Abstract
Background
A growing body of literature investigated childhood exposure to environmental chemicals in association with attention-deficit/hyperactivity disorder (ADHD) symptoms, but limited studies considered urinary mixtures of multiple chemical classes. This study examined associations of concurrent exposure to non-persistent chemicals with ADHD symptoms in children diagnosed with autism spectrum disorder (ASD), developmental delay (DD), and typical development (TD).
Methods
A total of 549 children aged 2–5 years from the Childhood Autism Risks from Genetics and Environment (CHARGE) case-control study were administered the Aberrant Behavior Checklist (ABC). This study focused on the ADHD/noncompliance subscale and its two subdomains (hyperactivity/impulsivity, inattention). Sixty-two chemicals from four classes (phenols/parabens, phthalates, organophosphate pesticides, trace elements) were quantified in child urine samples, and 43 chemicals detected in > 70% samples were used to investigate their associations with ADHD symptoms. Negative binomial regression was used for single-chemical analysis, and weighted quantile sum regression with repeated holdout validation was applied for mixture analysis for each chemical class and all chemicals. The mixture analyses were further stratified by diagnostic group.
Results
A phthalate metabolite mixture was associated with higher ADHD/noncompliance scores (median count ratio [CR] = 1.10; 2.5th, 97.5th percentile: 1.00, 1.21), especially hyperactivity/impulsivity (median CR = 1.09; 2.5th, 97.5th percentile: 1.00, 1.25). The possible contributors to these mixture effects were di-2-ethylhexyl phthalate (DEHP) metabolites and mono-2-heptyl phthalate (MHPP). These associations were likely driven by children with ASD as these were observed among children with ASD, but not among TD or those with DD. Additionally, among children with ASD, a mixture of all chemicals was associated with ADHD/noncompliance and hyperactivity/impulsivity, and possible contributors were 3,4-dihydroxy benzoic acid, DEHP metabolites, MHPP, mono-n-butyl phthalate, and cadmium.
Conclusions
Early childhood exposure to a phthalate mixture was associated with ADHD symptoms, particularly among children with ASD. While the diverse diagnostic profiles limited generalizability, our findings suggest a potential link between phthalate exposure and the comorbidity of ASD and ADHD.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Attention-defici/hyperactivity disorder (ADHD) is a neurodevelopmental disorder, in which the individual manifests developmentally inappropriate levels of symptoms of inattention and/or hyperactivity/impulsivity [1]. Symptoms associated with the disorder occur on a continuum. ADHD is highly common, with the prevalence ranging from 5.9% [2] to 9.4% [3] and is twice as common in males as in females [2]. Because ADHD symptoms are increasingly diagnosed in the autism population, with the publication of the Diagnostic and Statistical Manual–5 (DSM-5) edition permitting the co-morbid diagnosis of ADHD to be given in autistic individuals [1], it is important to understand what factors might influence the presence of ADHD symptoms in autistic as well as non-autistic individuals. Estimates of ADHD symptoms in autism vary with older studies finding lower estimates, for example 2% [4], and more recent studies, as high as 78% [5]. The importance of studying autistic youth with significant ADHD symptoms is reinforced by findings from a recent study indicating 1.2% of children in the U.S. have both disorders [6]. Our group found that the rate of ADHD symptoms in children diagnosed with autism as well as with neurodevelopmental disorders who do not have autism is significantly higher than expected in the general population [7].
Despite the high heritability of ADHD, environmental factors, including chemical exposures, nutrient deficiencies, preterm birth, pregnancy complications, and extreme deprivation, are also associated with development of ADHD [8, 9]. While the prenatal period has been recognized as the most sensitive window of neurodevelopment, chemical exposure during the early postnatal period has also been a focus due to the continued postnatal development of the brain [10, 11]. An accumulating body of epidemiological literature suggests that prenatal as well as early-life exposures to environmental chemicals are associated with ADHD diagnosis or symptoms [12, 13].
Young children are exposed to mixtures of non-persistent environmental chemicals, including environmental phenols and parabens, phthalates, organophosphate (OP) pesticides, and trace elements [14]. Many of these chemicals have the potential to induce neurotoxicity and contribute to behavioral problems in laboratory animals [15,16,17,18,19,20,21,22,23,24,25], through mechanisms such as the disruption of thyroid hormone homeostasis [26,27,28], oxidative stress [29,30,31], or inhibition of the enzyme acetylcholinesterase in the brain [29, 30, 32]. However, epidemiological studies investigating childhood exposure to these chemicals, either as an individual compound or a mixture, in association with ADHD diagnosis or related behaviors have reported mixed results [33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50]. Additionally, there have been limited studies focusing on exposure to mixtures of environmental chemicals across multiple classes to address real-world exposures [51,52,53].
This study aimed to examine if concurrent exposure to each chemical as well as a mixture of these chemicals is associated with ADHD symptoms in early childhood in a cohort that includes children diagnosed with autism spectrum disorder (ASD) or developmental delay (DD) and those with typical development (TD).
Methods
Study population
Our study population consisted of a subset of children from the Childhood Autism Risks from Genetics and Environment (CHARGE) case-control study [54]. The CHARGE study primarily recruited children who received services for ASD or DD through the California Department of Developmental Services. General population controls were randomly selected from state birth files and frequency-matched to the sex, age, and residential catchment area of ASD cases. Given the male-to-female ASD prevalence ratio, the goal was to recruit more males (80%) than females (20%). Children were eligible for inclusion in the CHARGE study if they were 2 to 5 years old at enrollment, born in California, living with at least one biologic parent who speaks English or Spanish, and residing in the study catchment areas. Details on study design, subject recruitment, and data collection protocols are available elsewhere [54]. After being enrolled, children were administered a set of standardized assessments to confirm their diagnosis (Fig. S1). For example, children recruited as having ASD were clinically confirmed. Children recruited as having DD or controls were screened for ASD and evaluated for DD. Diagnostic tools and algorithms to classify children into ASD, DD, or TD groups are described elsewhere [54]. The study protocol received approval from the University of California (UC) Davis Institutional Review Boards and the State of California Committee for the Protection of Human Subjects. Before collecting data, participants provided written consent.
Among those who were enrolled between 2006 and 2017, a total of 549 children who provided a sufficient volume (≥ 16 mL) of urine and were assessed for ADHD behaviors were included in this study (Fig. S1). These children were classified as either ASD (n = 225), DD (n = 88), or TD (n = 236).
Assessment of ADHD symptoms
Children at 2 to 5 years old were assessed for ADHD symptoms using the Aberrant Behavior Checklist (ABC) at the UC Davis Medical Investigations of Neurodevelopmental Disorders (MIND) Institute. The ABC was selected to assess behavioral symptoms because a substantial portion (57%) of the participants have intellectual disability. It was developed for children with neurodevelopmental concerns, particularly to assess the response to interventions [55]. The ABC has demonstrated moderate to high convergent validity with other commonly used scales, mostly in children with neurodevelopmental disorders [56, 57]. Furthermore, it showed good validity in children with ASD and TD [56] and in toddlers with neurodevelopmental disorders [58]. The ABC consists of 58 items, each of which is scored from 0 (not at all a problem) to 3 (the problem is severe in degree) with higher scores indicating greater problems [55]. The current study used the ADHD/noncompliance subscale of the ABC as the subscale items align most closely with those on the DSM-5 Text Revision (DSM-5-TR) [1] for ADHD, as opposed to the other subscales (Irritability, lethargy, stereotypy, and inappropriate speech). The ADHD/noncompliance subscale is composed of 16 items with a score range of 0–48 to assess ADHD symptoms. The ADHD/noncompliance subscale was further separated into two subdomains to explore the ADHD symptoms by subtypes: hyperactivity/impulsivity (10 items with a score range of 0–30) and inattention (3 items with a score range of 0–9) [7]. Items related to defiance and oppositionality were excluded, as according to both the current and most recent previous DSM-5-TR [1], Oppositional and Defiant Disorder is considered a separate disorder. When considering other commonly used behavioral instruments, such as Child Behavior Checklist [59] or Conners’ Parent Rating Scale [60], those items are assessed on separate scales. The list of items that belong to the ADHD/noncompliance subscale and two subdomains is shown in Table S1.
