Abstract
Background
The fat-to-muscle mass ratio (FMR), integrating the antagonistic effects of fat and muscle mass, has been suggested as a valuable indicator to assess cardiometabolic health independent of overall adiposity. However, the specific associations of total and regional FMR with cardiometabolic risk are poorly understood. We aimed to examine sex-specific associations of total and regional FMR with single and clustered cardiometabolic risk factors (CRFs).
Methods
13,505 participants aged 20 years and above were included in the cross-sectional study. Fat mass and muscle mass were assessed using a bioelectrical impedance analysis device. FMR was estimated as fat mass divided by muscle mass in corresponding body parts (whole body, arm, leg, and trunk). Clustered CRFs was defined as the presence of two or more risk factors, including hypertension, elevated blood glucose, dyslipidemia, insulin resistance (IR), and hyperuricemia. IR was assessed by the triglyceride glucose (TyG) index. Multivariable logistic regression models were applied to explore the associations of FMR in the whole body and body parts with single and clustered CRFs.
Results
The odds ratios (ORs) increased significantly for all single and clustered CRFs with the per quartile increase of total and regional FMR in both sexes (P for trend < 0.001), following adjustment for confounders. Among the regional parts, FMRs of the legs presented the strongest associations for clustered CRFs in both men and women, with adjusted OR of 8.54 (95% confidence interval (CI): 7.12–10.24) and 4.92 (95% CI: 4.24–5.71), respectively. Significant interactions (P for interaction < 0.05) were identified between age and FMRs across different body parts, as well as between BMI status and FMRs in different regions for clustered CRFs. Restricted cubic splines revealed significant non-linear relationships between FMRs of different body parts and clustered CRFs in both sexes (P for nonlinear < 0.05).
Conclusions
FMRs in the whole body and different regions were significantly associated with single and clustered CRFs in the general Chinese population. The association between FMR and clustered CRFs was more pronounced in youngers than in the elderly.
Similar content being viewed by others
Introduction
Cardiovascular diseases (CVDs) are the leading cause of mortality globally [1]. Cardiometabolic disorders, as main modifiable risk factors for CVD, have posed serious burden on individuals, families and society [1]. Therefore, it is urgent and crucial to prevent cardiometabolic disorder. Obesity, a well-established risk factor for CVDs and other chronic diseases, is also associated with clustering of other CRFs such as hypertension, elevated glucose and dyslipidemia [2]. Body mass index (BMI) is commonly used to assess overall adiposity in population studies. However, BMI has a major limitation in determining obesity since it cannot discriminate between fat and muscle content [3]. Body composition varies greatly among individuals with the same BMI. In addition, individuals with similar BMI levels can exhibit diverse metabolic characteristics, including differences in lipid profiles, glucose intolerance, and blood pressure (BP) [4, 5].
Several studies have revealed that body composition could play important roles in quantifying CRFs [6,7,8]. For example, muscle mass is considered a protective factor and had a negative relationship with cardiometabolic parameters [9]. By contrast, elevated fat mass is strongly related with adverse CRFs, including hypertension, dyslipidemia, and impaired glucose regulation [6]. Furthermore, a significant decrease in muscle mass and an increase in fat mass may lead to sarcopenia or sarcopenia obesity, both of which are proposed to have detrimental effects on cardiometabolic profiles and mortality [10, 11]. The components of body composition are intricately interrelated. Fat mass stands for the metabolic load, while muscle mass signifies metabolic capacity; determining CRFs within the context of their interrelationship but rather focusing on their absolute amounts, presents an intriguing avenue for research [12]. Hence, the FMR, a novel marker that integrates the effects of muscle and fat mass, has been considered a promising body composition indicator for CRFs, CVDs, and mortality [13 – 15].
Previous studies have reported that the FMR was associated with diabetes, hypertension, and metabolic syndrome (MetS) in both men and women [16,17,18]. However, there is a lack of research exploring the associations between total and regional FMR and insulin resistance, as well as clustered CRFs (two or more factors). Additionally, existing studies have been hampered by small sample sizes, a focus on Western populations, and a failure to consider FMR in different body parts, resulting in limited evidence in large-scale general populations, particularly in China [17, 18]. Considering that muscle gain and exercise may have site-specific effects, determining FMR associations at different anatomical sites (including arms, legs, and trunk) could provide segmental body information and enhance comprehension of potential clinical and public health implications, which still requires further research. Given the remarkable sex difference in body composition distribution, such as muscle mass and fat mass, sex-stratified analyses were performed in the current study.
