Abstract
Background
Spanish-speakers with non-English language preference and complex medical needs suffer disparities in quality of care, safety, and health outcomes. Communication challenges during prolonged hospitalizations for complex illnesses negatively influence how this group engages in their care and decision-making while hospitalized. Limited literature capturing the perspectives of Spanish-speaking patients in this context exists. Given the impact of language barriers on care and medical decision-making, this study documents the experiences of Spanish-speaking patients with NELP and hospitalized with complex care needs as well as caregivers and community leaders.
Methods
Using community-engaged recruitment strategies and semi-structured interviews and a focus group, we gathered insights from Spanish-speaking patients hospitalized for prolonged periods, caregivers, and community leaders from three geographic regions. Data were deidentified, transcribed, translated, coded in duplicate, and analyzed guided by grounded theory using NVivo.
Results
We interviewed 40 participants: 27 patients, 10 caregivers and 3 community leaders. We identified four major themes: (1) Disconnected experiences impeding interactions, communication, and decision-making (2) Inadequate interpreter services (3) Benefits and consequences of family at the bedside (4) Community -informed recommendations.
Conclusion
The study showed that in-person interpreters were preferred to virtual interpreters; yet interpreter access was suboptimal. This resulted in ad hoc family interpretation. Participants noted language negatively impacted patient’s hospital experience, including decreasing confidence in medical decision-making. Recommendations from patients, caregivers, and community leaders included expanding interpreter access, bolstering interpreter quality and accuracy, and increasing resources for patient education.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
As of 2021, there are over 25 million people with non-English language preference (NELP) in the United States (U.S.) [1]. Of note, NELP is a term that replaces the deficit-centering and ethnocentric label “limited English proficiency” (LEP) to describe an individual who prefers a language other than English in daily life [2]. Throughout this article, we will use “NELP” instead of “LEP” to continue this practice of reorienting language proficiency from a deficit model to a reflection of a person’s social context.
Patients with NELP suffer from an array of disparities, including worse health outcomes, higher rates of hospital readmission, longer hospital length of stay, and higher healthcare resource utilization [3,4,5,6,7]. While patients with NELP are legally entitled access to professional interpretation services [8], there is evidence that U.S. healthcare facilities often lack the resources and personnel to meet the language needs of patients with NELP [9, 10]. There has been a recent surge in literature related to disparities among populations and patients with NELP, including reviews and quantitative studies that examine disparities in numerous hospital settings and medical specialties [4, 5, 11,12,13,14,15,16,17,18].
Spanish-speakers comprise 77% of people with NELP in the U.S. [19]. The Hispanic and Latino community, a predominantly Spanish-speaking group, made up almost one quarter of COVID-19 deaths during the early parts of the pandemic [20], highlighting the disproportionate impact of the pandemic on these communities [21, 22]. Monolingual Spanish-speakers had higher rates of COVID-19 infection, COVID-19 related hospital stays, ICU admission, intubation, and mortality than other Hispanic groups [23, 24]. Those hospitalized with COVID-19, are likely to experience a complex illness, a serious or critical illness that may prompt prolonged hospitalization and presenting challenges in clinical care, medical decision-making, and goals of care conversations [25].
Given that the COVID-19 pandemic resulted in the hospitalization of many exclusively Spanish-speaking patients [24], understanding their experiences during prolonged hospitalization is an important avenue for study. There is considerable evidence that language services were restricted or even curtailed during the COVID-19 pandemic, potentially undermining communication for these individuals, yet few studies have explored this from the patient perspective [26, 27].
Some qualitative studies soliciting the perspectives of patients with NELP have been published but have mainly focused on outpatient settings [28,29,30,31,32]. In addition, there is a lack of qualitative studies that examine the experiences of previously hospitalized Spanish-speaking patients with complex illnesses utilizing community-engaged recruitment methodologies.
Community-engaged research (CER) studies prioritize the community’s needs and interests through robust communication and collaboration between academic institutions and community members [33]. CER can be designed and implemented in numerous ways, including involving the community throughout study design, implementation, dissemination, and solution creation [34]. Community-engagement is vital to health equity advancement because the community holds pertinent insights on the inequities experienced by their own members as well as potential solutions to remediate community mistrust from decades of exploitative research [33].
Our study’s objective was to utilize community-engaged recruitment methods and qualitative research to elicit and elucidate the unique experiences, beliefs, and perceptions of Spanish speakers who had been hospitalized due to complex illnesses, exploring interpreter use during admission, the impact of language barriers on medical decision-making, and the effect of COVID-19 on the hospital experience.
Methods
Study setting and design
The research team conducted a community-engaged, multi-site study between October 2022 and February 2023 in three geographic regions: the Southwest, Southeast, and Midwest of the U.S. We used videoconferencing to conduct virtual focus groups and semi-structured interviews in Spanish. The participants in this study were Spanish-speaking patients, their caregivers (e.g., family, loved ones, friends), and Hispanic leaders within the community. The Mayo Clinic Institutional Review Board approved the protocol (IRB ID: 22-003784). Oral informed consent was obtained from participants at the beginning of the focus groups and interviews.
Participants and recruitment
Inclusion criteria consisted of being 18 years or older and speaking Spanish as a primary language. Patients and caregivers had a recent experience of complex care in any hospital setting with a 10-day or greater stay within the last 3 years. The study also included community leaders, people who held community-based positions (e.g., CEO of safety net clinic, leader of Hispanic community center, religious leader) and had insights and opinions about complex care in hospital settings among Spanish-speaking members of their community.
The study utilized purposive sampling, using numerous recruitment tools. We collaborated with our institutional community engagement staff, attended in-person community events such as Latino heritage celebrations and faith gatherings held in Spanish. The research team also distributed paper and electronic recruitment material such as flyers that intentionally included wording that invited participants with experiences with language barriers and in-patient hospitalization due to complex illness, as well interpreter services, at sites frequented by Hispanic people and our institutions’ patient areas. To identify community leaders, Hispanic study team members leveraged personal and professional social networks, a purposive sampling strategy. We also used other recruitment strategies including electronic record review and portal messaging to identify patients admitted to our institutional hospitals who met inclusion criteria.
Patient and caregiver participants were remunerated with a modest cash incentive. The study did not remunerate community leaders.
Moderator and interview guide
The moderator and interview guide were developed by the multidisciplinary study team, comprised of biomedical ethics and health disparities researchers, an interpreter, physician researchers, and community-based research staff. It included questions based on literature review and the team’s content expertise and experience [27, 35, 36]. The research team explored the impact of language barriers on the hospital experience including communication, health outcomes, and care needs; interpreter access, use and challenges; and decision-making. We also asked about the impact of the COVID-19 pandemic on hospitalization experiences. Community leaders were asked similar question but tailored to evaluate their perspectives about the community. (See Appendix A).
Data collection and analysis
Based on geographical challenges and the ongoing impact of the COVID-19 pandemic on travel and daily life, we used a combination of virtual focus groups and one-on-one semi-structured interviews to offer the greatest accommodation to participants. Participants engaged in only one of the two data collection methods. Three bilingual study team members conducted focus groups and interviews in Spanish that lasted between 15 and 60 min. Interviews were audio-recorded, transcribed, translated and deidentified. When the study reached data saturation, and no new themes were identified, we ceased data collection [37, 38].