Urinary chemical quantification
Child spot urine samples were collected at the study visit when the child was 2 to 5 years of age. The urine samples were immediately stored at − 20 °C, and aliquots were shipped on dry ice to the New York State Department of Health’s Wadsworth Center’s Child Health Exposure Analysis Resource (CHEAR) Targeted Analysis Laboratory. A total of 62 trace organic chemicals were analyzed in urine within the CHEAR organic biomonitoring section at Wadsworth: 30 phenols/parabens, 20 phthalate metabolites, and 6 dialkylphosphate (DAP) metabolites of OP pesticides; 6 trace elements were measured in urine within the CHEAR inorganic biomonitoring section at Wadsworth. The chemical names and abbreviations of the 62 analytes are presented in Table S2. For analysis of phenols/parabens, urine samples were enzymatically deconjugated and extracted using liquid-liquid extraction and analyzed by high-performance liquid chromatography-tandem mass spectrometry (HPLC-MS/MS) [61,62,63]. For quantification of phthalate metabolites, urine samples were processed using enzymatic deconjugation followed by solid-phase extraction (SPE) prior to HPLC-MS/MS analysis [64, 65]. DAP metabolites were extracted from urine samples using SPE and analyzed by HPLC-MS/MS [66]. Trace elements in urine were analyzed within the CHEAR section of the Laboratory of Inorganic and Nuclear Chemistry at Wadsworth using Inductively Coupled Plasma Mass Spectrometry (ICP-MS) [67]. Detailed descriptions of the analytical method for each chemical class, including sample preparation, instrumental analysis, and mass spectrometric parameters, are available elsewhere [68].
Fifteen blinded duplicates were analyzed with study samples, along with multiple CHEAR reference materials, for quality assurance purposes. Median relative percentage differences of the valid duplicate samples, in which both were detected above the limit of detection (LOD), ranged from 5 to 46% for phenols/parabens, 5 to 38% for phthalate metabolites, 8 to 13% for OP pesticide metabolites, and 1 to 27% for trace elements (Table S3). The LODs ranged from 0.02 to 1 ng/mL for phenols/parabens, 0.01 to 5 ng/mL for phthalate metabolites, 0.02 to 0.1 ng/mL for pesticide metabolites, and 0.0007 to 0.45 ng/mL for trace elements (Table S3). Instrument software-generated values were used for urinary chemical concentrations below the LOD to reduce bias from replacing non-detected concentrations with a single value [69, 70].
Statistical analysis
Descriptive analysis
Among 62 analytes quantified in child urine samples, 43 chemicals with detection frequencies over 70%, including 21 phenols/parabens, 12 phthalates, 5 pesticides, and 5 trace elements, were included in the statistical analyses. Several zero or negative values, occurring as a result of blank correction of instrument software-generated values, were replaced with a fixed value (i.e., 0.0001) to allow natural log (ln)-transformation [71]. The positive nonzero values were then specific gravity (SG)-corrected using the following equation: Csg = C × [(SGmedian – 1)/(SG – 1), where Csg is the SG-corrected chemical concentration, C is the measured chemical concentration, SGmedian is the median (1.022) of SG values in this study samples, and SG is the measured SG value [72, 73].
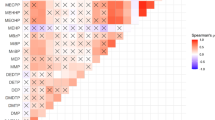
Spearman’s rank correlation coefficients among SG-corrected concentrations of 43 compounds were computed. Mono-2-(carboxymethyl) hexyl phthalate (MCMHP), mono-(2-ethyl-5-carboxypentyl) phthalate (MECPP), mono (2-ethyl-5-hydroxyhexyl) phthalate (MEHHP), and mono (2-ethyl-5-oxohexyl) phthalate (MEOHP), originating from the same parent compound, di-2-ethylhexyl phthalate (DEHP), showed strong correlations. Similarly, benzophenones and their metabolites, including 2,4-dihydroxybenzophenone (BP1), 2-hydroxy-4-methoxybenzophenone (BP3), 2,2′-dihydroxy-4-methoxybenzophenone (BP8), and 4-hydroxybenzophenone (OH4BP), also showed strong correlations due to the common exposure sources. Therefore, molar sums of DEHP metabolites and benzophenones were separately computed and used in the subsequent analysis rather than individual compounds.
Covariate selection
Potential confounders and risk factors for ADHD were identified a priori based on a directed acyclic graph (Fig. S2) [74]. ADHD/noncompliance subscale and two subdomain scores and SG-corrected chemical concentrations were compared by covariates using the Wilcox rank-sum or the Kruskal-Wallis test, and those variables that had associations with all three outcomes (p < 0.05) were selected as covariates. The final set of covariates includes: CHARGE case-control study frequency matching factors (child’s sex [female, male], age at assessment [in years; centered to the mean], and recruitment regional center), child’s birth year (2000–2004, 2005–2008, 2009–2013) and race/ethnicity (non-Hispanic White, non-Hispanic non-White, Hispanic) as an indicator of structural racism, maternal metabolic conditions (healthy weight/overweight and no metabolic conditions, obese or hypertensive disorder/gestational diabetes), parity (1, ≥ 2), highest education in household (high school/GED or less, some college credit, bachelor’s degree or higher) as an indicator of socioeconomic status, and diagnostic groups (ASD, DD, TD). Among the indicator variables of socioeconomic status, which were weak to moderately correlated with each other, parental education was selected, instead of mother’s age at delivery and homeownership, to avoid collinearity issues because it was most strongly associated with both exposures and outcomes.
Single-chemical analysis
Negative binomial regression models, adjusting for the covariates, were used to examine the associations of each chemical with the ADHD/noncompliance subscale and two subdomain scores to account for over-dispersed count outcomes. The SG-corrected concentrations were ln-transformed and standardized prior to the regression analyses. Count ratios (CRs) and 95% confidence intervals (CIs) were computed by exponentiating regression coefficients. The corresponding p-values were corrected for multiple comparisons using the false discovery rate (FDR) method per outcome and chemical class.
Mixture analysis
Repeated holdout validation for weighted quantile sum (WQS) regression for negative binomial outcomes was implemented to investigate the associations of each chemical class mixture with ABC scores [75]. For a WQS regression, the empirical weights, indicating the relative importance, of each chemical were estimated across 100 bootstrap samples in the randomly partitioned training set (40%). In the remaining test set (60%), the WQS index, representing the total body burden, was computed per each chemical class using the estimated weights [76, 77]. The WQS index was used in negative binomial regression models with adjustment of the covariates to examine its association with the outcomes. To obtain stable WQS estimates, the repeated holdout validation approach was used by randomly partitioning the dataset 100 times and performing the WQS regression on each set, generating 100 effect estimates and chemical weights and taking the median as the final estimate [75]. By iterating the partitioning process 100 times, this approach improves generalizability by mitigating the impact of sample-specific chemical weights and WQS index estimates and addressing the potential for unbalanced partitions and biased estimates from a single partition. Our focus was on the positive direction, as our hypothesis posited that the mixture index would be associated with higher ABC scores (i.e., greater behavioral problems). When a chemical class mixture showed significant associations in 95% of the repetitions (i.e., CR between the 2.5th and 97.5th percentiles [PCT] indicating either CR > 1 or CR < 1), its chemical weight distribution was presented. Based on the Busgang Criteria, chemicals that had 90 and 50% of the repetitions above their class threshold were defined as probable and possible contributors, respectively [68, 78]. For example, if a phthalate metabolite exceeded the class threshold (1/9 phthalate metabolites = 0.11) in over 50% of the repetitions, the metabolite was considered as a possible contributor.
