Abstract
Background
Although the “obesity paradox” is comprehensively elucidated in heart failure (HF) with reduced ejection fraction (HFrEF) and HF with preserved ejection fraction (HFpEF), the role of body composition in left ventricular (LV) remodeling, LV reverse remodeling (LVRR), and clinical outcomes is still unclear for HF with mildly reduced ejection fraction (HFmrEF).
Methods
Our study is a single-centre, prospective, and echocardiography-based study. Consecutive HFmrEF patients, defined as HF patients with a left ventricular ejection fraction (LVEF) between 40 and 49%, between January 2016 to December 2021 were included. Echocardiography was re-examined at 3-, 6-, and 12-month follow-up to assess the LVRR dynamically. Body mass index (BMI), fat mass, fat-free mass, percent body fat (PBF), CUN-BAE index, and lean mass index (LMI) were adopted as anthropometric parameters in our study to assess body composition. The primary outcome was LVRR, defined as: (1) a reduction higher than 10% in LV end-diastolic diameter index (LVEDDI), or a LVEDDI < 33 mm/m2, (2) an absolute increase of LVEF higher than 10 points compared with baseline echocardiogram, or a follow-up LVEF ≥50%. The secondary outcome was a composite of re-hospitalization for HF or cardiovascular death.
Results
A total of 240 HFmrEF patients were enrolled in our formal analysis. After 1-year follow-up based on echocardiography, 113 (47.1%) patients developed LVRR. Patients with LVRR had higher fat mass (21.7 kg vs. 19.3 kg, P = 0.034) and PBF (28.7% vs. 26.6%, P = 0.047) compared with those without. The negative correlation between anthropometric parameters and baseline LVEDDI was significant (all P < 0.05). HFmrEF patients with higher BMI, fat mass, PBF, CUN-BAE index, and LMI had more pronounced and persistent increase of LVEF and decline in LV mass index (LVMI). Univariable Cox regression analysis revealed that higher BMI (HR 1.042, 95% CI 1.002–1.083, P = 0.037) and fat mass (HR 1.019, 95% CI 1.002–1.036, P = 0.026) were each significantly associated with higher cumulative incidence of LVRR for HFmrEF patients, while this relationship vanished in the adjusted model. Mediation analysis indicated that the association between BMI and fat mass with LVRR was fully mediated by baseline LV dilation. Furthermore, higher fat mass (aHR 0.957, 95% CI 0.917–0.999, P = 0.049) and PBF (aHR 0.963, 95% CI 0.924–0.976, P = 0.043) was independently associated with lower risk of adverse clinical events.
Conclusions
Body composition played an important role in the LVRR and clinical outcomes for HFmrEF. For HFmrEF patients, BMI and fat mass was positively associated with the cumulative incidence of LVRR, while higher fat mass and PBF predicted lower risk of adverse clinical events but not LMI.
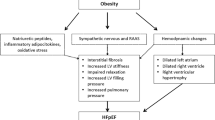
Graphical abstract

Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Heart failure (HF) is a global public health problem caused significant morbidity, considerable mortality, poor quality of life, and heavy health care expenditure [1, 2]. HF is a heterogenous and multi-faced clinical syndrome characterized by systemic congestion, and impaired cardiac structure and function [3, 4]. The pathophysiological hallmark of HF is myocardial remodeling, especially for left ventricle (LV). Pathological LV remodeling (LVR) is characterized by chamber dilation, ventricular wall thinning, or eccentric hypertrophy [5]. The mechanism of LVR is complex. Multiple factors, including mechanical stress, neurohormonal activation, inflammation and metabolic abnormality, participate in this pathological process [6, 7]. Persistent LVR correlates with poor prognosis of HF. Higher mortality and re-hospitalization rate have been observed in patients with more severe LVR [8,9,10]. Myocardial reverse remodeling, especially left ventricular reverse remodeling (LVRR), is an important indicator of the cardiac functional recovery and is associated with survival benefits and improved clinical outcomes for HF patients [11]. LVRR was characterized by restoration of LV geometry, normalization of LV systolic/diastolic function, and reversal of alterations of the cellular and extracellular composition [6, 12]. LVRR is an important therapeutic objective for HF treatment.
While obesity is a well-established risk factor for HF, overweight and obesity was associated with better prognosis and substantially improved survival in HF patients, which is termed as “obesity paradox” [13, 14]. It is still unclear whether the “obesity-survival paradox” in HF is a reliable phenomenon or a consequence of statistically methodological limitation such as reverse causation, mediation effect, confounding effect, or suppression effect. Moreover, the underlying mechanism of “obesity paradox” is still ambiguous. Earlier appearance of symptoms and access to medication, better tolerability of guideline-directed medical therapy (GDMT), higher levels of circulating cardioprotective adipokines, greater anti-inflammatory effects of elevated lipoproteins, greater weight reserves against the cardio-metabolic changes and cardiac cachexia may be the potential reasons for “obesity paradox” [13, 15, 16]. Interestingly, “obesity paradox” was also observed in the relationship between obesity and myocardial remodeling in HF with reduced ejection fraction (HFrEF). Previous study had demonstrated that obesity was an independent predictor for LVRR in patients with HFrEF, which may provide an explanation of the “obesity paradox” for HFrEF patients [17, 18]. Moreover, higher body mass index (BMI) was tightly associated with recovered/improved left ventricular ejection fraction (LVEF), and was an effective predictor for HF with improved ejection fraction (HFimpEF) [19].
However, the reasonability and reliability using body mass index (BMI) as an isolated anthropometric parameter to evaluate “obesity paradox” has been doubted [20]. One plausible explanation of “obesity paradox” is the inaccuracy and limitation of the BMI in characterizing the severity of obesity [21]. The absolute amount of body fat and its location, or its ratio to muscle can’t be accurately reflected by BMI. The other anthropometric indices, including fat mass, percent body fat (PBF), fat-free mass, and lean mass, can characterize the body composition and obesity more comprehensively. Furthermore, although the “obesity paradox” was well described in HFrEF and HF with preserved ejection fraction (HFpEF), clinical research concerning the “obesity paradox” for HFmrEF patients was limited [22, 23]. To data, the impact of body composition on LVRR and long-term prognosis is unclear in patients with HFmrEF. Thus, we conducted this prospective cohort study to explore the role of body composition in LVR, LVRR, and long-term clinical outcomes for patients with HFmrEF.
