Abstract
Background
Digital health technologies (DHT) have become an integral component of modern healthcare systems, offering the potential to improve healthcare delivery and outcomes. Guided by the Technology-Organization-Environment (TOE) framework, this study examines the impact of DHT adoption on healthcare workers' performance and workload in public and private hospitals in Mogadishu, Somalia.
Method
A stratified random sampling approach was used to collect data from 286 healthcare workers in public and private hospitals. Data were analyzed using Structural Equation Modeling (SEM) to test hypotheses and assess direct and mediating relationships among variables.
Results
The analysis revealed that DHT significantly improves healthcare workers' performance and workload respectively (β = 0.452, C.R. = 10.150, p < 0.001) and (β = 0.594, C.R. = 9.972, p < 0.001), organizational and environmental factors are positively impacting on healthcare workers' performance (β = 0.327, C.R. = 8.709, p < 0.001) and (β = 0.102, C.R. = 2.872, p = 0.004). Healthcare workers’ performance significantly reduces workload (β = 0.594, C.R. = 9.972, p < 0.001) and the mediating role of healthcare workers’ performance between DHT and workload were also confirmed (β = 0.281, C.R. = 5.9787, p < 0.001).
Conclusion
The findings underscore the critical role of DHT in enhancing healthcare workers' performance and reducing workload, with the TOE framework and performance acting as significant mediators. These results provide actionable insights for healthcare administrators and policymakers to optimize DHT implementation, support workforce efficiency, and address workload challenges through strategic organizational and environmental adaptations.
Similar content being viewed by others
Introduction
Digital health technologies (DHTs) have emerged as essential tools in modern healthcare, transforming the delivery, management, and accessibility of health services. These technologies includes electronic health records (EHRs), telemedicine platforms and health information systems addresses critical challenges in healthcare systems by improving operational efficiency by enabling data-driven decision-making and enhancing communication among stakeholders [1]– [4]. The growing demand for healthcare services, particularly in resource-constrained settings, highlights the importance of adopting DHTs to bridge gaps in infrastructure, workforce, and service delivery [5, 6]. The value of DHT adoption lies in its potential to optimize healthcare workers' performance by reducing manual workflow, enhancing task efficiency, and fostering better patient engagement [7, 8]. In a low resource setting where health workers can be overstretched to the level of burnout, this technology could safe staff time, reduce stress and improve performance as well as service delivery [9]. Adopting these technologies requires organizational structure, operational readiness, leadership commitment, availability of resources, external environmental pressures such as regulatory frameworks and market dynamics.
The Diffusion of Innovation (DOI) Theory [10] explains how innovations are adopted over time within an organization or society. It provides insights into how digital health technologies (DHT) are perceived and accepted by healthcare workers, especially in terms of perceived advantages, compatibility, and complexity. DHT adoption directly impacts healthcare workers' performance by improving efficiency, communication, and patient outcomes [11, 12]. Conversely, the adoption of these technologies may also introduce new challenges, such as increased cognitive load, technological anxiety, and user resistance, which could offset their benefits [9]. While DHTs show promise in supporting health workforce development, particularly in low- and middle-income countries, more evidence is needed regarding their effectiveness at scale, including return on investment and the role of government policies [13]. Moreover, the Technological-Organizational-Environmental (TOE) framework provides a robust theoretical foundation for understanding the complexities of DHT adoption. The technological dimension emphasizes ease of use, perceived usefulness, and technological capability, while the organizational dimension focuses on internal readiness, leadership, and resource allocation. The environmental dimension encompasses external influences such as government policies, societal demands, and competitive pressures [14, 15]. Together, these dimensions influence the degree to which DHTs can be successfully implemented and their subsequent impact on healthcare workers’ performance and workload.
While previous studies have explored DHT adoption, several critical gaps remain. These gaps primarily revolve around implementation challenges, the impact on healthcare workers' competencies, and the need for structured frameworks to facilitate DHT integration into healthcare systems [13, 16,17,18]. First, most research had focused on the application of the TOE framework in business or e-commerce settings, with limited exploration in healthcare, particularly in resource-constrained environments [19, 20]. Second, the impact of DHT adoption on healthcare workers’ performance and workload remains underexplored [9]. Finally, there is a lack of research on the mediating role of healthcare workers’ performance in balancing workload and technology adoption [21], While it is known that DHTs can alleviate administrative burdens, there is insufficient evidence on whether this translates into better patient care or introduces new complexities, such as over-reliance on technology or increased training requirements [18].
This study aims to fill knowledge gaps and make several contributions to the literature the full impact of digital health technology adoption on healthcare workers' performance, particularly in low-resource settings. Moreover, the research would provide further insight to DOI and TOE frameworks by demonstrating how DHT contributes towards healthcare workers’ performance that led to reduced workload. The study integrates TOE framework, DOI theory, DHT, healthcare workers’ performance and workload. We seek empirical evidence to support theoretical models and constructs in contexts beyond developed countries. Thus, the research questions are set out: (1) How organizational and environmental factors influence DHT adoption. (2) How DHT adoption affects healthcare workers’ performance and workload. (3) how does healthcare workers’ performance mediate the relationship between DHT adoption and workload.
Theoretical background and hypotheses
Diffusion of innovations theory
The Diffusion of Innovation (DOI) theory, created by social scientist E.M. Rogers in 1962, describes how an idea or behavior spreads through a specific population or society over time. This process ultimately leads to the adoption of new ideas or behaviors by the public within a social system [10]. The Diffusion of Innovation (DOI) theory explains how new ideas or technologies spread through a population over time [22]. Relative advantage, such as improved patient care and operational efficiency, significantly influences the adoption of digital health technologies. For instance, clinicians are more likely to adopt innovations that demonstrate clear benefits over existing practices [23]. The adoption of e-health technologies can be predicted using DOI dimensions such as relative advantage, compatibility, and complexity [24]. Users are more likely to adopt technologies that they believe offers significant benefits over existing solutions [25]. A foundational understanding of technology is essential for professionals advocating digital health tools, as it influences their ability to promote these innovations effectively [26]. However, we consider how digital health technology adoption impacts healthcare workers’ performance.
Digital health technologies adoption and healthcare worker’s performance
The adoption of digital health technologies (DHTs) involves integrating these tools into healthcare systems to streamline operations, improve diagnostic capabilities and ensure equitable access to healthcare services. Key factors influencing the DHT adoption include technological readiness, infrastructure, and system development capabilities [27, 28] . For instance, the integration of electronic medical records (EMR) had been accelerated by advancements in system interoperability and institutional support. Telemedicine enables remote consultations, reducing the need for physical visits, which had proven to be critical during the COVID-19 pandemic [4, 29]. Mobile health applications empower users to track health behaviors and access medical information, promoting preventive care and self-management [30]. Wearable devices provide real-time health monitoring, fostering proactive patient engagement [31]. Additionally, DHTs facilitate health worker training, improve supervision, and enhance communication among healthcare teams [13]. DHT adoption has been particularly impactful in addressing geographical barriers, ensuring healthcare access for individuals in remote and underserved areas. During the COVID-19 pandemic, teleconsultations, e-diagnosis, and surveillance systems demonstrated the transformative potential of DHTs in primary healthcare [29]. Automation in medical documentation and information exchange further streamlines processes, reducing administrative burdens and improving institutional efficiency [32].