Using data from the China National Health Survey (CNHS), we aimed to comprehensively assess the sex-specific relationship between FMR in various body regions (including the whole body, arm, leg, and trunk) and CRFs, both individually and clustering multiple risk factors.
Materials and methods
Study design and participants
A cross-sectional study was conducted in Guangdong (South China), Jilin (Northeastern China), and Jiangsu (East China) provinces from April to November 2023. The present study originated from the CNHS, an ongoing nationally representative cross-sectional study initiated in 2012. Additional details about the study design have been provided elsewhere [19]. In short, a multi-stage stratified cluster sampling method was used to recruit permanent residents aged 20 years and above in both urban and rural areas. In this study, the respondents completed a standardized questionnaire and underwent physical measurements to collect health-related information, including demographic characteristics, lifestyle factors, and personal disease history. Moreover, venous blood samples were collected after an 8-hour fasting period for the measurement of glucose and serum lipid levels.
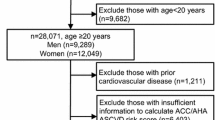
A total of 13,904 Chinese Han adults completed the survey. We excluded participants under the age of 20, with missing information on the measurement of CRFs, or those with missing data on body composition parameters (muscle mass and fat mass in the trunk, arm, and leg), the remaining 13,505 subjects in the final analysis consisting of 5,208 men and 8,297 women (Supplemental Fig. 1). The study has been carried out in accordance with the Declaration of Helsinki. The Ethical Review Committee of the Institute of Basic Medical Sciences Chinese Academy of Medical Sciences, Beijing, China, has approved this study under the protocol (No. 2022177 and No. 2022134). Written informed consent was obtained from all participants.
Exposure assessment
Data on height, weight, and body composition were collected by trained program staff using well-calibrated instruments according to a standard protocol. Height was measured in centimeter (to the nearest 0.1 cm) without shoes using a stadiometer (SECA, Germany). After the height measurement, weight (in kilograms to the nearest 0.1 kg) and body composition were measured in light clothes and bare feet using a standard multi-frequency segmental Tanita MC780MA analyzer (Tanita Inc, Japan) by the method of bioelectrical impedance analysis (BIA). To ensure accurate measurements, participants were instructed to place their bare feet on the designated markings on the analyzer platform and to keep their feet still and in full contact with the platform. Simultaneously, participants were asked to grip the two metal handles firmly using their hands, allowing their arms to hang loosely by their sides. The BIA method, validated for accuracy and precision [20, 21], was used to estimate muscle mass and fat mass in the whole body, trunk, left arm, right arm, left leg, and right leg. The right and left arms/legs and trunk were integrated into a whole body. FMR was defined as fat mass divided by estimated muscle mass in the corresponding body parts. Therefore, the total and regional (arm, leg, and trunk) FMRs were the exposures to be examined. In the analysis, FMR values were classified into quartiles (Q1-Q4) from the lowest (Q1) to the highest (Q4).
Outcome assessment
Clustered CRFs was defined as the presence of two or more risk factors, including hypertension, elevated blood glucose, dyslipidemia, IR, and hyperuricemia.
BP was measured three times on the upper right arm using an electronic BP device (Omron HEM-907, Japan) with the participant in a sitting posture. There was one minute between each measurement and the average of three readings was recorded. Hypertension was defined as the participant who had a mean systolic BP ≥ 140 mmHg and/or a mean diastolic BP ≥ 90 mmHg and/or self-reported diagnosed hypertension by a physician and/or receiving antihypertensive medication [22]. Elevated blood glucose was defined as a fasting plasma glucose (FPG) level ≥ 6.1 mmol/L, or a self-reported diagnosis of diabetes [23]. Dyslipidemia was defined as high total cholesterol (high TC, a TC level ≥ 6.2 mmol/L), or high triglyceride (high TG, a TG level ≥ 2.3 mmol/L), or high low-density lipoprotein cholesterol (high LDL-C, a LDL-C level ≥ 4.1 mmol/L), or low high-density lipoprotein cholesterol (low HDL-C, a HDL-C level ≤ 1.0 mmol/L), or a self-reported diagnosed dyslipidemia [24]. IR was assessed by the TyG index, which is a simple and reliable clinical marker of IR [25, 26]. The TyG index was calculated as Ln [TG (mg/dl)×FPG (mg/dl)/2] [27]. IR was defined as a TyG index above the 75th percentile for each sex in the study population [28]. Hyperuricemia was defined as a serum uric acid (SUA) level > 420 µmol/L in men and SUA > 360 µmol/L in women, or current use of SUA-lowering drugs [29, 30].
