Abstract
Background
Research on the effect of pesticide exposure on health has been largely focused on occupational settings. Few reviews have synthesized the associations between dietary pesticide exposure and health outcomes in non-occupationally exposed adults.
Objective
We aim to summarize the evidence regarding dietary pesticide exposure and non-communicable diseases (NCD) in adults, using a systematic review of prospective studies.
Methods
Electronic and manual searches were performed until July 2023. The inclusion criteria were the following: 1) adults aged ≥ 18years, 2) (non)-randomized trials, prospective cohort studies, 3) dietary exposure to pesticides. A bias analysis was carried out using the Nutrition Evidence Systematic Review guidelines based on the Cochrane ROBINS-I.
Results
A total of 52 studies were retrieved and 6 studies that met the above criteria were included. Studies were conducted either in France or in the United States. The studies investigated the risk of cancer (n = 3), diabetes (n = 1), cardiovascular diseases (n = 1), and mortality (n = 1). The quality of the studies varied with overall grades derived from the bias analysis ranging from low to moderate bias. The level of evidence was estimated as low for the risk of cancer while the grading was not assignable for other outcomes, as only one study per outcome was available.
Conclusions
Although further research is warranted to examine more in depth the relationships between low-dose chronic exposure to pesticides through diet and NCD outcomes in non-occupationally-exposed adults, studies suggest a possible role of exposure to dietary pesticide on health. Standardized methodological guidelines should also be proposed to allow for comparison across studies.
Similar content being viewed by others
Introduction
Cancer, diabetes, cardiovascular and chronic respiratory diseases are non-communicable diseases (NCD) responsible for 41 million deaths per year [1]. They account for over 80% of all premature NCD-related deaths worldwide [1]. Environment is a major determinant of health and according to the World Health Organization (WHO), known chemical substances (including pesticides) are responsible for 25% of chronic diseases worldwide [2].
Identifying possible levers for reducing exposure to pesticides would enable the development of effective public health strategies. In particular, minimizing exposure to active substances which are currently in use could help prevent NCD [3].
Agricultural pesticides are chemical substances widely used in agriculture to enhance food production, to which individuals are chronically exposed from both occupation (e.g. agricultural workers) and everyday life through air, dust, food/drink (e.g. general population).
The most common pathways of pesticide exposure include the cutaneous, digestive and respiratory routes. The cutaneous route is the main route of exposure in the workplace (i.e. among farmers, agricultural workers, manufacturers, and handlers of these substances). Exposure through the respiratory route concerns certain specific professional practices in closed environments. In the general population, the dietary route is considered the main route of exposure by the WHO, through the intake of contaminated food or drinks [4].
Experimental studies have documented a number of mechanistic pathways through which pesticide exposure could affect health [5,6,7]. With regard to epidemiological evidence, exposure to pesticides has been associated with increased risk of different pathologies such as non-Hodgkin’s lymphoma, multiple myeloma, prostate cancer, Parkinson’s disease as well as cognitive disorders and respiratory diseases [8,9,10,11].
Apart from the health burden, the massive use of pesticides could represent a significant social burden. Thus, a recent study estimated that the social costs attributable to synthetic pesticide use amounted to 372 million euros in 2017 in France, of which 48.5 million euros were related to health costs [12].
However, original research and review studies on the impact of pesticides on human health generally focus on occupational settings, without considering the general population for which diet is the main source of exposure.
Hence, this systematic review aims to synthesize the evidence, from prospective studies, concerning the associations between dietary exposure to pesticides and diet-related NCD and mortality caused by NCD in adults.
Methods
We systematically reviewed prospective studies aimed at estimating the associations between dietary exposure to pesticides and NCD among adults. The methodology for conducting systematic review in nutrition and public health developed by the United States Department of Agriculture (USDA)’s Nutrition Evidence Systematic Review (NESR) team [13] was used. This systematic review was planned and conducted in accordance with the standards of PRISMA-2020 [14].