Methods
Study design and participants
Our study was a single-centre, prospective, echocardiography-based, observational study, which was approved by the Ethics Committee of Qilu Hospital of Shandong University. The study was performed in accordance with the Declaration of Helsinki. A total of 394 consecutive patients diagnosed as HFmrEF at Qilu Hospital cardiology department and managed by an established CHF management system between January 2016 to December 2021 were enrolled in our study. The study protocol and flowchart were shown in Fig. 1.
The inclusion criteria included: (i) Confirmed HFmrEF at screening period, defined as patients with a LVEF between 40% and 49%; (ii) New York Heart Association (NYHA) functional class II to IV; (iii) available echocardiography at baseline and programmed follow-up; (iv) age≥18 years old, (v) retrievable necessary clinical data. The exclusion criteria included: (i) incomplete essential clinical data, (ii) age < 18 years old, (iii) heart transplantation, cardiac resynchronization therapy, or left ventricular assist device implantation status, (iv) malignant diseases, such as neoplasm, and (v) any condition with life expectancy less than 1 year.
At the terminal of our study, 58 patients with incomplete clinical data, 3 patients with age less than 18 years old, and 93 patients with unfinished programed follow-up were excluded. After exclusion, the remaining 240 HFmrEF were enrolled in our final analysis (Fig. 1).
Echocardiography examination
The echocardiographic data was obtained from echocardiographic reports conducted by 2-dimensional and targeted M-mode echocardiography with Doppler color flow mapping. The Phillip EPIQ7C system (Philips Ultrasound, Bothell, WA, USA), UST-52,105 probe (1.0–5.0 MHz), and Hitachi Aloka Prosound F75 system were used for our echocardiographic study. Comprehensive echocardiographic parameters were measured according to the American Society of Echocardiography and European Association of Cardiovascular Imaging recommendation. The LVEF is calculated via biplane modified Simpson’s method in the apical four- and two-chamber view. The left ventricular end-diastolic diameter (LVEDD), interventricular septal end-diastolic thickness (IVSTd), and left ventricular posterior wall end-diastolic thickness (LVPWTd) was measured using parasternal long-axis views. The left atrial diameter (LAD) was measured via apical 4-chamber views at the end of systole. The right ventricular end-diastolic diameter (RVEDD) was measured via the minor-axis in the apical four-chamber view at the end of diastole. The echocardiographic index was calculated as the following formula:
Left ventricular end-diastolic diameter index (LVEDDI, mm/m2) = LVEDD/body surface area (BSA).
Left ventricular mass index (LVMI, g/m2) = 0.80 × 1.04×[(IVSTd + LVEDD + LVPWTd)3– LVEDD3] + 0.6 g/ BSA.
Relative wall thickness (RWT) = 2×[LVPWTd/LVEDD].
BSA was calculated via the Du Bois formula. Left ventricular hypertrophy (LVH) was diagnosed when LVMI above the reference upper limits (95 g/m2 in women and 115 g/m2 in men). Participants with LVH was further categorized as concentric hypertrophy (RWT ≥ 0.43) and eccentric hypertrophy (RWT < 0.43) according to RWT. The mitral valve function was assessed through a semi-qualitative way based on color doppler flow imaging. All Echocardiography was performed by a panel of experienced sonographers and echocardiographic experts.
Body composition assessment
The body composition parameters enrolled in our study included BMI, fat-free mass, fat mass, PBF, the Clínica Universidad de Navarr—Body Adiposity Estimator (CUN-BAE) index, and lean mass index (LMI). The BMI was calculated by the formula: BMI (kg/m2) = body weight (kg)/ the square of the height (m2). According to Working Group on Obesity in China, we defined low weight was defined as low weight/underweight as a BMI less than 18.5 kg/m2, healthy/normal weight as a BMI of 18.5–23.9 kg/m2, overweight as a BMI of 24.0–27.9 kg/m2, and obesity as a BMI ≥ 28.0 kg/m2 [24, 25].
The estimated fat-free mass was calculated according to the Kuch formula: Fat-free mass (kg) = 5.1×(height [m]1.14) ×(weight [kg]0.41) for males, and 5.34×(height [m]1.47) ×(weight [kg]0.33) for females [26]. The Kuch formula, an accurate tool to estimate fat-free mass, was derived from bioelectrical impedance analysis (BIA), and has been applicated in several clinical studies [27, 28]. Fat mass was calculated via the formula: Fat mass (kg) = body weight (kg)– fat-free mass (kg). The PBF was calculated as the ratio of fat mass to total body weight. Furthermore, the CUN-BAE index was also calculated [29, 30]. The CUN-BAE index is a reliable and easy-to-apply tool to estimate PBF, which has been confirmed by large-population studies [31, 32]. The CUN-BAE index was calculated via the formula: CUN-BAE index = -44.988 + (0.503×age) + (10.689×sex) + (3.172×BMI)– (0.026×BMI2) + (0.181×BMI×sex)– (0.020×BMI×age)– (0.005×BMI2×sex) + (0.00021×BMI2×age). The value of sex was codified as 0 for males and 1 for females. The LMI was calculated via the formula: LMI (kg/m2) = (1-BF%) × BMI (kg/m2) [29, 30]. As for no reference value could be recommended for Chinese population, the patients were categorized into three groups according to the gender-specific tertiles of fat-free mass, fat mass, PFB, CUN-BAE index, or LMI. The method to assess and estimate body composition has been widely applicated in previous studies [33, 34]. High consistency between estimated anthropometric parameters and body composition measured by dual-energy X-ray absorptiometry (DEXA) has been validated in previous studies concerning anthropometric measurements, highlighting the validity of the estimated anthropometric indices adopted in our study [26, 35, 36].
Clinical and laboratory data
Comprehensively essential data were prospectively collected by experienced data inspectors. Clinical variates, including (i) demographic data, (ii) physical examination parameters: admission monitored blood pressure, heart rate, NYHA functional class, (iii) cardiovascular complications, (iv) echocardiographic parameters, (v) laboratory data, including hemoglobin, N-terminal B-type natriuretic peptide (NT-proBNP), serum potassium, serum sodium, and the estimated glomerular filtration rate (eGFR), and (vi) medical therapy, including angiotensin-converting enzyme inhibitors (ACEI)/ angiotensin II receptor blockers (ARB)/ angiotensin receptor/neprilysin inhibitors (ARNI), beta-blockers, mineralocorticoid-receptor antagonist (MRA), and sodium-glucose cotransporter-2 inhibitor (SGLT2i), were collected for the analysis of our study. The eGFR was calculated via the Chronic Kidney Disease Epidemiology Collaboration creatinine 2021 (CKD-EPI 2021) equation.
