2022;32(6):710–22. https://doi.org/10.1080/10503307.2021.2015637.
de Jong K, de Goede M. Why do some therapists not deal with outcome monitoring feedback? A feasibility study on the effect of regulatory focus and person-organization fit on attitude and outcome. Psychother Res. 2015;25(6):661–8. https://doi.org/10.1080/10503307.2015.1076198.
Bovendeerd B, de Jong K, de Groot E, Moerbeek M, Hafkenscheid A, de Keijser J. The effect of therapist characteristics on the use and outcome of systematic client feedback in outpatient mental healthcare. Clin Psychol Psychother. 2023;30(5):1146–57. https://doi.org/10.1002/cpp.2873.
Rodriguez A, Terrones L, Brookman-Frazee L, Regan J, Smith A, Lau AS. Associations between cultural identity and attitudes toward routine progress monitoring in a sample of ethnically diverse community therapists. Psychol Serv. 2020;17(3):282–90. https://doi.org/10.1037/ser0000327.
She Z, Xu H, Cormier G, Drapeau M, Duncan BL. Culture matters: Chinese mental health professionals’ fear of losing face in routine outcome monitoring [published online ahead of print, 2023 Jul 31]. Psychother Res. 2023;1–12. https://doi.org/10.1080/10503307.2023.2240949.
Douglas S, Bala N, Bovendeerd B, van Sonsbeek M, Hovland RT, Moltu C. Cross-cultural leadership perspectives on the use of clinical feedback in mental health. Paper presented at: Society for Psychotherapy Research 52nd Annual International Meeting; June 23–26, 2021; Heidelberg, Germany.
Happell B, Roper C, Gough K. A user-derived evaluation framework for mental health services: does routine outcome measurement satisfy the objectives of service users? Final report. Rockhampton: Central Queensland University; 2007.
Guthrie D, McIntosh M, Callaly T, Trauer T, Coombs T. Consumer attitudes towards the use of routine outcome measures in a public mental health service: a consumer-driven study. Int J Ment Health Nurs. 2008;17(2):92–7. https://doi.org/10.1111/j.1447-0349.2008.00516.x.
Unsworth G, Cowie H, Green A. Therapists’ and clients’ perceptions of routine outcome measurement in the NHS: a qualitative study. Counselling Psychother Res. 2012;12(1):71–80. https://doi.org/10.1080/14733145.2011.565125.
Hoy J. The space between: making room for the unique voices of mental health consumers within a standardized measure of mental health recovery. Adm Policy Ment Health. 2014;41(2):158–76. https://doi.org/10.1007/s10488-012-0446-4.
Wolpert M. Uses and abuses of patient reported outcome measures (PROMs): potential iatrogenic impact of PROMs implementation and how it can be mitigated. Adm Policy Ment Health. 2014;41(2):141–5. https://doi.org/10.1007/s10488-013-0509-1.
Wolpert M, Curtis-Tyler K, Edbrooke-Childs J. A qualitative exploration of patient and clinician views on Patient Reported Outcome Measures in Child Mental Health and Diabetes Services. Adm Policy Ment Health. 2016;43(3):309–15. https://doi.org/10.1007/s10488-014-0586-9.
Solstad SM, Castonguay LG, Moltu C. Patients’ experiences with routine outcome monitoring and clinical feedback systems: a systematic review and synthesis of qualitative empirical literature. Psychother Res. 2019;29(2):157–70. https://doi.org/10.1080/10503307.2017.1326645.
Hovland RT, Ytrehus S, Mellor-Clark J, Moltu C. How patients and clinicians experience the utility of a personalized clinical feedback system in routine practice. J Clin Psychol. 2023;79(3):711–28. https://doi.org/10.1002/jclp.22992.
Moltu C, Veseth M, Stefansen J, et al. This is what I need a clinical feedback system to do for me: a qualitative inquiry into therapists’ and patients’ perspectives. Psychother Res. 2018;28(2):250–63. https://doi.org/10.1080/10503307.2016.1189619.
Koementas-de Vos MMW, van Dijk M, Tiemens B, De Jong K, Witteman CLM, Nugter MA. (2022). Feedback-informed Group Treatment: A Qualitative Study of the Experiences and Needs of Patients and Therapists, International Journal of Group Psychotherapy, 2022:72(3):193–227.
Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Res Psychol. 2006;3(2):77–101. https://doi.org/10.1191/1478088706qp063oa.
Braun V, Clarke V. Reflecting on reflexive thematic analysis. Qualitative Res Sport Exerc Health. 2019;11(4):589–97. https://doi.org/10.1080/2159676X.2019.1628806.
Braun V, Clarke V, Can I. Use TA? Should I use TA? Should I not use TA? Comparing reflexive thematic analysis and other pattern-based qualitative analytic approaches. Couns Psychother Res. 2021;21:37–47. https://doi.org/10.1002/capr.12360.