Search strategy & eligibility criteria
An electronic search of articles was conducted using (MEDLINE) (via PubMed) until July 2023 with no restriction to calendar date. A PRISMA checklist is provided in Supplemental Table 1. The systematic review has been registered in Prospero (Number CRD42022383916).
The literature search was conducted by two authors (JBau, EK-G). Moreover, the reference lists from the identified articles were checked to search for further relevant studies.
The detailed query used in PubMed is presented in Supplemental Method 1.
Inclusion and exclusion criteria
Studies were selected for the review if they met all the criteria, as described in Table 1.
Human biomonitoring studies were excluded since they do not allow to identify the source of exposure. Regarding the outcome, the focus was on NCD and NCD-related mortality, i.e. non-infectious diseases which typically include the four main following types: cardiovascular diseases (CVD), diabetes, cancer and chronic respiratory diseases.
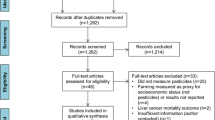
Eligible full-text papers were independently and critically assessed by two authors (JBau, EK-G). A flowchart of the selection process is provided (Fig. 1).
Data extraction
After study selection, the two reviewers extracted the following characteristics: the first author’s last name, year of publication, journal name, study origin, cohort name, sample size, number of cases, age at entry, sex, study duration, exposure assessment, and outcome assessment.
Then, risk estimates (hazard ratios (HR) and corresponding 95% confidence intervals (CI)), and adjustment factors were collected. In the case where several models with different adjustments were provided, the most extensively adjusted model was selected for extraction of the risk estimates.
Risk of bias and grading of evidence
A bias analysis was conducted by JBau and EK-G (epidemiologists), according to the guidelines of NESR based on the Cochrane ROBINS-I (Risk Of Bias In Non-randomized Studies of Interventions ROBIN-I method) [15]. For each study, this analysis included the following items [15]: bias due to confounding, bias in selection of participants into the study, bias in classification of exposures, bias due to departures from intended exposures (potential change of exposure over time), bias due to missing data, bias in measurement of the outcome and bias in selection of the reported results. The different biases are graded according to four levels of judgment: low, moderate, serious, and critical, plus a grading for “no information” [15]. Agreement was observed between the two investigators for four domains (confounding, missing data, measurement of the outcomes and selection of reported results). A second evaluation was carried out for domains where disagreements were observed and a consensus was reached. An overall statement of bias analysis (i.e., ROB, Risk Of Bias) was provided and an overview of risk of bias for each study was illustrated using the Robvis tool [16]. PR, first author of two selected studies did not contribute to the decisions as regards the risk of bias analysis.
Grade of evidence was then assessed according to NESR guidelines using 5 items: the aforementioned-derived ROB, consistency, directness, precision, and generalizability, which were rated on a 4-level scale: strong, moderate, limited, or not assignable (i.e. lack of evidence or severe methodological issues). The grading terminology and definitions are provided in the publication by NESR [13].
Results
A flowchart describing the selection of studies is shown in Fig. 1. For each excluded study, reasons for exclusion are presented in Supplemental Table 2.
Among the 52 eligible studies (of which 2 were manually identified), a total of 6 studies were selected [17,18,19,20,21,22]. The characteristics of each study are presented in Table 2.
Method for assessment of pesticide exposure
The Pesticide Residue Burden Score (PRBS)
Pesticide exposure was assessed in the US cohort studies (conducted in the Nurses’ Health Study (NHS, NHSII) and Health Professional Follow-up Study (HPFS) [17, 18, 20, 22]), using a broad indicator, named PRBS. This indicator combines pesticide surveillance data from the USDA (> 400 different pesticide residues) and food frequency questionnaire (FFQ) consumption data. It allows to classify individuals according to their pesticide residue exposure from fruits and vegetable (F&V) intake.
The PRBS has been validated against 1) urinary concentrations of pesticide biomarkers of organophosphates and pyrethroids, and the 2,4-dichlorophenoxyacetic acid, measured in 90 men participating in the Environment and Reproductive Health cohort study [23] and 2) pesticide metabolites, assessed in 3,679 individuals of the US nationally representative survey NHANES [24].