Two research team members conducted an initial analysis of transcripts to create a codebook, a framework to highlight common themes amongst participants. Data was analyzed using the codebook informed by grounded theory methodology with open, axial, and selective coding [39]. All data was coded, managed, and analyzed using NVivo Version 13 (Lumivero, Denver, CO) software. All transcripts were coded in duplicate, and coders met weekly to reach thematic consensus on all transcripts, ensuring coder reliability [40, 41]. The codebook was modified and refined during the coding process with the additions of parent and child codes. Coding definitions were progressively clarified during data analysis. Once coding was completed, investigators met to generate consensus on pertinent and representative themes, and to select representative quotes.
Results
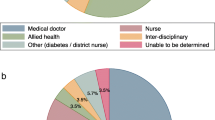
We enrolled 27 patients (PT), 10 caregivers (CG), and 3 community leaders (CL) (n = 40). We conducted 1 focus group and 36 one-on-one interviews. The focus group consisted of four participants, 2 patients and 2 caregivers. Additional demographic data for the focus group and semi-structured interview participants are reported in Table 1. Within our cohort, 90% participated in an interview and only 10% participated in a focus group.
Theme 1: Disconnected experiences impeding interactions, communication and decision-making (table 2)
Spanish-speaking patients described feeling disconnected from the healthcare team. Patients noted that they could not express themselves to healthcare staff and that the language barrier inhibited their understanding of their medical care. Participants also stated that the language barrier stifled their confidence in medical decision-making and ability to express themselves. Participants reported that professional interpreters helped facilitate confident decision-making among patients and caregivers. In response to a lack of professional interpretation services, participants or their clinicians utilized numerous workarounds, including drawings, electronic translation applications, and body gestures.
Theme 2: Inadequate interpreter services (table 3)
Most participants were offered, had access to, and used diverse interpretation modalities while hospitalized. However, some participants noted they were not offered interpreter services. Participants reported a preference for in-person interpretation over other modalities, such as remote video and phone interpretation. Participants noted that professional in-person interpretation facilitated use of body language and gestures, aiding communication. Furthermore, patients felt more comfortable and trusted in-person interpreters resulting in improved rapport building. When requested, however in-person interpretation services were frequently delayed.
Remote video interpretation services were perceived to provide some benefits over in-person interpreters, for example convenience and immediacy. One participant noted a benefit of virtual modalities reduced the risk of pathogenic transmission and supported infection mitigation. However, several participants expressed major concerns about using remote interpretation services including frequent technological and connectivity problems, causing frustration. Furthermore, participants conveyed that virtual interpreters were at times distracted and interpreting in non-professional environments. Consequently, patients and caregivers cited inaccurate and lower quality interpretation. Additionally, many participants noted virtual interpretation was impersonal and “flavorless” citing lack of body language and physical presence, leading to a sense of detachment.
Some participants also noted that elderly patients may not feel comfortable with virtual interpreters. Lastly, participants also expressed privacy concerns with tablet remote interpretation due to challenges with appropriately positioning the camera during patient interactions.
More broadly, community leaders commented that interpretation services use language that does not have a direct translation from English to Spanish. This can cause more confusion for patients and their families. An example a community leader cited was “comfort care”: in which they noted that Spanish-speaking patients might have difficulty comprehending the concept.
Theme 3: Benefits and consequences of family at the bedside (table 4)
Family caregivers were an important part of Spanish-speaking patients’ hospital experiences, with participants citing that family has great importance in the Hispanic community. Many participants relied on family members to interpret important medical information to the healthcare team, especially when a professional interpreter was unavailable or not present. Many caregivers expressed a desire to stay with their hospitalized loved ones and patient participants noted that this decreased feelings of loneliness and anxiety. Furthermore, some participants noted that their family members provided additional clinical care, including changing urinary catheter bags. While family functioned as part of a patient’s support system, our study confirmed that family members also frequently served as interpreters when professional interpretation services were unavailable or delayed. The COVID-19 pandemic visitation restrictions however, impacted the role of family in different ways.
Using family as interpreters introduced challenges for patients and their caregivers. Family members expressed that the additional responsibility can be challenging causing discomfort. Some participants also noted that family members lacked training, adequate health literacy, and sufficient language proficiency to accurately interpret for the patient, creating confusion for the patient and healthcare team. Participants also noted that when family members interpreted frequently, they assumed the additional responsibility of being a designated surrogate decision maker.
Theme 4: Community-informed recommendations (table 5)
When asked to offer recommendations, patient and caregiver participants offered several suggestions, particularly related to professional interpreter accessibility and quality. Overwhelmingly, they wished that hospitals would hire more in-person interpreters to mitigate shortages and delays. They also desired that medical staff become more aware about the need to use and how to access interpreter services. Some participants even recommended that hospitals hire dedicated bilingual health staff to ensure language needs are met.
Patient and caregivers urged interpreters to use accessible language and hospitals to provide additional education and Spanish resources in response to lower health literacy. They advocated for additional training for interpreters regardless of modality, and hospitals to consider accountability measures to bolster the quality of medical interpretation.
In response to conceptually challenging medical terminology, community leaders also recommended that professional interpreters should streamline interpretation and use accessible language. Community leaders encouraged hospitals to provide more education and resources about patients’ rights to free interpreter services, citing patients’ lack of knowledge and awareness.
Regarding decision-making, community leaders encouraged clinicians to employ the teach-back method to ensure patients have a complete understanding of their treatment plans and care more broadly. Community leaders also highlighted the role of professional interpreters in supporting discussions and medical decision-making.
Community leaders recognized that many Spanish-speaking patients worry about the cost of their care, including interpretation services. Therefore, community leader participants recommended that patients connect with community health workers and patient navigators to access resources to ease the burden of care and streamline ongoing care. Finally, community leaders urged patients and health facilities to engage and utilize surrounding community organizations to assist Spanish-speaking patients throughout their hospital experience.
Discussion
This community-engaged qualitative study recruited and highlighted the unique voices of Spanish-speaking community leaders, caregivers, and patients who had been hospitalized for prolonged periods to garner insights about the impact of language barriers on the hospital experience, the use of interpreter services, and the impact of COVID-19. There is limited literature capturing the voices of Spanish-speaking patients and caregivers hospitalized either before or since the start of the COVID-19 pandemic. Most of the existing literature is focused on hospitalized pediatric patients [42,43,44].
Participants noted that sometimes clinicians did not utilize or try to engage interpreters. Participants perceived that interpreter accessibility challenges stemmed from clinicians’ lack of knowledge and training or initiative to request these services for patients and caregivers, as well as a general lack of interpreter availability [10, 45, 46]. Similar findings were noted by Schenker et al. in a cross-sectional study that documented clinician’s frequent underutilization of interpretation services. Other studies have also identified this trend, and some have shown worse patient outcomes related to lack of access [47,48,49,50].
