Abstract
Background
The continuum of care (CoC) in maternal health refers to the continuity of individual reproductive health care across the antenatal, intrapartum, and postnatal periods. The CoC is an indicator of the quality of maternal and newborn health outcomes and women’s empowerment is crucial to improving maternal and neonatal health service access and utilisation.
Objective
To examine the spatial patterns of continuum of care use for maternal and neonatal health services and its correlation with women’s empowerment.
Methods
We analysed data from the Ethiopian Demographic and Health Surveys (EDHS) of 2011 and 2016. All women aged 15–49 who had live births in the preceding five years of the DHS surveys were included in the analysis. We measured the continuum of care using the modified co-coverage index (CoCI), which consisted of six indicators. Women’s empowerment was assessed using a validated survey-based Women’s Empowerment (SWPER) index. We used the Getis-Ord-Gi* spatial analysis tool to portray locations with clusters of CoC service use and spatial correlations between CoC use and women empowerment.
Results
None of the newborn-mother pairs in the 2011 survey received the entire continuum of care and only 2.5% of newborn-mother pairs received the full range of continuum of care services in the 2016 survey. In 2016, 6.9% of mother-newborn pairs received the basic CoC services (four or more antenatal care [ANC] visits, skilled birth attendance [SBA], and postnatal care [PNC]), and no mother-newborn pair received all three services at the same time in 2011. The Amhara, Afar, and Somali regional states had the least CoC service use in both surveys. There was a positive spatial correlation between CoC use and women’s empowerment domains.
Conclusion
Our analysis showed that the use of four or more ANC visits, SBS, newborn PNC, Bacillus Calmette-Guérin (BCG) vaccine uptake, and tetanus toxoid protection at birth were low in Ethiopia. Women empowerment domains were found to have a positive spatial correlation with CoC services use. To improve and preserve continuity of care, it is critical to leverage every maternal health facility encounter to encourage sustained service usage at each step of the continuum. Government policies should prioritise women’s empowerment and raise public awareness of maternity services.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
One of the strategies to reduce maternal and neonatal mortality is to improve healthcare provisions for mothers and babies across the reproductive continuum [1]. Reproductive health care use and positive outcomes of maternal and newborn health are inextricably linked. According to a Global Burden of Disease study, countries with a maternal mortality ratio (MMR) of less than 15 per 100,000 live births had 98% coverage in at least one antenatal care visit, 95% coverage in four antenatal care visits, 97% coverage in facility-based delivery, and 99% coverage of skilled birth attendance [2]. Countries with lower maternal health services coverage—76% for at least one antenatal care visit, 45% for four antenatal care visits, 41% for facility-based deliveries, and 48% for skilled birth attendance—had maternal mortality ratios (MMR) exceeding 500 per 100,000 live births [2].
Despite the initiatives to achieve universal health coverage (UHC) by the Ethiopian government, maternal and neonatal health services utilisation is quite low [3, 4]. The Ethiopian Health Sector Transformation Plan (HSTP-II) aspires to achieve UHC through expanding access to services and improving the provision of quality and equitable, comprehensive health services at all levels. Enhancing maternal, neonatal and child health are among the priority targets in the plan aiming to increase skilled delivery attendance to 76%, coverage of ANC 4 to 81%, and coverage of postnatal care to 76% [5]. According to the 20,189 mini-EDHS data, less than half (48%) of live births occurred in health facility and only 43% of pregnant women got four or more antenatal care visits. Recent studies based on the 2016 EDHS indicate that coverage COC remains critically low in Ethiopia [6]. Furthermore, there is a substantial dropout rate among women from the maternal continuum of care after initial antenatal care booking. These findings highlight a significant public health challenge in the country [7]. Access to basic obstetric and neonatal care services [8], as well as the utilisation of maternal health services [9], varies significantly among administrative areas in the country.
The CoC is one of the health service strategic frameworks and indicators of maternal, newborn, child and adolescent health [1, 10]. It has two dimensions; the first dimension encompasses the time of care throughout the lifecycle, during pregnancy, childbirth, childhood, and adolescence. The second dimension indicates the place that spans home, community, and health care [10, 11]. Each stage in the continuum should be a positive experience to ensure that women and their babies reach their full potential for health and well-being [12, 13].
There are two summary measures of coverage: the composite coverage index (CCI) and the co-coverage index (CoCI) [14]. The CCI is the weighted average coverage of services calculated at a group level CoCI indicator is a simple count of how many services are received at an individual level out of a set of services [15].