This index is based on the three following criteria (from the pesticide surveillance program): the percentage of F&V samples with any detectable pesticide residues, the percentage of F&V samples with any pesticide residues above tolerance levels, and the percentage of F&V samples with three or more individual detectable pesticides. For each contamination index, FFQ-F&V are ranked according to their tertile-distribution (assigning 0, 1 or 2 for each respective tertile). Each score is then summed up to obtain the PRBS, which ranges from 0 to 6. A high-pesticide-residue status is given to F&V with a score ≥ 4, a low-pesticide-residue status is given to F&V with a score lower than 4, and an undetermined-pesticide-residue status is given to F&V without contamination data. Cumulative average intakes (per servings per day) of high-, low- and undetermined-pesticide residue F&V are then calculated for each participant and modeled as continuous variables and as quintiles.
Plant-based food exposure profiles derived from contamination data
In the French studies [19, 21], pesticide exposure was estimated by combining plant-based food consumption and CVUAS contamination data for 25 specific pesticides, including substances authorized in organic farming. Exposure profiles were then identified using the non-negative matrix factorization method [25]. This method is a non-supervised dimensionality reduction technique, developed by Lee et Seung [25], especially adapted for parsimonious data subject to the constraints of assay methods (limits of detection and quantification).
Risk of bias assessment
Studies were all conducted in the United States or France, and involved from 13,149 [21] to 180,316 participants [20]. The follow-up duration varied from 5 [21] to 20y [17]. Investigated outcomes included mortality (overall and by causes), cancer (notably breast cancer and glioma), coronary heart diseases (CHD), and type 2 diabetes (T2D).
A risk of bias analysis for each study was conducted and is detailed in Fig. 2. Overall, the quality of reviewed studies was high, studies were rated as having low or moderate risk of bias.
Association study results
The main findings are reported in Table 3.
Cancer
Three studies investigating the risk of cancer in relation to dietary pesticide exposure were identified. One study conducted in the three cohorts of American men and women reported no association between pesticide residue levels by F&V status and risk of cancer, regardless of the location [20]. Another study, conducted within the same cohorts, investigating the risk of glioma reported a higher risk among NHS participants with high intake of high-residue F&V (HRQ5 vs. Q1 = 2.99, 95%CI (1.38; 6.44)) but no association was observed in the other cohorts. In addition, no associations were observed when studying overall or low-residue F&V consumption [18]. The study conducted among French women from the NutriNet-Santé study reported a lower risk of postmenopausal breast cancer among women highly exposed to a mixture of pesticides authorized in organic farming (negatively correlated to synthetic pesticides) (HRQ5 vs. Q1 = 0.57; 95%CI (0.34;0.93)) [21]. A positive association between postmenopausal breast cancer and the mixture correlated to chlorpyrifos, imazalil, malathion, thiabendazole was also detected among women with overweight (including obesity): HRQ5 vs. Q1 = 4.13; 95%CI (1.50;11.44). Other NMF-extracted components were not associated with the risk of postmenopausal breast cancer.
Heart and metabolic diseases
A single study conducted in the same American cohorts evaluated the association between high and low-pesticide residue F&V and CHD [22]. A negative association between intake of low-pesticide residue F&V and the risk of CHD, was observed: HR Q5 vs. Q1 = 0.82; 95%CI (0.71, 0.94). On the opposite, no association was detected for intake of high-pesticide residue F&V.
An association between pesticide exposure and the risk of T2D was found in the NutriNet-Santé study, with a higher risk among participants with higher exposure to a profile of synthetic pesticides: HRQ5 vs. Q1 = 1.47, 95%CI (1.00, 2.18) [19]. A pesticide exposure profile weakly correlated to synthetic pesticides and highly correlated with pesticides authorized in organic farming, was associated with a lower risk of T2D: HRQ5 vs. Q1 = 0.31, 95%CI (0.10, 0.94), only among individuals with overall high dietary quality.