Follow-up protocol and study outcomes
The study scheme was illustrated in Fig. 1. The HF patients enrolled in our study was managed by an established CHF management system as previous described [37]. All patients were managed by a panel of experienced specialist HF cardiologists. The optimal guideline-directed medical therapy was well administrated. All participants would receive the echocardiographic transvaluation at 3-, 6-, and 12- month follow-up to dynamically reassess cardiac function and myocardial reverse remodeling. Patients got LVRR at any follow-up timepoint were all categorized as LVRR group in our final analysis. The protocol for follow-up was ratified by the Institutional Review Board of Qilu Hospital.
The primary outcome of our study was LVRR. The standardized definition of LVRR is still non-uniform. In accordance with previous literature [38,39,40], the composite criteria of LVRR adopted by our study included: (1) a reduction higher than 10% in LVEDDI, or a LVEDDI < 33 mm/m2, (2) an absolute increase of LVEF higher than 10 points compared with baseline echocardiogram, or a follow-up LVEF ≥50%. The change in LVEDDI was calculated as follows: (LVEDDI of baseline echocardiogram– LVEDDI of follow-up echocardiogram)/LVEDDI of baseline echocardiogram ×100%. The secondary outcome of our study was a composite of re-hospitalization for HF or death from cardiovascular causes.
Statistical analysis
The continuous variables were expressed as medians with interquartile ranges (25th–75th percentiles) or mean ± standard deviations, and were compared via Mann-Whitney U test or t-test. The categorical variables were expressed as frequencies and percentages, and were compared through Chi-square test or Fisher’s exact probability tests.
To assess the relationship between body composition and baseline LV remodeling in HFmrEF patients, Pearson’s correlation analysis was conducted. Furthermore, the multivariate linear regression analysis was conducted to eliminate the influence of gender and age. To explore the association between body composition and LVRR or clinical outcomes, Kaplan–Meier curve analysis, log-rank (Mantel-Cox) test, and log-rank test for trend were conducted. To further assess the role of body composition in LVRR and clinical prognosis, univariable and multivariable Cox regression analysis was conducted. The hazard ratio (HR) and 95% confidence intervals (CIs) was calculated. Univariable Cox regression was performed for the crude model, and multivariable Cox-proportional hazard analyses was performed for the adjusted model to eliminate potential confounders. These covariates with statistical significance (P < 0.05) in the crude model would be further adopted in the multivariable analysis. The restricted cubic spline (RCS), using four knots, was performed to investigate the potential non-linear relationship between anthropometric parameters and LVRR. The mediation analysis was performed using the ‘mediation’ R package to evaluate the proportional contribution of baseline myocardial remodeling on the association of body composition with LVRR. Statistically significant echocardiographic parameters in the crude Cox regression model, including baseline LVEF and LVEDDI, was selected as mediating variables, while the other variables were adopted as covariates. Mediation analysis using LVRR as mediator was also conducted to explore the potential mediation role of LVRR in the association between body composition and clinical outcomes. A two-tailed p-value less than 0.05 was regarded as statistically significant.
The data were analyzed via IBM SPSS Statistics version 25, 2017 (IBM, Armonk, New York), R (version 4.1.0) software and GraphPad Prism version 8, 2018 (GraphPad Software, Inc.).
Results
Baseline demographic and clinical characteristics
A total of 240 HFmrEF patients were enrolled in our final analysis. The demographic and clinical characteristics of the study population stratified by LVRR and clinical events were illustrated in Table 1. For overall HFmrEF patients, the median age was 48 years old, and 75% patients was male. The main etiology of HF was ischemic etiology (36.6%). The majority of HFmrEF patients (62.1%) had NYHA functional class III or IV. For co-morbidities, hypertension, diabetes mellitus, and atrial fibrillation was coexisted in 30.0%, 17.9%, and 15.0% of the patients, respectively. Furthermore, optimal medical therapy was widely used. The prescription rate of ACEI/ARB/ARNI, beta-blockers, MRA and SGLT2i was 99.2%, 100%, 89.6%, and 39.6%, separately.
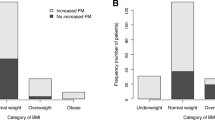
During the 1-year follow-up period, 113 (47.1%) HFmrEF patients got LVRR. The anthropometric parameters varied dramatically between patients with LVRR or without. Although not statistically significant, the BMI was higher in patients with LVRR compared with those without. Moreover, higher proportion of overweight and obesity was observed in patients with LVRR. Furthermore, HFmrEF patients with LVRR exhibited higher fat mass and PBF (all P < 0.05). The levels of the CUN-BAE index and LMI were similar between patients with LVRR or without for HFmrEF. Apart from anthropometric parameters, HF patients with LVRR tended to be younger and had less severe symptoms. Their baseline myocardial remodeling was milder, reflected by higher baseline LVEF and lower LVEDDI. No statistically significant difference was observed in the laboratory tests and medical treatment.
After a median follow-up of 35 months (95% CI 32–38 months), a total of 47 (19.6%) patients suffered cardiovascular death or re-hospitalization for HF. Compared to those without clinical events, the BMI, fat-free mass, fat mass, PBF, and LMI was lower in patients suffered adverse clinical events (all P < 0.05). Furthermore, patients with adverse clinical events tended to be older, and had lower DBP, heart rate, lower prevalence of coronary artery disease, as well as severer mitral regurgitation.
The demographic, clinical, biochemical, and echocardiographic characteristics also varied significantly across the anthropometric measurements, which had been illustrated in Table S1-6. In general, patients with higher BMI, fat-free mass, or fat mass were younger, and had higher frequency of hypertension. Furthermore, patients in higher tertiles of anthropometric parameters had higher LVEDD and lower LVEDDI.