Covariates
The following potential confounding factors were considered in the present study: age, residential area (rural/urban), region, educational level (elementary school or below, or secondary school, or college or higher), smoking status (never, ever, or current), drink status (never, ever, or current), physical activities [light level of both occupational and leisure-time physical activity (low); moderate or high level of either occupational or leisure-time physical activity (moderate); moderate or high level of both occupational and leisure-time physical activity (high)]. The information on menopausal status was obtained through self-reported in the face-to-face questionnaire, where they were asked whether they had experienced menstrual bleeding within the past 12 months. BMI was calculated as weight in kilograms divided by the square of the height in meters (kg/m2). BMI categories were defined as underweight (< 18.5 kg/m2), normal (18.5–23.9 kg/m2), overweight, or obesity (≥ 24 kg/m2) [31].
Statistical analysis
Continuous variables were expressed as mean ± standard deviation (SD) or median (interquartile range, IQR), and categorical variables were reported as frequency (percentage, %). Comparisons of baseline characteristics between men and women were conducted using a t-test or Mann-Whitney U-test for continuous variables and a Chi-square-test for categorical variables.
Multivariable logistic regression models were applied to estimate ORs and 95% CIs for the associations between quartiles of total and regional FMR and CRFs in men and women. Models were adjusted for age (continuous variable), residential area, region, educational level, smoking status, drinking status, physical activities, and menopausal status in women. The associations of FMR in total and body parts with the specific dyslipidemia components, including high TC, high TG, high LDL-C, and low HDL-C, were also examined. The linear trend test was performed using the median value of sex-specific FMR for each quartile estimated as a continuous variable in the models. We further performed restricted cubic splines (RCS) with four knots at the 5th, 35th, 65th, and 95th percentiles to explore the potential nonlinear association between FMR and clustered CRFs. RCS analysis was conducted using R software (version 4.2.2). The interaction analyses were performed to investigate the relationship between FMR and clustered CRFs stratified by age (20–39 years, 40–59years, or ≥ 60 years), BMI categories (BMI < 24 kg/m2 and BMI ≥ 24 kg/m2), and menopausal status in women (yes/no). The potential interactions were measured by using the likelihood ratio test to compare models with and without a cross-product term. We further conducted a sensitivity analysis to assess the robustness of our results. Participants with a previous diagnosis of hypertension, diabetes, dyslipidemia, and hyperuricemia were excluded to minimize the potential impact of reverse causality. Data analyses were performed using SAS, version 9.4 (SAS Institute Inc, Cary, NC, USA). A two-sided P value < 0.05 was considered to be statistically significant.
Results
General characteristics of participants
Table 1 summarizes the general characteristics of the study population by sex. A total of 13,505 participants were included in the present study, which comprised 5,208 men (mean age, 53.27 ± 12.93 years) and 8,297 women (mean age, 51.82 ± 12.31 years). Among the women, 58.48% (4,852 out of 8,297) had experienced menopause. Overall, the total and regional FMR significantly differed between men and women (P < 0.001). It was observed that there were notable sex differences in single CRFs, with men presenting higher prevalence in various aspects, excluding IR. Additionally, the prevalence of clustered CRFs was higher in men compared to women and increased with age (Supplemental Table 1). The demographic characteristics of the participants according to the quartiles FMR of the whole body in men and women are shown in Supplemental Table 2. Participants in Q4 of whole FMR had the highest prevalence of hypertension, elevated blood glucose, dyslipidemia, hyperuricemia, and clustered CRFs compared to participants in the other three FMR quartiles in both sexes (all P < 0.001).
Total and regional fat-to-muscle mass ratio and cardiometabolic risk
The associations of total and regional FMR with CRFs were examined using multivariable logistic regression models by sex as shown in Table 2. After adjusting for confounding factors, the FMR in whole body and body parts exhibited significant associations with all examined risk factors (all P < 0.05) in men and women. Compared with the Q1, the multivariable-adjusted ORs of the Q4 of total FMR for hypertension, elevated blood glucose, dyslipidemia, insulin resistance, and hyperuricemia were 5.28 (95% CI: 4.39–6.34), 2.33 (95% CI: 1.92–2.83), 4.15 (95% CI: 3.50–4.91), 5.47 (95% CI: 4.39–6.82), and 4.11 (95%CI: 3.42–4.93), respectively, for men and 3.29 (95% CI: 2.82–3.85), 2.47 (95% CI: 2.06–2.96), 2.42 (95% CI: 2.11–2.78), 5.10 (95% CI: 4.28–6.07), and 3.92 (95%CI: 3.29–4.67), respectively, for women. The associations of the total and regional FMR with the risk of dyslipidemia components are shown in Supplemental Table 3. Compared with the Q1, the effect of the FMR Q4 was significant for high TC, high TG, high LDL-C, and low HDL-C in women, whereas the association of FMR in the arms for high TC and high LDL-C was not statistically significant in men.