Byrne D. A worked example of Braun and Clarke’s approach to reflexive thematic analysis. Qual Quantity. 2022;56:1391–412. https://doi.org/10.1007/s11135-021-01182-y.
Seligman MEP. Flourish. New York: Free; 2011.
de Shazer S, Dolan Y, Korman H, McCollum E, Trepper T, Berg IK. Haworth brief therapy series. More than miracles: the state of the art of solution-focused brief therapy. New York, NY, US: Haworth; 2007.
Bovendeerd B, de Jong K, Colijn S, et al. Systematic client feedback to brief therapy in basic mental healthcare: study protocol for a four-centre clinical trial. BMJ Open. 2019;9(5):e025701. https://doi.org/10.1136/bmjopen-2018-025701.
Boeschen Hospers JM. Evalueren per sessie: het gehele behandelproces in zicht: een pilotstudie naar het gebruik van ROM bij oudertrainingen. [Master’s thesis, Twente University]. 2012. https://purl.utwente.nl/essays/62326 Accessed 10 Nov 2023.
Miller SD, Duncan BL, Brown J, Sparks J, Claud D. (2003). The outcome rating scale: A preliminary study of the reliability, validity, and feasibility of a brief visual analog measure. Journal of Brief Therapy, 2023;2:91–100.
Duncan B, Miller S, Sparks J, Claud D, Reynolds L, Brown J, Johnson LD. The Session Rating Scale: preliminary psychometric properties of a working alliance measure. J Brief Therapy. 2003;3:3–12.
Keyes CL. The mental health continuum: from languishing to flourishing in life. J Health Soc Behav. 2002;43(2):207–22.
Lamers SM, Westerhof GJ, Bohlmeijer ET, ten Klooster PM, Keyes CLIËNT. Evaluating the psychometric properties of the Mental Health Continuum-Short Form (MHC-SF). J Clin Psychol. 2011;67(1):99–110. https://doi.org/10.1002/jclp.20741.
Lambert MJ, Morton JJ, Hatfield DR, Harmon C, Hamilton S, Shimokawa K, et al. Administration and scoring manual for the OQ-45.2 (Outcome Questionnaire). 3 ed. Wilmington, DE: American Professional Credentialing Services LLC; 2004.
de Jong K, Nugter MA, Lambert MJ, Burlingame. GM. Handleiding Voor afname en scoring Van De Outcome Questionnaire (OQ-45). [Manual for administration and scoring of the Outcome Questionnaire (OQ-45)]. Salt Lake City: OQ Measures LLC; 2009.
Kiger ME, Varpio L. Thematic analysis of qualitative data: AMEE Guide 131. Med Teach. 2020;42(8):846–54. https://doi.org/10.1080/0142159X.2020.1755030.
Finlay L. Thematic analysis: the ‘Good’, the ‘Bad’ and the ‘Ugly’. Eur J Qualitative Res Psychother. 2021;11:103–16.
Sandelowski M, Leeman J. Writing usable qualitative health research findings. Qual Health Res. 2012;22(10):1404–13. https://doi.org/10.1177/1049732312450368.
O’Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med. 2014;89(9):1245–51. https://doi.org/10.1097/ACM.0000000000000388.
Woldendorp JJ. The Polder Model: From Disease to Miracle? Dutch Neo-corporatism 1965–2000. Amsterdam: Thela Thesis, 2005. 399 p.
Acknowledgements
The authors wish to thank the patients from the participating centers of Mindfit for their participation in the study, the patient advisory board of the Dimence Group for their advice, and numerous colleagues of the Dimence Group for their additional help.
Funding
This work was supported by the Research-foundation of Postmaster Psychologie Opleidingen (PPO) the Netherlands, grant number PPO-RF-18CM, and the Dimence Groep, the Netherlands, grant number CWOBB112014. The University of Groningen financially supported JdK’s contributions to the study. None of the sponsors had a role in the design and conducting of the study nor in preparation, review, or approval of the manuscript.
Author information
Authors and Affiliations
Contributions
BB wrote the study proposal, the manuscript and led the research project. BB, EdG and JdK developed the study design and coordinated the data acquisition. JdK and KdJ supervised the research project. BB was involved in every step of the data-analysis, EdG participated in generating the initial themes, EdG, KdJ and JdK were involved in the reviewing and developing of themes and in the refining, defining and naming of themes. All authors provided comments on manuscript drafts and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by the Medical Ethics Committee of the University of Twente (K15-11, METC Twente). All participants were informed about the content of this study and the potential risks before each interview. Written consent was obtained from all participants.
Consent for publication
Not Applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Bovendeerd, B., de Jong, K., de Groot, E. et al. Patient perspectives on systematic client feedback in Dutch outpatient mental healthcare, a qualitative case reports study. BMC Health Serv Res 24, 957 (2024). https://doi.org/10.1186/s12913-024-11404-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-024-11404-2