In our study, we found that participants favored in-person interpreters over remote modalities due to perceptions that remote interpretation was impersonal and more prone to inaccuracy. However, existing literature on modality preference demonstrates a variety of findings. A study using survey methodology among Spanish-speaking pediatric patients and their parents noted that parents were more satisfied with in-person than telephone interpreters [51], and a prospective cohort study by Stevens also found that patients exhibited more comfort with an in-person interpreter [52]. A study involving hospital personnel and Spanish-speaking patients documented participants’ perceptions that remote interpretation was detached but warranted in some situations such as emergencies, coinciding with our participants’ perspective that remote interpretation offers immediacy and convenience [53].
Another study evaluating the implementation of video remote interpretation in a metropolitan children’s hospital found that benefits included decreased wait times and that it supplemented in-person interpretation, affirming our study’s participants perception of remote interpretation’s convenience [54]. Although the challenges of remote interpretation, such as connectivity issues, have been previously documented, these can potentially be remedied through education and implementation rounds, suggesting that intentional implementation and troubleshooting may address some challenges faced by patients [54].
However, other studies report no difference in patient satisfaction between in-person and video interpreter modalities [55, 56]. Notably, those studies were conducted before the COVID-19 pandemic and did not focus on the in-patient experience. Given the reduced family visitation and potential for isolation, the desire for in-person connection may have caused a preference for in-person interpreters in our study [57, 58]. Furthermore, our study focuses on patients with complex illness that require challenging conversations that particularly benefit from in-person interpretation [35, 59, 60]. Studies suggest that ICU clinicians support in-person interpreter engagement for complex patients not only for verbatim language interpretation but also cultural brokering and to act as “health literacy guardians”, countering the so-called “Triple threat” [35, 36, 61].
Our study highlights caregiver and family members’ sense of duty to interpret and care for their hospitalized loved ones, citing that a family’s role in one’s care is an integral part of Latino culture. A qualitative study by Pines et al. reported that some patients with NELP prefer family interpretation over professional interpreters in certain situations, such as providing comfort to the patient [62]. Rosenberg et al. also documented that family members felt an obligation to support and interpret for hospitalized loved ones [63]. However clinicians may over-rely on family interpreters [64]. Literature suggests family interpreters act as a supplement to professional interpreters in addition to serving as an advocate and emotional support [63, 65]. In fact, participants in our study articulated concerns about relying on family members whose poor interpretation might lead to miscommunication or even potential harm, a finding not previously documented about patient perspectives. Despite these worries, in response to a lack of available interpreters, patients often relied on family members to interpret when presented with no alternatives.
Other scholars have raised ethical concerns about family interpretation; these include concerns about bias, accuracy, incomplete interpretation of all medical information, and intentional withholding of information that might be perceived to upset their loved one (for example non-disclosure of a poor prognosis or diagnosis) [66,67,68]. These concerns were also identified in a qualitative study assessing physician perception of family interpreters’ skill-level and accuracy [69]. No participants in our study articulated concerns about non-disclosure specifically but clearly some participants voiced concerns about accuracy impeding their care while hospitalized. Notably, although some studies have found Spanish-speaking patients feel like a burden due to their language needs, none of our patient participants expressed this concern [70].
A novel finding of our study is that the role of surrogate decision-maker fell upon the family member who had the most advanced English skills. While no studies, to our knowledge, have documented this family dynamic in medical care, higher quality clinician-family communication results in more confident decision-making [71]. In our study, the primary family interpreter served as a language broker between the healthcare team and family; therefore, this person had the most information to make an informed decision on behalf of the incapacitated patient. This finding raises questions about how clinicians may best initiate conversations about surrogate decision-making among family members and caregivers. In cases where a patient lacks a legally designated durable power of attorney, decision-making authority may be determined by state laws [72]. Clinicians may need to consider how language proficiency may influence who is chosen to have decision-making authority on behalf of the incapacitated patient.
Our study confirmed that language barriers make decision-making more difficult for Spanish-speaking patients. There is limited literature that seeks the perspective of Spanish-speaking patients about language barriers and medical decision-making. A recent multisite cohort study by Piscitello et al. noted an increase in unilateral do not resuscitate orders among Spanish speaking patients during the pandemic which may reflect communication difficulties that impacted decision-making and subsequent care [73]. An additional qualitative study also found that immigrant patients and physicians perceive that the language barrier poses difficulty during shared decision-making [74]. Other studies have also demonstrated the association between language and differences in decision-making [11, 27]. Given that our study focuses on complex patients with prolonged stays and challenging decision making as well as limited interpretation services, these findings are concerning.
Many participants recommended that hospitals should hire more in-person interpreters, echoing previous calls for hospitals to expand interpreter accessibility to address disparities in communication and care [75]. To address shortages and delays within professional interpretation services more broadly, patients and caregivers suggested that hospitals hire English-Spanish bilingual healthcare staff (e.g., physicians, nurses). This finding resonates within the literature. Work by Diamond et al., and a perspective by Knuesel et al., supports language concordant care provided by bilingual clinicians for increased patient satisfaction and improved health outcomes [13, 75,76,77]. Unfortunately, increasing language diversity in medical schools and the medical workforce and hiring sufficient bilingual clinicians may continue to be a challenge [78]. Additionally, there are other concerns in providing Spanish-language concordant care; for example, there are no standardized processes to assess Spanish proficiency or good training for healthcare professionals to provide Spanish-language concordant care [79,80,81,82]. However, potentially in the future health systems will be able to leverage these resources when available to provide optimized care to this vulnerable population. Otherwise, providing consistent professional interpretation services should be the norm in practice, meeting ethical and legal standards [83].
Other approaches to meeting the language needs of patients is to focus on optimizing interpreter services effectiveness and workflows to address barriers in the provision of interpreters [84]. A strategy the research team has developed and are currently testing with a pragmatic clinical trial is using artificial intelligence and informatics to identify patients with NELP and complex care needs to prioritize in-person interpreter use among patients experiencing complicated interventions or having challenging preference-sensitive decision-making. The team has integrated the algorithm into the clinical and interpreter services workflow and provide active outreach to clinicians with a secure chat through the electronic medical record nudging them to use an interpreter. Moreover, this strategy was considered acceptable and helpful to clinicians and other stakeholders [85]. Interim results from this work have shown a 37% increase in interpreter use in our intervention group [86]. Other use of artificial intelligence and machine learning to provide interpretation or translation (written word) require further study and cannot yet be recommended as acceptable modalities [87]. To address shortages of interpreters, career investment programs can train already existing healthcare staff (such as desk or housekeeping staff) to become interpreters in languages the institution may need that are spoken by the local population [88].
Clinicians also need better training about how to effectively work with interpreters as robust and effective training programs are lacking for both trainees and clinicians [89]. When managing patients with NELP and complex care needs we also recommend pre-encounter huddles between clinicians and interpreters prior to the discussion with patients and family. This strategy can increase bidirectional information sharing between interpreters and clinicians and improve the communication and the quality of the patient/family interpreted discussion [90,91,92].
Community leaders provided important insights towards mitigating disparities experienced by Spanish-speaking patients, such as engaging patient navigators and community health workers to educate patients and optimize their care transitions. They also supported hospital collaboration with local Spanish-speaking organizations. Several studies note that patient navigator and community health worker programs contribute to improvement in patient health outcomes [93, 94]. Hospital collaboration with community organizations and faith-based groups have also been shown to improve community health [95,96,97]. Community leader insights as key informants are fundamental for understanding the needs of Spanish-speaking-patients [98, 99]. Patient education and community engagement efforts can reduce readmission rates and hospital care costs, thus beneficial for patients, healthcare staff, and hospital administrators [100]. Additionally, in our study, community leaders noted a need for patients to advocate for themselves by requesting professional interpreter services.