Maternal healthcare utilisation has been connected to gender power dynamics in low- and middle-income countries [16]; and women’s empowerment has been widely considered as an important concept in international development goals [17, 18]. The World Bank defined women empowerment as a person’s capacity to make effective choices, that is, as the capacity to transform choices into desired actions and outcomes [19]. The extent or degree to which a person is empowered is influenced by personal agency (the capacity to make purposive choice) and opportunity structure (the institutional context in which choice is made) [19]. In this study, we used the survey-based Women’s Empowerment (SWPER) index to measure women’s empowerment domains [20]. The SWPER index is suitable for survey-based data and validated initially for African countries and that has been expanded to low- and middle-income countries. Studies in low- and middle-income countries have shown that women’s empowerment can play an important role in maternal health services use [21,22,23,24]. A study from 31 developing countries showed that women with the highest empowerment score were more likely to use modern contraception, attend four or more antenatal care visits and have a skilled attendant at birth [18]. Another study from Albania showed that the number of ANC visits was positively related with the number of decisions a women made in the household [24]. Plenty of studies investigated the factors affecting maternal CoC service use by examining individual level data [6, 7, 9, 23, 25]. However, our study aims to illustrate the interaction between CoC use and women’s empowerment through spatial analysis. Visual tools can create maps and spatial representations of data, highlighting areas of concern and success. These visualisations help in quickly identifying patterns, facilitating better decision-making and communication [26]. Policymakers and health planners can use spatial analysis to allocate resources more efficiently and design targeted interventions. For example, regions with low CoC coverage and low women’s empowerment might require more focused initiatives [27].
Methods and materials
Data source and extraction
We analysed data from the EDHS. Four waves of EDHS surveys have been conducted in Ethiopia so far at five-year intervals since 2000. We used the 2011 and 2016 EDHS surveys for the current analysis because the other surveys did not incorporate all indicators for CoCI. The 2011 and 2016 EDHS surveys used the Ethiopian population and housing census sampling frame conducted in 2007 by the Ethiopia Central Statistical Agency (CSA). The samples for the EDHS survey were selected using a two-stage cluster sampling technique using census enumeration areas (EAs) as primary sampling units and households as secondary sampling units. An enumeration area (EA), also known as a cluster, is a small geographic region with 150 to 200 households [28].
The EDHS samples were stratified and selected in two stages. Regions were stratified into urban and rural areas, and samples of EAs were selected independently in each stratum in two stages. The sampling frame contains information about the EA location, type of residence (urban or rural), and the estimated number of residential households. In the selected EAs, a complete listing of households was carried out for each survey. The response rate for household interviews in both the 2011 and 2016 surveys was 98%, while the response rates for eligible women were 95% in 2011 and 94.6% in 2016. More detailed methods are described in the main reports [29, 30].
Population
All women aged 15 to 49 years who were married (in union) at the time of data collection and had a live birth in the five years preceding the survey were included. As the women’s empowerment domains such as attitude towards husband beating and decision-making power in the household measured based on the interactions between the woman and her husband, only married (in union) women were included. The DHS survey collects data on antenatal, perinatal and postnatal care services for the most recent births, and the analysis was based on these populations. Newborns younger than two days were excluded to allow sufficient time for postnatal care assessment. The study comprised 14,174 women-newborn pairs.
Measurements
The primary outcome was the use of maternal and neonatal CoC services. We defined the continuum of care for mother and newborn care during pregnancy, childbirth, and the postnatal period, which has been used in previous literature [31, 32], and we used the co-coverage index for spatial analysis as per the recommendation elsewhere [14]. Continuum of care service was measured using the modified CoCI, which comprised of six indicators, including at least four antenatal care visits, tetanus protection at birth, skilled birth attendance, BCG vaccination, breastfeeding initiation within one hour of birth, and postnatal care visits for babies within the first two days of birth (see Table 1).
We used the survey-based Women’s Empowerment (SWPER) index to measure women’s empowerment domains. [33], which has three domains: (1) decision-making power, (2) attitudes towards violence, and (3) social independence. The decision-making index was computed from three items related to health care, major household purchases, and visiting friends/relatives. The second domain is an index created by items that capture attitudes towards violence and women’s opinions about whether wife beating is justified in various scenarios. The third domain was created from items related to social independence, including education, frequency of reading newspapers or magazines, age at birth of the first child and first cohabitation, and age and education differences between the woman and her husband. A composite measure for each domain was created using standardised scores of the corresponding items. First, the variables were recoded as shown in the supplementary file (see Table S1 ), and standardisation was carried out based on the SWPER guideline [20].