Correlation between body composition and LV remodeling
We evaluated the correlation between anthropometric parameters and baseline echocardiographic parameters (Fig. 2). As indicated in previous studies, the high consistency between the CUN-BAE index and PBF was also observed in our study. The anthropometric indices positively correlated to LVEDD and LV wall thickness, which was consistent to previous multiple echocardiographic studies. However, the inverse correlation between LVEDDI with BMI (r=-0.49, P < 0.001), fat-free mass (r=-0.55, P < 0.001), fat mass (r=-0.50, P < 0.001), PBF (r=-0.30, P < 0.001), and LMI (r=-0.52, P < 0.001) was significant for HFmrEF patients. After adjusted by sex and age, the multivariate linear regression analysis also revealed the tightly negative association between LVEDDI and above anthropometric parameters (Table S7). The anthropometric parameters did not significantly correlate to LVEF and LVMI.
Longitudinal echocardiographic trajectories during follow-up
The dynamic change of echocardiographic parameters of HFmrEF patients stratified by anthropometric parameters tertiles was depicted in Fig. 3. More pronounced and persistent increase of LVEF and decline in LVMI was observed in HFmrEF patients with obesity, highest tertile of fat mass, PBF, CUN-BAE index, and LMI (Fig. 3, all P < 0.05). For the longitudinal changes of echocardiographic parameters across the tertiles of fat-free mass, no obvious difference was detected.
Impact of body composition on LVRR
The univariable and multivariable Cox-proportional hazard analyses was conducted to explore the impact of body composition on LVRR. The crude Cox regression model showed that higher baseline BMI (HR 1.042, 95% CI 1.002–1.083, P = 0.037) and fat mass (HR 1.019, 95% CI 1.002–1.036, P = 0.026) were each significantly associated with higher LVRR rate for HFmrEF (Table 2). Kaplan–Meier curve analysis and the log-rank trend test also illustrated that cumulative incidence of LVRR was significantly higher in HFmrEF patients with obesity or with highest tertile of fat mass (all P < 0.05, Fig. 4 ). However, these correlations were attenuated and no longer significant after additional adjustment for potential confounders. No statistical significance was observed in the relationship between other anthropometric parameters and LVRR. No obvious nonlinear relationships between anthropometric parameters and LVRR were detected via RCS plot (Figure S1). The sensitivity analysis using 6-month echocardiography data also revealed that the anthropometric measurements was associated with the cumulative incidence of LVRR at 6-month follow-up in the univariable Cox regression model, while the relationship vanished in the adjusted model (Table 3).
The role of body composition in clinical outcomes
As shown in Fig. 5 , the rate of rehospitalization for HF and cardiovascular death was significantly lower in for HFmrEF patients with obesity, higher fat-free mass, fat mass, PBF, or LMI (all P for log-rank test for trend < 0.05). Univariable Cox regression analysis also revealed that higher BMI, fat mass, PBF, fat-free mass, and LMI was associated with higher risk of adverse clinical outcomes for HFmrEF (Table 4). However, only fat mass (aHR 0.957, 95% CI 0.917–0.999, P = 0.049) and PBF (aHR 0.963, 95% CI 0.924–0.976, P = 0.043) was confirmed as independent factor for prognosis of HFmrEF after adjusted by potential confounders. Apart from LMI (P for non-linearity: 0.046), no obvious nonlinear relationship between anthropometric induces and clinical outcomes was detected (Figure S2).
Mediation analysis
Given that the association between body composition and LVRR vanished after adjustment by covariates, we want to explore the underling mechanism. We speculate that the higher LVRR rate in patients with higher BMI or fat mass was attributed to their milder baseline LV dilation, considered the significantly negative relationship between baseline LVEDDI and anthropometric parameters. Thus, we conducted the mediation analysis using baseline LVEF and LVEDDI as mediator variables to explore whether and how baseline LVR affect the relationship between body composition with LVRR. Baseline LVEDDI were found to be the full mediating factor in the relationship between BMI and fat mass with LVRR in HFmrEF (Fig. 6A-B).
For HFmrEF patients, we also wanted to explore whether the “obesity paradox” of clinical prognosis could be explained by the inverse relationship between body composition and LVRR. Thus, further mediation analysis was conducted using LVRR as mediator variate. However, the mediation effect of LVRR was weak in the association between anthropometric parameters and clinical outcomes (Fig. 6C-F).
Discussion
In the echocardiography-based cohort study concerning the “obesity paradox” in HFmrEF, our main findings included: (i) the anthropometric parameters correlated inversely with baseline LVEDDI; (ii) HFmrEF patients with higher BMI, fat mass, PBF, CUN-BAE index, or LMI, had more significant improvement of LVEF and decline in LVMI over time; (iii) higher BMI and fat mass was associated with higher LVRR rate for HFmrEF patients; (iv) fat mass and PBF were independent predictors for adverse clinical events for HFmrEF; (v) the association of body composition and LVRR was largely mediated by baseline LVEDDI. To our best knowledge, our research was the first prospective cohort study to explore the role of body composition in LVR, LVRR and long-term clinical prognosis for HFmrEF patients, which will offer more insights and knowledge to the “obesity paradox” in HF.
“Obesity paradox” is an enduring topic in the field of CHF. Although obesity is an important contributor to the growing prevalence of HF, obesity was associated with improved survival and better outcomes in individuals with prevalent CHF, which has been revealed in multiple study populations [41]. The phenomenon of “obesity paradox” has been reported in different HF phenotypes [42, 43]. Although the inverse relationship between BMI and clinical prognosis has been comprehensively elucidated in HFrEF and HFpEF, little clinical researches has revealed the “obesity paradox” in HFmrEF until recently [42,43,44]. Moreover, in previous studies, it is inappropriate using BMI as the single anthropometric index to estimate the total adiposity burden. There are numerous defects and limitations for BMI as a surrogate measure of the amount of adipose tissue. BMI can’t accurately reflect the absolute amount and actual distribution of body fat [45]. More direct measurement of adiposity and body composition, such as fat mass, fat-free mass, and percent body fat, was more appropriate for interpretation of “obesity paradox”. Thus, we conduct the prospective study to comprehensively understand the role of body composition in HFmrEF using multiple anthropometric induces. In consistent to previous studies, we also found that higher BMI was associated with lower rate of adverse clinical events. More significantly, we explore the impact of body composition on LVR and LVRR via a rigorous and longitudinal echocardiographic follow-up scheme, which provide deeper insights to “obesity paradox” in HF.