Figure 1 illustrates the effect [OR (95% CI)] of FMR quartiles on clustered CRFs by sex. Following adjustment for confounding factors, the FMR in whole body and body parts were significantly associated with clustered CRFs (all P < 0.05) in men and women. FMRs were more strongly associated with clustered CRFs in men compared to women. Among the regional body parts, FMR of the legs presented the strongest associations in both men and women, with adjusted OR of 8.54 (95% CI: 7.12–10.24) and 4.92 (95% CI: 4.24–5.71), respectively. Notably, the adjusted ORs displayed a significant increase with ascending FMR quartiles from Q1 to Q4 (all P for trend < 0.001), for both the whole body and regional body parts. Figure 2 visualized the nonlinear associations between FMRs and clustered CRFs using RCS analysis. A J-shaped association were observed between total and regional FMR and clustered CRFs in both men and women (all P for non-linear < 0.05).
The effect [OR (95% CI)] of quartile of FMR on clustered cardiometabolic risk factors by sex. All models were adjusted for age, physical activity, education level, smoking status, residential area, drinking, region, and menopausal status in women. Clustered cardiometabolic risk was defined as the presence of 2 or more risk factors, including hypertension, elevated blood glucose, dyslipidemia, insulin resistance, and hyperuricemia. (a) FMR of the whole body, trunk, arm and leg in men; (b) FMR of the whole body, trunk, arm and leg in women. FMR: Fat-to-muscle mass ratio; OR: odds ratio; CI: confidence interval
Association of fat-to-muscle mass ratio (FMR) with clustered cardiometabolic risk by sex. All models were adjusted for age, physical activity, education level, smoking status, residential area, drinking, region, and menopausal status in women. Clustered cardiometabolic risk was defined as the presence of 2 or more risk factors, including hypertension, elevated blood glucose, dyslipidemia, insulin resistance, and hyperuricemia. (a-d) FMR of the whole body, trunk, arm and leg in men; (e-h) FMR of the whole body, trunk, arm and leg in women. Odds ratios are reported by solid lines and 95% CIs by shaded areas. The reference point is the 50th percentile for each FMR, using four knots at the 5th, 35th, 65th, and 95th percentiles. FMR: Fat-to-muscle mass ratio; OR: odds ratio; CI: confidence interval
Age-stratified, BMI-stratified analyses and sensitivity analyses
Stratified analysis by age group was conducted to identify whether age modified the relationship between FMR and clustered CRFs (Table 3). Interestingly, the association between FMR and clustered CRFs was more pronounced in youngers (adults aged 20–39 years) than in the elderly (adults aged 60 years or above) in both sexes. The significant modifying effect was observed in women (all P for interaction < 0.001); while the effect was only observed in the arms and legs of men. We also observed a significant interaction between FMR in the whole body and specific body parts and BMI category on clustered CRFs in both sexes, excepting FMR of the whole body and legs in men (all P for interaction < 0.05; Table 4). Similarly, significant interaction effects were observed for menopausal status in women (all P for interaction < 0.05; Supplemental Table 4). In sensitivity analysis, similar findings were found when excluding the participants with a previous diagnosis of hypertension, diabetes, dyslipidemia, and hyperuricemia (Supplemental Table 5).
Discussion
In the large-scale cross-sectional study that covered northeast, north, and south China, we found a promising and easy-to-use body composition indicator—FMR and explored its association with cardiometabolic health. The findings demonstrated a significant association between FMRs in various body regions and single as well as clustered CRFs in both sexes. In addition, these associations were strongly modified by age group and BMI category for both sexes. Among the regional body parts, FMRs of the legs presented the strongest associations in men and women. To our knowledge, the present study is the first to identify the sex-specific associations of FMRs in different body regions with single and clustered CRFs among the general Chinese population.