Data analysis
Descriptive analyses of percentages of services utilisation in the continuum at each survey was carried out. The spatial patterns of maternal and neonatal CoC use were analysed, and statistically significant clusters of lower CoCI values were used to compare CoC coverage. Global Moran’s I statistics [34] and Getis-Ord Gi* statistics were adopted to detect the spatial clusters of the continuum of care service use. Global Moran’s I is a scale that ranges from − 1 to + 1, where a value of + 1 indicates the entire distribution showed similarity [35, 36], and spatial clustering was detected. Once the presence of overall clustering is detected in the data, the Getis-Ord Gi* statistics was used to identify the local hot and cold spot areas. A cold spot is an area where lower CoCI values are significantly clustered. In contrast, a hot spot area is one where higher CoCI values are clustered compared to its surroundings [37].
Spatial interpolation [38] was applied to obtain a value of the continuum of care at locations where data had not been recorded. We used the empirical Bayesian kriging (EBK) [39] method to interpolate data to the un-sampled areas. The spatial patterns of the continuum of care were displayed using high-resolution maps.
We used a geographically weighted regression (GWR) model to see the spatial relationships between CoC use and women empowerment. Geographically Weighted Regression is a statistical technique that allows variations in relationships between predictors and outcome variables over space to be measured within a single modelling framework [40]. The underlying idea of GWR is that parameters may be estimated anywhere in the study area given a dependent variable and a set of one or more independent variables which have been measured at places whose location is known [41]. We applied GWR with an adaptive Kernel-type approach. Kernel type in the GIS ArcToolbox specifies if the Kernel is constructed as a fixed distance or if it is allowed to vary in extent as a function of feature density. The adaptive approach allows the spatial context to vary as a function of a specified number of neighbours. Where feature distribution is dense, the spatial context is smaller; where feature distribution is sparse, the spatial context is larger [40].
Ethics approval
Ethical approval was granted by the University of Technology Sydney Human Research Ethics Committee (Approval number: ETH19-4488). Approval to access and use the DHS dataset was obtained from the DHS program. The analysis used secondary data, and there was no contact with study participants.
Results
We analysed the continuum of care coverage as measured by the co- coverage index, which consists of six indicators. A total of 14,174 newborn-mother pairs (7,131 from 2011 to 7,043 from 2016 EDHS surveys) were included in the analysis. The completion of each indicator of the co-coverage index was examined. In both surveys, postnatal care for newborn babies had the lowest utilisation coverage, with 0.3% in 2011 and 12.0% in 2016 (see Table 2).
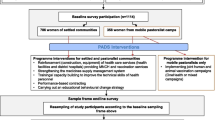
None of the newborn-mother pairs utilised the complete continuum of care services in the 2011 survey, and 13% of newborn-mother pairs received no continuum of care intervention at all. In the 2016 survey, 2.5% of newborn-mother pairs utilised complete CoC services, while 6.2% did not receive any service. One in ten in 2011 and one in four mother-newborn pairs in 2016 used over half (four or more) of the CoC services (see Fig. 1). In 2016, 6.9% of mother-newborn pairs received the basic CoC services (four or more ANC visits, SBA, and postnatal care), and no mother-newborn pair received all three treatments at the same time.
The number of continuum of care services received by newborn-mother pair varies related to educational level and wealth position, with better outcomes at higher educational levels and richer wealth quantiles (see Table 3).
Spatial patterns of continuum of care coverage
The interpolated estimation, i.e. the predicted spatial distributions of the continuum of care, including for areas where data were not taken, showed that in 2011 EDHS survey most places in the Amhara, Afar and Somali regional states had the least coverage for maternal and newborn health services. On the other hand, Harari, Dire Dawa, Tigray, and a few locations in Oromia regional state, had hot spots suggesting better coverage of maternal and newborn health services.
Similarly, in the 2016 survey, the majority of Amhara, Afar, and Somali regional states had the least service coverage. Better service coverage has been mapped most locations of Oromia, Addis Ababa, Harari, Diredawa, SNNP, Benshangul Gumuz, Tigray regional states and a few locations in Amhara and Gambela regional states.
Figure 2 shows interpolated spatial patterns of the continuum of care coverage for maternal and neonatal health services for the 2011 EDHS (upper panel) and 2016 EDHS (lower panel). The dark red colour indicates the hot spot areas (high coverage); the dark blue colour indicates the cold spots (low coverage), and the yellow ramp colour indicates areas with no significant distribution or random distributions of the CoC service use. The Co-coverage index (CoCI) intervals indicate the average number of continuum of care services received at a cluster level.
We investigated the relationships between the spatial clustering of the continuum of care use and women empowerment domains. We fit a GWR model to evaluate the relationships and found a positive spatial correlation between CoC service use and women empowerment domains. In the 2011 EDHS survey, there was a stronger positive spatial correlation between attitude towards violence and CoCI in north-eastern, central, and western Ethiopia, Dire Dawa, Harari, Tigray, central and western Oromia, parts of Benishangul Gumuz and Gambella regional states demonstrated a positive spatial correlation between CoCI and decision-making domain. Except for the Amhara region, Gambella, and a few areas in Oromia, the social independence domain was found to have a positive correlation with CoCI across the country (Figure S1).