The impact of body composition on LV structure and function is complex. Excess body weight and increased total blood volume resulted in a rise in cardiac output, stroke volume, and LV end-diastolic pressure. These hemodynamic changes further leaded to enlargement of cardiac chamber and an increase in heart weight and LV wall thickness, thus exacerbated LVR and LV dysfunction [46, 47]. In consistent to previous researches, our study also revealed that the anthropometric indexes, including BMI, fat-free mass, fat mass, and LMI, positively correlated to LVEDD and LV wall thickness for HFmrEF patients. However, a significant inverse relationship between anthropometric indices and LVEDDI was observed in our study. Similar morphologic alteration was also detected in another single-center study. AlRahimi et al. reported the negative correlation between BMI and LV end-diastolic volume index (LVEDVI) for males [48]. Although LVEDD and LV end-diastolic volume (LVEDV) reflected the LV diameter and volume more intuitionistic, LVEDDI and LVEDVI eliminated the bias caused by BSA and body composition to some extent, which could assess the degree of LV dilation more accurately. What is more important, the relationship between body composition and LVR was unclear for HFmrEF patients. Our study revealed that higher body weight and fat mass negatively correlated to baseline LV dilation for HFmrEF. This intriguing finding should be verified in large scale multicenter studies.
LVRR is the pathophysiological hallmark of myocardial recovery and the important therapeutic target for HF. LVRR indicates normalization of LV geometry, significantly increased LV contractility, and improvement of LV function, thus was associated with survival benefits and better prognosis [6]. Better cardiac reverse remodeling of the obese patients may be the underlying mechanism for “obesity paradox” in HF. Previous literatures have pointed out the important role of body composition in LVRR for HF patients. Cescau et al. reported that higher BMI (OR 1.10, 95% CI 1.02–1.19) was associated with higher likelihood of LVRR for HFrEF patients [17]. Another single center prospective study also found that higher BMI (OR 1.151, 95% CI 1.046–1.267) and epicardial adipose tissue volume (OR 1.008, 95% CI 1.000-1.015) was associated with higher rate of LVRR for patients with non-ischemic cardiomyopathy in crude Cox regression model. However, after adjusted by confounders, only the epicardial adipose tissue volume (OR 1.010, 95% CI 1.001–1.019) was validated as the independent predictor for LVRR for [49]. For CHF patients receiving cardiac resynchronization therapy (CRT), BMI was also associated with LVRR and could predict the response to CRT [18]. In the present study, univariable Cox regression analysis indicated that BMI and fat mass was associated with higher cumulative incidence of LVRR for HFmrEF patients via echocardiography dynamic reexaminations. However, this relationship vanished after adjusted by covariates. Our further mediation analysis revealed that higher rate of LVRR in obese patients benefited from their lower baseline LVEDDI and milder LV dilation. The plausible explanation for the “obesity-paradox” may be that patients with higher BMI, fat-free mass, or fat mass had higher frequency of hypertension, and the propensity of arterial hypertension in obese CHF patients made them more likely to tolerate the drug titration of GDMT. Thus, patients with higher BMI exhibited better cardiac reverse remodeling, and had better prognosis than those with lean body mass. For that higher BMI in general was correlated with higher muscle mass, another viewpoint put more emphasis on the adverse impact of sarcopenia on myocardial remodeling in patients with lower weight, thus affect the relationship between BMI and LVRR [49, 50]. Moreover, the lower proinflammatory cytokines, such as tumor necrosis factor alpha, in patients with higher BMI could ameliorate cardiac cachexia, which provided another explanation of “obesity paradox” [18, 51]. The detailed pathophysiological mechanism should be explored in further biological experiments.
Body composition is also tightly associated with the short-term and long-term prognosis for CHF patients. Apart from above mentioned “obesity paradox”, higher fat mass, PBF and lean mass was also associated with improved survival for CHF patients, which has been validated in multiple clinical researches. Konishi et al. revealed that increased fat mass (HR 0.954, 95% CI 0.916–0.993) was independently associated with reduced all-cause mortality for HF patients [52]. A retrospective cohort study identified that increased PBF (HR 0.45, 95% CI 0.22–0.93) correlated with lower risk of short-term cardiac events [53]. A post-hoc analysis of the China PEACE 5p-HF Study also reported that higher LMI exerted a cardioprotective effects and was associated with lower 1-year mortality for HF patients [54]. In our study, we also found that patients with higher BMI, fat mass, PBF, and LMI was with lower risk of re-hospitalization or cardiovascular death. The proposed explanations for the association between body composition and clinical prognosis of HF were complex and ambiguous. Firstly, HF is a catabolic state, and patients with higher body fat and muscle mass had better metabolic reserve and benefits to against cardiac cachexia [13]. secondly, the adipokines and myokines secreted by adipose tissue and skeletal muscle, including omentin, myonectin, and brain-derived neurotrophic factor, could exert cardioprotective effect [55, 56]. Thirdly, the low cardiorespiratory fitness and favorable hemodynamic profile may be the other underlying mechanism for “obesity paradox”.
There were still some limitations in our study. Firstly, our research was just a single-centre study. Due to the prospective design and rigorous echocardiography transvaluation scheme, the sample size was limited. Furthermore, for the specificity of our study cohort, the conclusion should not be popularized and utilized to general clinical practice. Secondly, the body composition indices in our study were estimated via anthropometric prediction equation but not directly measured by DEXA, bioelectrical impedance analysis, or magnetic resonance imaging. Furthermore, the fat mass was calculated based on the estimated fat-free mass, which could not fully reflect the actual fat mass. Although these anthropometric estimation formulas derived from large population study was highly consistent to direct measurements, further investigation based on DEXA or MRA should be conducted to validate our conclusion. Thirdly, the distribution of fat (such as visceral fat, subcutaneous fat, or ectopic fat) could not be assessed in our study. Which type of adipose tissue played a more important role in the “obesity-paradox” was unclear in our study, which limited the interpretation of our results. Fourthly, the criteria of LVRR adopted in our study was mainly depended on LV diameter rather than LV volume. Regional LV remodeling may result in dilated LV diameter but normal volume, which caused the discordance of LVEDDI and LVEDVI to define LVRR. More accurate quantification of LVRR should be assessed by three-dimensional echocardiography or cardiac magnetic resonance.