Associations between total mixtures of all 43 analytes, and ABC scores were investigated using random subset WQS with repeated holdout validation, which iteratively selects random subsets of 7 chemicals (√43 ~ 7) and estimates weight parameters by combining results across multiple ensemble steps [75, 79].
Stratified/effect modification analysis
As children with ASD, followed by those with DD, showed more ADHD symptoms when compared to those with TD [7, 58], the mixture analyses were stratified by diagnostic group (i.e., ASD, DD, and TD). Furthermore, as previous studies reported sex-specific associations of phenols, phthalates, OP pesticides, and trace elements with child neurodevelopment [13, 80,81,82,83], child’s sex was evaluated as an effect modifier in the mixture models for ADHD/noncompliance. Sex-stratified interaction WQS regression models, with 100 repeated holdouts, were constructed by including the interaction term between sex and WQS index in addition to their main effects and covariates [78, 84]. These models allow for sex-specific effect estimates and chemical weights.
All analyses were performed with an open-source R software, version 4.1.0 (R Foundation for Statistical Computing, Vienna, Austria), including the “gWQS” package [85]. A statistical significance level was set at 0.05 for unadjusted p-values and 0.10 for FDR-corrected p-values.
Results
ABC scores by demographic characteristics
The majority of the study children were males (80.1%) and born non-preterm (87.6%), and approximately 49% of them were non-Hispanic white (Table 1). More than half of the children were born to mothers who were not obese in pre-pregnancy and did not have any metabolic conditions (63.8%) and were multiparous (56.1%). Most of the participating families had a highest education level of a bachelor’s degree or higher (56.6%) and owned a home (60.4%).
Median (interquartile range) for ABC scores in the whole study population were 7 (1, 19) for the ADHD/noncompliance subscale, 4 (1, 11) for the hyperactivity/impulsivity subdomain, and 2 (0, 4) for the inattention subdomain. The ABC scores differed by demographic characteristics (Table 1). Non-preterm children had lower ABC scores than children born pre-term, and non-Hispanic white and Hispanic children had lower scores compared to non-Hispanic, non-White (i.e., Asian, Black, and multi-racial) children. Children whose mothers were 30 to 34 years old at delivery had lower scores than those whose mothers were younger than 30 years or at or older than 35 years. Children born to mothers who were obese in pre-pregnancy or had hypertensive disorder or gestational diabetes had higher scores compared to those born to mothers who were not obese or did not have metabolic conditions. The first-born children had higher scores than the second- or later-born children. Children born to parents whose maximum education level was high school or less had higher scores than those born to parents with higher education. Children from families that owned a home had lower scores than those from families that did not. In terms of diagnostic groups, children with ASD had the highest, those with DD had the second highest, and those with TD had the lowest scores.
Child urinary chemical concentrations
Detection frequency and distributions of SG-uncorrected concentrations of each chemical in child urine samples are presented in Table S3. Sixteen out of 30 phenols/parabens, 11 out of 20 phthalate metabolites, 5 out of 6 pesticide metabolites, and 4 out of 6 trace elements were detected in greater than 90% of the samples. Several chemicals within each class were significantly correlated with each other (Fig. S3). Specifically, benzophenones (BP1, BP3, and BP8) showed strong correlations, as did DEHP metabolites (MCMHP, MECPP, MEHHP, and MEOHP). Correlations were weak to moderate among other phthalate metabolites (Spearman’s rank correlation coefficients [rsp] = 0.22–0.69) and among pesticide metabolites (rsp = 0.28–0.67), while they were moderate to strong among parabens (rsp = 0.30–0.78). There were differences in urinary chemical concentrations across all demographic characteristics, particularly birth year for all chemical classes, child sex for phthalate metabolites, homeownership for pesticide metabolites, and diagnostic groups for trace elements (Fig. S4).
Associations of individual chemical concentrations with ADHD/noncompliance subscale and two subdomain scores
There were several associations between individual urinary chemical concentrations and ABC scores, as shown in volcano plots (Fig. 1). Among all children, ∑DEHP was associated with higher scores of all three subscale/subdomains (CR = 1.09, 95% CI: 1.00, 1.20 for ADHD/noncompliance; CR = 1.11, 95% CI: 1.01, 1.22 for hyperactivity/impulsivity; CR = 1.06, 95% CI: 0.99, 1.13 for inattention) (Table S4). Two other phthalate metabolites were marginally associated with higher scores: mono-n-butyl phthalate (MNBP) with hyperactivity/impulsivity (CR = 1.10, 95% CI: 1.00, 1.21) and mono-carboxy isononyl phthalate (MCINP) with inattention (CR = 1.07, 95% CI: 0.99, 1.15). On the other hand, two phenols/parabens were associated with lower ABC scores: 3,4-dihydroxy benzoic acid (DHB34) with ADHD/noncompliance (CR = 0.90, 95% CI: 0.82, 0.99) and hyperactivity/impulsivity (CR = 0.90, 95% CI: 0.81, 0.99) and triclosan with ADHD/noncompliance (CR = 0.90, 95% CI: 0.82, 0.99) and inattention (CR = 0.89, 95% CI: 0.83, 0.96). However, after correcting for FDR, only the association between triclosan and inattention remained significant (Table S4). Pesticide metabolites and trace elements were not associated with ABC scores.
Volcano plots of covariate-adjusted CRs and unadjusted p-values of SG-corrected, ln-transformed, and standardized urinary chemical concentrations in association with ABC ADHD/noncompliance subscale and two subdomain scores among 549 CHARGE children. Red dots represent chemicals with an unadjusted p < 0.05 and an FDR-corrected p < 0.10, orange dots represent chemicals with an unadjusted p < 0.05, and blue dots represent chemicals with a 0.05 < unadjusted p < 0.10. Negative binomial regression models were adjusted for CHARGE case-control study frequency matching factors (child’s sex, age at assessment, and recruitment regional center), child’s birth year and race/ethnicity, parity, parental education, maternal metabolic conditions, and diagnosis. ABC, Aberrant Behavior Checklist; ADHD, attention-deficit/hyperactivity disorder; BUPB, butyl paraben; CHARGE, Childhood Autism Risks from Genetics and Environment; CR, count ratio; DEHP, di-2-ethylhexyl phthalate; DHB34, 3,4-dihydroxy benzoic acid; FDR, false discovery rate; MCINP, mono-carboxy isononyl phthalate; MNBP, mono-n-butyl phthalate; SG, specific gravity
Associations of chemical class and total mixtures with ADHD/noncompliance subscale and two subdomain scores
Mixture analyses showed that the phthalate index was associated with higher scores of ADHD/noncompliance (median CR = 1.10, 2.5th and 97.5th PCT: 1.00, 1.21) and hyperactivity/impulsivity (median CR = 1.09, 2.5th and 97.5th PCT: 1.00, 1.25) among all children (Table 2). For both associations, ∑DEHP (17 and 15%, respectively) and mono-2-heptyl phthalate (MHPP) (23 and 16%, respectively) exceeded the class threshold (i.e., 1/9*100 = 11%) in over 50% of 100 repetitions and therefore were considered possible contributors based on the Busgang Criteria (Fig. 2). MNBP additionally contributed to the associations between the phthalate index and hyperactivity/impulsivity.