Ultimately, the adoption of digital health technologies aligns with efforts to modernize healthcare systems and enhance performance by integrating these technologies, healthcare institutions can foster better communication, operational efficiency, and improved patient outcomes. The success of DHT adoption depends on addressing challenges related to technological readiness, staff training, and infrastructure development to maximize its potential impact [27, 28]. Technological factors such as ease of use, system integration, and reliability influence healthcare workers' ability to adopt and effectively utilize DHTs [27]. However, the research posits that DHT adoption enhances healthcare workers’ performance.
Technology-Organization-Environment (TOE) framework
In a hospital setting, the adoption and implementation of technological innovations are influenced by three main contexts: technological, organizational, and environmental, as outlined by Depietro et al.( 1990). The technological context encompasses both internal and external technologies that are relevant to hospitals. This includes the medical equipment and healthcare processes. The organizational context involves the hospital's characteristics and resources, such as size, degree of centralization and formalization, management structure, human resources, available surplus resources, and interconnections among staff members. The environmental context includes factors such as the size and structure of the healthcare industry, the hospital's competitors, broader economic environment, and regulatory conditions.
These three contexts provide both limitations and opportunities for technological innovation in hospitals. They shape how hospitals identify, search, and ultimately adopt new technologies [15]. The adoption of digital health technology significantly affects healthcare workers’ performance, as evidenced by various studies. The Technology-Organization-Environment (TOE) framework plays a crucial role in determining the readiness and success of big data adoption in healthcare organizations [33]. Digital healthcare enhances communication between healthcare providers and patients at the intersection of technology and healthcare, leading to improved performance and efficiency among healthcare workers [8]. Furthermore, organizational characteristics moderate the relationship between information technology integration and the performance of public hospitals by emphasizing the need for customized technologies to fit organizational characteristics for optimal performance [34]. Furthermore, the TOE framework was extended to explore digital marketing adoption in start-ups, demonstrating its impact on organizational performance. While the TOE model provides a structured approach to understanding technology adoption, it is essential to consider that individual perceptions and resistance to change can significantly impact the effectiveness of digital health technology implementation in healthcare settings. Thus, in the line with the context of research on digital health technology adoption, we consider the variables organizational factor, environmental factor and technology factor.
Organizational factor and healthcare workers’ performance
Organizational policies and infrastructure, such as funding, processes and training can significantly affect the adoption of digital technologies [27]. Management and external support are key predictors of mHealth adoption [35], while government policies and organizational readiness are fundamental for AI adoption in healthcare [36]. Organizational learning capacity mediates the relationship between innovative technology and healthcare performance, emphasizing the need for continuous learning and adaptation within healthcare organizations [11]. A strong organizational culture positively impacts healthcare professionals' performance by fostering discipline and teamwork. Studies show that understanding cultural dynamics within healthcare settings can lead to improved patient care outcomes [37]. Adequate facilities and infrastructure are essential for motivating healthcare workers and enhancing their job performance [38]. Organizational factors significantly influence healthcare workers' performance and patient outcomes. Work climate has been shown to positively affect organizational citizenship behavior and negatively impact counterproductive work behavior in rural health settings [39]. Organizational factors, such as training, leadership support, and size of the hospital, further enable healthcare workers to leverage these technologies for improved performance [8]. The study, included perceived training, size of the hospitals, top management support, and resource availability. Therefore, the present research proposes that Organizational factor has a positive impact healthcare workers’ performance.
Environmental factor and healthcare workers’ performance
Regulatory and environmental pressures, including governmental mandates, shape the decisions to adopt healthcare technologies [28]. The TOE framework has also been applied to assess big data adoption readiness in healthcare organizations, revealing that technological, organizational, and environmental factors contribute significantly to adoption [33]. Individual and environmental factors, such as effort, abilities, physical conditions, and training, affect healthcare workers' performance [40]. The study found that the layout of technical equipment positively correlates with the performance of Community Health Workers in health houses, while the layout of office equipment negatively affects performance. Optimizing the physical work environment is crucial for enhancing healthcare service delivery [41].Environmental factors include such as policy support and patient demand for digital solutions, create external pressures that drive DHT adoption [31]. The study included patient demand, pressure from other hospitals. Hence, the current study posits that environmental factor impact the healthcare workers’ performance.
Healthcare workers’ performance and workload
A study found a direct correlation between nurse workload and performance, suggesting that high workloads negatively affect the quality of care provided [42] . Significant negative influence of workload on healthcare worker performance was established, emphasizing the need for balanced task distribution [43]. Research at Bhakti Husada Hospital revealed that 58.6% of nurses experienced heavy workloads, correlating with high stress levels (63.8%) among them [44]. The integration of digital health technologies (DHTs) into healthcare systems has significant implications for the performance and workload of health workers. While DHTs promise to enhance efficiency and communication, their implementation often coincides with increased workload and stress among health professionals. Digital health technologies (DHTs) have shown positive impacts on healthcare worker performance and workload reduction. Studies indicate that DHTs enhance healthcare providers' efficiency [45], and healthcare professionals have reported that DHTs reduce workload, ensure continuity of care, and facilitate faster and more accurate decision making [46]. Healthcare worker performance refers to their ability to deliver quality care efficiently and effectively, often measured by patient outcomes, adherence to protocols, and productivity. Workload refers to the volume of tasks and responsibilities assigned to healthcare workers. However, with presence of DHT, healthcare workers’ performance has significantly impact of workload.
Mediating role of healthcare workers’ performance
Successful integration of digital health technologies can alleviate some administrative burdens, allowing healthcare workers to focus more on patient care [47]. A supportive work environment and adequate facilities can mitigate the negative impacts of workload, enhancing overall performance even in the presence of DHT [48]. Research suggests that digital health technologies (DHT) can reduce workload and improve care continuity for healthcare workers [46]. Despite potential benefits, the introduction of digital health technologies can initially increase workloads due to the need for training and adaptation. High rates of work-related stress among healthcare workers indicate that without proper support, digital tools may exacerbate existing workload issues [49]. The relationship between DHT, workload, and performance is complex. Poor infrastructure can negate DHT benefits, causing delays and frustrations [46]. A study found a significant relationship between workload and employee performance, indicating that higher workloads correlate with lower performance levels [50]. Psychological factors such as stress, anxiety, and depression also mediate this relationship, exacerbating burnout and further diminishing performance [51]. Increased workload has been shown to negatively influence healthcare workers' performance, with studies indicating a significant correlation (P = 0.000) between high workload and decreased performance levels [43].Effective mediation, such as training and support systems, is crucial for maximizing the benefits of digital health technologies while minimizing workload [45]. Accordingly, the research proposes that healthcare workers’ performance play a mediating role in the relationship between DHT and workload.
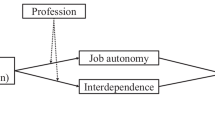
Based on the above discussions the study proposed the following hypotheses. See Fig. 1
-
H1. Digital health technology adoption positively impacts healthcare workers’ performance.
-
H2. Digital health technology adoption has a significant impact on healthcare worker’s workload.
-
H3. Environmental factor has a positive impact healthcare workers’ performance.
-
H4. Organizational factor has a positive impact healthcare workers’ performance.
-
H5. Healthcare workers’ performance has a significant impact on healthcare workers’ performance.
-
H6. Healthcare workers’ performance mediates the relationship between digital health technology adoption and workload.