Several studies have identified the relationships of fat mass and muscle mass separately with CRFs in diverse populations. However, these findings have exhibited inconsistent conclusions. A perspective cohort study of 132,324 participants (mean age, 37.1 years) with a 4-year follow-up, revealed a significant association between low relative skeletal muscle mass and the incidence of hypertension in men after adjustment for confounding factors, whereas, no statistically significant association was observed in women [32]. A cross-sectional study included 1,413 community-dwelling older adults found that muscle mass was negatively associated with MetS in both sexes [33]. Another study involving older people aged 75 years and above, indicated that muscle mass was associated with Mets in women, while no significant association was evidenced in men after adjusting for fat mass [34]. Likewise, the evidence regarding the association between fat mass and CRFs is not always consistent, with some studies reporting a positive association between arm fat mass and CRFs [35] and others finding no such association [36]. The reasons for the apparent discrepancies in these associations remain unclear, but the metabolic load-capacity model provides a plausible explanation. Thus, it is important to consider fat mass and muscle mass together to mitigate such inconsistencies. FMR may be a potential index reflecting the combined effects of fat mass and skeletal muscle mass [37].
Multiple epidemiologic studies have confirmed the association of FMR with CRFs. A nationally representative study including Korean adults reported a positive relationship between FMR and the prevalence of MetS and insulin resistance [38]. Chen et al. performed a population-based observational study of 66,829 adults and found a strong association of FMR with hypertension, prediabetes, and diabetes mellitus [16]. Another cross-sectional study involving 875 participants yielded similar results, demonstrating that a higher FMR was significantly linked with impaired fasting glucose metabolic risk [39]. These findings support our hypothesis that FMR is a valuable indicator for screening CRFs, suggesting the significance of considering the balance of fat mass and muscle mass when exploring CRFs in the general population.
Our study demonstrated that FMRs were more strongly associated with clustered CRFs in men compared to women. This may be caused by differences in fat distribution, estrogen, and androgen levels, and sex-specific genetics [40, 41]. However, few of these studies have explored the associations between FMR and CRFs in different body regions. In the present study, we found that FMR of the legs presented the strongest associations for clustered CRFs in men and women. This result is similar to a study of a British population that revealed a stronger association between FMR in legs and diabetes than FMR in the arms and trunk [17]. The findings suggest that the balance of muscle and fat in the legs is more important for cardiometabolic health. They also emphasize the importance of targeted interventions to improve muscle and fat mass in specific body regions as a preventative measure for CRFs in clinical and public health settings.
We observed that the positive association between FMR and clustered CRFs was remarkably strengthened among younger participants, suggesting that the early improvements in muscle mass and strength have a more pronounced impact on overall health outcomes. This finding is consistent with a prior study utilizing the UK Biobank database, revealing a heightened association between FMRs and diabetes in young adults compared to older adults [17]. Individuals aged 20–60 typically experience stronger metabolic activity with a relatively faster metabolic rate than older people [42]. At this stage, the body may exhibit increased sensitivity to fluctuations in the FMRs, making it more susceptible to such variations. Furthermore, the elderly faced challenges of decline in physical abilities, increased comorbidities, impairment of mental health, and limited life expectancy [43]. These factors may offset the clinical benefits derived from the improvement of body composition.
The underlying biological mechanisms have been proposed to understand the relationship between FMR and CRFs. Adipose tissue serves not only as an energy reservoir but also as an active endocrine organ, secreting various pro-inflammatory cytokines such as tumor necrosis factor and interleukin 6, thereby leading to chronic inflammation [44]. The chronic inflammation in adipose tissue may cause IR and metabolic disorders, consequently increasing the risk of high blood glucose, hypertension, and dyslipidemia [45]. On the other hand, skeletal muscle stands as the principal site for insulin-regulated glucose uptake. A decline in muscle mass is significantly correlated with decreased insulin sensitivity [46]. Our study identified a positive association between FMR and IR, providing further support for this correlation. Whole-body IR is the important pathogenic factor of cardiometabolic diseases including dyslipidemia and type 2 diabetes mellitus [47]. Given the advantageous and adverse attributes of muscle and fat mass, the cumulative effect of the balance between the two body components could potentially impact CRFs.