In the 2016 survey, areas in north-western, central, central-east, western, and south-western Ethiopia were found to have a positive spatial correlation between CoCI and attitude towards violence. Northern, central eastern, northwestern, and southwestern Ethiopia revealed a positive spatial correlation between CoCI and the decision-making domain. Except for the central and western parts of Ethiopia, the social independence domain had a stronger spatial correlation with CoCI throughout the country (see Figure S2).
The global estimation summary indicated an overall positive relationship between the co-coverage index and three of women’s empowerment domains. As the empowerment domains’ scores increased, so did the CoCI score. The relationship between social independence and CoCI was found to be stronger in both surveys.
Discussion
We examined the performance of CoC services, spatial patterns of the continuum of care (CoC) use for maternal and neonatal health services and the relationship between the continuum of care use and women’s empowerment based on the 2011 and 2016 EDHS surveys. In the five years preceding the surveys, one in five pregnant women in 2011 and less than one in three in the 2016 EDHS had at least four antenatal care visits. On the other hand, one in ten pregnant women used skilled birth attendance in 2011, a figure that rose to one in three by 2016. These findings are significantly lower than the service uptake targets set by the Ethiopian health sector strategic plan to be achieved by the end of 2020 [42], which can also impact attaining the SDG targets of reducing maternal and neonatal mortality. These findings place Ethiopia among the bottom five countries in terms of ANC services utilisation, along with Afghanistan (17.8% in 2015) [43], Bangladesh (23.8 in 2011) [44], Yemen (25.1% in 2013), and Chad (31.0% in 2015) [45]. The SBA coverage also placed the country among the bottom five counties with services utilisation. These findings are also lower than study findings from an analysis of DHS data in Sub-Saharan African countries, where 54.5% of pregnant women had four or more antenatal care visits, and a study from lower-middle-income Southeast Asian countries, where 76.6% of pregnant women had four or more antenatal care visits [25]. As antenatal care is the natural entry point for subsequent maternal and neonatal care services, strategies should be designed to accelerate the uptake of ANC services.
Findings from this analysis showed that 93.8% of Ethiopian women had the chance to interact with the health system at least for one of the six services. However, these opportunities do not seem to be adequately utilized to ensure the provision of comprehensive services. This highlights a significant gap in the effective use of available healthcare interactions to deliver a continuum of care, suggesting that future efforts should focus on maximising these interactions to provide comprehensive maternal and neonatal healthcare.
Ethiopia also had the lowest rate of neonatal postnatal care, with 0.3% in 2011 and 12.0% in 2016. These figures are lower than those reported in Kenya (35.6% in 2014) [46] and Rwanda (19.2% in 2015) [47], respectively.
In our study, none of the newborn-mother pairs in the 2011 survey used the entire continuum of care services (6 services). A very small number of newborn-mother pairs received the full range of continuum of care services. This is slow progress that would make meeting the ambitious targets of the Ethiopian Health Sector Transformation Plan difficult (HSTP-II). The HSTP-II aimed to reduce maternal mortality to 279 per 100,000 live births by 2025, as well as under-5 and neonatal mortality to 44 and 21 per 1,000 live births, respectively [5].
Less than a tenth of mother-newborn pairs completed the basic CoC services (four or more ANC visits, SBA, and postnatal care). This is lower than what was found in Sierra Leone, where 17.9% of mothers use these three CoC services in 2019 [48]. This is also lower than the coverage in sub-Saharan countries where 25% of the mothers completed at least three CoC services (ANC4+, SBA and PNC) [25], and a study from lower-middle-income countries in Southeast Asia where 43.4%of mother-newborn pairs used at least three CoC services [49]. This disparity demonstrates how far Ethiopian CoC coverage lags behind the average in these two comparable regions. One of the contributing factors to the lower rate of service utilisation could be the lack of compassionate and respectful maternity care throughout pregnancy and birth. Findings showed that disrespect, neglect, lack of supportiveness and abuse during facility delivery in Ethiopia are not uncommon [50].
We also found that Ethiopia has one of the lowest rates of BCG vaccination and tetanus toxoid protection at birth. In terms of BCG uptake, Ethiopia ranked second least among the DHS-surveyed countries [51]. Tetanus toxoid protection at birth was 48.3% in 2011 and 49.0% in 2016, far lower than countries in the region such as Tanzania (88.0%), Malawi (90.2%), and Burundi (84.3%) [52,53,54]. Because tetanus is a serious disease, it has received national and international policy attention. The World Health Assembly endorsed the global initiative to eliminate maternal and neonatal tetanus by 2020, targeting South Asian and sub-Saharan countries, including Ethiopia [55]. However, Ethiopia’s vaccine coverage does not appear to be on track to meet the targets any time soon. No progress has been made in the five years between 2011 and 2016.