Estimated weight distributions of urinary phthalate metabolites from 100 repetitions of weighted quantile sum (WQS) regression for (A) ADHD/compliance subscale and (B) hyperactivity/impulsivity subdomain. Boxes indicate 25th, 50th, and 75th percentiles, diamonds indicate mean, and whiskers indicate 10th and 90th percentiles of weights. The dashed line indicates the threshold (1/# of chemicals in the mixture). ADHD, attention-deficit/hyperactivity disorder; DEHP, di-2-ethylhexyl phthalate; MBzP, mono-benzyl phthalate; MCINP, mono-carboxy isononyl phthalate; MCIOP, mono-carboxy isooctyl phthalate; MCPP, mono (3-carboxypropyl) phthalate; MEP, monoethyl phthalate; MHPP, mono-2-heptyl phthalate; MIBP, mono-isobutyl phthalate; MNBP, mono-n-butyl phthalate
Stratified analysis by diagnostic group revealed several associations among children with ASD but not among children with DD or TD (Table 2). Among children with ASD, the phthalate index was also associated with higher scores of all three subscale/subdomains: ADHD/noncompliance (median CR = 1.15, 2.5th and 97.5th PCT: 1.06, 1.26), hyperactivity/impulsivity (median CR = 1.22, 2.5th and 97.5th PCT: 1.07, 1.37), and inattention (median CR = 1.10, 2.5th and 97.5th PCT: 1.02, 1.20). While ∑DEHP, mono-benzyl phthalate (MBZP), MHPP, and MNBP were common possible contributors for ADHD/noncompliance (12, 11, 13, and 21%, respectively) and hyperactivity/impulsivity (12, 12, 12, and 17%, respectively), MHPP, mono-isobutyl phthalate (MIBP), and MNBP were possible contributors for inattention (12, 19, and 19%, respectively) (Fig. 3). The total mixture index, of which DHB34, ∑DEHP, MBZP, MHPP, MNBP, and cadmium (Cd) were identified as possible contributors, was associated with higher scores of ADHD/noncompliance (median CR = 1.15, 2.5th and 97.5th PCT: 1.01, 1.29; median weight: 8, 5, 5, 4, 7, and 3%, respectively) and hyperactivity/impulsivity (median CR = 1.21, 2.5th and 97.5th PCT: 1.04, 1.36; median weight: 3, 6, 5, 6, 10, and 5%, respectively) (Table 2 and Fig. 3). The WQS regression models for each chemical class restricted to DD or TD did not converge (Table 2). Only the models for total mixtures converged, but none of them showed significant associations.
Estimated weight distributions of urinary chemicals from 100 repetitions of weighted quantile sum (WQS) regression, restricted to children with ASD. Phthalate metabolites in association with ADHD/noncompliance subscale, hyperactivity/impulsivity subdomain, and inattention subdomain are presented in (A), (B), and (C), respectively. Total chemicals in association with ADHD/noncompliance subscale and hyperactivity/impulsivity subdomain are presented in (D) and (E), respectively. Boxes indicate 25th, 50th, and 75th percentiles, diamonds indicate mean, and whiskers indicate 10th and 90th percentiles of weights. The dashed line indicates the threshold (1/# of chemicals in the mixture). Full chemical names are listed in Table S2. ADHD, attention-deficit/hyperactivity disorder; ASD, autism spectrum disorder
Sex-stratified interaction WQS regression models revealed no significant effect modification by child’s sex for associations between any mixture and ABC scores, as evaluated using the 2.5th and 97.5th PCTs of the interaction term between WQS index and child’s sex (Table S5). However, the phthalate index was associated with higher scores of ADHD/noncompliance among males only (median CR = 1.32, 2.5th and 97.5th PCT: 1.01, 2.70), with ∑DEHP and MHPP identified as possible contributors (Fig. S5a). On the other hand, the pesticide index was associated with higher scores of ADHD/noncompliance among females only (median CR = 1.28, 2.5th and 97.5th PCT: 1.03, 2.69), with diethylthiophosphate and dimethyldithiophosphate identified as possible contributors (Fig. S5b).
Discussion
In the present study, concurrent measurement of environmental phenols and parabens, phthalates, OP pesticides, and trace elements in child urine samples were examined in association with ADHD symptoms, specifically the ADHD/noncompliance subscale and the hyperactivity/impulsivity and inattention subdomains, among 2- to 5-year-old children diagnosed with either ASD, DD, or TD. In the single-chemical analysis, DEHP metabolites were cross-sectionally associated with increased hyperactivity and impulsivity, while triclosan with decreased inattention (Table 3). In the mixture analysis using WQS regression, exposure to phthalate mixtures was associated with ADHD symptoms, especially hyperactivity and impulsivity, and the possible chemicals of concern were DEHP metabolites, MHPP, and MNBP.
These findings were likely driven by children with ASD, as the associations remained similar among children with ASD, but not among children with DD or TD. In addition, among children with ASD, a mixture of phthalate metabolites, possibly contributed by MIBP and MNBP, were associated with greater inattention. Further, mixtures of all chemicals, including phenols and parabens, phthalates, OP pesticides, and trace elements, were associated with ADHD symptoms, especially hyperactivity and impulsivity, and common possible contributors were DHB34, DEHP metabolites, MBZP, MHPP, MNBP, and Cd. These findings suggest that the early childhood exposure to several phthalates, parabens, and cadmium may be associated with the comorbidity of ASD and ADHD. One possible reason why we observed these associations among children with ASD only is higher and more variable ABC scores compared to those with DD or TD. However, as children with ASD are likely to have different dietary habits, behaviors, and usage of personal care products [86, 87] resulting in different exposure patterns to these non-persistent chemicals, potential reverse causality cannot be ruled out. Further studies on chemical exposures in relation to diets and behaviors in children with ASD can help address these questions.
Our findings on associations between childhood phthalate exposure, as an individual compound or a mixture, and greater ADHD symptoms in young children are generally in line with previous studies. One prospective study on childhood phthalate exposure in association with ADHD-related behaviors reported that MNBP and monoethyl phthalate (MEP) as well as phthalate metabolite mixtures, possibly contributed by MCINP, MEP, and MBZP, were associated with more externalizing problems, indicating more hyperactivity, aggression, and conduct problems in children aged 2–8 years [88]. Another study observed cross-sectional associations of greater ADHD traits with MBZP at 2 years [89]. Most of the other cross-sectional studies examining ADHD diagnosis or related behaviors in middle-childhood or adolescence reported adverse associations with DEHP metabolites [90,91,92,93,94] and di-n-butyl phthalate metabolites [33, 92, 93, 95,96,97], while a few additional prospective studies did not find convincing associations [98,99,100]. Young children not only have different exposure patterns to phthalates from their mothers, as indicated by weak correlations of phthalate metabolite concentrations in young children with those in their mothers’ prenatal or postnatal urine samples [101, 102], but also higher body burden [103, 104]. Therefore, the accumulating epidemiological evidence warrants further longitudinal investigations on early childhood exposure to phthalates and ADHD-related behaviors to establish causality, particularly in prospective study settings.
Underlying mechanisms of phthalates’ effects on ADHD remain unclear. ADHD is associated with alterations in the dopamine system and associated brain regions, such as the striatum, and potentially, the midbrain [105,106,107,108,109]. Toxicological studies reported that rats or mice neonatally exposed to DEHP or dicyclohexyl phthalate had impaired tyrosine hydroxylase immunoreactivity within midbrain dopaminergic nuclei [18, 110]. Neonatal exposure of rats to DEHP or dibutyl phthalate expressed hyperactivity, concomitantly with alterations in gene expression in the midbrain and striatum [19, 22, 23]. In addition to the effect of phthalates on subcortical structures, cortical thickness is modestly thinner in children with ADHD and delayed in maturation in comparison to control participants [111, 112]. Among children with ADHD, DEHP metabolite concentrations were negatively correlated with cortical thickness in the right middle and superior temporal gyri, suggesting a possible role of DEHP in impaired brain structures [93].