Strengths and limitations
This study has several strengths. We leveraged community-engaged recruitment methodology as an important tool to include the most relevant perspectives in understanding equity issues associated with language barriers, specifically among Spanish speaking patients with complex medical needs. Our qualitative methods using a focus group and semi-structured interviews were conducted in Spanish by bilingual personnel, bridging the language gap between participants and English-centric research. Qualitative studies can deeply characterize the experiences of participants by utilizing a holistic perspective to explore phenomena [101, 102]. Additionally, the purpose of qualitative methods is to understand the meaning of participants’ perspectives and the context surrounding them [102]. We were able to conduct the study across multiple sites in three regions. We used robust data analysis approaches and triangulated our data by interviewing diverse groups (patients, caregivers, community leaders). These measures bolstered the study’s scientific rigor and validity and ensured the trustworthiness of our findings and strengthened the relevance of the discoveries [103].
This study also has some limitations. Firstly, we had initially planned to conduct focus groups for data collection, but scheduling challenges and a substantial proportion of no-shows compelled us to switch to one-on-one semi structured interviews to ensure consistent data collection [104]. The advantage of one-on-one semi-structured interviews is that they may foster a more comfortable environment for the participant, facilitating more dialogue between the interviewer and the interviewee however focus groups can foster interactive dialogue between participants [104]. Many participants were patients within our health system, an institution that tends to have more robust patient resources, although some were hospitalized in other institutions. Therefore, some findings may not be generalizable to other institutions and settings [105]. As with similar studies, this study may be prone to selection bias with those having strong opinions or an affinity with this topic agreeing to be involved. Although, the interview guide included questions about COVD-19 experiences, participants did not provide many perspectives on this, despite prompting. It is important to note that disentangling the contribution of poor language proficiency and low health literacy is sometimes challenging particularly with complex illnesses that may require complicated interventions however the focus of this study was intentionally language barriers [106, 107].
Further directions
Spanish is the most common language spoken in the United States after English [108] and much of the literature surrounding language barriers describes languages frequently spoken throughout the U.S., such as Spanish, Mandarin, Vietnamese and others [109]. However, future work is needed to understand the experiences of patients who speak languages of lesser diffusion such as indigenous Central American languages and Karen, a group of languages spoken in Myanmar [110, 111]. The development of guidelines for bilingual clinicians when interacting with patients is needed as well as metrics to evaluate clinician proficiency. Additionally, while inclusion of non-English speaking participants is especially important in research at the intersection of health and language, generally, research in all disciplines can benefit from inclusion of non-English participants. Increased protections for vulnerable populations (e.g., incarcerated people, pregnant people) is necessary to prevent exploitative research; however, these protections can also be a deterrent to conduct research with these populations. Further work is needed to provide guidance on how to include participants from disenfranchised backgrounds that prevents exploitation but facilitates more inclusive research opportunities and can make research more generalizable [112]. If legal and ethical imperatives are not sufficient for institutions to provide access to language services, the economic benefits may be. Work examining the costs of providing interpreter services in diverse settings is needed to demonstrate how optimizing communication can positively impact length of stay, healthcare utilization and other measures as well as patient satisfaction [113,114,115,116,117].
Conclusion
This qualitative study that utilized community-engaged recruitment strategies sought to deeply characterize the hospital experience of Spanish-speaking patients with NELP and complex health needs. This vulnerable patient group were more prone to poor communication with their healthcare team, resulting in some distress and challenges during medical decision-making. If access to professional interpretation services occurred, it was usually remote video interpretation and participants often found the interpretation to be inaccurate and low-quality. Many participants relied on family members for interpretation, care, and support. Recommendations for hospitals from participants included expanding in-person interpreter accessibility, training bilingual clinicians, enhancing remote interpretation quality, and developing resources towards patient education.
Data availability
Availability of Data and Materials: The datasets used and analyzed in this study are available from the corresponding author on reasonable request.
Abbreviations
- LEP:
-
Limited English Proficiency
- NELP:
-
Non-English Language Preference
- U.S.:
-
United States
- CER:
-
Community-Engaged Research
References
Language and Education. Migration Policy Institute; [https://www.migrationpolicy.org/data/state-profiles/state/language/US#
Ortega P, Shin TM, Martínez GA. Rethinking the term Limited English proficiency to Improve Language-Appropriate Healthcare for all. J Immigr Minor Health. 2022;24(3):799–805.
Rawal S, Srighanthan J, Vasantharoopan A, Hu H, Tomlinson G, Cheung AM. Association between Limited English proficiency and revisits and readmissions after hospitalization for patients with Acute and Chronic conditions in Toronto, Ontario, Canada. JAMA. 2019;322(16):1605–7.
John-Baptiste A, Naglie G, Tomlinson G, Alibhai SMH, Etchells E, Cheung A, et al. The effect of English language proficiency on length of stay and in-hospital mortality. J Gen Intern Med. 2004;19(3):221–8.
Karliner LS, Kim SE, Meltzer DO, Auerbach AD. Influence of language barriers on outcomes of hospital care for general medicine inpatients. J Hosp Med. 2010;5(5):276–82.
Hampers LC, Cha S, Gutglass DJ, Binns HJ, Krug SE. Language barriers and resource utilization in a pediatric emergency department. Pediatrics. 1999;103(6 Pt 1):1253–6.
Cheng EM, Chen A, Cunningham W. Primary Language and Receipt of Recommended Health Care among hispanics in the United States. J Gen Intern Med. 2007;22(2):283–8.
Section 1557: Ensuring Meaningful Access for Individuals with Limited English Proficiency Civil Rights. U.S. Department of Health & Human Services; [https://www.hhs.gov/sites/default/files/1557-fs-lep-508.pdf
Green AR, Nze C. Language-based inequity in Health Care: who is the poor historian? AMA J Ethics. 2017;19(3):263–71.
Schenker Y, Pérez-Stable EJ, Nickleach D, Karliner LS. Patterns of interpreter use for hospitalized patients with limited English proficiency. J Gen Intern Med. 2011;26(7):712–7.
Barwise A, Jaramillo C, Novotny P, Wieland ML, Thongprayoon C, Gajic O, et al. Differences in Code Status and End-of-life decision making in patients with Limited English proficiency in the Intensive Care Unit. Mayo Clin Proc. 2018;93(9):1271–81.
Berdahl TA, Kirby JB. Patient-provider communication disparities by Limited English proficiency (LEP): Trends from the US Medical Expenditure Panel Survey, 2006–2015. J Gen Intern Med. 2019;34(8):1434–40.
Diamond L, Izquierdo K, Canfield D, Matsoukas K, Gany F. A systematic review of the impact of patient–physician Non-english Language Concordance on Quality of Care and outcomes. J Gen Intern Med. 2019;34(8):1591–606.