Methodology
Research design
The study employed a quantitative research design, utilizing a cross-sectional survey to examine the impact of digital health technologies (DHT) adoption on healthcare workers’ performance and workload. The study integrated Diffusion Innovation Theory (DOI), Technology-Organization-Environment (TOE) framework, to explore the mediating relationships between digital health technology adoption and workload.
Population and sample technique
The target population comprised healthcare workers employed in both public and private hospitals in Mogadishu, Somalia. The study included a diverse range of healthcare roles, including doctors, nurses, IT personnel, public health officers, and administrative staff, to capture a holistic view of the impact of DHT. Stratification reduces the potential for bias by ensuring proportional representation from all strata [52]. Moreover, stratification also provides meaningful comparisons can be made between groups (e.g., doctors vs. nurses, public vs. private hospitals) to assess variations in the impact of digital health technologies. Hence, stratified random sampling technique was employed to ensure representation across different healthcare roles and hospital types (public and private). This approach allowed for the collection of balanced and reliable data. G*Power was used to determine the minimum sample size. For a margin error of 0.05, statistical power of 0.95, effect size of 0.15, and three predictors, the minimum sample size was calculated to be 119 responses. As plot shows in Fig. 2.
In addition, descriptive statistics of 286 respondents reported in result section, structural equation modeling utilized to test the mediating role of healthcare workers’ performance, in particular, AMOS – SPSS employed in the data analysis.
Data collection
Data was collected through a self-administered survey questionnaires and distributed to the selected healthcare workers using Kobo Toolbox, the collected data was exported to MS Excel. The questionnaire included items measuring constructs related to digital health technologies, healthcare workers’ performance, workload, DOI and the TOE framework. The instrument was pre-tested to ensure reliability and validity, with adjustments made to optimize clarity and relevance. Ethical approval and informed consent were obtained before data collection. Moreover, respondents were assured of anonymity and confidentiality to encourage honest and unbiased responses.
Measurement development
The variables assessed—healthcare workers' performance, healthcare workers' workload, digital health technologies, and the organization factor, environment factor in a part (TOE) framework—were measured using scales sourced from prior studies with appropriate modifications to fit the healthcare context. The 5-point Likert Scale was employed to measure each item (1 = strongly disagree, 5 = strongly agree). Table 1 displays the number of measurement items along with their corresponding sources.
Data analysis method
The data was analyzed using the Statistical Package for Social Science (SPSS) and the Analysis of Moment Structures (AMOS). Structural Equation Modeling (SEM) was employed as the analytical approach, as it is particularly suitable for testing complex relationships between multiple variables and evaluating mediation effects. The analysis was conducted in three main stages:
-
1.
Common method bias and inspecting the inner structural model: This step involved to check the potential bias of the study.
-
2.
Measurement Model Validation: This step involved assessing the reliability, convergent validity, and discriminant validity of the constructs to ensure the measurement model accurately reflected the latent variables.
-
3.
Structural Model Testing: Hypothesized relationships between variables were examined through path analysis. Mediation effects were also tested to understand the indirect relationships among variables.
-
4.
Goodness-of-Fit Indices: The model's fit to the data was evaluated using several fit indices, including the Goodness of Fit Index (GFI), Adjusted Goodness of Fit Index (AGFI), Incremental Fit Index (IFI), Normed Fit Index (NFI), Comparative Fit Index (CFI), Tucker-Lewis Index (TLI), and Root Mean Square Error of Approximation (RMSEA).
Data analysis and results
Demographic profile
Table 2 describes the demographic profile of the respondents in the study on digital health technology adoption in Mogadishu hospitals revealed that the majority were male (54.9%) and aged between 36 and 40 years (35.3%). Most participants were full-time employees (55.9%) with 6–10 years of working experience (67.8%), and doctors constituted the largest professional group (76.2%). The prevalent income range was $501–$1000 (55.9%), and the most commonly used digital health technology was electronic health records (63.3%).
Common method bias
Harman's single-factor test, were conducted to detect and address common method variance in the dataset. Harman’s Single Factor test was executed to identify the potential threat of CMB [62]. The results indicated that a single component explained only 42.95% of the total variation. Since this figure is below 50%, it suggests that CMB is not a concern in this study.
Inspecting the inner structural model
The collinearity statistics for the independent variables were assessed using Tolerance and Variance Inflation Factor (VIF) to identify potential multicollinearity concerns. The results indicate that all variables have Tolerance values above 0.1 and VIF values below 5, suggesting an acceptable level of collinearity within the model [63]. Digital health technology (Tolerance = 0.491, VIF = 2.037), healthcare workers’ performance (Tolerance = 0.384, VIF = 2.603), technology factor (Tolerance = 0.399, VIF = 2.508), and environment factor (Tolerance = 0.442, VIF = 2.261) demonstrate no significant multicollinearity concerns. The organization factor exhibits the lowest Tolerance value (0.294) and the highest VIF (3.406) among the predictors; however, these values remain within acceptable limits, indicating moderate but non-critical multicollinearity. Table 3 presented the result.
Measurement model
The measurement model demonstrated strong reliability and validity for the constructs used in this study. Indicators with factor loadings below 0.60 were excluded [64]. As Table 3 shows the range of factor loadings between 0.646 and 0.813. Therefore, all items are above 0.6. Squared multiple correlations are in the range between 0.417 and 0.661. All squared multiple correlations (R-squared) should be a minimum of 0.40 [65]. Furthermore, in structure equation model, the reliability of data most exceed 0.7 [66] indicating strong indicator reliability. Composite reliability (CR) values for all constructs exceeded the threshold of 0.7, ranging from 0.728 to 0.895. Convergent validity is supported, with AVE values above or close to the recommended threshold of 0.5, which suggests a need for further refinement [67]. Discriminant validity was established, as the square root of AVE for each construct exceeded the inter-construct correlations, and the Maximum Shared Variance (MaxR[H]) values confirmed distinctiveness among constructs (see Tables 4 and 5). Furthermore, to assess the discriminant validity of the constructs, the Heterotrait-Monotrait (HTMT) Ratio procedure was employed. According to [68], discriminant validity is established when the HTMT values are less than or equal to 0.90. Values exceeding this threshold suggest a lack of discriminant validity between constructs. The study, all HTMT values are below the 0.90 threshold, confirming that discriminant validity is achieved. The HTMT values for the constructs are presented in the Table 6.
Reliability and validity
Structure model
The structural model allows researchers to test specific hypotheses about the strength and significance of relationships (path coefficients) between variables. H1 revealed a significant positive relationship between DHT adoption and healthcare workers’ performance (β = 0.473, C.R = 12.879, p < 0.001). These findings align with previous research, which highlights that digital health tools, such as electronic health records and telemedicine systems, enhance operational efficiency, improve decision-making, and reduce errors among healthcare workers [8, 11, 69]. The effective integration of DHT enables healthcare professionals to access real-time data, facilitating better patient care. H2 A strong positive association was found between digital health technology (DHT) and workload reduction among healthcare workers (β = 0.241, C.R. = 4.767, p < 0.001). Although DHT can enhance productivity, these technologies may also increase the demand for new skills and continuous learning, thereby contributing to reduce workload for healthcare workers. This is consistent with the work of [70], who noted that while DHT reduces administrative burdens, it often necessitates adaptation and training, which can momentarily increase workload. H3, Organizational factors within the TOE framework significantly influenced healthcare workers’ performance (β = 0.327, C.R = 8.709, p < 0.001). This finding highlights the importance of supportive leadership, clear policies, and adequate resources for technology adoption. The results corroborate studies by [71], which emphasize that organizational readiness and culture play a pivotal role in leveraging DHT for performance improvement. H4 Environmental factors also positively affected healthcare workers’ performance (β = 0.102, C.R = 2.872, p = 0.004). External pressures, such as regulatory policies and patient expectations, encourage healthcare institutions to adopt advanced technologies, indirectly benefiting workers' performance. This aligns with findings [72], which indicate that environmental drivers push organizations to modernize their systems. H5, the study found a significant positive relationship between healthcare workers' performance and workload (β = 0.594, C.R = 9.972, p < 0.001). While improved performance may lead to better outcomes, it can also result in increased responsibilities, as noted by [73, 74]. This highlights the dual-edged nature of performance improvements, where gains in efficiency may be accompanied by higher expectations and responsibilities.