Significant associations of a phthalate metabolite mixture with ADHD symptoms were observed among males only, with no evident effect modification by sex. However, given that this study population includes four times more males than females, thus potentially underpowered for detecting associations in females, these findings should be interpreted with caution. Phthalates are reported to interfere with thyroid functions, which are essential for normal brain development, in a sexually dimorphic manner [26, 28], and early thyroid hormone disruption may contribute to the development of ADHD [113]. Still, regarding phthalate exposure and ADHD-related behaviors, there is inconsistent evidence on effect modification by sex [81, 88, 90, 91, 96, 97] or mediation by thyroid hormone [114]; therefore, these should be explored in future studies.
There are a limited number of studies examining associations of prenatal or childhood exposure to mixtures of multiple classes of urinary chemicals with ADHD diagnosis or related behaviors. Guilbert et al., who quantified phthalate/plasticizer metabolites and phenols/parabens in 416 prenatal maternal urine samples, observed that a chemical mixture, primarily weighted for BP3, triclosan, methyl paraben (MEPB), ethyl paraben (ETPB), and several phthalate metabolites (diisononyl phthalate metabolites, di (isononyl)cyclohexane-1,2-dicarboxylate metabolites, MBZP, MEP), was associated with more externalizing behaviors in 2-year-old French children [115]. Van den Dries et al. reported null associations of prenatal exposure to mixtures of phthalates, BPA, and OP pesticides with attention problems in 782 Dutch children aged 6 years [116]. Maitre et al. that measured pre- and postnatal environmental exposures from outdoor, indoor, chemical, lifestyle and social domains in 1287 European mother-child pairs observed associations of prenatal exposure to an OP pesticide metabolite, dimethyl phosphate (DMP), with more externalizing symptoms at 6–11 years of age, while those of childhood DMP exposure with less ADHD symptoms [51]. Waits et al. examined concurrent exposure to phthalates, OP pesticides, and nonylphenol in relation to 76 ADHD diagnoses versus 98 controls in Taiwanese children aged 4–15 years. They observed associations of a chemical mixture, primarily contributed by two OP pesticide metabolites (DMP, diethyl phosphate [DEP]) and two phthalate metabolites (MEP, MBZP), with increased odds of ADHD [53]. Many of these chemicals, to which the general population is simultaneously exposed, have endocrine disrupting potentials and share common mechanisms, including disruption of thyroid and neurotransmitter functions [21, 26, 117, 118], and concentrations of these chemicals frequently measured in the urine are correlated within and across class [53, 68, 115, 116, 119, 120]. Therefore, mixture analyses using multiple chemical classes helps with understanding of mixture effects of environmental chemicals on child neurobehaviors.
This study was strengthened by quantification of 62 chemicals from four chemical groups in urine samples of young children. WQS was employed to examine associations of chemical mixtures with ADHD-related behaviors, allowing for modeling multiple chemical exposures, which were correlated with each other, and minimizing the multiple comparisons problem. However, several limitations should be noted. First, due to the cross-sectional design, our results do not represent causal effects of childhood chemical exposures on ADHD symptoms. Second, this study also relied on concentrations of non-persistent chemicals measured in a spot urine sample, which reflect recent exposure. In young children, several phenols, phthalate metabolites, OP pesticides, and trace elements showed moderate reproducibility over short-term periods but reduced reproducibility over longer time frames [121,122,123,124,125,126,127]. Third, as this study used child urine samples as an exposure matrix, instead of whole blood samples, several other trace elements, especially known neurotoxicants, were not able to be included as analytes. Fourth, though an array of sociodemographic variables were considered as covariates, there is potential residual confounding by unmeasured factors related to diet, lifestyle, or parental ADHD symptoms. Fifth, our results cannot be generalized to general population because approximately 57% of our study population included children with ASD or DD, who showed more ADHD symptoms than those with TD. Still, the diverse diagnostic profile enabled us to examine childhood exposure to chemical mixtures in association with the comorbidity of ASD and ADHD, while exploring their association with ADHD behaviors in typically developing children. As distinct exposure mixture patterns may have differential effects on children based on their susceptibility, further investigations into ADHD symptoms among children with neurodevelopmental disorders are warranted.
Conclusions
In the CHARGE population, comprised of 2- to 5-year-old children diagnosed with ASD, DD, and TD, concurrent exposure to a phthalate mixture, highly weighted for DEHP metabolites and MHPP, was associated with greater ADHD symptoms, possibly driven by children with ASD. Among children with ASD, a mixture of all chemicals were associated with ADHD symptoms, and possible chemicals of concern were one phenol (DHB34), several phthalate metabolites (DEHP metabolites, MBZP, MHPP, and MNBP), and a trace element (Cd). Because children with ASD not only have more pronounced ADHD behaviors but also show different exposure patterns to non-persistent chemicals due to different diet and behaviors, further attention to exposure of these children to possible neurotoxicants are warranted. Future investigation on exposure to mixtures of larger number of chemicals that share similar exposure sources could better address real-world exposures, in association with ADHD symptoms.
Availability of data and materials
Lab and epidemiological data are hosted at the Human Health Exposure Analysis Resources (HHEAR) Data Center Repository (https://hheardatacenter.mssm.edu/).
References
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. text rev. ed. Washington DC; 2022.
Willcutt EG. The prevalence of DSM-IV attention-deficit/hyperactivity disorder: a meta-analytic review. Neurotherapeutics. 2012;9:490–9.
Danielson ML, Bitsko RH, Ghandour RM, Holbrook JR, Kogan MD, Blumberg SJ. Prevalence of parent-reported ADHD diagnosis and associated treatment among US children and adolescents, 2016. J Clin Child Adolesc Psychol. 2018;47:199–212.
Hanson E, Cerban BM, Slater CM, Caccamo LM, Bacic J, Chan E. Brief report: prevalence of attention deficit/hyperactivity disorder among individuals with an autism spectrum disorder. J Autism Dev Disord. 2013;43:1459–64.
Brookman-Frazee L, Stadnick N, Chlebowski C, Baker-Ericzén M, Ganger W. Characterizing psychiatric comorbidity in children with autism spectrum disorder receiving publicly funded mental health services. Autism. 2018;22:938–52.
Casseus M. Prevalence of co-occurring autism spectrum disorder and attention deficit/hyperactivity disorder among children in the United States. Autism. 2022;26:1591–7.
Lyall K, Schweitzer JB, Schmidt RJ, Hertz-Picciotto I, Solomon M. Inattention and hyperactivity in association with autism spectrum disorders in the CHARGE study. Res Autism Spectr Disord. 2017;35:1–12.
Banerjee TD, Middleton F, Faraone SV. Environmental risk factors for attention-deficit hyperactivity disorder. Acta Paediatr. 2007;96:1269–74.
Faraone SV, Banaschewski T, Coghill D, Zheng Y, Biederman J, Bellgrove MA, et al. The world federation of ADHD international consensus statement: 208 evidence-based conclusions about the disorder. Neurosci Biobehav Rev. 2021;128:789–818.
Heyer DB, Meredith RM. Environmental toxicology: sensitive periods of development and neurodevelopmental disorders. Neurotoxicol. 2017;58:23–41.
Stiles J, Jernigan TL. The basics of brain development. Neuropsychol Rev. 2010;20:327–48.
Moore S, Paalanen L, Melymuk L, Katsonouri A, Kolossa-Gehring M, Tolonen H. The association between ADHD and environmental chemicals—a scoping review. Int J Environ Res Public Health. 2022;19:2849.
Schantz SL, Eskenazi B, Buckley JP, Braun JM, Sprowles JN, Bennett DH, et al. A framework for assessing the impact of chemical exposures on neurodevelopment in ECHO: opportunities and challenges. Environ Res. 2020;188:109709.
CDC, 2022. Fourth Report on Human Exposure to Environmental Chemicals, Updated Tables, March 2022. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention. Atlanta, GA.