Eneriz-Wiemer M, Sanders LM, Barr DA, Mendoza FS. Parental limited English proficiency and health outcomes for children with special health care needs: a systematic review. Acad Pediatr. 2014;14(2):128–36.
Hampers LC, Cha S, Gutglass DJ, Binns HJ, Krug SE. Language barriers and Resource utilization in a Pediatric Emergency Department. Pediatrics. 1999;103(6):1253–6.
Schenker Y, Karter AJ, Schillinger D, Warton EM, Adler NE, Moffet HH, et al. The impact of limited English proficiency and physician language concordance on reports of clinical interactions among patients with diabetes: the DISTANCE study. Patient Educ Couns. 2010;81(2):222–8.
van Rosse F, de Bruijne M, Suurmond J, Essink-Bot ML, Wagner C. Language barriers and patient safety risks in hospital care. A mixed methods study. Int J Nurs Stud. 2016;54:45–53.
Chipman SA, Meagher K, Barwise AK. A Public Health Ethics Framework for Populations with Limited English proficiency. Am J Bioeth. 2023:1–16.
Whatley M, Batalova J. Limited English Proficient Population of the United States in 2011. Migration Policy Inst; 2013 07/25/2013.
Andrasfay T, Goldman N. Reductions in 2020 US life expectancy due to COVID-19 and the disproportionate impact on the Black and latino populations. Proc Natl Acad Sci U S A. 2021;118(5).
Ayala IN, Garcia-Mendez JP, Tekin A, Malinchoc M, Barwise AK. Association between Ethnicity and mortality outcomes in patients with COVID-19: a Mayo Clinic VIRUS Registry Cohort Study. J Racial Ethn Health Disparities. 2024.
Barwise A, Tekin A, Domecq Garces JP, Gajic O, Pickering BW, Malinchoc M. Impact of SARS-CoV-2 Vaccine Rollout on Hispanic and non-hispanic admission and mortality trends: an interrupted Time Series Analysis. Chest. 2023.
Rodriguez-Diaz CE, Guilamo-Ramos V, Mena L, Hall E, Honermann B, Crowley JS, et al. Risk for COVID-19 infection and death among latinos in the United States: examining heterogeneity in transmission dynamics. Ann Epidemiol. 2020;52:46–e532.
Lopez S, Longcoy J, Avery E, Isgor Z, Jeevananthan A, Perez J et al. The impact of Language on Hospital outcomes for COVID-19 patients: a study of Non-english speaking hispanic patients. J Racial Ethn Health Disparities. 2023:1–7.
Roberts CM, Levi M, McKee M, Schilling R, Lim WS, Grocott MPW. COVID-19: a complex multisystem disorder. Br J Anaesth. 2020;125(3):238–42.
Barwise A, Balls-Berry J, Soleimani J, Karki B, Barrett B, Castillo K, et al. Interventions for end of life decision making for patients with Limited English proficiency. J Immigr Minor Health. 2020;22(4):860–72.
Barwise AK, Nyquist CA, Espinoza Suarez NR, Jaramillo C, Thorsteinsdottir B, Gajic O, et al. End-of-life decision-making for ICU patients with Limited English proficiency: a qualitative study of Healthcare Team insights. Crit Care Med. 2019;47(10):1380–7.
Villalona S, Castañeda H, Wilson JW, Romero-Daza N, Yanez Yuncosa M, Jeannot C. Discordance between satisfaction and health literacy among spanish-speaking patients with Limited English-Proficiency seeking Emergency Department Care. Hisp Health Care Int. 2023;21(2):60–7.
Xiong P, Lor M, Park LS, Jacobs EA. How patients with Limited English proficiency make Health Care decisions: Hmong patients’ perspectives. WMJ. 2023;122(3):178–83.
Squires A, Gerchow L, Ma C, Liang E, Trachtenberg M, Miner S. A multi-language qualitative study of limited English proficiency patient experiences in the United States. PEC Innov. 2023;2:100177.
Yeheskel A, Rawal S. Exploring the ‘Patient experience’ of individuals with Limited English proficiency: a scoping review. J Immigr Minor Health. 2019;21(4):853–78.
Hadziabdic E, Hjelm K. Arabic-speaking migrants’ experiences of the use of interpreters in healthcare: a qualitative explorative study. Int J Equity Health. 2014;13(1):49.
Wolff M, Maurana CA. Building Effective Community—Academic partnerships to Improve Health: a qualitative study of perspectives from communities. Acad Med. 2001;76(2).
Payán DD, Zawadzki MJ, Song AV. Advancing community-engaged research to promote health equity: considerations to improve the field. Perspect Public Health. 2022;142(3):139–41.
Suarez NRE, Urtecho M, Jubran S, Yeow ME, Wilson ME, Boehmer KR, et al. The roles of medical interpreters in intensive care unit communication: a qualitative study. Patient Educ Couns. 2021;104(5):1100–8.
Espinoza Suarez NR, Urtecho M, Nyquist CA, Jaramillo C, Yeow ME, Thorsteinsdottir B, et al. Consequences of suboptimal communication for patients with limited English proficiency in the intensive care unit and suggestions for a way forward: a qualitative study of healthcare team perceptions. J Crit Care. 2021;61:247–51.
Francis JJ, Johnston M, Robertson C, Glidewell L, Entwistle V, Eccles MP, et al. What is an adequate sample size? Operationalising data saturation for theory-based interview studies. Psychol Health. 2010;25(10):1229–45.
Saunders B, Sim J, Kingstone T, Baker S, Waterfield J, Bartlam B, et al. Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quant. 2018;52(4):1893–907.
Corbin J, Strauss A. Basics of qualitative research. SAGE; 2015.
O’Connor C, Joffe H. Intercoder Reliability in Qualitative Research: debates and practical guidelines. Int J Qualitative Methods. 2020;19:1609406919899220.
MacQueen KM, McLellan E, Kay K, Milstein B. Codebook Development for Team-based qualitative analysis. CAM J. 1998;10(2):31–6.
Tam I, Gist L, Patel A, Fisher E, Rhee KE. The parent’s perspective: a Focus Group Study on Spanish Interpreter Services for Hospitalized Children. Acad Pediatr. 2022;22(1):98–106.
Stephen JM, Zoucha R, Cazzell M, Devido J. Cultural care needs of Spanish speaking parents with limited English proficiency whose children are hospitalized: an ethnonursing study. J Pediatr Nurs. 2023;69:62–70.
Batton E, Hurst S, Ramos C, Catalan L, Freeman M, Marc-Aurele K. Communication in the neonatal ICU for Spanish speaking parents: a qualitative interview study. BMC Pediatr. 2023;23(1):481.
Aitken G. Medical students as certified interpreters. AMA J Ethics. 2019;21(3):E232–8.
Dwyer J. Babel, justice, and democracy: reflections on a shortage of interpreters at a public hospital. Hastings Cent Rep. 2001;31(2):31–6.
Jimal D, Chaplin T, Walker M. Interpretation Services in a Canadian Emergency Department: how often are they utilized for patients with Limited English. Proficiency? Cureus. 2022;14(12):e32288.
Tang AS, Kruger JF, Quan J, Fernandez A. From admission to discharge: patterns of interpreter use among resident physicians caring for hospitalized patients with limited English proficiency. J Health Care Poor Underserved. 2014;25(4):1784–98.