The results indicate that integrating the DHT can directly improve the quality and effectiveness of healthcare services. H2 examined the relationship between DHT and the TOE framework and demonstrated a strong positive impact (β = 0.525, C.R. = 11.853, p < 0.001). This finding highlights the role of the TOE framework as a critical mediator for successful DHT adoption, which has been supported by studies that emphasize the importance of technological, organizational, and environmental factors in driving adoption [60]. H3 explored the influence of the TOE framework on healthcare workers' performance, which was also positive and significant (β = 0.461, C.R. = 9.448, p < 0.001). This suggests that the TOE framework facilitates the effective implementation of DHT, enhancing performance by addressing organizational readiness and external pressures [75]. H4 assessed the relationship between healthcare workers' performance and workload reduction, showing a strong positive effect (β = 0.765, C.R. = 17.511, p < 0.001). This finding is consistent with the notion that improved performance driven by efficient digital systems can alleviate workload by automating routine tasks and streamlining operations [76]. suggested that improved performance might lead to a reduced workload for healthcare workers. The results are presented in Table 7andFig. 3.
Mediation analysis
The mediating analysis revealed that healthcare workers' performance partial mediates the relationship between DHT and workload (Indirect Effect β = 0.281, C.R = 5.978, p < 0.001). This suggests that while digital health technology (DHT) directly impacts workload, its influence is also channeled through improved performance and partial mediated. These findings align with studies that emphasize the indirect pathways through which technology adoption affects operational dynamics in healthcare settings [77]. This highlights the importance of the digital health technology adoption in maximizing the healthcare workers’ performance, suggesting that a supportive organizational and environmental context is essential for achieving optimal outcomes. It highlights the dual benefits of DHT in improving efficiency and reducing strain on healthcare workers, particularly in high-pressure environments. The result is presented in Table 8 and summary of the hypotheses presented in Table 9.
Model fit index
The model fit results indicate that the proposed structural equation model (SEM) provides a good fit to the data. The Chi-Square statistic (χ2 = 920.641, p < 0.000) suggests that the model does not fit the data perfectly; however, this statistic is sensitive to sample size. The degrees of freedom (DF = 480) reflect the model's complexity, while the Relative Chi-Square (χ2/DF = 1.918) indicates a good fit, as values below 3 are considered acceptable [78, 79]. The Goodness-of-Fit Index (GFI = 0.838) and the Adjusted Goodness-of-Fit Index (AGFI = 0.811) fall slightly below the recommended threshold of 0.9. However, the Comparative Fit Index (CFI = 0.914) and Tucker-Lewis Index (TLI = 0.906) both exceed the threshold of 0.9, indicating good model fit relative to a null model. The Root Mean Square Error of Approximation (RMSEA = 0.057) is well below the threshold of 0.08, confirming a satisfactory fit while accounting for model complexity. Overall, the indices suggest that while the model may have minor limitations, it provides a reasonably good representation of the data. The results are presented in Fig. 4.
Discussion
The findings of this study provide valuable insights into the impact of digital health technologies (DHT) on healthcare workers' performance and workload in public and private hospitals in Mogadishu, Somalia. The results indicated a significant positive relationship between the adoption of DHT and healthcare workers' performance. Digital health systems such as electronic medical records, telemedicine platforms, and automated workflows enhance healthcare delivery by reducing administrative burdens, improving accuracy, and facilitating better communication. This finding aligns with previous research demonstrating that the implementation of DHT can enhance efficiency, accuracy, and decision making in healthcare settings [80,81,82] from the perspective of Diffusion of Innovation (DOI) theory [10], these technologies represent innovations that diffuse within healthcare institutions, with adoption largely influenced by perceived relative advantage, compatibility with existing workflows, and ease of use. The study findings support the DOI premise that successful adoption depends on how well innovations address users' needs and concerns, emphasizing the importance of proper training and awareness in encouraging uptake among healthcare professionals.
Organizational factors play a critical role in facilitating the adoption and effectiveness of DHT. As [60] explain in the Technology Organization Environment (TOE) framework, organizational readiness—comprising leadership, infrastructure, and training—significantly influences the success of technological implementation. This study builds on that premise, emphasizing that without sufficient organizational support, even the most advanced technologies may fail to achieve their desired impact. Similarly [83] assert that investments in change management and continuous staff training are critical for ensuring that healthcare workers fully leverage the potential of DHT. In the context of DOI theory, the adoption of DHT within healthcare organizations depends on key factors such as organizational innovativeness and leadership support which influence how quickly and effectively innovations are adopted. The study highlighted for healthcare organizations to focus not only on adopting advanced technologies but also on ensuring the readiness of their organizational structures and the external environment to support these technologies. These results are consistent with prior studies, such as those by [84], which emphasize that the interplay between technology, organizational policies, and environmental factors significantly enhances the effectiveness of technological adoption.
Environmental factors, such as regulatory policies, societal expectations, and resource availability, also emerge as influential drivers in this study. These factors, often outside the control of individual organizations, create the broader context within which healthcare institutions operate. Previous studies, such as those by [85], highlight the importance of government incentives and collaborations with non-governmental organizations in fostering technology adoption in resource-limited settings. This underscores the need for systemic reforms and strategic partnerships to create an enabling environment for DHT implementation.
The study found that digital health technology (DHT) has a significant positive impact on reducing healthcare workers’ workload. This aligns with existing literature that highlights how DHT can streamline administrative tasks, automate routine processes, and enhance efficiency in patient care delivery. For instance [86], emphasized that digital health tools, such as electronic health records (EHRs) and automated scheduling systems, reduce the time spent on documentation and coordination, allowing healthcare workers to focus more on direct patient care. By digitizing processes that were previously manual, DHT alleviates the administrative burden and improves task allocation, ultimately reducing workload. However, it is important to note that while DHT reduces workload in many aspects, improper implementation or lack of user training can lead to the opposite effect.
The study also reveals a positive association between healthcare worker’s performance and workload. This indicates that as healthcare workers perform more effectively, they are better equipped to manage their workload, leading to enhanced efficiency and productivity. Improved performance likely results in better time management, optimized use of resources, and reduced errors, thereby alleviating the pressures of a heavy workload. These findings align with previous studies that highlight how enhanced individual performance can positively influence organizational workload management [36, 46]. Consequently, improving healthcare workers' performance not only benefits individual efficiency but also contributes to overall organizational effectiveness in managing workforce challenges.