Mortality
Based on data from the three very large US prospective cohorts, another study examined the association of intake of F&V according to pesticide residue status with mortality and found an inverse association with intake of low-pesticide-residue F&V: HRQ5vsQ1 0.64, 95%CI (0.59, 0.68), but not with intake of high-pesticide-residue F&V [17]. This trend was observed for mortality caused by CVD, cancer and respiratory diseases.
Quality of evidence grading
Grading of evidence for each health outcome is presented in Table 4. With regard to cancer, 3 studies were available (with one reporting no association and two a positive association), the level of evidence therefore can be considered as low. For the other outcomes, only one was available, leading to a non-assignable grade for the association.
Discussion
Quality of the included studies
Studies were based on large samples, validated outcomes limiting misclassification, and exposure was derived from detailed food consumption and contamination data. Included studies also accounted for a wide range of potential confounding factors, including dietary patterns which are strongly correlated to pesticide exposure [26, 27]. However, residual confounding can never be excluded from observational studies, even when a wide range of confounders are considered. The studies conducted in the American health cohorts used an index previously validated aiming to classify F&V according to pesticide contamination level. Of note, F&V were classified into simple pesticide residue status categories, which meant that actual quantitative contamination information was not considered when estimating pesticide exposure while the contamination range can be large within both low and high contaminated F&V categories. In particular, the six validated categories of the PRBS were collapsed in binary variables (high/low) in these studies.
In these studies, farming practices with different regulations for pesticide use (i.e. organically or conventionally-grown) were not distinguished nor intake of other potentially pesticide-contaminated foods such as cereals. In contrast, the French studies [19, 21] accounted for detection/quantification limits to build pessimist and optimistic exposure scenario, as recommended by the WHO [28].
However, in the French studies, follow-up duration was short (median follow-up time was approximately 5 years) while it was much longer in the American studies, leading to a very high statistical power in the US studies. In addition, all studies were conducted in Western populations and therefore generalizability is limited for low- or middle-income countries. The American studies focused on F&V while the French studies focused on all foods from plant origin, limiting comparison.
We did not identify any RCT. The level of evidence from prospective observational studies is not as high as that from RCT, however pesticide exposure is a typical case where RCTs are hardly feasible due to technical and ethical issues [29].
Grading level of evidence
Overall, the studies reporting an association between pesticide exposure and NCD outcomes pointed in the direction of a deleterious effect. The study on mortality risk in the general population showed no association with consumption of high-pesticide-residue F&V, as opposed to consumption of low-pesticide-residue F&V which were linked to a protective effect. Among the three studies modeling cancer incidence, two reported a positive association between higher dietary exposure to pesticide residues and risk of glioma and postmenopausal breast cancer (specifically among women with overweight or obesity), respectively and the third study reported no association with all studied sites. The French study focusing on T2D risk showed an association with high exposure to a specific profile of synthetic pesticides. A lower risk of CHD was observed among high American consumers of low-pesticide-residue F&V, while no protective effects were detected with the consumption of high-pesticide-residue F&V. Overall, the number of studies per outcome was very limited, limiting the possibility to grade the level of evidence. For other outcomes than cancer, the grading was not assignable as only one was available. Overall – although not many – studies were of high quality and suggested a role of pesticide exposure through food on health, in particular, risk of cancer and subsequent mortality. This seems consistent with a recent systematic review on pesticides and risk of cancer [11].