Jensen JL, Sweeney A, Gill C, Mahtani R, Teal EN, Stuebe AM, et al. Evaluation of Patient Access to Spanish-Language-Concordant Care on a Postpartum Unit. Nurs Womens Health. 2022;26(6):429–38.
Flores G. The impact of medical interpreter services on the quality of health care: a systematic review. Med Care Res Rev. 2005;62(3):255–99.
Garcia EA, Roy LC, Okada PJ, Perkins SD, Wiebe RA. A comparison of the influence of Hospital-Trained, Ad Hoc, and Telephone interpreters on Perceived satisfaction of Limited English-Proficient Parents presenting to a Pediatric Emergency Department. Pediatr Emerg Care. 2004;20(6).
Stevens L, Mitchell P, Vasquez J, Lopez G, Gutierrez A, McGrath M. 384 spanish-speaking patient satisfaction with interpreter services in the emergency department: comparison of in-person versus live-feed video interpretation. Ann Emerg Med. 2011;58(4):S308.
Feiring E, Westdahl S. Factors influencing the use of video interpretation compared to in-person interpretation in hospitals: a qualitative study. BMC Health Serv Res. 2020;20(1):856.
Marshall LC, Zaki A, Duarte M, Nicolas A, Roan J, Colby AF, et al. Promoting Effective Communication with Limited English proficient families: implementation of Video Remote Interpreting as Part of a Comprehensive Language Services Program in a children’s hospital. Joint Comm J Qual Patient Saf. 2019;45(7):509–16.
Joseph C, Garruba M, Melder A. Patient satisfaction of telephone or video interpreter services compared with in-person services: a systematic review. Aust Health Rev. 2018;42(2):168–77.
Locatis C, Williamson D, Gould-Kabler C, Zone-Smith L, Detzler I, Roberson J, et al. Comparing In-Person, video, and Telephonic Medical Interpretation. J Gen Intern Med. 2010;25(4):345–50.
Hart JL, Turnbull AE, Oppenheim IM, Courtright KR. Family-centered care during the COVID-19 era. J Pain Symptom Manage. 2020;60(2):e93–7.
Moss SJ, Krewulak KD, Stelfox HT, Ahmed SB, Anglin MC, Bagshaw SM, et al. Restricted visitation policies in acute care settings during the COVID-19 pandemic: a scoping review. Crit Care. 2021;25(1):347.
Silva MD, Adelman RD, Singh V, Gupta R, Moxley J, Sobota RM, et al. Healthcare Provider perspectives regarding Use of Medical interpreters during End-of-life conversations with Limited English Proficient patients. Am J Hosp Palliat Care. 2022;39(2):220–7.
Schwei RJ, Schroeder M, Ejebe I, Lor M, Park L, Xiong P, et al. Limited English proficient patients’ perceptions of when interpreters are needed and how the decision to utilize interpreters is made. Health Commun. 2018;33(12):1503–8.
Schyve PM. Language differences as a barrier to quality and safety in health care: the Joint Commission perspective. J Gen Intern Med. 2007;22(Suppl 2):360–1.
Pines RL, Jones L, Sheeran N. Using Family members as Medical interpreters: an explanation of Healthcare Practitioners’ normative practices in Pediatric and neonatal departments in Australia. Health Commun. 2020;35(7):902–9.
Rosenberg E, Seller R, Leanza Y. Through interpreters’ eyes: comparing roles of professional and family interpreters. Patient Educ Couns. 2008;70(1):87–93.
Gray B, Hilder J, Donaldson H. Why do we not use trained interpreters for all patients with limited English proficiency? Is there a place for using family members? Aust J Prim Health. 2011;17(3):240–9.
Hadziabdic E, Albin B, Heikkila K, Hjelm K. Family members’ experiences of the use of interpreters in healthcare. Prim Health care Res Dev. 2014;15(2):156–69.
Ho A. Using family members as interpreters in the clinical setting. J Clin Ethics. 2008;19(3):223–33.
Blanchard J. Who decides, patient or family? AMA J Ethics. 2007;9(8):537–42.
White J, Plompen T, Osadnik C, Tao L, Micallef E, Haines T. The experience of interpreter access and language discordant clinical encounters in Australian health care: a mixed methods exploration. Int J Equity Health. 2018;17(1):151.
Rosenberg E, Leanza Y, Seller R. Doctor-patient communication in primary care with an interpreter: physician perceptions of professional and family interpreters. Patient Educ Couns. 2007;67(3):286–92.
Steinberg EM, Valenzuela-Araujo D, Zickafoose JS, Kieffer E, DeCamp LR. The battle of managing language barriers in health care. Clin Pediatr. 2016;55(14):1318–27.
Majesko A, Hong SY, Weissfeld L, White DB. Identifying family members who may struggle in the role of surrogate decision maker. Crit Care Med. 2012;40(8):2281–6.
DeMartino Erin S, Dudzinski David M, Doyle Cavan K, Sperry Beau P, Gregory Sarah E, Siegler M et al. Who decides when a patient can’t? Statutes on alternate decision makers. N Engl J Med.376(15):1478–82.
Piscitello GM, Tyker A, Schenker Y, Arnold RM, Siegler M, Parker WF. Disparities in unilateral do not resuscitate Order Use during the COVID-19 pandemic. Crit Care Med 9900.
Suurmond J, Seeleman C. Shared decision-making in an intercultural context: barriers in the interaction between physicians and immigrant patients. Patient Educ Couns. 2006;60(2):253–9.
Herzberg EM, Barrero-Castillero A, Matute JD. The healing power of language: caring for patients with limited English proficiency and COVID-19. Pediatr Res. 2022;91(3):526–8.
Knuesel S, Chuang W, Olson E, Betancourt J. Language barriers, equity, and COVID-19: the impact of a novel Spanish language care group. J Hosp Med. 2021;16(2):109–11.
Gershengorn HB, Patel S, Mallow CM, Falise J, Sosa MA, Parekh DJ, et al. Association of language concordance and restraint use in adults receiving mechanical ventilation. Intensive Care Med. 2023;49(12):1489–98.
Barr DA, Gonzalez ME, Wanat SF. The Leaky Pipeline: factors Associated with early decline in interest in Premedical studies among underrepresented minority undergraduate students. Acad Med. 2008;83(5).
Ortega P. Spanish Language Concordance in U.S. Medical Care: a multifaceted challenge and call to action. Acad Med. 2018;93(9).
Fernández A, Pérez-Stable EJ. ¿Doctor, habla español? Increasing the Supply and Quality of Language-Concordant Physicians for Spanish-speaking patients. J Gen Intern Med. 2015;30(10):1394–6.
Andres E, Wynia M, Regenstein M, Maul L. Should I call an interpreter?-How do physicians with second language skills decide? J Health Care Poor Underserved. 2013;24(2):525–39.
Lion KC, Thompson DA, Cowden JD, Michel E, Rafton SA, Hamdy RF, et al. Clinical Spanish use and language proficiency testing among pediatric residents. Acad Med. 2013;88(10):1478–84.
Gray B, Hilder J. The ethics of interpreter use. Clin Ethics. 2021;16(4):354–8.