Promising progress in the CoC services in Ethiopia was seen in the initiation of breastfeeding within an hour of birth. Ethiopia placed third next to Burundi and Malawi, with encouraging progress from 51.7% in 2011 to 73.0% in 2016.
We have also investigated the spatial patterns of the continuum of care (CoC) use for maternal and neonatal health services and the relationship between the continuum of care use and women’s empowerment. There was a positive spatial relationship between CoC service use and domains of women’s empowerment. The presence of positive spatial relationship means the higher the women empowerment domain the better the CoC services use. Women’s empowerment has been found to correlate with the use of CoC services in most parts of the country. This is because women’s ability to decide on their behalf and take steps to use health services can be influenced by their household autonomy. When women have greater control over financial resources, mobility, and health-related decisions, they are more likely to seek and receive necessary maternal and neonatal health services. Furthermore, empowered women are more likely to advocate for the health needs of their children, ensuring timely immunizations and check-ups [56]. Study findings from Pakistan [57] and Bangladesh [58] supported these findings showing the positive impact of women’s empowerment towards maternal health services use. This implies that women’s empowerment must be prioritised in maternal and neonatal health strategies. The health-care system should encourage spouses accompany during antenatal, delivery, and postnatal care. Health professionals, particularly health extension workers who are in close contact with the majority of the rural community, should support women’s empowerment initiatives such as awareness raising, open family discussions and assist in maternal health planning and execution.
The continuum of care (CoC) concept for maternal and neonatal health has been regarded as a key principle and framework to support policies and initiatives to save women’s and newborns’ lives and promote overall health [59]. As the co-coverage index as a measurement of CoC considers the delivery of a group of maternal and neonatal care services, it can help to understand the overall patterns of summary measures and locate population groups lagging behind. Spatial analysis of the CoC use could help policymakers assess which parts of the country are benefiting from current services, how these services are clustered within a given setting and identify subnational areas that are not being reached [15]. The continuity of maternal and child health intervention packages is receiving increased attention as a strategy to improve overall service delivery and maternal and neonatal health outcomes [60].
Strength and limitations
This study explored the use of continuum of care services as measured by the co-coverage index using a rigorous spatial analyses technique. The results are based on a nationally representative survey. However, the study has some limitations. As the analysis was based on secondary data the limitations that are pertinent of the DHS survey such as recall bias and social desirability bias could affect the findings. The displacement of GPS coordinates for privacy reasons can potentially have an impact on hot spot and cold spot estimation to some extent. However, we have mitigated potential misinterpretations by focusing on larger area-level interpretations. While BCG is typically administered at birth, it can also be given within the first month. To avoid a significant reduction in our sample size, we included all babies aged 2 to 28 days. This may lead to an underestimation of BCG vaccination levels. Data for contextual factors that can affect health service access such as health facility type-to-population ratios, health worker type-to-population ratios, paved roads per square kilometres and other health infrastructures are not available in the DHS survey, and therefore, we were not able to consider in the analysis.
Conclusions
Our analysis showed that the use of four or more ANC visits, SBS, newborn postnatal care, BCG vaccine uptake, and tetanus toxoid protection at birth were very low in Ethiopia. Particularly, the Amhara, Afar, and Somali regions consistently exhibited lower levels of continuity of care services. The situation in the Amhara region is expected to deteriorate further due to the ongoing civil war, which is severely disrupting health service activities. Women’s empowerment domains were found to have a positive spatial correlation with CoC services use. To improve the current state of maternal and neonatal health, efforts should be directed towards increasing the use of CoC services. To increase the use of maternal and neonatal health services, it is critical to maximise healthcare contacts and guarantee continuity of care across the entire continuum. Women’s empowerment needs to be consistently prioritised in government policies via education, political and economic participation. Raising public awareness about maternity services is essential by using the influence of health professionals, local associations, and mass media.
Data availability
The data that support the findings of this study are available from the DHS Program database accessed from https://dhsprogram.com/Data/.