Furthermore, the study found the mediating role of the healthcare worker’s performance in the relationship between DHT and healthcare worker’s workload. This result suggests the critical role that improved performance plays in translating the benefits of DHT into tangible workload reductions. When DHT optimizes healthcare workers’ performance—such as through better task efficiency, enhanced decision-making, and improved accuracy—it indirectly alleviates their workload by reducing the time and effort required to accomplish tasks. Previous studies had consistently highlighted this mediating role. For example, [87] found that digital tools like decision-support systems and electronic health records enable workers to make quicker and more informed decisions, leading to enhanced performance outcomes. In turn, this increased efficiency minimizes redundancy and delays in task execution, thereby reducing the overall workload [88, 89]. When healthcare workers find DHT intuitive and valuable, their performance improves, making it easier to handle workloads.
Implications for research
Theoretically, the study contributes significantly to the body of knowledge on digital health technology (DHT) adoption by integrating healthcare workers’ performance and workload within the framework of the Diffusion Innovation Theory (DOI) and Technology-Organization-Environment (TOE) model. First, the research validates the DOI and TOE framework as a robust theoretical foundation for examining the interplay between digital technology adoption, organizational factors, and performance outcomes in healthcare. The findings reinforce the critical role of organizational and environmental factors in facilitating DHT adoption and optimizing its impact on healthcare worker performance.
Second, the study extends the existing literature by emphasizing the mediating role of healthcare workers’ performance in linking DHT to workload reduction. Third, it provides the understanding of how organizational and environmental factors interact with technological adoption to influence workforce outcomes. These findings validate and extend the applicability of the DOI and TOE framework in healthcare settings, demonstrating its relevance in linking technology adoption to performance improvements. From a practical perspective, the findings of this study offer valuable insights for healthcare organizations, policymakers, and technology developers hence organizations should focus on implementing user-friendly digital health technologies (DHT) that enhance healthcare workers’ performance, as improved performance directly contributes to workload reduction. Policymakers need to establish supportive environments for DHT adoption by providing adequate training, fostering leadership support, and ensuring the availability of resources to encourage effective use of technology. Training programs should emphasize improving the digital literacy and confidence of healthcare workers, especially in resource-constrained settings. Furthermore, organizations should align DHT with workforce capacity by adopting technologies that automate routine tasks, streamline administrative processes, and improve task efficiency to alleviate healthcare workers’ workload while maintaining high-quality care. In resource-limited environments like Mogadishu, Somalia, targeted investments in cost-effective and scalable DHT can deliver significant benefits if challenges related to organizational and environmental factors are adequately addressed. Finally, strengthening leadership, resource allocation, workplace policies, government regulations, infrastructure, and cultural acceptance is critical to ensuring the successful adoption and long-term sustainability of DHT in healthcare systems.
Conclusion
The study investigated the impact of digital health technologies (DHT) on healthcare workers' performance and workload through the lens of the DOI and Technology-Organization-Environment (TOE) model, and mediating effect healthcare workers’ performance in the relationship between digital health technologies (DHT) and healthcare workers’ workload. The findings revealed that DHT significantly enhances healthcare workers' performance and reduces their workload, highlighting the transformative potential of these technologies in healthcare settings. Furthermore, the study highlights the importance of integrating DHT with supportive organizational structures, robust technological infrastructure, and a conducive external environment to maximize their impact. Moreover, the mediating role of healthcare workers' performance in the relationship between DHT and workload demonstrates the importance of focusing on strategies that improve worker efficiency and productivity. These insights have both theoretical and practical implications, contributing to the body of knowledge on DHT adoption and providing actionable recommendations for healthcare organizations and policymakers to address workload challenges in resource-constrained settings. This research contributes to the growing body of knowledge on digital health and organizational frameworks, providing practical implications for policymakers and healthcare administrators to enhance worker performance and reduce workload through strategic DHT adoption.
Limitations and future research direction
This study has several limitations that should be acknowledged. First, the data was collected from healthcare workers in public and private hospitals within a specific geographical region. This may limit the generalizability of the findings. Future research should consider expanding the study to include healthcare workers from diverse geographical locations and healthcare systems. A broader sample would provide a more comprehensive understanding of digital health technology (DHT) adoption and its impact across different settings. Second, while this study offers valuable insights from a low-resource setting, cross-contextual research is needed to explore regional and cultural variations in DHT adoption. Conducting comparative studies across different socioeconomic and healthcare environments could provide a more nuanced understanding of how DHT adoption influences healthcare worker performance and workload. Third, the study utilized a quantitative research approach, which provides an initial understanding of the relationships between DHT adoption, performance, and workload. However, incorporating qualitative data in future research could offer deeper insights into the underlying mechanisms driving these relationships. Longitudinal studies could also be beneficial in capturing the long-term effects of DHT adoption on healthcare worker performance and workload. Additionally, the study is subject to potential biases, such as social desirability bias, where healthcare workers might overstate or understate their experiences related to workload and technology use. Future research could mitigate this bias by employing alternative data collection methods, such as third-party evaluations, observational studies, or triangulation with qualitative data. Finally, this study primarily focused on the role of DHT adoption within the Digital Health Adoption (DHA), DOI and Technology-Organization-Environment (TOE) framework. Future research may explore additional mediating or moderating factors, such as individual competencies, institutional policies, organizational culture, leadership styles, employee characteristics, or socioeconomic influences. Examining these factors could provide a more comprehensive understanding of the relationships between DHT adoption, the Diffusion of Innovation (DOI) theory, the TOE framework, healthcare worker performance, and workload.
Data availability
The datasets and materials used in this study are openly available and can be accessed through Figshare https://doi.org/10.6084/m9.figshare.28377662.
Abbreviations
- AI:
-
Artificial intelligence
- DHT:
-
Digital Health Technology
- TOE:
-
Technology-Organization-Environment
- DOI:
-
Diffusion of Innovation
- HWP:
-
Health Worker Performance
- HWW:
-
Health Worker Workload
- ORGF:
-
Organizational Factor
- ENVF:
-
Environmental Factor
- SPSS AMOS:
-
Statistical Package for Social Science (SPSS) and the Analysis of Moment Structures (AMOS)
- SEM:
-
Structural Equation Modeling
- GFI:
-
Goodness of Fit Index
- AGFI:
-
Adjusted Goodness of Fit Index
- IFI:
-
Incremental Fit Index
- NFI:
-
Normed Fit Index
- CFI:
-
Comparative Fit Index
- TLI:
-
Tucker-Lewis Index
- RMSEA:
-
Root Mean Square Error of Approximation
- CMB:
-
Common Method Bias
- VIF:
-
Variance Inflation Factor
- CR:
-
Composite Reliability
- AVE:
-
Average Variance Extracted
- C.R:
-
Critical Ratio
References
Negash YT, Calahorrano Sarmiento LE. Smart product-service systems in the healthcare industry: Intelligent connected products and stakeholder communication drive digital health service adoption. Heliyon. 2023;9(2):e13137. https://doi.org/10.1016/j.heliyon.2023.e13137.
Mulukuntla S, Pamulaparthyvenkata S. “Digital Transformation in Healthcare: Evaluating the Impact of Telemedicine and Health Information Systems on Patient Care”, EPH - Int. J Med Heal Sci. 2020;6(03):27–33.
Colombo F, Oderkirk J, Slawomirski L. Health Information Systems, Electronic Medical Records, and Big Data in Global Healthcare: Progress and Challenges in OECD Countries. In: Haring R, Kickbusch I, Ganten D, Moeti M, editors. Handbook of Global Health. Cham: Springer International Publishing; 2020. p. 1–31.