Conclusions
For Chinese HFmrEF patients, the body composition plays an important role in LVRR and long-term prognosis. Higher BMI and fat mass was associated with higher incidence of LVRR, while this relationship was fully mediated by baseline LVEDDI. It is the fat mass and PBF rather than LMI are the independent predictors for adverse clinical events for HFmrEF patients.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
- ACEI:
-
Angiotensin-converting enzyme inhibitor
- ARB:
-
Angiotensin II receptor blocker
- ARNI:
-
Angiotensin receptor/neprilysin inhibitor
- BIA:
-
Bioelectrical impedance analysis
- BMI:
-
Body mass index
- BSA:
-
Body surface area
- CUN-BAE:
-
Clínica Universidad de Navarr—Body Adiposity Estimator
- DEXA:
-
Dual-energy X-ray absorptiometry
- eGFR:
-
Estimated glomerular filtration rate
- GDMT:
-
Guideline-directed medical therapy
- HF:
-
Heart failure
- HFimpEF:
-
HF with improved ejection fraction
- HFmrEF:
-
HF with mildly reduced ejection fraction
- HFpEF:
-
HF with preserved ejection fraction
- HFrEF:
-
HF with reduced ejection fraction
- IVSTd:
-
Interventricular septal end-diastolic thickness
- LAD:
-
Left atrial diameter
- LMI:
-
Lean mass index
- LV:
-
Left ventricular
- LVEDD:
-
LV end-diastolic diameter
- LVEDDI:
-
LV end-diastolic diameter index
- LVEF:
-
LV ejection fraction
- LVH:
-
LV hypertrophy
- LVMI:
-
LV mass index
- LVPWTd:
-
LV posterior wall end-diastolic thickness
- LVR:
-
LV remodeling
- LVRR:
-
LV reverse remodeling
- MRA:
-
Mineralocorticoid-receptor antagonist
- NT-proBNP:
-
N-terminal pro-B-type natriuretic peptide
- NYHA:
-
New York Heart Association
- PBF:
-
Percent body fat
- RCS:
-
Restricted cubic spline
- RVEDD:
-
Right ventricular end-diastolic diameter
- SGLT2i:
-
Sodium-glucose cotransporter-2 inhibitor
References
Bui AL, Horwich TB, Fonarow GC. Epidemiology and risk profile of heart failure. Nat Rev Cardiol. 2011;8(1):30–41. https://doi.org/10.1038/nrcardio.2010.165.
Riccardi M, Sammartino AM, Piepoli M, Adamo M, Pagnesi M, Rosano G, et al. Heart failure: an update from the last years and a look at the near future. ESC Heart Fail. 2022;9(6):3667–93. https://doi.org/10.1002/ehf2.14257.
Tomasoni D, Adamo M, Lombardi CM, Metra M. Highlights in heart failure. ESC Heart Fail. 2019;6(6):1105–27. https://doi.org/10.1002/ehf2.12555.
La Franca E, Manno G, Ajello L, Di Gesaro G, Minà C, Visconti C, et al. Physiopathology and diagnosis of congestive heart failure: Consolidated certainties and New perspectives. Curr Probl Cardiol. 2021;46(3):100691. https://doi.org/10.1016/j.cpcardiol.2020.100691.
Wu QQ, Xiao Y, Yuan Y, Ma ZG, Liao HH, Liu C, et al. Mechanisms contributing to cardiac remodelling. Clin Sci (Lond). 2017;131(18):2319–45. https://doi.org/10.1042/CS20171167.
Kim GH, Uriel N, Burkhoff D. Reverse remodelling and myocardial recovery in heart failure. Nat Rev Cardiol. 2018;15(2):83–96. https://doi.org/10.1038/nrcardio.2017.139.
Schirone L, Forte M, Palmerio S, Yee D, Nocella C, Angelini F, et al. A review of the Molecular mechanisms underlying the development and progression of Cardiac Remodeling. Oxid Med Cell Longev. 2017;2017:3920195. https://doi.org/10.1155/2017/3920195.
Tayal B, Sogaard P, Delgado-Montero A, Goda A, Saba S, Risum N, Gorcsan J 3. rd. Interaction of Left Ventricular Remodeling and Regional Dyssynchrony on Long-Term Prognosis after Cardiac Resynchronization Therapy. J Am Soc Echocardiogr. 2017;30(3):244–50. https://doi.org/10.1016/j.echo.2016.11.010.
Kitaoka H, Kubo T, Okawa M, Hayato K, Yamasaki N, Matsumura Y, Doi YL. Impact of metalloproteinases on left ventricular remodeling and heart failure events in patients with hypertrophic cardiomyopathy. Circ J. 2010;74(6):1191–6. https://doi.org/10.1253/circj.cj-09-1013.
Yamaguchi S, Abe M, Arasaki O, Shimabukuro M, Ueda S. The prognostic impact of a concentric left ventricular structure evaluated by transthoracic echocardiography in patients with acute decompensated heart failure: a retrospective study. Int J Cardiol. 2019;287:73–80. https://doi.org/10.1016/j.ijcard.2018.07.097.
Wilcox JE, Fang JC, Margulies KB, Mann DL. Heart failure with recovered left ventricular ejection Fraction: JACC Scientific Expert Panel. J Am Coll Cardiol. 2020;76(6):719–34. https://doi.org/10.1016/j.jacc.2020.05.075.
Chudý M, Goncalvesová E. Prediction of left ventricular reverse remodelling: a Mini Review on clinical aspects. Cardiology. 2022;147(5–6):521–8. https://doi.org/10.1159/000526986.
Horwich TB, Fonarow GC, Clark AL. Obesity and the Obesity Paradox in Heart failure. Prog Cardiovasc Dis. 2018 Jul-Aug;61(2):151–6. https://doi.org/10.1016/j.pcad.2018.05.005
Lavie CJ, Milani RV, Ventura HO. Obesity and cardiovascular disease: risk factor, paradox, and impact of weight loss. J Am Coll Cardiol. 2009;53(21):1925–32. https://doi.org/10.1016/j.jacc.2008.12.068.
Gupta PP, Fonarow GC, Horwich TB. Obesity and the obesity paradox in heart failure. Can J Cardiol. 2015;31(2):195–202. https://doi.org/10.1016/j.cjca.2014.08.004.
Alebna PL, Mehta A, Yehya A, daSilva-deAbreu A, Lavie CJ, Carbone S. Update on obesity, the obesity paradox, and obesity management in heart failure. Prog Cardiovasc Dis 2024 Jan-Feb;82:34–42. https://doi.org/10.1016/j.pcad.2024.01.003
Cescau A, Van Aelst LNL, Baudet M, Cohen Solal A, Logeart D. High body mass index is a predictor of left ventricular reverse remodelling in heart failure with reduced ejection fraction. ESC Heart Fail. 2017;4(4):686–9. https://doi.org/10.1002/ehf2.12172.