Ahmed A, Frohn E. A predictive and prescriptive analytical framework for scheduling language medical interpreters. Health Care Manag Sci. 2021;24(3):531–50.
Barwise AK, Curtis S, Diedrich DA, Pickering BW. Using artificial intelligence to promote equitable care for inpatients with language barriers and complex medical needs: clinical stakeholder perspectives. J Am Med Inf Assoc. 2024;31(3):611–21.
Strechen I, Wilson P, Eltalhi T, Piche K, Herasevich S, Tiong I, et al. Interim results from a stepped Wedge Cluster Randomized Trial using Artificial Intelligence to increase interpreter use for patients with Language barriers. C103 disparities social determinants health pulmonary crit care sleep med. 2024; American Thoracic Society International Conference Abstracts(American Thoracic Society):A6730–A.
Bakdash L, Abid A, Gourisankar A, Henry TL. Chatting beyond ChatGPT: advancing Equity through AI-Driven Language Interpretation. J Gen Intern Med. 2024;39(3):492–5.
Wilkes RC, Bartley SJ. A model for career planning in healthcare: investing in a career development program will retain workers for growth. Online J Workforce Educ Dev. 2007;2(3):3.
Fukui N, Partain DK, Yeow ME, Farfour HN, Prokop L, Barwise A. Learning to collaborate with medical interpreters in health professions education: a systematic review of training programs. Med Teach. 2024;46(2):258–72.
Norris WM, Wenrich MD, Nielsen EL, Treece PD, Jackson JC, Curtis JR. Communication about end-of-life care between language-discordant patients and clinicians: insights from medical interpreters. J Palliat Med. 2005;8(5):1016–24.
Betancourt JR, Renfrew MR, Green AR, Lopez L, Wasserman M. Improving Patient Safety Systems for Patients With Limited English Proficiency: A Guide for Hospitals: Agency for Healthcare Research and Quality; 2012 [https://www.ahrq.gov/sites/default/files/publications/files/lepguide.pdf
Barwise A, Yeow ME, Partain DK. The Premise and Development of CHECK IN-Check-In for Exchange of Clinical and Key Information to Enhance Palliative Care discussions for patients with Limited English proficiency. Am J Hosp Palliat Care. 2021;38(6):533–8.
Norris SL, Chowdhury FM, Van Le K, Horsley T, Brownstein JN, Zhang X, et al. Effectiveness of community health workers in the care of persons with diabetes. Diabet Med. 2006;23(5):544–56.
Natale-Pereira A, Enard KR, Nevarez L, Jones LA. The role of patient navigators in eliminating health disparities. Cancer. 2011;117(S15):3541–50.
Hamadi HY, Zhao M, Park S, Xu J, Haley DR, Lox C, et al. Improving Health and Addressing Social Determinants of Health through Hospital Partnerships. Popul Health Manag. 2023;26(2):121–7.
Hilts KE, Yeager VA, Gibson PJ, Halverson PK, Blackburn J, Menachemi N. Hospital Partnerships for Population Health: a systematic review of the literature. J Healthc Manag. 2021;66(3):170–98.
Michener L, Aguilar-Gaxiola S, Alberti PM, Castaneda MJ, Castrucci BC, Harrison LM, et al. Engaging with communities - lessons (re)learned from COVID-19. Prev Chronic Dis. 2020;17:E65.
Huang L, Cleveland T, Clift K, Egginton JS, Pacheco-Spann L, Johnson MG, et al. Key stakeholder perspectives of Community Engagement efforts and the impact of the Covid-19 pandemic. J Prim Care Community Health. 2022;13:21501319221133076.
Faifua D. The key informant technique in qualitative research. Sage; 2014.
Kripalani S, Theobald CN, Anctil B, Vasilevskis EE. Reducing Hospital Readmission Rates: current strategies and future directions. Annu Rev Med. 2014;65(1):471–85.
Black N. Why we need qualitative research. J Epidemiol Community Health. 1994;48(5):425–6.
Maxwell J, The, SAGE Handbook of Applied Social Research Methods. 2009 2023/11/27. Thousand Oaks Thousand Oaks, California: SAGE Publications, Inc. 2. https://methods.sagepub.com/book/the-sage-handbook-of-applied-social-research-methods-2e
Varpio L, Ajjawi R, Monrouxe LV, O’Brien BC, Rees CE. Shedding the cobra effect: problematising thematic emergence, triangulation, saturation and member checking. Med Educ. 2017;51(1):40–50.
Baillie L. Exchanging focus groups for individual interviews when collecting qualitative data. Nurse Res. 2019.
Rahman M. The advantages and disadvantages of using qualitative and quantitative approaches and methods in Language Testing and Assessment Research: A literature review. J Educ Learn. 2016;6:102.
Singleton K, Krause EM. Understanding cultural and linguistic barriers to health literacy. Ky Nurse. 2010;58(4):4.
Sentell T, Braun KL. Low health literacy, limited English proficiency, and health status in asians, latinos, and other racial/ethnic groups in California. J Health Commun. 2012;17(Suppl 3):82–99.
Batalova JZ. Jie. Language Diversity and English proficiency in the United States. Migration Policy Institute; 2016.
Twersky SE, Jefferson R, Garcia-Ortiz L, Williams E, Pina C. The Impact of Limited English proficiency on Healthcare Access and outcomes in the U.S.: a scoping review. Healthc (Basel). 2024;12(3).
Gany F, Gonzalez CJ, Schutzman EZ, Pelto D. Engaging the Community To Develop Solutions for languages of Lesser Diffusion. 2016. p. 149–69.
Whyatt B, Pavlović N. Translating languages of low diffusion: current and future avenues. Interpreter Translator Train. 2021;15.
Barwise AK, Allyse MA, Hirsch JR, McGowan ML, Meaghar KM, Riggan KA. Wither vulnerability? The Over/Under Protection Dilemma and Research Equity. Am J Bioeth. 2023;23(6):113–6.
Khoong EC, Fernandez A. Addressing gaps in interpreter use: time for implementation Science Informed Multi-level interventions. J Gen Intern Med. 2021;36(11):3532–6.
Jacobs EA, Sadowski LS, Rathouz PJ. The impact of an enhanced interpreter service intervention on hospital costs and patient satisfaction. J Gen Intern Med. 2007;22(Suppl 2):306–11.
Zhang B, Wright AA, Huskamp HA, Nilsson ME, Maciejewski ML, Earle CC, et al. Health care costs in the last week of life: associations with end-of-life conversations. Arch Intern Med. 2009;169(5):480–8.
Jacobs EA, Leos GS, Rathouz PJ, Fu P Jr. Shared networks of interpreter services, at relatively low cost, can help providers serve patients with limited English skills. Health Aff (Millwood). 2011;30(10):1930–8.
Brandl EJ, Schreiter S, Schouler-Ocak M. Are trained Medical interpreters Worth the cost? A review of the current literature on cost and cost-effectiveness. J Immigr Minor Health. 2020;22(1):175–81.
Acknowledgements
Acknowledgement: This work was supported by a grant from the Mayo Clinic Center for Health Equity and Community Engaged Research. The authors thank the staff of Center for Health Equity and Community Engaged Research in Arizona and Florida for their supportive role in participant recruitment.