The strengths of the study include the large sample size of the Chinese general population, which enables sufficient statistical power to examine the associations and interactions. In addition, the data collection process across three provinces adhered to standardized protocols, with subsequent analysis meticulously adjusting for multiple confounders. Notably, the study used a comprehensive index that evaluates both total and body regions, integrating the impacts of muscle and fat mass to evaluate CRFs in the study. Meanwhile, we acknowledge some potential limitations. First, the study is a cross-sectional design, it is limited in interpreting causality between FMR and CRFs. Second, fat mass and muscle mass were not measured by high precision imaging techniques such as magnetic resonance imaging or dual x-ray absorptiometry (DXA). Nevertheless, BIA was a feasible method and an adequate measurement to estimate body composition such as body fat and muscle in large-scale epidemiological studies due to it is convenient, fast, noninvasive, cost-effective and easy to implement [48]. Last, our study included the general Han population in three provinces in China, which may affect the generalizability of the findings to other regions or countries. Large-scale prospective cohort studies involving multi-ethnic adults are needed in the future to further validate the association between FMR and CRFs and to explore the complex mechanisms.
In conclusion, the findings of this study demonstrated a significant association between FMR and both single and clustered cardiometabolic risk factors in the general Chinese population, regardless of body region. These associations were particularly pronounced among young adults. Our finding highlights the importance of early surveillance of muscle mass, fat mass, and FMR to alleviate the burden of cardiometabolic disease.
Data availability
“The datasets analyzed during the present study are available from the corresponding author on reasonable request.”
Change history
10 September 2024
Reference citations 131415 should be 13-15
Abbreviations
- BIA:
-
Bioelectrical impedance analysis
- BMI:
-
Body mass index
- BP:
-
Blood pressure
- CI:
-
Confidence interval
- CRFs:
-
Cardiometabolic risk factors
- CVD:
-
Cardiovascular disease
- FMR:
-
Fat-to-muscle mass ratio
- FPG:
-
Fasting plasma glucose
- HDL-C:
-
High-density lipoprotein cholesterol
- IR:
-
Insulin resistance
- IQR:
-
Interquartile range
- LDL-C:
-
Low-density lipoprotein cholesterol
- MetS:
-
Metabolic syndrome
- OR:
-
Odds ratio
- RCS:
-
Restricted cubic splines
- SUA:
-
Serum uric acid
- SD:
-
Standard deviation
- TC:
-
Total cholesterol
- TG:
-
Triglyceride
- TyG:
-
Triglyceride glucose
References
Mensah GA, Fuster V, Murray CJL, et al. Global Burden of Cardiovascular diseases and risks, 1990–2022. J Am Coll Cardiol. 2023;82(25):2350–473.
Chooi YC, Ding C, Magkos F. The epidemiology of obesity. Metabolism. 2019;92:6–10.
Romero-Corral A, Somers VK, Sierra-Johnson J, et al. Accuracy of body mass index in diagnosing obesity in the adult general population. Int J Obes (Lond). 2008;32(6):959–66.
Shea JL, King MT, Yi Y, et al. Body fat percentage is associated with cardiometabolic dysregulation in BMI-defined normal weight subjects. Nutr Metab Cardiovasc Dis. 2012;22(9):741–7.
De Lorenzo A, Bianchi A, Maroni P, et al. Adiposity rather than BMI determines metabolic risk. Int J Cardiol. 2013;166(1):111–7.
Ramírez-Vélez R, Correa-Bautista JE, Sanders-Tordecilla A, et al. Percentage of body Fat and Fat Mass Index as a Screening Tool for metabolic syndrome prediction in Colombian University students. Nutrients. 2017;9(9):1009.
Schorr M, Dichtel LE, Gerweck AV, et al. Sex differences in body composition and association with cardiometabolic risk. Biol Sex Differ. 2018;9(1):28.
He J, Zhang B, Fan Y, et al. Comparison of bioelectrical body and visceral fat indices and anthropometric measures in relation to type 2 diabetes by sex among Chinese adults, a cross-sectional study. Front Public Health. 2023;11:1001397.
Zhang H, Lin S, Gao T et al. Association between Sarcopenia and metabolic syndrome in Middle-aged and older non-obese adults: a systematic review and Meta-analysis. Nutrients 2018, 10(3).
Chung JY, Kang HT, Lee DC, et al. Body composition and its association with cardiometabolic risk factors in the elderly: a focus on sarcopenic obesity. Arch Gerontol Geriatr. 2013;56(1):270–8.
Wei S, Nguyen TT, Zhang Y, et al. Sarcopenic obesity: epidemiology, pathophysiology, cardiovascular disease, mortality, and management. Front Endocrinol (Lausanne). 2023;14:1185221.
Bosy-Westphal A, Braun W, Geisler C, et al. Body composition and cardiometabolic health: the need for novel concepts. Eur J Clin Nutr. 2018;72(5):638–44.
Zhou R, Chen HW, Lin Y, et al. Total and Regional Fat/Muscle Mass ratio and risks of Incident Cardiovascular Disease and Mortality. J Am Heart Assoc. 2023;12(17):e030101.