Cai C, Hua W, Ding LG, Wang J, Chen KP, Yang XW, et al. Association of body mass index with cardiac reverse remodeling and long-term outcome in advanced heart failure patients with cardiac resynchronization therapy. Circ J. 2014;78(12):2899–907. https://doi.org/10.1253/circj.cj-14-0812.
Ye LF, Li XL, Wang SM, Wang YF, Zheng YR, Wang LH. Body Mass Index: an effective predictor of Ejection Fraction Improvement in Heart failure. Front Cardiovasc Med. 2021;8:586240. https://doi.org/10.3389/fcvm.2021.586240.
Butt JH, Petrie MC, Jhund PS, Sattar N, Desai AS, Køber L, et al. Anthropometric measures and adverse outcomes in heart failure with reduced ejection fraction: revisiting the obesity paradox. Eur Heart J. 2023;44(13):1136–53. https://doi.org/10.1093/eurheartj/ehad083.
Carbone S, Lavie CJ, Arena R. Obesity and heart failure: focus on the obesity Paradox. Mayo Clin Proc. 2017;92(2):266–79. https://doi.org/10.1016/j.mayocp.2016.11.001.
Guo L, Liu X, Yu P, Zhu W. The obesity Paradox in patients with HFpEF with or without Comorbid Atrial Fibrillation. Front Cardiovasc Med. 2022;8:743327. https://doi.org/10.3389/fcvm.2021.743327.
Li S, Zheng Y, Huang Y, He W, Liu X, Zhu W. Association of body mass index and prognosis in patients with HFpEF: a dose-response meta-analysis. Int J Cardiol. 2022;361:40–6. https://doi.org/10.1016/j.ijcard.2022.05.018.
Pan XF, Wang L, Pan A. Epidemiology and determinants of obesity in China. Lancet Diabetes Endocrinol. 2021;9(6):373–392. doi: 10.1016/S2213-8587(21)00045-0. Erratum in: Lancet Diabetes Endocrinol. 2021;9(7):e2. https://doi.org/10.1016/S2213-8587(21)00149-2
Zhou BF, Cooperative Meta-Analysis Group of the Working Group on Obesity in China. Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults–study on optimal cut-off points of body mass index and waist circumference in Chinese adults. Biomed Environ Sci. 2002;15(1):83–96.
Kuch B, Gneiting B, Döring A, Muscholl M, Bröckel U, Schunkert H, et al. Indexation of left ventricular mass in adults with a novel approximation for fat-free mass. J Hypertens. 2001;19(1):135–42. https://doi.org/10.1097/00004872-200101000-00018.
Lu J, Yin L. Sex differences in left ventricular stroke work and cardiac power output per unit myocardium relate to blood pressure in apparently healthy adults. PLoS ONE. 2023;18(1):e0280143. https://doi.org/10.1371/journal.pone.0280143.
Gotsman I, Keren A, Amir O, Zwas DR. Increased estimated fat-free mass and fat mass associated with improved clinical outcome in heart failure. Eur J Clin Invest. 2022;52(1):e13655. https://doi.org/10.1111/eci.13655.
Zhou K, Xiang J, Li GY, Pu XB, Zhang L. Body composition and mortality in a cohort study of Chinese patients with hypertrophic cardiomyopathy. Front Cardiovasc Med. 2023;10:988274. https://doi.org/10.3389/fcvm.2023.988274.
Huang FY, Wang H, Huang BT, Liu W, Peng Y, Zhang C, et al. The influence of body composition on the N-terminal pro-B-type natriuretic peptide level and its prognostic performance in patients with acute coronary syndrome: a cohort study. Cardiovasc Diabetol. 2016;15:58. https://doi.org/10.1186/s12933-016-0370-0.
Gómez-Ambrosi J, Silva C, Catalán V, Rodríguez A, Galofré JC, Escalada J, et al. Clinical usefulness of a new equation for estimating body fat. Diabetes Care. 2012;35(2):383–8. https://doi.org/10.2337/dc11-1334.
Vinknes KJ, Nurk E, Tell GS, Sulo G, Refsum H, Elshorbagy AK. The relation of CUN-BAE index and BMI with body fat, cardiovascular events and diabetes during a 6-year follow-up: the Hordaland Health Study. Clin Epidemiol. 2017;9:555–66. https://doi.org/10.2147/CLEP.S145130.
Xu K, Khan MS, Li TZ, Gao R, Terry JG, Huo Y, et al. AI body composition in Lung Cancer Screening: added Value Beyond Lung Cancer Detection. Radiology. 2023;308(1):e222937. https://doi.org/10.1148/radiol.222937.
Pishgar F, Shabani M, Quinaglia AC, Silva T, Bluemke DA, Budoff M, Barr RG, et al. Quantitative analysis of adipose depots by using chest CT and associations with all-cause Mortality in Chronic Obstructive Pulmonary Disease: longitudinal analysis from MESArthritis Ancillary Study. Radiology. 2021;299(3):703–11. https://doi.org/10.1148/radiol.2021203959.
Xu K, Li T, Khan MS, Gao R, Antic SL, Huo Y, et al. Body composition assessment with limited field-of-view computed tomography: a semantic image extension perspective. Med Image Anal. 2023;88:102852. https://doi.org/10.1016/j.media.2023.102852.
Markus MR, Werner N, Schipf S, Siewert-Markus U, Bahls M, Baumeister SE, et al. Changes in Body Weight and Composition are Associated with changes in Left Ventricular geometry and function in the General Population: SHIP (study of Health in Pomerania). Circ Cardiovasc Imaging. 2017;10(3):e005544. https://doi.org/10.1161/CIRCIMAGING.116.005544.
Wang C, Lin Z, Miao D, Zhang H, Fu K, Zhang X, et al. Dose titration of sacubitril/valsartan for heart failure with reduced ejection fraction: a real-world study. ESC Heart Fail. 2023;10(3):1961–71. https://doi.org/10.1002/ehf2.14367.
Nijst P, Martens P, Mullens W. Heart failure with myocardial recovery - the patient whose heart failure has improved: what Next? Prog Cardiovasc Dis. 2017 Sep-Oct;60(2):226–36. https://doi.org/10.1016/j.pcad.2017.05.009
Valli F, Bursi F, Santangelo G, Toriello F, Faggiano A, Rusconi I, et al. Long-Term effects of Sacubitril-Valsartan on Cardiac Remodeling: a parallel echocardiographic study of Left and Right Heart adaptive response. J Clin Med. 2023;12(7):2659. https://doi.org/10.3390/jcm12072659.