Pawar DK, Gujarathi S, Gupta R, Khan A, Tiwari A. A Detail Review on Digital Health Technologies. Int J Res Appl Sci Eng Technol. 2024;12(2):621–30. https://doi.org/10.22214/ijraset.2024.58371.
Holl F, Kircher J, Hertelendy AJ, Sukums F, Swoboda W. “Tanzania’s and Germany’s Digital Health Strategies and Their Consistency With the World Health Organization’s Global Strategy on Digital Health 2020–2025: Comparative Policy Analysis”. J Med Internet Res. 2024;26(1). https://doi.org/10.2196/52150.
Alunyu AE, Amiyo MR, Nabukenya J. Contextualised digital health communication infrastructure standards for resource-constrained settings: Perception of digital health stakeholders regarding suitability for Uganda’s health system. PLOS Digit Heal. 2024;3(9):1–21. https://doi.org/10.1371/journal.pdig.0000603.
Agarwal R, Gao GG, DesRoches C, Jha AK. The digital transformation of healthcare: Current status and the road ahead. Inf Syst Res. 2010;21(4):796–809. https://doi.org/10.1287/isre.1100.0327.
Anusi IH, Mutambara E. “Digital Technology and Health Workers’ Performance: A Case of Hospitals in Nigeria and South Africa”. Int J Soc Sci Relig. 2022;355–380. https://doi.org/10.53639/ijssr.v3i3.118.
Edo OC, Ang D, Etu EE, Tenebe I, Edo S, Diekola OA. Why do healthcare workers adopt digital health technologies - A cross-sectional study integrating the TAM and UTAUT model in a developing economy. Int J Inf Manag Data Insights. 2023;3(2): 100186. https://doi.org/10.1016/j.jjimei.2023.100186.
Rogers EM. Diffusion of Innovations, Fifth edit. New York: Free Press; 2003.
Abdulla Alzaabi HOE, Hasan H, Akmal S. “Mediation Model of Digital Technology Factors Affecting Health Care Service Performance” Int J Sustain Constr Eng Technol. 2022;13(4):104–120, 2022. https://doi.org/10.30880/ijscet.2022.13.04.009.
Leonard KL, Masatu MC, Vialou A. Getting doctors to do their best: The roles of ability and motivation in health care quality. J Hum Resour. 2007;42(3):682–700. https://doi.org/10.3368/jhr.xlii.3.682.
Long LA, Pariyo G, Kallander K. Digital technologies for health workforce development in low- and middle-income countries: A scoping review. Glob Heal Sci Pract. 2018;6(Supplement 1):S41–8. https://doi.org/10.9745/GHSP-D-18-00167.
Awa HO, Ojiabo OU, Orokor LE. Integrated technology-organization-environment (T-O-E) taxonomies for technology adoption. J Enterp Inf Manag. 2017;30(6):893–921. https://doi.org/10.1108/JEIM-03-2016-0079.
Depietro R, Wiarda E, Fleischer M.“The context for change: Organization, technology and environment”. Processes Technol Innov. 1990:151–175.
Borges do Nascimento IJ et al. “Barriers and facilitators to utilizing digital health technologies by healthcare professionals,” npj Digit. Med. 2023;6(1)1–28 https://doi.org/10.1038/s41746-023-00899-4.
Hovenga E, Hovenga H. “Addressing workforce knowledge gaps in digital health,” in Roadmap to Successful Digital Health Ecosystems: A Global Perspective, E. Hovenga and H. B. T.-R. to S. D. H. E. Grain, Eds. Academic Press, 2022:537–554.
Jarvis K, Thetford C, Turck E, Ogley K, Stockley RC. “Understanding the Barriers and Facilitators of Digital Health Technology (DHT) Implementation in Neurological Rehabilitation: An Integrative Systematic Review”. Heal Serv Insights. 2024;17 https://doi.org/10.1177/11786329241229917.
MT, TM Q Nguyen, “Balancing Security and Privacy in the Digital Age: An In-Depth Analysis of Legal and Regulatory Frameworks Impacting Cybersecurity Practices.,” Int J Intell Autom Comput. 2023;6(5):1–12. Available: https://research.tensorgate.org/index.php/IJIAC/article/view/61.
Yeh CH, Lee GG, Pai JC. Using a technology-organization-environment framework to investigate the factors influencing e-business information technology capabilities. Inf Dev. 2015;31(5):435–50. https://doi.org/10.1177/0266666913516027.
Ferava F, Anindita R, Hilmy MR. The Motivation as A Mediation Relationship of Work Load Performance in Medical Record Staff at X Hospital. J Multidiscip Acad. 2021;5(2):137–42.
SBNSA. Singh, “Designing culturally acceptable screening for breast cancer through artificial intelligence-two case studies” J Fam Med Prim Care. 2019.
Novikov Z, Singer SJ, Milstein A. Innovation Diffusion Across 13 Specialties and Associated Clinician Characteristics. Adv Health Care Manag. 2024;22:97–115. https://doi.org/10.1108/S1474-823120240000022005.
Putteeraj M, Bhungee N, Somanah J, Moty N. Assessing E-Health adoption readiness using diffusion of innovation theory and the role mediated by each adopter’s category in a Mauritian context. Int Health. 2022;14(3):236–49. https://doi.org/10.1093/inthealth/ihab035.
Shaikh IM, Amin H. Influence of innovation diffusion factors on non-users’ adoption of digital banking services in the banking 4.0 era. Inf Discov Deliv. 2025;53(1):12–21. https://doi.org/10.1108/IDD-05-2023-0044.
Shi J. Bridging the Digital Divide in Mental Health: An Innovation Diffusion-Based Framework for Advancing Digital Literacy among Professionals. Lect Notes Educ Psychol Public Media. 2024;38(1):53–65. https://doi.org/10.54254/2753-7048/38/20240587.
Anthony Jnr B. “Examining the adoption of telehealth during public health emergencies based on technology organization environment framework,” J. Sci. Technol. Policy Manag. 2023. https://doi.org/10.1108/JSTPM-05-2022-0079.
Wolverton CC, Lanier PA. “Utilizing the Technology-Organization-Environment Framework to Examine the Adoption Decision in a Healthcare Context”. 2018;401–423. https://doi.org/10.4018/978-1-5225-7214-5.ch018.
Ndayishimiye C, Lopes H, Middleton J. A systematic scoping review of digital health technologies during COVID-19: a new normal in primary health care delivery. Health Technol (Berl). 2023;13(2):273–84. https://doi.org/10.1007/s12553-023-00725-7.
Marent B Henwood F. “Digital health”. Encycl Heal Res Soc Sci. 2023;88–93 https://doi.org/10.1097/naq.0000000000000371.
Paul PK, Moumtzoglou A, Bandyopadhyay A, Hoque M, Kumar NS, Saavedra R. Indian Digital Health Information Systems: Initiatives and Opportunities with Socio-economic Perspective. Econ Aff (New Delhi). 2024;69(2):1175–89. https://doi.org/10.46852/0424-2513.3.2024.39.
Shokirovich AS. “Opportunities of Digital Technologies in The Healthcare System”. Int J Innov Res Multidiscip Educ. 2024;3(6). https://doi.org/10.58806/ijirme.2024.v3i6n14.
EAA Ghaleb, Dominic PDD, Fati SM, Muneer A, Ali RF. “The assessment of big data adoption readiness with a technology–organization–environment framework: A perspective towards healthcare employees,” Sustain. 2021;13(15). https://doi.org/10.3390/su13158379.