Abbreviations
- BCG:
-
Bacillus Calmette-Guérin
- CCI:
-
Composite Coverage Index
- CoC:
-
Continuum of Care
- CoCI:
-
Co-coverage Index
- DTP:
-
Diphtheria–Tetanus–Pertussis
- EDHS:
-
Ethiopian Demographic and Health Surveys
- HSTP:
-
Health Sector Development Plan
- MMR:
-
Maternal Mortality Ratio
- PNC:
-
Postnatal Care
- SBA:
-
Skilled Birth Attendance
- SBA:
-
Skilled Birth Attendant
- SDGs:
-
Sustainable Development Goals
- SWPER:
-
Survey-based Women’s Empowerment
References
Lawn JE, Blencowe H, Kinney MV, Bianchi F, Graham WJ. Evidence to inform the future for maternal and newborn health. Best Pract Res Clin Obstet Gynecol. 2016;36:169–83.
Kassebaum NJ, Barber RM, Bhutta ZA, Dandona L, Gething PW, Hay SI, Kinfu Y, Larson HJ, Liang X, Lim SS. Global, regional, and national levels of maternal mortality, 1990–2015: a systematic analysis for the global burden of Disease Study 2015. Lancet. 2016;388(10053):1775–812.
Tarekegn SM, Lieberman LS, Giedraitis V. Determinants of maternal health service utilization in Ethiopia: analysis of the 2011 Ethiopian demographic and Health Survey. BMC Pregnancy Childbirth. 2014;14:1–13.
Tiruneh GT, Demissie M, Worku A, Berhane Y. Predictors of maternal and newborn health service utilization across the continuum of care in Ethiopia: a multilevel analysis. PLoS ONE. 2022;17(2):e0264612.
Ministry of Health Ethiopia. Health sector transformation plan (HSTP-II) 2020/21-2024/25. In.: Federal Ministry of Health Addis Ababa, Ethiopia; 2020.
Gebremedhin AF, Dawson A, Hayen A. Determinants of continuum of care for maternal, newborn, and child health services in Ethiopia: analysis of the modified composite coverage index using a quantile regression approach. PLoS ONE. 2023;18(1):e0280629.
Muluneh AG, Kassa GM, Alemayehu GA, Merid MW. High dropout rate from maternity continuum of care after antenatal care booking and its associated factors among reproductive age women in Ethiopia, evidence from demographic and Health Survey 2016. PLoS ONE. 2020;15(6):e0234741.
Kibret GD, Demant D, Hayen A. Geographical accessibility of emergency neonatal care services in Ethiopia: analysis using the 2016 Ethiopian emergency obstetric and neonatal care survey. BMJ open. 2022;12(6):e058648.
Tarekegn SM, Lieberman LS, Giedraitis V. Determinants of maternal health service utilization in Ethiopia: analysis of the 2011 Ethiopian demographic and Health Survey. BMC Pregnancy Childbirth. 2014;14(1):161.
World Health Organization. The World Health Report 2005-make every mother and child count. In. Geneva. Swizerland: WHO; 2005.
Yeji F, Shibanuma A, Oduro A, Debpuur C, Kikuchi K, Owusu-Agei S, Gyapong M, Okawa S, Ansah E, Asare GQ, et al. Continuum of Care in a maternal, Newborn and Child Health Program in Ghana: low completion rate and multiple obstacle factors. PLoS ONE. 2015;10(12):e0142849–0142849.
Kikuchi K, Ansah EK, Okawa S, Enuameh Y, Yasuoka J, Nanishi K, Shibanuma A, Gyapong M, Owusu-Agyei S, Oduro AR. Effective linkages of continuum of care for improving neonatal, perinatal, and maternal mortality: a systematic review and meta-analysis. PLoS ONE. 2015;10(9):e0139288.
Mohan D, LeFevre AE, George A, Mpembeni R, Bazant E, Rusibamayila N, Killewo J, Winch PJ, Baqui AH. Analysis of dropout across the continuum of maternal health care in Tanzania: findings from a cross-sectional household survey. Health Policy Plann. 2017;32(6):791–9.
Wehrmeister FC, Restrepo-Mendez M-C, Franca GVA, Victora CG, Barros AJD. Summary indices for monitoring universal coverage in maternal and child health care. Bull World Health Organ. 2016;94(12):903.
Victora CG, Fenn B, Bryce J, Kirkwood BR. Co-coverage of preventive interventions and implications for child-survival strategies: evidence from national surveys. Lancet. 2005;366(9495):1460–6.
Alenoghena I, Isah E, Isara A. Maternal health services uptake and its determinants in public primary health care facilities in edo state, Nigeria. Niger Postgrd Med J. 2015;22(1):25–31.
Kishor S, Gupta K. Gender equality and women′ s empowerment in India. National Family Health Survey (NFHS-3) India, 2005-06. In. Mumbai. India: International Institute of Population Sciences; 2009.
Ahmed S, Creanga AA, Gillespie DG, Tsui AO. Economic status, education and empowerment: implications for maternal health service utilization in developing countries. PLoS ONE. 2010;5(6):e11190.