Mechanistic pathways
The biological mechanisms through which pesticides can alter biological functioning have been extensively described in experimental studies. Pesticides can affect human health through multiple pathways involving several target organs. In turn, these alterations result in a higher risk of various pathologies (cancers, CVD, respiratory pathologies, neurodegenerative diseases, etc.) [30]. First of all, some pesticides (e.g. organophosphorus compounds) can induce dysregulations of carbohydrate and lipid metabolisms [31], through several underlying mechanisms involving oxidative stress, alterations of insulin secretion, paraoxonase inhibition, or cholinesterase inhibition [32]. Some contaminants may also influence adipocyte proliferation and differentiation by interacting with different nuclear receptors [33, 34]. Next, pesticides may cause genetic alterations (mutation and premutagenic alterations) by direct interactions with the genetic material, leading to DNA damage or chromosomal aberrations [30]. Pesticides may also induce epigenetic modifications such as DNA methylation [30]. Third, pesticides may act as endocrine disruptors, i.e. they can interfere with the synthesis, secretion, transport, binding, action, metabolism or elimination of hormones [35, 36]. The endocrine disrupting properties of pesticides (e.g. organophosphorus moieties) have been indeed widely documented [37] and refer to their ability to mimic estrogenic function by acting as a ligand for receptors, converting other steroids to active estrogens, or increasing the expression of estrogen-sensitive genes [38]. In addition, anti-androgenic effects, through inhibition of androgen-binding receptors, have also been described for organochlorine insecticides, carbamates, and triazines. Finally, organophosphates may inhibit thyroid hormone receptors and pyrethroids may inhibit the action of progesterone [38]. Although not clearly documented, the gut microbiota could potentially play a role in the relationship between pesticides and health notably by inducing a reduction in prevalence of Bifidobacteria and Lactobacillus and an increase in Enterococcus and Bacteroides [39].
Recommendations for further work
Development of well-conducted ad hoc studies is warranted to increase the level of evidence on the impact of dietary pesticide exposure on diet-related NCD. Surveillance components have been included in monitoring surveys in some countries, but long-term prospective population-based studies aiming at estimating the association between dietary exposure to pesticides and human health are needed. Although of interest, accurate exposure measurement (e.g. using biomarkers) is currently expensive and requires high logistic resources limiting its use in large-scale cohorts. Moreover, urinary biomarkers do not generally allow to consider long-term exposure and usually reflect overall exposure, making it difficult to disentangle the various routes of exposure (dietary, respiratory, and cutaneous). This does not make it possible to focus specifically on the dietary route, which is the main route of exposure in the general population, and for which preventive individual and collective actions can be undertaken. To overcome these aspects, the matching of consumption and contamination data is a relevant option which requires: 1) the existence of high-quality consumption and contamination databases, covering a large panel of regions including countries from global South, and a long time period, 2) easy access to these databases and 3) interoperability of the consumption and contamination databases. In addition, a major issue concerns the comparison between studies. For example, regulations vary across countries and change over time. The way pesticide exposure is assessed can also considerably differ depending on the study (e.g. single molecules or mixture of molecules can be considered). Different types of variables (e.g. exposure vs non-exposure or low-level vs high-level contaminated foods) can also be used to reflect different exposure levels. To our knowledge, there are indeed no official international recommendations providing standardized guidance on the way to estimate dietary exposure, including the type of molecules to be prioritized, and the type of statistical modelling to be conducted. There is, therefore, an urgent need to develop a new generation of epidemiological studies considering a common methodological framework to assess exposure to pesticides through diet, in order to better characterize the risk for individuals, and to conduct meta-analyses in the future. While working on specific residues allows comparison across studies, it is also of great importance to focus on mixture rather than single molecules, for the same reasons dietary patterns rather than single nutrients are studied in nutritional epidemiology [40, 41]. It will allow to consider potential synergic, antagonist, or cumulative effects. Exposure is the result of each food’s contamination but also depends on consumption patterns. When studying exposure to pesticides in the general population, diet is the main route (chronic exposure to low doses), thus the regional context and current regulation should be considered to focus on authorized active substances, as an important public health target. This implies that updated analyses are conducted, to account for changes in exposure patterns following newly banned active substances. Then, farming practices for food production are strong determinants and should be better assessed.
Conclusion
Finally, studies investigating the impact of exposure to dietary pesticides on the onset and progression of NCD in adults are scarce. In addition, studies were conducted in the Western context (France and the United States) and studies in other settings are necessary. Furthermore, prospective studies using detailed pesticide exposure with various endpoints are warranted and various sources of pesticide exposure should also be controlled for. In terms of public health implications, a reduction and minimization of pesticide exposure, notably by the dietary route, may be an important lever for health promotion at the population level. The most harmful residues should be subject to increased monitoring to determine priorities for prohibition and research to propose alternatives.