Davidson PW, Myers GJ, Weiss B. Mercury exposure and child development outcomes. Pediatrics. 2004;113:1023–9.
Dinocourt C, Legrand M, Dublineau I, Lestaevel P. The neurotoxicology of uranium. Toxicol. 2015;337:58–71.
Grandjean P, Herz KT. Trace elements as paradigms of developmental neurotoxicants: Lead, methylmercury and arsenic. J Trace Elem Med Biol. 2015;31:130–4.
Ishido M, Masuo Y, Sayato-Suzuki J, Oka S, Niki E, Morita M. Dicyclohexylphthalate causes hyperactivity in the rat concomitantly with impairment of tyrosine hydroxylase immunoreactivity. J Neurochem. 2004;91:69–76.
Ishido M, Morita M, Oka S, Masuo Y. Alteration of gene expression of G protein-coupled receptors in endocrine disruptors-caused hyperactive rats. Regul Pept. 2005;126:145–53.
Mason LH, Harp JP, Han DY. Pb Neurotoxicity: Neuropsychological effects of lead toxicity. BioMed Res Int. 2014;2014:840547. https://doi.org/10.1155/2014/840547.
Masuo Y, Ishido M. Neurotoxicity of endocrine disruptors: possible involvement in brain development and neurodegeneration. J Toxicol Environmental Health Part B. 2011;14:346–69.
Masuo Y, Ishido M, Morita M, Oka S. Effects of neonatal treatment with 6-hydroxydopamine and endocrine disruptors on motor activity and gene expression in rats. Neural plast. 2004a;11:59–76.
Masuo Y, Morita M, Oka S, Ishido M. Motor hyperactivity caused by a deficit in dopaminergic neurons and the effects of endocrine disruptors: a study inspired by the physiological roles of PACAP in the brain. Regul Pept. 2004b;123:225–34.
Naughton SX, Terry AV Jr. Neurotoxicity in acute and repeated organophosphate exposure. Toxicol. 2018;408:101–12.
Osorio-Rico L, Santamaria A, Galván-Arzate S. Thallium toxicity: general issues, neurological symptoms, and neurotoxic mechanisms. In: Aschner M, Costa L. (eds) neurotoxicity of metals. Advances in neurobiology, vol 18. Cham: Springer; 2017. https://doi.org/10.1007/978-3-319-60189-2_17.
Ghassabian A, Trasande L. Disruption in thyroid signaling pathway: a mechanism for the effect of endocrine-disrupting chemicals on child neurodevelopment. Front Endocrinol. 2018;9:204.
Hlisníková H, Petrovičová I, Kolena B, Šidlovská M, Sirotkin A. Effects and mechanisms of phthalates’ action on neurological processes and neural health: a literature review. Pharmacol Rep. 2021;73:386–404.
Miodovnik A, Edwards A, Bellinger DC, Hauser R. Developmental neurotoxicity of ortho-phthalate diesters: review of human and experimental evidence. Neurotoxicol. 2014;41:112–22.
Ganie SY, Javaid D, Hajam YA, Reshi MS. Mechanisms and treatment strategies of organophosphate pesticide induced neurotoxicity in humans: a critical appraisal. Toxicol. 2022;472:153181.
Tsai Y-H, Lein PJ. Mechanisms of organophosphate neurotoxicity. Curr opin toxicol. 2021;26:49–60.
Valko M, Morris H, Cronin M. Metals, toxicity and oxidative stress. Curr Med Chem. 2005;12:1161–208.
Richardson JR, Fitsanakis V, Westerink RH, Kanthasamy AG. Neurotoxicity of pesticides. Acta Neuropathol. 2019;138:343–62.
Arbuckle TE, Davis K, Boylan K, Fisher M, Fu J. Bisphenol a, phthalates and lead and learning and behavioral problems in Canadian children 6–11 years of age: CHMS 2007–2009. Neurotoxicol. 2016;54:89–98.
Bao Q-S, Lu C-Y, Song H, Wang M, Ling W, Chen W-Q, et al. Behavioural development of school-aged children who live around a multi-metal sulphide mine in Guangdong province, China: a cross-sectional study. BMC Public Health. 2009;9:1–8.
Bouchard MF, Bellinger DC, Wright RO, Weisskopf MG. Attention-deficit/hyperactivity disorder and urinary metabolites of organophosphate pesticides. Pediatrics. 2010;125:e1270–7.
Ciesielski T, Weuve J, Bellinger DC, Schwartz J, Lanphear B, Wright RO. Cadmium exposure and neurodevelopmental outcomes in US children. Environ Health Perspect. 2012;120:758–63.
Eskenazi B, Marks AR, Bradman A, Harley K, Barr DB, Johnson C, et al. Organophosphate pesticide exposure and neurodevelopment in young Mexican-American children. Environ Health Perspect. 2007;115:792–8.
Guo J, Wu C, Zhang J, Li W, Lv S, Lu D, et al. Maternal and childhood urinary phenol concentrations, neonatal thyroid function, and behavioral problems at 10 years of age: the SMBCS study. Sci Total Environ. 2020;743:140678.
Gustin K, Tofail F, Vahter M, Kippler M. Cadmium exposure and cognitive abilities and behavior at 10 years of age: a prospective cohort study. Environ Int. 2018;113:259–68.
Kim S, Arora M, Fernandez C, Landero J, Caruso J, Chen A. Lead, mercury, and cadmium exposure and attention deficit hyperactivity disorder in children. Environ Res. 2013;126:105–10.
Li Y, Zhang H, Kuang H, Fan R, Cha C, Li G, et al. Relationship between bisphenol a exposure and attention-deficit/hyperactivity disorder: a case-control study for primary school children in Guangzhou. China Environ pollut. 2018b;235:141–9.
Oulhote Y, Bouchard MF. Urinary metabolites of organophosphate and pyrethroid pesticides and behavioral problems in Canadian children. Environ Health Perspect. 2013;121:1378–84.
Renzetti S, Cagna G, Calza S, Conversano M, Fedrighi C, Forte G, et al. The effects of the exposure to neurotoxic elements on Italian schoolchildren behavior. Sci Rep. 2021a;11:1–12.
Roen EL, Wang Y, Calafat AM, Wang S, Margolis A, Herbstman J, et al. Bisphenol a exposure and behavioral problems among inner city children at 7–9 years of age. Environ Res. 2015;142:739–45.
Roy A, Kordas K, Lopez P, Rosado JL, Cebrian ME, Vargas GG, et al. Association between arsenic exposure and behavior among first-graders from Torreon. Mexico Environ res. 2011;111:670–6.
Stacy SL, Papandonatos GD, Calafat AM, Chen A, Yolton K, Lanphear BP, et al. Early life bisphenol a exposure and neurobehavior at 8 years of age: identifying windows of heightened vulnerability. Environ Int. 2017b;107:258–65.
Tewar S, Auinger P, Braun JM, Lanphear B, Yolton K, Epstein JN, et al. Association of bisphenol a exposure and attention-deficit/hyperactivity disorder in a national sample of US children. Environ Res. 2016;150:112–8.
Yoo S-J, Joo H, Kim D, Lim MH, Kim E, Ha M, et al. Associations between exposure to bisphenol a and behavioral and cognitive function in children with attention-deficit/hyperactivity disorder: a case-control study. Clin Psychopharmacol Neurosci. 2020;18:261.
Yousef S, Adem A, Zoubeidi T, Kosanovic M, Mabrouk AA, Eapen V. Attention deficit hyperactivity disorder and environmental toxic metal exposure in the United Arab Emirates. J Trop Pediatr. 2011;57:457–60.
Yu CJ, Du JC, Chiou HC, Chung MY, Yang W, Chen YS, et al. Increased risk of attention-deficit/hyperactivity disorder associated with exposure to organophosphate pesticide in Taiwanese children. Androl. 2016;4:695–705.