Malongo IK, Muathe S, Waithaka ST. The Moderating Effect of Organizational Characteristics on The Relationship Between Information Technology Integration and Performance: Empirical Evidence from Selected Public Hospitals in Kenya. Int J Manag Inf Technol. 2019;14:3359–67.
Bin Naeem S, Azam M, Kamel Boulos MN, Bhatti R. Leveraging the TOE Framework: Examining the Potential of Mobile Health (mHealth) to Mitigate Health Inequalities. Inf. 2024;15(4):1–17. https://doi.org/10.3390/info15040176.
Yang J, Luo B, Zhao C, Zhang H. “Artificial intelligence healthcare service resources adoption by medical institutions based on TOE framework”. Digit Heal. 2022;8(193) https://doi.org/10.1177/20552076221126034.
Almutairi RL, et al. Analysis of organizational culture factors that influence the performance of health care professionals: A literature review. J Public Health Africa. 2022;13(s2):74–8. https://doi.org/10.4081/jphia.2022.2415.
Suriyanti S, Azlan SN. Tangible and Intangible Factors Affecting the Organizational Performance of Remote Health Workers. J Minds Manaj Ide dan Inspirasi. 2023;10(1):85–100. https://doi.org/10.24252/minds.v10i1.33690.
Jayasuriya R, Jayasinghe UW, Wang Q. Health worker performance in rural health organizations in low- and middle-income countries: Do organizational factors predict non-task performance? Soc Sci Med. 2014;113:1–4. https://doi.org/10.1016/j.socscimed.2014.04.042.
Ida Ayu Laksmi Arnita Utari and Dety Mulyanti. Faktor-Faktor Yang Mempengaruhi Kinerja Tenaga Kesehatan Di Rumah Sakit: Tinjauan Teoritis. J Kesehat Amanah. 2023;7(1):51–60. https://doi.org/10.57214/jka.v7i1.264.
Yusefzadeh H, Nabilou B. Work environment factors and provider performance in health houses: a case study of a developing country. BMC Res Notes. 2020;13(1):4–9. https://doi.org/10.1186/s13104-020-05346-1.
Tinta Y, Muhtar A, Risal A. Relationship Between Workload and Nurse Performance in the Inpatient Ward of Nene Mallomo Hospital. J Community Heal Provis. 2024;4(3):151–7.
Ratioktavia Kusumawardani D, Wahyu Lelly Hana Setyanti S, Mirzania A. “the Influence of Workload, Motivation and Work Environment on the Performance of Employees”. Spectr J Soc Sci. 2024;1(2)61–66. https://doi.org/10.61552/sjss.2024.02.003.
Mutianingsih M, Putri NL, Iskandar M, Putri FF. “The Relationship of Workload with Nurses ’ job stress at Bhakti Husada Hospital Cikarang”. J Educ Innov Public Heal. 2024;2(3).
Borges do Nascimento IJ. The global effect of digital health technologies on health workers’ competencies and health workplace: an umbrella review of systematic reviews and lexical-based and sentence-based meta-analysis. Lancet Digit Heal. 2023;5(8):e534–44. https://doi.org/10.1016/S2589-7500(23)00092-4.
Mensah NK et al. “Perceived impact of digital health technology on health professionals and their work: A qualitative study in Southern Ghana”. Digit Heal. 2023;9. https://doi.org/10.1177/20552076231218838.
Lahtiranta J. Mediator – enabler for successful digital health care. Finnish J eHealth eWelfare. 2017;9(4):284–98. https://doi.org/10.23996/fjhw.60923.
Duan SX, Deng H, Wibowo S. Exploring the impact of digital work on work–life balance and job performance: a technology affordance perspective. Inf Technol People. 2023;36(5):2009–29. https://doi.org/10.1108/ITP-01-2021-0013.
Kremer L, Lipprandt M, Röhrig R, Breil B.“Examining Mental Workload Relating to Digital Heal Technologies in Health Care: Systematic Review”. J Med Internet Res. 2022;24. https://doi.org/10.2196/40946.
Dwi B, Rahmawati Z, Mudayana AA. The Relationship between Workload and Work Discipline with Employee Performance at Nyi Ageng Serang Kulon Progo Hospital. Int J Healthc Res. 2022;5(2):32–42.
Sun J, Sarfraz M, Ivascu L, Iqbal K, Mansoor A. “How Did Work-Related Depression, Anxiety, and Stress Hamper Healthcare Employee Performance during COVID-19? The Mediating Role of Job Burnout and Mental Health”. Int J Environ Res Public Health. 2022;19(16). https://doi.org/10.3390/ijerph191610359.
Tipton E, Hedges L, Vaden-Kiernan M, Borman G, Sullivan K, Caverly S. Sample Selection in Randomized Experiments: A New Method Using Propensity Score Stratified Sampling. J Res Educ Eff. 2014;7(1):114–35. https://doi.org/10.1080/19345747.2013.831154.
Nikou S, Agahari W, Keijzer-Broers W, de Reuver M. Digital healthcare technology adoption by elderly people: A capability approach model. Telemat Informatics. 2020;53:101315. https://doi.org/10.1016/j.tele.2019.101315.
Yoon J, et al. Development and Validation of Digital Health Technology Literacy Assessment Questionnaire. J Med Syst. 2022;46(2):1–11. https://doi.org/10.1007/s10916-022-01800-8.
Nguyen PH, Kim SS, Tran LM, Menon P, Frongillo EA. Intervention Design Elements Are Associated with Frontline Health Workers’ Performance to Deliver Infant and Young Child Nutrition Services in Bangladesh and Vietnam. Curr Dev Nutr. 2019;3(8):nzz070. https://doi.org/10.1093/cdn/nzz070.
Epstein A, et al. Does health worker performance affect clients’ health behaviors? A multilevel analysis from Bangladesh. BMC Health Serv Res. 2019;219(1):1–9. https://doi.org/10.1186/s12913-019-4205-z.
Leiter MP, Maslach C. Areas of Worklife: a Structured Approach To Organizational Predictors of Job Burnout. Res Occup Stress Well Being. 2003;3(03):91–134. https://doi.org/10.1016/S1479-3555(03)03003-8.
Portoghese I, Galletta M, Coppola RC, Finco G, Campagna M. Burnout and workload among health care workers: The moderating role of job control. Saf Health Work. 2014;5(3):152–7. https://doi.org/10.1016/j.shaw.2014.05.004.
Michael CM, Leiter P. “Preventing burnout and building engagement : a complete program for organizational renewal”. 2000.
Tornatzky LG, Fleischer M. The Uncertainties of Technological Innovation. 1990;273(3).
De Campos MCT, Marziale MHP, Santos JLF. Cross-cultural adaptation and validation of the world health organization health and work performance questionnaire to brazilian nurses. Rev da Esc Enferm. 2013;47(6):1338–44. https://doi.org/10.1590/S0080-623420130000600013.
Ooi K-B, Lee V-H, Tan GW-H, Hew T-S, Hew J-J. Cloud computing in manufacturing: The next industrial revolution in Malaysia? Expert Syst Appl. 2018;93:376–94. https://doi.org/10.1016/j.eswa.2017.10.009.
Kim JH. Multicollinearity and misleading statistical results. Korean J Anesthesiol. 2019;72(6):558–69. https://doi.org/10.4097/kja.19087.