Alsop R, Heinsohn N. Measuring empowerment in practice: structuring analysis and framing indicators. Volume 3510. World Bank; 2012.
Ewerling F, Raj A, Victora CG, Hellwig F, Coll CVN, Barros AJD. SWPER Global: A survey-based women’s empowerment index expanded from Africa to all low-and middle-income countries. J Global Health 2020, 10(2).
Kawaguchi L, Fouad NAM, Chiang C, Elshair IHH, Abdou NM, El Banna SR, Aoyama A. Dimensions of women’s empowerment and their influence on the utilization of maternal health services in an Egyptian village: a multivariate analysis. Nagoya J Med Sci. 2014;76(1–2):161.
Yadav AK, Sahni B, Jena PK. Education, employment, economic status and empowerment: implications for maternal health care services utilization in India. J Public Affairs. 2021;21(3):e2259.
Ahuru RR. The influence of women empowerment on maternal and childcare use in Nigeria. Int J Healthc Manag. 2021;14(3):690–9.
Sado L, Spaho A, Hotchkiss DR. The influence of women’s empowerment on maternal health care utilization: evidence from Albania. Soc Sci Med. 2014;114:169–77.
Alem AZ, Shitu K, Alamneh TS. Coverage and factors associated with completion of continuum of care for maternal health in sub-saharan Africa: a multicountry analysis. BMC Pregnancy Childbirth. 2022;22(1):1–12.
Kamel Boulos MN, Resch B, Crowley DN, Breslin JG, Sohn G, Burtner R, Pike WA, Jezierski E, Chuang K-YS. Crowdsourcing, citizen sensing and sensor web technologies for public and environmental health surveillance and crisis management: trends, OGC standards and application examples. Int J Health Geogr. 2011;10:1–29.
Cromley EK, McLafferty S. GIS and public health. Guilford Press; 2012.
Central Statistical Agency (CSA). [Ethiopia]: Summary and statistical report of the 2007 population and housing census: population size by age and sex. In. Addis Ababa, Ethiopia; 2008.
Central Statistical Agency (CSA) [Ethiopia] and ICF. Ethiopia Demographic and Health Survey 2012. In. Addis Ababa, Ethiopia, and Rockville. Maryland, USA: CSA and ICF; 2012.
Central Statistical Agency (CSA) [Ethiopia] and ICF. Ethiopia Demographic and Health Survey 2016. In. Addis Ababa, Ethiopia, and Rockville. Maryland, USA: CSA and ICF; 2017.
Iqbal S, Maqsood S, Zakar R, Zakar MZ, Fischer F. Continuum of care in maternal, newborn and child health in Pakistan: analysis of trends and determinants from 2006 to 2012. BMC Health Serv Res. 2017;17(1):189.
Wang W, Hong R. Levels and determinants of continuum of care for maternal and newborn health in Cambodia-evidence from a population-based survey. BMC Pregnancy Childbirth. 2015;15:62–62.
Ewerling F, Lynch JW, Victora CG, van Eerdewijk A, Tyszler M, Barros AJD. The SWPER index for women’s empowerment in Africa: development and validation of an index based on survey data. Lancet Global Health. 2017;5(9):e916–23.
Moran PAP. The interpretation of statistical maps. J Royal Stat Soc Ser B (Methodological). 1948;10(2):243–51.
Tillé Y, Dickson MM, Espa G, Giuliani D. Measuring the spatial balance of a sample: a new measure based on Moran’s I index. Spat Stat. 2018;23:182–92.
Parra-Amaya ME, Puerta-Yepes ME, Lizarralde-Bejarano DP, Arboleda-Sánchez S. Early detection for dengue using local indicator of spatial association (LISA) analysis. Diseases. 2016;4(2):16.
Fischer MM, Getis A. Handbook of applied spatial analysis: software tools, methods and applications. Springer Science & Business Media; 2009.
Wu Y, Hung M-C. Comparison of spatial interpolation techniques using visualization and quantitative assessment. Appl Spat Stat 2016:17–34.
Krivoruchko K. Empirical bayesian kriging. ArcUser Fall. 2012;6(10):1145.
Fotheringham AS, Brunsdon C, Charlton M. Geographically weighted regression: the analysis of spatially varying relationships. Wiley; 2003.
Charlton M, Fotheringham S, Brunsdon C. Geographically weighted regression. White Paper Natl Centre Geocomputation Natl Univ Irel Maynooth 2009, 2.
Ministry of Health Ethiopia. Health Sector Transformation Plan (HSTP-I). In. Addis Ababa. Ethiopia: Federal Ministry of Health (FMOH); 2015.