Maitre L, Julvez J, López-Vicente M, Warembourg C, Tamayo-Uria I, Philippat C, et al. Early-life environmental exposure determinants of child behavior in Europe: a longitudinal, population-based study. Environ Int. 2021;153:106523.
Shoaff JR, Coull B, Weuve J, Bellinger DC, Calafat AM, Schantz SL, et al. Association of exposure to endocrine-disrupting chemicals during adolescence with attention-deficit/hyperactivity disorder–related behaviors. JAMA Netw Open. 2020;3:e2015041–1.
Waits A, Chang C-H, Yu C-J, Du J-C, Chiou H-C, Hou J-W, et al. Exposome of attention deficit hyperactivity disorder in Taiwanese children: exploring risks of endocrine-disrupting chemicals. J Expos Sci Environ Epidemiol. 2022;32:169–76.
Hertz-Picciotto I, Croen LA, Hansen R, Jones CR, Van de Water J, Pessah IN. The CHARGE study: an epidemiologic investigation of genetic and environmental factors contributing to autism. Environ Health Perspect. 2006;114:1119–25.
Aman MG , Singh NN , Stewart AW , Field CJ. The aberrant behavior checklist: a behavior rating scale for the assessment of treatment effects. Am J Mental Defic. 1985;89(5):485–91.
Kaat AJ, Lecavalier L, Aman MG. Validity of the aberrant behavior checklist in children with autism spectrum disorder. J Autism Dev Disord. 2014;44:1103–16.
Miller ML, Fee VE, Jones CJ. Psychometric properties of ADHD rating scales among children with mental retardation. Res Dev Disabil. 2004;25:477–92.
Karabekiroglu K, Aman MG. Validity of the aberrant behavior checklist in a clinical sample of toddlers. Child Psychiatry Hum Dev. 2009;40:99–110.
Achenbach TM, Rescorla LA. Manual for the ASEBA preschool forms and profiles. Burlington VT: University of Vermont Research center for children youth; 2000.
Conners CK. Conner’s rating scales—revised technical manual. Toronto ON: Multi-Health Systems Inc; 1997.
Asimakopoulos AG, Thomaidis NS, Kannan K. Widespread occurrence of bisphenol a diglycidyl ethers, p-hydroxybenzoic acid esters (parabens), benzophenone type-UV filters, triclosan, and triclocarban in human urine from Athens. Greece Sci total environ. 2014;470:1243–9.
Li AJ, Xue J, Lin S, Al-Malki AL, Al-Ghamdi MA, Kumosani TA, et al. Urinary concentrations of environmental phenols and their association with type 2 diabetes in a population in Jeddah. Saudi Arabia Environ res. 2018a;166:544–52.
Rocha BA, Asimakopoulos AG, Honda M, da Costa NL, Barbosa RM, Barbosa F Jr, et al. Advanced data mining approaches in the assessment of urinary concentrations of bisphenols, chlorophenols, parabens and benzophenones in Brazilian children and their association to DNA damage. Environ Int. 2018;116:269–77.
Li AJ, Martinez-Moral M-P, Al-Malki AL, Al-Ghamdi MA, Al-Bazi MM, Kumosani TA, et al. Mediation analysis for the relationship between urinary phthalate metabolites and type 2 diabetes via oxidative stress in a population in Jeddah. Saudi Arabia Environ int. 2019;126:153–61.
Rocha BA, Asimakopoulos AG, Barbosa F Jr, Kannan K. Urinary concentrations of 25 phthalate metabolites in Brazilian children and their association with oxidative DNA damage. Sci Total Environ. 2017;586:152–62.
Li AJ, Banjabi AA, Takazawa M, Kumosani TA, Yousef JM, Kannan K. Serum concentrations of pesticides including organophosphates, pyrethroids and neonicotinoids in a population with osteoarthritis in Saudi Arabia. Sci Total Environ. 2020a;737:139706.
Minnich MG, Miller DC, Parsons PJ. Determination of as, cd, Pb, and hg in urine using inductively coupled plasma mass spectrometry with the direct injection high efficiency nebulizer. Spectrochim Acta B At Spectrosc. 2008;63:389–95.
Bennett DH, Busgang SA, Kannan K, Parsons PJ, Takazawa M, Palmer CD, et al. Environmental exposures to pesticides, phthalates, phenols and trace elements are associated with neurodevelopment in the CHARGE study. Environ Int. 2022;161:107075.
Richardson DB, Ciampi A. Effects of exposure measurement error when an exposure variable is constrained by a lower limit. Am J Epidemiol. 2003;157:355–63.
Schisterman EF, Vexler A, Whitcomb BW, Liu A. The limitations due to exposure detection limits for regression models. Am J Epidemiol. 2006;163:374–83.
Buckley JP, Kuiper JR, Bennett DH, Barrett ES, Bastain T, Breton CV, et al. Exposure to contemporary and emerging Chemicals in Commerce among pregnant women in the United States: the environmental influences on child health outcome (ECHO) program. Environ Sci Technol. 2022;56(10):6560–73. https://doi.org/10.1021/acs.est.1c08942.
Boeniger MF, Lowry LK, Rosenberg J. Interpretation of urine results used to assess chemical exposure with emphasis on creatinine adjustments: a review. Am Ind Hyg Assoc J. 1993;54:615–27.
Kuiper JR, O'Brien KM, Ferguson KK, Buckley JP. Urinary specific gravity measures in the US population: implications for the adjustment of non-persistent chemical urinary biomarker data. Environ Int. 2021;156:106656.
Hernán MA, Hernández-Díaz S, Robins JM. A Structural Approach to Selection Bias. Epidemiology. 2014;15(5):615–25. https://www.jstor.org/stable/20485961.
Tanner EM, Bornehag C-G, Gennings C. Repeated holdout validation for weighted quantile sum regression. MethodsX. 2019;6:2855–60.
Carrico C, Gennings C, Wheeler DC, Factor-Litvak P. Characterization of weighted quantile sum regression for highly correlated data in a risk analysis setting. J Agric Biol Environ Stat. 2015;20:100–20.
Lazarevic N, Barnett AG, Sly PD, Knibbs LD. Statistical methodology in studies of prenatal exposure to mixtures of endocrine-disrupting chemicals: a review of existing approaches and new alternatives. Environ Health Perspect. 2019;127:026001.
Busgang SA, Spear EA, Andra SS, Narasimhan S, Bragg JB, Renzetti S, et al. Application of growth modeling to assess the impact of hospital-based phthalate exposure on preterm infant growth parameters during the neonatal intensive care unit hospitalization. Sci Total Environ. 2022;850:157830.
Curtin P, Kellogg J, Cech N, Gennings C. A random subset implementation of weighted quantile sum (WQSRS) regression for analysis of high-dimensional mixtures. Commun Stat Simulat Comput. 2021;50:1119–34.
Bauer JA, Fruh V, Howe CG, White RF, Claus Henn B. Associations of metals and neurodevelopment: a review of recent evidence on susceptibility factors. Curr Epidemiol Rep. 2020;7:237–62.
Jankowska A, Nazareth L, Kaleta D, Polanska K. Review of the existing evidence for sex-specific relationships between prenatal phthalate exposure and Children’s neurodevelopment. Int J Environ Res Public Health. 2021;18:13013.
Minatoya M, Kishi R. A review of recent studies on bisphenol a and phthalate exposures and child neurodevelopment. Int J Environ Res Public Health. 2021;18:3585.
Sapbamrer R, Hongsibsong S. Effects of prenatal and postnatal exposure to organophosphate pesticides on child neurodevelopment in different age groups: a systematic review. Environ Sci Pollut Res. 2019;26:18267–90.