Availability of data and materials
Researchers from public institutions can submit a collaboration request including information on the institution and a brief description of the project to collaboration@etude-nutrinet-sante.fr. All requests will be reviewed by the steering committee of the NutriNet-Sante study. A financial contribution may be requested. If the collaboration is accepted, a data access agreement will be necessary and appropriate authorizations from the competent administrative authorities may be needed. In accordance with existing regulations, no personal data will be accessible.
Abbreviations
- aDQI:
-
Animal-based Diet Quality Index
- CVUAS:
-
Chemisches und Veterinäruntersuchungsamt Stuttgart
- cDQI:
-
Comprehensive Diet Quality Index
- CHD:
-
Coronary heart diseases
- CVD:
-
Cardiovascular diseases
- FFQ:
-
Food frequency questionnaire
- F&V:
-
Fruits and vegetables
- HPFS:
-
Health Professional Follow-up Study
- ICD:
-
International Classification of Diseases
- NESR:
-
Nutrition Evidence Systematic Review
- NCD:
-
Non-communicable diseases
- NHS:
-
Nurses’ Health Study
- NHSII:
-
Nurses’ Health Study II
- ROB:
-
Risk Of Bias
- ROBINS-I:
-
Risk Of Bias In Non-randomized Studies of Interventions
- pDQI:
-
Plant-based Diet Quality Index
- PRBS:
-
Pesticide Residue Burden Score
- T2D:
-
Type 2 Diabetes
- USDA:
-
United States Department of Agriculture
- WHO:
-
World Health Organization
References
World Health Organization. Noncommunicable diseases - key facts. Available from: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases. [cited 14 Nov 2022].
World Health Organization Health Risk Assessment Toolkit. Chemical hazards. International Program on Chemical Safety Harmonization Project Document. no. 8, WHO, 2010. https://www.who.int/publications/i/item/who-humanhealth-risk-assessment-toolkit.
Wyckhuys KAG, Aebi A, Bijleveld van Lexmond MFIJ, Bojaca CR, Bonmatin JM, Furlan L, et al. Resolving the twin human and environmental health hazards of a plant-based diet. Environ Int. 2020;144:106081.
ANSES. Recommandations et perspectives pour une surveillance nationale de la contamination de l’air par les pesticides. 2010. Available from: https://www.anses.fr/fr/system/files/ORP-Ra-2010AirPesticide.pdf.
Kim KH, Kabir E, Jahan SA. Exposure to pesticides and the associated human health effects. Sci Total Environ. 2017;575:525–35.
Mostafalou S, Abdollahi M. Pesticides: an update of human exposure and toxicity. Arch Toxicol. 2017;91(2):549–99.
Androutsopoulos VP, Hernandez AF, Liesivuori J, Tsatsakis AM. A mechanistic overview of health associated effects of low levels of organochlorine and organophosphorous pesticides. Toxicology. 2013;307:89–94.
Collectif INSERM. Salle de presse | Inserm. Pesticides: Effets sur la santé, une expertise collective de l’Inserm. 2013. Available from: http://presse.inserm.fr/pesticides-effets-sur-la-sante-une-expertise-collective-de-linserm/8463/ [cited 21 Aug 2016].
Schinasi L, Leon M. Non-hodgkin lymphoma and occupational exposure to agricultural pesticide chemical groups and active ingredients: a systematic review and meta-analysis. Int J Environ Res Public Health. 2014;11(4):4449–527.
Rojas-Rueda D, Morales-Zamora E, Alsufyani WA, Herbst CH, AlBalawi SM, Alsukait R, et al. Environmental risk factors and health: an umbrella review of meta-analyses. Int J Environ Res Public Health. 2021;18(2):704.