Funding
This article was supported by an internal grant from the Mayo Clinic Center for Health Equity and Community Engagement Research.
Author information
Authors and Affiliations
Contributions
Author Contributions: Amelia K. Barwise, Megan A. Allyse, Laura M. Pacheco-Spann, Maria Graciela D. Capetillio Porraz, Maria A. Caruso, Andres H. Guillen Lozoya, and Nicholas V. Nguyen contributed to the study conception and design. Data collection was performed by Andres H. Guillen Lozoya, Maria A. Caruso, and Maria Graciela D. Capetillo Porraz. Data analysis was performed by Nicholas V. Nguyen and Amelia K. Barwise. The first draft of the manuscript was written by Nicholas V. Nguyen and Amelia K. Barwise, and all authors commented on previous versions of the manuscript. Amelia K. Barwise, Megan A. Allyse, Laura M. Pacheco-Spann, Maria Graciela D. Capetillio Porraz, Maria A. Caruso, Andres H. Guillen Lozoya, and Nicholas V. Nguyen read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This research study was approved by the Mayo Clinic Institutional Review Board (IRB ID: 22-003784). Participants orally consented to take part in this research study.
Consent for publication
Participants consented to their data to be published.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix A: Moderator/Interview script for patients, loved ones, caregivers and community leaders
Appendix A: Moderator/Interview script for patients, loved ones, caregivers and community leaders
Patients, Loved Ones, and Caregivers
Brief Introduction:
Greetings, and thank you for your participation in our research study to better understand complex care among Spanish-speaking communities.
Your participation will take around 60 min and at any time you can decline to answer a question or participate in a portion of the focus group. We will be recording our conversation. However, you may remain anonymous if you choose and we will keep any identifying information about you completely confidential.
We will divide the session in topics such as hospital experience, decision-making, needs, interpretation, and covid. If you agree and do not have further questions, we will start the session. We ask that you please refrain from using first and last names of any patients, family members, caregivers, and/or the name of any medical facility. This will help us ensure that we don’t capture identifying information in today’s recorded discussion.
Questions:
-
Hospital Experience.
Today we’re going to be talking about what it is like to spend time in the hospital when you have a language barrier and are very sick.
We are trying to make sure everyone has the best experience and gets the best care possible. Some reasons someone might be in the hospital would be if they got very sick and had to go to intensive care, or if they had a surgery, or some other medical condition that meant they had to spend more than two weeks in the hospital.
-
Has anyone had experience with being in the hospital or having a family member in the hospital?
-
Yes/No.
-
Can you tell me about that experience?
-
If you haven’t had a family member in the hospital, maybe you have friends or community members who you’ve heard from?
-
What kinds of things were they in the hospital for and how did things go?
-
How do you think language barriers affect the hospital experience?
-
Do you have suggestions for how the experience could be improved for those with language barriers?
-
Any barriers for doing this or things that might help?
-
Decision-making.
Prompts: For example, having to decide about being resuscitated, going on a breathing machine, having the palliative care team review the case, needing to make a decision about stopping a treatment that was not helping.
-
What types of decision did you or your loved ones need to make?
-
How did you make those decisions?
-
Do language barriers make the process harder?
-
Do you have suggestions about how that could be improved? Any barriers for doing this or things that might help?
-
Needs.
-
What types of needs were well met?
-
What types of needs were not well met?
-
Do you have suggestions about how that could be improved? Any barriers for doing this or things that might help?
-
-
Interpretation.
-
Did you or your loved one use an interpreter in the hospital?
-
It might have been a telephone, video or in-person interpreter? What was that like?
-
Did you find it helped you with communication with the healthcare team?
-
Either to share your concerns or questions or to better understand what the healthcare team were saying?
-
Do you have suggestions about how that could be improved? Any barriers for doing this or things that might help?
-
Do you have a preference for how you like interpretation done or how you like to get interpreter services?
-
Can you share your thoughts about why you think that?
-
-
Interpretation Pre-COVID.
-
Did you or your loved one ever have an interpreter before COVID when you were hospitalized?
-
Did you find any differences with how interpreter services were provided?
-
Community Leaders
Brief Introduction.
Greetings, and thank you for your participation in our research study to better understand complex care among Spanish-speaking communities.
Your participation will take around 60 min and at any time you can decline to answer a question or participate in a portion of the focus group. We will be recording our conversation. However, you may remain anonymous if you choose and we will keep any identifying information about you completely confidential. We will divide the session in topics such as hospital experience, decision-making, needs, interpretation, and covid. If you agree and don’t have further questions, we will start the session. We ask that you please refrain from using first and last names of any patients, family members, caregivers, and/or the name of any medical facility. This will help us ensure that we don’t capture identifying information in today’s recorded discussion.
-
Hospital Experience.
-
Has anyone had experience with being in the hospital or having a family member in the hospital?
-
Yes/No.
-
Can you tell me about that experience?
-
If you haven’t had a family member in the hospital, maybe you have friends or community members who you’ve heard from?
-
What kinds of things were they in the hospital for and how did things go?
-
How do you think language barriers affect the hospital experience?
-
Do you have suggestions for how the experience could be improved for those with language barriers?
-
Any barriers for doing this or things that might help?
-
-
Decision-making.
Prompts: For example, having to decide about being resuscitated, going on a breathing machine, having the palliative care team review the case, needing to make a decision about stopping a treatment that was not helping.
Prompts: For example, by children/parents, siblings, chaplains, close family friends, spouses or partners or someone else?
-
How do you think those decisions are made?
-
Do patients who are able get involved in that decision? Do they ask family members to make decisions for them?
-
Do language barriers make the process harder?
-
Do you have suggestions about how that could be improved? Any barriers for doing this or things that might help?
-
Needs.
-
What types of patient needs are well met?
-
What types of patient needs are not well met?
-
Do you have suggestions about how that could be improved? Any barriers for doing this or things that might help?
-
-
Interpretation.
-
What do you know and think about interpreter services in hospitals?
-
It might be a telephone, video or in-person interpreter. What are your thoughts about these modes of interpreting?
-
Do you think professional interpretation is helpful to improve communication with the healthcare team?
-
Either to share concerns or questions or to better understand what the healthcare team are saying?
-
Do you think the interpreter or interpreter services can help with discussions of all options, outcomes, treatments, explain things clearly, and are able to share patient and family questions and concerns with the healthcare team?
-
Do you have suggestions about how interpreter services could be improved? Any barriers for doing this or things that might help?
-
-
Interpretation Pre-COVID.
-
Have you heard anything from community members about how interpreter services were provided during COVID-19?
-
Do you know how much or whether this changed much during the pandemic compared to pre-COVID?
-
Do you think there were any differences with how interpreter services were provided?
-
Any thoughts about this including how it affected patients and loved ones?
-
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Nguyen, N.V., Guillen Lozoya, A.H., Caruso, M.A. et al. Through the eyes of Spanish-speaking patients, caregivers, and community leaders: a qualitative study on the in-patient hospital experience. Int J Equity Health 23, 164 (2024). https://doi.org/10.1186/s12939-024-02246-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12939-024-02246-9