National Institute of Population Research Training. ICF International: Afganistan Demographic and Health Survey 2015. 2015.
National Institute of Population Research Training, ICF International. Bangladesh Demographic and Health Survey 2011. In. Dhaka, Bangladesh: NIPORT, Mitra and Associates, and ICF International; 2013.
National Institute of Population Research Training, ICF International. Chad Demographic and Health Survey 2014–2015. In.; 2016.
Kenya National Bureau of Statistics, Ministry of Health Kenya, National Aids Control Council Kenya, Kenya Medical Research Institute. National Council for Population Development: Kenya Demographic and Health Survey 2014. In. Rockville, MD, USA; 2015.
National Institute of Statistics. Rwanda Ministry of Finance, I. C. F. International: Rwanda Demographic and Health Survey 2014-15. In. Kigali, Rwanda; 2016.
Sserwanja Q, Mutisya LM, Nuwabaine L, Kamara K, Mutebi RK, Musaba MW. Continuum of maternal and newborn health in Sierra Leone: a 2019 national survey. Archives Public Health. 2022;80(1):1–12.
Andriani H, Rahmawati ND, Fauzia S, Kosasih RI. Population-based study on the maternal-newborn-child Health Continuum of Care: evidence from Lower-Middle-Income Countries in Southeast Asia. Asia Pac J Public Health. 2022;34(5):10105395221088615.
Wassihun B, Zeleke S. Compassionate and respectful maternity care during facility based child birth and women’s intent to use maternity service in Bahir Dar, Ethiopia. BMC Pregnancy Childbirth. 2018;18(1):1–9.
The DHS. Program STATcompiler.
Ministry of Health CDGE, Children - Mo HTM, Ministry of Health - Mo HZ, National Bureau of Statistics NBST, Office of Chief Government Statistician OZ., Icf: Tanzania Demographic and Health Survey and Malaria Indicator Survey 2015–2016. In. Dar es Salaam, Tanzania: MoHCDGEC, MoH, NBS, OCGS, and ICF; 2016.
Minstry of health Burundi, Icf: Burundi Troisième Enquête Démographique et de Santé 2016–2017. In, Bujumbura. Burundi; 2017.
National Statistical Office Malawi, Icf. Malawi Demographic and Health Survey 2015-16. In. Zomba, Malawi; 2017.
World Health Organization. Protecting all against tetanus: guide to sustaining maternal and neonatal tetanus elimination (MNTE) and broadening tetanus protection for all populations. 2019.
Vizheh M, Rapport F, Braithwaite J, Zurynski Y. The impact of women’s agency on accessing and using maternal healthcare services: a systematic review and meta-analysis. Int J Environ Res Public Health. 2023;20(5):3966.
Mallick L. Trends and the relationship between maternal health and empowerment in Pakistan, 2012–2018. DHS Program, ICF; 2020.
Rahman R, Rahman M, Haque SE. Empowerment dimensions and their relationship with continuum care for maternal health in Bangladesh. Sci Rep. 2021;11(1):18760.
Kerber KJ, de Graft-Johnson JE, Bhutta ZA, Okong P, Starrs A, Lawn JE. Continuum of care for maternal, newborn, and child health: from slogan to service delivery. Lancet. 2007;370(9595):1358–69.
Darmstadt GL, Bhutta ZA, Cousens S, Adam T, Walker N, De Bernis L, Team LNSS. Evidence-based, cost-effective interventions: how many newborn babies can we save? Lancet. 2005;365(9463):977–88.
Acknowledgements
The authors would like to thank the DHS program for providing the datasets for this analysis. The authors are also express gratitude to the University of Technology Sydney and the Australian government. This research is supported by an Australian Government Research Training Program Scholarship.
Funding
This research did not receive any specific grant from public, commercial, or not-for-profit funding agencies.
Author information
Authors and Affiliations
Contributions
GDK, AH and DD conceptualised the study idea and devised a study design and analysis approach. GD carried out data analysis and interpretation and drafted the manuscript. AH, AD and DD critically reviewed the manuscript for its intellectual content. All authors read and approved the manuscript for submission.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was granted by the University of Technology Sydney Human Research Ethics Committee (Approval number: ETH19-4488). Approval to access and use the DHS dataset was obtained from the Demographic and Health Surveys Program. Informed consent was waived by the University of Technology Sydney Human Research Ethics Committee, because the analysis used secondary data, and there was no contact with study participants and informed consent was not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Kibret, G.D., Demant, D., Dawson, A. et al. Spatial patterns of maternal and neonatal continuum of care use and its correlations with women’s empowerment. BMC Health Serv Res 24, 1018 (2024). https://doi.org/10.1186/s12913-024-11453-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-024-11453-7