Cavalier H, Trasande L, Porta M. Exposures to pesticides and risk of cancer: evaluation of recent epidemiological evidence in humans and paths forward. Int J Cancer. 2023;152(5):879–912.
Alliot C, Adams-Marin M, Borniotto D, Baret PV. The social costs of pesticide use in France. Front Sustain Food Syst. 2022;6:1027583.
Spill MK, English LK, Raghavan R, Callahan E, Güngör D, Kingshipp B, et al. Perspective: USDA nutrition evidence systematic review methodology: grading the strength of evidence in nutrition- and public health-related systematic reviews. Adv Nutr. 2022;13(4):982–91.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. 2021;10(1):89.
Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919.
McGuinness LA, Higgins JPT. Risk-of-bias VISualization (robvis): An R package and Shiny web app for visualizing risk-of-bias assessments. Res Syn Meth. 2021;12(1):55–61.
Sandoval-Insausti H, Chiu YH, Wang YX, Hart JE, Bhupathiraju SN, Mínguez-Alarcón L, et al. Intake of fruits and vegetables according to pesticide residue status in relation to all-cause and disease-specific mortality: results from three prospective cohort studies. Environ Int. 2022;15(159):107024.
Cote DJ, Bever AM, Chiu YH, Sandoval-Insausti H, Smith-Warner SA, Chavarro JE, et al. Pesticide residue intake from fruit and vegetable consumption and risk of glioma. Am J Epidemiol. 2022;191(5):825–33.
Rebouillat P, Vidal R, Cravedi JP, Taupier-Letage B, Debrauwer L, Gamet-Payrastre L, et al. Prospective association between dietary pesticide exposure profiles and type 2 diabetes risk in the NutriNet-Santé cohort. Environ Health. 2022;21(1):57.
Sandoval-Insausti H, Chiu YH, Lee DH, Wang S, Hart JE, Mínguez-Alarcón L, et al. Intake of fruits and vegetables by pesticide residue status in relation to cancer risk. Environ Int. 2021;156:106744.
Rebouillat P, Vidal R, Cravedi JP, Taupier-Letage B, Debrauwer L, Gamet-Payrastre L, et al. Prospective association between dietary pesticide exposure profiles and postmenopausal breast-cancer risk in the NutriNet-Santé cohort. Int J Epidemiol. 2021;50(4):1184–98.
Chiu YH, Sandoval-Insausti H, Ley SH, Bhupathiraju SN, Hauser R, Rimm EB, et al. Association between intake of fruits and vegetables by pesticide residue status and coronary heart disease risk. Environ Int. 2019;132:105113.
Chiu YH, Williams PL, Mínguez-Alarcón L, Gillman M, Sun Q, Ospina M, et al. Comparison of questionnaire-based estimation of pesticide residue intake from fruits and vegetables with urinary concentrations of pesticide biomarkers. J Expo Sci Environ Epidemiol. janv 2018;28(1):31–9.
Hu Y, Chiu YH, Hauser R, Chavarro J, Sun Q. Overall and class-specific scores of pesticide residues from fruits and vegetables as a tool to rank intake of pesticide residues in United States: a validation study. Environ Int. 2016;92–93:294–300.
Lee DD, Seung HS. Learning the parts of objects by non-negative matrix factorization. Nature. 1999;401(6755):788–91.
Baudry J, Rebouillat P, Allès B, Cravedi JP, Touvier M, Hercberg S, et al. Estimated dietary exposure to pesticide residues based on organic and conventional data in omnivores, pesco-vegetarians, vegetarians and vegans. Food Chem Toxicol. 2021;153:112179.
Rebouillat P, Vidal R, Cravedi JP, Taupier-Letage B, Debrauwer L, Gamet-Payrastre L, et al. Estimated dietary pesticide exposure from plant-based foods using NMFderived profiles in a large sample of French adults. Eur J Nutr. 2021;60:1475–88.