He H, Pan L, Wang D, et al. The association between muscle-to-fat ratio and cardiometabolic risks: the China National Health Survey. Exp Gerontol. 2023;175:112155.
Yu B, Sun Y, Du X, et al. Age-specific and sex-specific associations of visceral adipose tissue mass and fat-to-muscle mass ratio with risk of mortality. J Cachexia Sarcopenia Muscle. 2023;14(1):406–17.
Chen YY, Fang WH, Wang CC, et al. Fat-to-muscle ratio is a useful index for cardiometabolic risks: a population-based observational study. PLoS ONE. 2019;14(4):e0214994.
Wang N, Sun Y, Zhang H, et al. Total and regional fat-to-muscle mass ratio measured by bioelectrical impedance and risk of incident type 2 diabetes. J Cachexia Sarcopenia Muscle. 2021;12(6):2154–62.
Xu K, Zhu HJ, Chen S, et al. Fat-to-muscle ratio: a New Anthropometric Indicator for Predicting Metabolic Syndrome in the Han and Bouyei populations from Guizhou Province, China. Biomed Environ Sci. 2018;31(4):261–71.
He H, Pan L, Pa L, et al. Data Resource Profile: the China National Health Survey (CNHS). Int J Epidemiol. 2018;47(6):1734–f1735.
Cheng KY, Chow SK, Hung VW, et al. Diagnosis of Sarcopenia by evaluating skeletal muscle mass by adjusted bioimpedance analysis validated with dual-energy X-ray absorptiometry. J Cachexia Sarcopenia Muscle. 2021;12(6):2163–73.
Mijnarends DM, Meijers JM, Halfens RJ, et al. Validity and reliability of tools to measure muscle mass, strength, and physical performance in community-dwelling older people: a systematic review. J Am Med Dir Assoc. 2013;14(3):170–8.
Zhang M, Shi Y, Zhou B, et al. Prevalence, awareness, treatment, and control of hypertension in China, 2004-18: findings from six rounds of a national survey. BMJ. 2023;380:e071952.
Chinese Diabetes Society. Guideline for the prevention and treatment of type 2 diabetes mellitus in China (2020 editon). Chin J Diabetes Mellitus. 2021;13(4):315–409.
Li JJ, Zhao SP, Zhao D, et al. 2023 Chinese guideline for lipid management. Front Pharmacol. 2023;14:1190934.
Guerrero-Romero F, Simental-Mendía LE, González-Ortiz M, et al. The product of triglycerides and glucose, a simple measure of insulin sensitivity. Comparison with the euglycemic-hyperinsulinemic clamp. J Clin Endocrinol Metab. 2010;95(7):3347–51.
Lopez-Jaramillo P, Gomez-Arbelaez D, Martinez-Bello D, et al. Association of the triglyceride glucose index as a measure of insulin resistance with mortality and cardiovascular disease in populations from five continents (PURE study): a prospective cohort study. Lancet Healthy Longev. 2023;4(1):e23–33.
Simental-Mendía LE, Rodríguez-Morán M, Guerrero-Romero F. The product of fasting glucose and triglycerides as surrogate for identifying insulin resistance in apparently healthy subjects. Metab Syndr Relat Disord. 2008;6(4):299–304.
Son DH, Ha HS, Lee YJ. Association of Serum Alkaline Phosphatase with the TG/HDL ratio and TyG index in Korean adults. Biomolecules 2021, 11(6).
Zhang M, Zhu X, Wu J, et al. Prevalence of Hyperuricemia among Chinese adults: findings from two nationally Representative cross-sectional surveys in 2015-16 and 2018-19. Front Immunol. 2021;12:791983.
Johnson RJ, Bakris GL, Borghi C, et al. Hyperuricemia, Acute and chronic kidney Disease, Hypertension, and Cardiovascular Disease: report of a Scientific Workshop Organized by the National Kidney Foundation. Am J Kidney Dis. 2018;71(6):851–65.
Zhou BF. Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults–study on optimal cut-off points of body mass index and waist circumference in Chinese adults. Biomed Environ Sci. 2002;15(1):83–96.
Han JM, Lee MY, Lee KB, et al. Low relative skeletal muscle mass predicts incident hypertension in Korean men: a prospective cohort study. J Hypertens. 2020;38(11):2223–9.
Song P, Han P, Zhao Y, et al. Muscle mass rather than muscle strength or physical performance is associated with metabolic syndrome in community-dwelling older Chinese adults. BMC Geriatr. 2021;21(1):191.