Feng J, Liang L, Chen Y, Tian P, Zhao X, Huang B, et al. Big Endothelin-1 as a predictor of reverse remodeling and prognosis in dilated cardiomyopathy. J Clin Med. 2023;12(4):1363. https://doi.org/10.3390/jcm12041363.
Aryee EK, Ozkan B, Ndumele CE. Heart failure and obesity: the latest pandemic. Prog Cardiovasc Dis 2023 May-Jun;78:43–8. https://doi.org/10.1016/j.pcad.2023.05.003
Prausmüller S, Heitzinger G, Pavo N, Spinka G, Goliasch G, Arfsten H, et al. Malnutrition outweighs the effect of the obesity paradox. J Cachexia Sarcopenia Muscle. 2022;13(3):1477–86. https://doi.org/10.1002/jcsm.12980.
Santiago E, Domingo M, Aimo A, Giannoni A, Passino C, Codina P, et al. Body mass index and outcomes in ischaemic versus non-ischaemic heart failure across the spectrum of ejection fraction. Eur J Prev Cardiol. 2021;28(9):948–55. https://doi.org/10.1177/2047487320927610.
Reinhardt M, Schupp T, Abumayyaleh M, Lau F, Schmitt A, Abel N, et al. Obesity Paradox in Heart failure with mildly reduced ejection fraction. Pragmat Obs Res. 2024;15:31–43. https://doi.org/10.2147/POR.S444361.
Goossens GH. The metabolic phenotype in obesity: Fat Mass, Body Fat distribution, and adipose tissue function. Obes Facts. 2017;10(3):207–15. https://doi.org/10.1159/000471488.
Lavie CJ, Alpert MA, Arena R, Mehra MR, Milani RV, Ventura HO. Impact of obesity and the obesity paradox on prevalence and prognosis in heart failure. JACC Heart Fail. 2013;1(2):93–102. https://doi.org/10.1016/j.jchf.2013.01.006.
Cho IJ, Lee SE, Pyun WB. Association of body adiposity with left ventricular concentric remodeling and diastolic dysfunction. Echocardiography. 2024;41(7):e15872. https://doi.org/10.1111/echo.15872.
AlRahimi J, Aboud A, AlQuhaibi AS, Almaghrabi Y, Alghamdi YS, Mufti HN. Effect of isolated obesity on left ventricular function and structure: a single-center experience. Cureus. 2021;13(3):e13988. https://doi.org/10.7759/cureus.13988.
Yamaguchi Y, Shibata A, Yoshida T, Tanihata A, Hayashi H, Kitada R, et al. Epicardial adipose tissue volume is an independent predictor of left ventricular reverse remodeling in patients with non-ischemic cardiomyopathy. Int J Cardiol. 2022;356:60–5. https://doi.org/10.1016/j.ijcard.2022.03.051.
Shi K, Zhang G, Fu H, Li XM, Yu SQ, Shi R, et al. Reduced thoracic skeletal muscle size is associated with adverse outcomes in diabetes patients with heart failure and reduced ejection fraction: quantitative analysis of Sarcopenia by using cardiac MRI. Cardiovasc Diabetol. 2024;23(1):28. https://doi.org/10.1186/s12933-023-02109-7.
Takiguchi M, Yoshihisa A, Miura S, Shimizu T, Nakamura Y, Yamauchi H, et al. Impact of body mass index on mortality in heart failure patients. Eur J Clin Invest. 2014;44(12):1197–205. https://doi.org/10.1111/eci.12354.
Konishi M, Akiyama E, Matsuzawa Y, Sato R, Kikuchi S, Nakahashi H, et al. Prognostic impact of muscle and fat mass in patients with heart failure. J Cachexia Sarcopenia Muscle. 2021;12(3):568–76. https://doi.org/10.1002/jcsm.12702.
Ohori K, Yano T, Katano S, Kouzu H, Honma S, Shimomura K, et al. High percent body fat mass predicts lower risk of cardiac events in patients with heart failure: an explanation of the obesity paradox. BMC Geriatr. 2021;21(1):16. https://doi.org/10.1186/s12877-020-01950-9.
Ge Y, Liu J, Zhang L, Gao Y, Wang B, Wang X, et al. Association of lean body Mass and Fat Mass with 1-Year mortality among patients with heart failure. Front Cardiovasc Med. 2022;9:824628. https://doi.org/10.3389/fcvm.2022.824628.
Takada S, Sabe H, Kinugawa S. Abnormalities of skeletal muscle, adipocyte tissue, and lipid metabolism in Heart failure: practical therapeutic targets. Front Cardiovasc Med. 2020;7:79. https://doi.org/10.3389/fcvm.2020.00079.
Wan S, Cui Z, Wu L, Zhang F, Liu T, Hu J, et al. Ginsenoside Rd promotes omentin secretion in adipose through TBK1-AMPK to improve mitochondrial biogenesis via WNT5A/Ca2 + pathways in heart failure. Redox Biol. 2023;60:102610. https://doi.org/10.1016/j.redox.2023.102610.
Acknowledgements
The graphic abstract was created with Biorender with publication license (Agreement Number: MN2795C5OY).
Funding
This study was supported by the National Key Research and Development Program of China (No. 2021YFF0501404, 2021YFF0501403), the grants of the National Natural Science Foundation of China (No. 82200303 and 81873516), the Shandong Provincial Natural Science Foundation (ZR2022QH056).
Author information
Authors and Affiliations
Contributions
Xiaoping Ji and Huixia Lu: Designed and supervised the study and methodology. Kang Fu: Writing the original draft, and conducted formal analysis. Youran Dong, Zhiyuan Wang, Junlin Teng, Congyi Cheng, and Cong Su: contributed the data collection, interpretation of the data, and participated in the literature research.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Fu, K., Dong, Y., Wang, Z. et al. The role of body composition in left ventricular remodeling, reverse remodeling, and clinical outcomes for heart failure with mildly reduced ejection fraction: more knowledge to the “obesity paradox”. Cardiovasc Diabetol 23, 334 (2024). https://doi.org/10.1186/s12933-024-02430-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-024-02430-9