GEMS / Food-EURO. Second Workshop on Reliable Evaluation of Low-Level Contamination of Food Report on a Workshop in the Frame of GEMS / Food-EURO Kulmbach. 1999. Available from: https://www.semanticscholar.org/paper/GEMS-%2F-Food-EURO-Second-Workshop-on-Reliable-of-of/7d5162794a407ce3361458649750a63b6bda3381 [cited 10 Jan 2023].
Lichtenstein AH, Petersen K, Barger K, Hansen KE, Anderson CAM, Baer DJ, et al. Perspective: design and conduct of human nutrition randomized controlled trials. Adv Nutr. 2021;12(1):4–20.
Mostafalou S, Abdollahi M. Pesticides and human chronic diseases: evidences, mechanisms, and perspectives. Toxicol Appl Pharmacol. 2013;268(2):157–77.
Karami-Mohajeri S, Abdollahi M. Toxic influence of organophosphate, carbamate, and organochlorine pesticides on cellular metabolism of lipids, proteins, and carbohydrates: a systematic review. Hum Exp Toxicol. 2011;30(9):1119–40.
Rahimi R, Abdollahi M. A review on the mechanisms involved in hyperglycemia induced by organophosphorus pesticides. Pestic Biochem Physiol. 2007;88(2):115–21.
Casals-Casas C, Desvergne B. Endocrine disruptors: from endocrine to metabolic disruption. Annu Rev Physiol. 2011;73(1):135–62.
Lau C, Abbott BD, Corton JC, Cunningham ML. PPARs and xenobiotic-induced adverse effects: relevance to human health. PPAR Res. 2011;2010:e954639.
Crisp TM, Clegg ED, Cooper RL, Wood WP, Anderson DG, Baetcke KP, et al. Environmental endocrine disruption: an effects assessment and analysis. Environ Health Perspect. 1998;106(suppl 1):11–56.
Bergman Å, United Nations Environment Programme, World Health Organization. State of the science of endocrine disrupting chemicals - 2012 an assessment of the state of the science of endocrine disruptors. Geneva: WHO: UNEP; 2013. Available from: http://www.who.int/ceh/publications/endocrine/en/index.html [cited 26 Mar 2021].
Mnif W, Hassine AIH, Bouaziz A, Bartegi A, Thomas O, Roig B. Effect of endocrine disruptor pesticides: a review. Int J Environ Res Public Health. 2011;8(6):2265–303.
McKinlay R, Plant JA, Bell JNB, Voulvoulis N. Endocrine disrupting pesticides: implications for risk assessment. Environ Int. 2008;34(2):168–83.
Utembe W, Kamng’ona AW. Gut microbiota-mediated pesticide toxicity in humans: methodological issues and challenges in the risk assessment of pesticides. Chemosphere. 2021;271:129817.
Jacobs DR Jr, Gross MD, Tapsell LC. Food synergy: an operational concept for understanding nutrition. Am J Clin Nutr. 2009;89(1938-3207 (Electronic)):1543S–1548S.
Ocke MC. Evaluation of methodologies for assessing the overall diet: dietary quality scores and dietary pattern analysis. Proc Nutr Soc. 2013;72(1475-2719 (Electronic)):191–9.
Funding
Justine Berlivet is supported by a fellowship from the Fondation pour la Recherche Médicale, grant number ENV202109013962 to Emmanuelle Kesse-Guyot.
Author information
Authors and Affiliations
Contributions
EK-G and JBau designed the research, conducted the literature search, analyzed the data and drafted a first version of the manuscript. PR, CS and JBer contributed to interpretation of data. All authors critically revised the manuscript and approved the final version to be published. JBau and EK-G are the guarantors.
Corresponding author
Ethics declarations
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplemental Method 1.
Request for research. Supplemental Table 1. PRISMA Checklist. Supplemental Table 2. Excluded studies and reasons for exclusion.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Baudry, J., Rebouillat, P., Samieri, C. et al. Dietary pesticide exposure and non-communicable diseases and mortality: a systematic review of prospective studies among adults. Environ Health 22, 76 (2023). https://doi.org/10.1186/s12940-023-01020-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12940-023-01020-8