Koo HS, Kim MJ, Kim KM, et al. Decreased muscle mass is not an independent risk factor for metabolic syndrome in Korean population aged 70 or older. Clin Endocrinol (Oxf). 2015;82(4):509–16.
Hu G, Bouchard C, Bray GA, et al. Trunk versus extremity adiposity and cardiometabolic risk factors in white and African American adults. Diabetes Care. 2011;34(6):1415–8.
Sánchez-López M, Ortega FB, Moya-Martínez P, et al. Leg fat might be more protective than arm fat in relation to lipid profile. Eur J Nutr. 2013;52(2):489–95.
Prado CM, Wells JC, Smith SR, et al. Sarcopenic obesity: a critical appraisal of the current evidence. Clin Nutr. 2012;31(5):583–601.
Seo YG, Song HJ, Song YR. Fat-to-muscle ratio as a predictor of insulin resistance and metabolic syndrome in Korean adults. J Cachexia Sarcopenia Muscle. 2020;11(3):710–25.
Gamboa-Gómez CI, Simental-Mendía LE, Rodríguez-Morán M, et al. The fat-to-lean mass ratio, a novel anthropometric index, is associated to glucose metabolic disorders. Eur J Intern Med. 2019;63:74–8.
Randall JC, Winkler TW, Kutalik Z, et al. Sex-stratified genome-wide association studies including 270,000 individuals show sexual dimorphism in genetic loci for anthropometric traits. PLoS Genet. 2013;9(6):e1003500.
Lovejoy JC, Champagne CM, de Jonge L, et al. Increased visceral fat and decreased energy expenditure during the menopausal transition. Int J Obes (Lond). 2008;32(6):949–58.
Pontzer H, Yamada Y, Sagayama H, et al. Daily energy expenditure through the human life course. Science. 2021;373(6556):808–12.
Mooradian AD. Evidence-based management of diabetes in older adults. Drugs Aging. 2018;35(12):1065–78.
Kunz HE, Hart CR, Gries KJ, et al. Adipose tissue macrophage populations and inflammation are associated with systemic inflammation and insulin resistance in obesity. Am J Physiol Endocrinol Metab. 2021;321(1):E105–21.
Madero M, Katz R, Murphy R, et al. Comparison between different measures of Body Fat with kidney function decline and Incident CKD. Clin J Am Soc Nephrol. 2017;12(6):893–903.
Merz KE, Thurmond DC. Role of skeletal muscle in insulin resistance and glucose uptake. Compr Physiol. 2020;10(3):785–809.
Lee SH, Park SY, Choi CS. Insulin resistance: from mechanisms to therapeutic strategies. Diabetes Metab J. 2022;46(1):15–37.
Kim M, Shinkai S, Murayama H, et al. Comparison of segmental multifrequency bioelectrical impedance analysis with dual-energy X-ray absorptiometry for the assessment of body composition in a community-dwelling older population. Geriatr Gerontol Int. 2015;15(8):1013–22.
Acknowledgements
We gratefully thank all staffs of CNHS program and all the participants in Guangdong, Jilin, and Jiangsu provinces. We also thank Li Wang, Li Pan, Yanhong Wang, Yingying Zhu, Xiaoli Zhu, Wenwen Diao for their professional advises and efforts in the fieldwork.
Funding
This work was supported by Research on the Basic Resources of Science and Technology in the Ministry of Science and Technology (2022FY100800), CAMS Innovation Fund for Medical Sciences (2021-I2M-1-023), and State Key Laboratory Special Fund (2060204).
Author information
Authors and Affiliations
Contributions
Study concept and design: SG, HH, and LZ; Acquisition of data: SG, HH, LZ, HY, CX, OQ, LY, XT, TJ, LA, LB, LQ, XT, WW, HH, XD, CZ, and WZ; Analysis and interpretation of data: LZ; Drafting of the manuscript: LZ; Critical revision of the manuscript for important intellectual content: SG and HH. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The Ethical Review Committee of the Institute of Basic Medical Sciences Chinese Academy of Medical Sciences, Beijing, China, has approved this study under the protocol (No. 2022177 and No. 2022134). Written informed consent was obtained from all participants.
Competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Lu, Z., Hu, Y., Chen, X. et al. Sex-specific associations between total and regional Fat-to-muscle Mass ratio and cardiometabolic risk: findings from the China National Health Survey. Nutr J 23, 104 (2024). https://doi.org/10.1186/s12937-024-01007-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12937-024-01007-2