Gefen D, Straub D. “A Practical Guide To Factorial Validity Using PLS-Graph: Tutorial And Annotated Example”. Commun Assoc Inf Syst. 2005;16. https://doi.org/10.17705/1cais.01605.
Bollen KA. A New Incremental Fit Index for General Structural Equation Models. Sociol Methods Res. 1989. https://doi.org/10.1177/0049124189017003004.
Hair JF, Sarstedt M, Ringle CM, Mena JA. An assessment of the use of partial least squares structural equation modeling in marketing research. J Acad Mark Sci. 2012;40(3):414–33. https://doi.org/10.1007/s11747-011-0261-6.
Fornell C, Larcker DF. Evaluating Structural Equation Models with Unobservable Variables and Measurement Error. J Mark Res. 1981;18(1):39. https://doi.org/10.2307/3151312.
Henseler J, Ringle CM, Sarstedt M. A new criterion for assessing discriminant validity in variance-based structural equation modeling. J Acad Mark Sci. 2015;43(1):115–35. https://doi.org/10.1007/s11747-014-0403-8.
Kruse CS, Mileski M, V. Alaytsev, E. Carol, and A. Williams, “Adoption factors associated with electronic health record among longterm care facilities: A systematic review,” BMJ Open 2015;5(1). https://doi.org/10.1136/bmjopen-2014-006615.
Dunn Lopez K. et al. “Electronic health record usability and workload changes over time for provider and nursing staff following transition to new EHR,” Appl Ergon. 2021;93:103359. 2021. https://doi.org/10.1016/j.apergo.2021.103359.
Lundstrom T, Pugliese G, Bartley J, Cox J, Guither C. Organizational and environmental factors that affect worker health and safety and patient outcomes. Am J Infect Control. 2002;30(2):93–106. https://doi.org/10.1067/mic.2002.119820.
Faqih KMS, Jaradat M-IR. Mobile Healthcare Adoption among Patients in a Developing Country Environment: Exploring the Influence of Age and Gender Differences. Int Bus Res. 2015;8(9):142–74. https://doi.org/10.5539/ibr.v8n9p142.
Gardner RL, et al. Physician stress and burnout: the impact of health information technology. J Am Med Informatics Assoc. 2019;26(2):106–14. https://doi.org/10.1093/jamia/ocy145.
Alotaibi YK, Federico F. The impact of health information technology on patient safety. Saudi Med J. 2017;38(12):1173–80. https://doi.org/10.15537/smj.2017.12.20631.
Baker J. “The Technology–Organization–Environment Framework,” Y. K. Dwivedi, M. R. Wade, and S. L. Schneberger, Eds. New York, NY: Springer New York. 2012;231–245.
Kovacs R, Lagarde M. Does high workload reduce the quality of healthcare? Evidence from rural Senegal. J Health Econ. 2022;82:102600. https://doi.org/10.1016/j.jhealeco.2022.102600.
Windle R. “INNOVATION IN professionals ’ adoption and use of”. J Innov Heal Inform. 2018;25(1).
Kline RB. Response to Leslie Hayduk’s review of principles and practice of structural equation modeling,1 4th edition. Can Stud Popul. 2018;45(3–4):188–95. https://doi.org/10.25336/csp29418.
Tabri N, Elliott CM. Principles and Practice of Structural Equation Modeling. 2012;1(1).
Al-Worafi YM. Electronic Patient Records in Developing Countries: Achievements and Challenges. In: Al-Worafi YM, editor. Handbook of Medical and Health Sciences in Developing Countries. Cham: Springer International Publishing; 2024. p. 1–21.
Coorevits P, et al. Electronic health records: New opportunities for clinical research. J Intern Med. 2013;274(6):547–60. https://doi.org/10.1111/joim.12119.
Zhang T, Lu C, Kizildag M. Banking ‘on-the-go’: examining consumers’ adoption of mobile banking services. Int J Qual Serv Sci. 2018;10(3):279–95. https://doi.org/10.1108/IJQSS-07-2017-0067.
Brommeyer M, Liang Z. “A Systematic Approach in Developing Management Workforce Readiness for Digital Health Transformation in Healthcare”. Int J Environ Res Public Health. 2022;19(21). https://doi.org/10.3390/ijerph192113843.
Degroote SE, Marx TG. The impact of IT on supply chain agility and firm performance: An empirical investigation. Int J Inf Manage. 2013;33(6):909–16. https://doi.org/10.1016/j.ijinfomgt.2013.09.001.
Alrahbi D, Khan M, Hussain M. Exploring the motivators of technology adoption in healthcare. Int J Healthc Manag. 2021;14(1):50–63. https://doi.org/10.1080/20479700.2019.1607451.
Alkhwaldi AF. Understanding the acceptance of business intelligence from healthcare professionals’ perspective: an empirical study of healthcare organizations. Int J Organ Anal. 2024;32(9):2135–63. https://doi.org/10.1108/IJOA-10-2023-4063.
Mohammadnejad F, Freeman S, Klassen-Ross T, Hemingway D, Banner D. Impacts of Technology Use on the Workload of Registered Nurses: A Scoping Review. J Rehabil Assist Technol Eng. 2023;10:1–11. https://doi.org/10.1177/20556683231180189.
Alharasis EE, Alkhwaldi AF. “The Implementation of Advanced AIS and the Accounting Data Quality: The Case of Jordanian SMEs,” in Lecture Notes in Computer Science (including subseries Lecture Notes in Artificial Intelligence and Lecture Notes in Bioinformatics). 2024;14721 LNCS:149–173. https://doi.org/10.1007/978-3-031-61318-0_11.
O. M. H. K. An. R. A.-S. J. T. S. A.-A. M. F. Azam, “ANTECEDENTS OF BUSINESS ANALYTICS ADOPTION AND IMPACTS ON BANKS’ PERFORMANCE: THE PERSPECTIVE OF THE TOE FRAMEWORK AND RESOURCE-BASED VIEW,” Interdiscip. J. Information, Knowledge, Manag. 2023;1(2010):150–154.
Acknowledgements
We acknowledge all healthcare workers who participated in this research and those who did not. we appreciate their busy time.
Funding
This study did not receive any financial support.
Author information
Authors and Affiliations
Contributions
Abdulkadir Jeilani Mohamud: Writing – original draft, Project administration, Methodology, Investigation, Data curation, Conceptualization, Formal analysis. Abdinur Hussein Mohamed: Writing – review & editing, Writing – original draft, Supervision, Project administration, Investigation, Data curation, Conceptualization.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study examines “Impact of Digital Health Technologies Adoption on Healthcare Workers' Performance and Workload: Perspective with DOI and TOE Models” Researchers ensured that participants were informed about the study's purpose, procedures, risks, and benefits, could withdraw at any time, and obtained voluntary and informed consent from participants and their legal guardians before their involvement in the research. This study was conducted in accordance with the principles of the Declaration of Helsinki. Ethical approval was received from the Institutional Review Board (MU-IRB) (MUIRB/19/24/001) of Mogadishu University and the ethics committee of the Training and Research Hospital Recep Tayyip Erdogan in Mogadishu, Somalia (date: 07.09.2024, Decision No 1053).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Jeilani, A., Hussein, A. Impact of digital health technologies adoption on healthcare workers’ performance and workload: perspective with DOI and TOE models. BMC Health Serv Res 25, 271 (2025). https://doi.org/10.1186/s12913-025-12414-4
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1186/s12913-025-12414-4