Gennings C, Svensson K, Wolk A, Lindh C, Kiviranta H, Bornehag C-G. Using metrics of a mixture effect and nutrition from an observational study for consideration towards causal inference. Int J Environ Res Public Health. 2022;19:2273.
Renzetti S, Gennings C, Curtin PC. gWQS: an R package for linear and generalized weighted quantile sum (WQS) regression. J Stat Softw. 2019:1–9.
Bandini LG, Anderson SE, Curtin C, Cermak S, Evans EW, Scampini R, et al. Food selectivity in children with autism spectrum disorders and typically developing children. J Pediatr. 2010;157:259–64.
Hertz-Picciotto I, Bergman Å, Fängström B, Rose M, Krakowiak P, Pessah I, et al. Polybrominated diphenyl ethers in relation to autism and developmental delay: a case-control study. Environ Health. 2011;10:1–11.
Li N, Papandonatos GD, Calafat AM, Yolton K, Lanphear BP, Chen A, et al. Gestational and childhood exposure to phthalates and child behavior. Environ Int. 2020b;144:106036.
Ku H-Y, Tsai T-L, Wang P-L, Su P-H, Sun C-W, Wang C-J, et al. Prenatal and childhood phthalate exposure and attention deficit hyperactivity disorder traits in child temperament: a 12-year follow-up birth cohort study. Sci Total Environ. 2020;699:134053.
Chopra V, Harley K, Lahiff M, Eskenazi B. Association between phthalates and attention deficit disorder and learning disability in US children, 6–15 years. Environ Res. 2014;128:64–9.
Hu D, Wang Y-X, Chen W-J, Zhang Y, Li H-H, Xiong L, et al. Associations of phthalates exposure with attention deficits hyperactivity disorder: a case-control study among Chinese children. Environ Pollut. 2017;229:375–85.
Kim B-N, Cho S-C, Kim Y, Shin M-S, Yoo H-J, Kim J-W, et al. Phthalates exposure and attention-deficit/hyperactivity disorder in school-age children. Biol Psychiatry. 2009;66:958–63.
Park S, Lee J-M, Kim J-W, Cheong J, Yun H, Hong Y-C, et al. Association between phthalates and externalizing behaviors and cortical thickness in children with attention deficit hyperactivity disorder. Psychol Med. 2015;45:1601–12.
Watkins DJ, Meeker JD, Tamayo-Ortiz M, Sánchez BN, Schnaas L, Peterson KE, et al. Gestational and peripubertal phthalate exposure in relation to attention performance in childhood and adolescence. Environ Res. 2021;196:110911.
Jankowska A, Polańska K, Koch HM, Pälmke C, Waszkowska M, Stańczak A, et al. Phthalate exposure and neurodevelopmental outcomes in early school age children from Poland. Environ Res. 2019b;179:108829.
Tsai C-S, Chou W-J, Lee S-Y, Lee M-J, Chou M-C, Wang L-J. Phthalates, Para-hydroxybenzoic acids, bisphenol-a, and gonadal hormones’ effects on susceptibility to attention-deficit/hyperactivity disorder. Toxics. 2020;8:57.
Won E-K, Kim Y, Ha M, Burm E, Kim Y-S, Lim H, et al. Association of current phthalate exposure with neurobehavioral development in a national sample. Int J Hyg Environ Health. 2016;219:364–71.
Daniel S, Balalian AA, Insel BJ, Liu X, Whyatt RM, Calafat AM, et al. Prenatal and early childhood exposure to phthalates and childhood behavior at age 7 years. Environ Int. 2020;143:105894.
Huang H-B, Kuo P-H, Su P-H, Sun C-W, Chen WJ, Wang S-L. Prenatal and childhood exposure to phthalate diesters and neurobehavioral development in a 15-year follow-up birth cohort study. Environ Res. 2019;172:569–77.
Jankowska A, Polańska K, Hanke W, Wesołowska E, Ligocka D, Waszkowska M, et al. Prenatal and early postnatal phthalate exposure and child neurodevelopment at age of 7 years–polish mother and child cohort. Environ Res. 2019a;177:108626.
Myridakis A, Fthenou E, Balaska E, Vakinti M, Kogevinas M, Stephanou EG. Phthalate esters, parabens and bisphenol-a exposure among mothers and their children in Greece (Rhea cohort). Environ Int. 2015;83:1–10.
Song NR, On JW, Lee J, Park J-D, Kwon H-J, Yoon HJ, et al. Biomonitoring of urinary di (2-ethylhexyl) phthalate metabolites of mother and child pairs in South Korea. Environ Int. 2013;54:65–73.
Choi J, Knudsen LE, Mizrak S, Joas A. Identification of exposure to environmental chemicals in children and older adults using human biomonitoring data sorted by age: results from a literature review. Int J Hyg Environ Health. 2017;220:282–98.
Wang Y, Zhu H, Kannan K. A review of biomonitoring of phthalate exposures. Toxics. 2019;7:21.
Elliott BL, D’Ardenne K, Mukherjee P, Schweitzer JB, McClure SM. Limbic and executive meso-and nigrostriatal tracts predict impulsivity differences in attention-deficit/hyperactivity disorder. Biol Psychiat: Cognit Neurosci Neuroimag. 2022;7:415–23.
Kowalczyk OS, Mehta MA, O’Daly OG, Criaud M. Task-based functional connectivity in attention-deficit/hyperactivity disorder: a systematic review. Biol Psychiatry Global Open Sci. 2022;2:350–67.
Rosch KS, Crocetti D, Hirabayashi K, Denckla MB, Mostofsky SH, Mahone EM. Reduced subcortical volumes among preschool-age girls and boys with ADHD. Psychiatry Res Neuroimaging. 2018;271:67–74.
Shvarzman R, Crocetti D, Rosch KS, Li X, Mostofsky SH. Reduced basal ganglia tissue-iron concentration in school-age children with attention-deficit/hyperactivity disorder is localized to limbic circuitry. Exp Brain Res. 2022;240:3271–88.
Swanson JM, Kinsbourne M, Nigg J, Lanphear B, Stefanatos GA, Volkow N, et al. Etiologic subtypes of attention-deficit/hyperactivity disorder: brain imaging, molecular genetic and environmental factors and the dopamine hypothesis. Neuropsychol Rev. 2007;17:39–59.
Tanida T, Warita K, Ishihara K, Fukui S, Mitsuhashi T, Sugawara T, et al. Fetal and neonatal exposure to three typical environmental chemicals with different mechanisms of action: mixed exposure to phenol, phthalate, and dioxin cancels the effects of sole exposure on mouse midbrain dopaminergic nuclei. Toxicol Lett. 2009;189:40–7.
Bernanke J, Luna A, Chang L, Bruno E, Dworkin J, Posner J. Structural brain measures among children with and without ADHD in the adolescent brain and cognitive development study cohort: a cross-sectional US population-based study. Lancet Psychiatry. 2022;9:222–31.
Shaw P, Malek M, Watson B, Sharp W, Evans A, Greenstein D. Development of cortical surface area and gyrification in attention-deficit/hyperactivity disorder. Biol Psychiatry. 2012;72:191–7.
Drover SS, Villanger GD, Aase H, Skogheim TS, Longnecker MP, Zoeller RT, et al. Maternal thyroid function during pregnancy or neonatal thyroid function and attention deficit hyperactivity disorder: a systematic review. Epidemiol (Cambridge Mass). 2019;30:130.
Engel SM, Villanger GD, Nethery RC, Thomsen C, Sakhi AK, Drover SS, et al. Prenatal phthalates, maternal thyroid function, and risk of attention-deficit hyperactivity disorder in the Norwegian mother and child cohort. Environ Health Perspect. 2018;126:057004.
Guilbert A, Rolland M, Pin I, Thomsen C, Sakhi AK, Sabaredzovic A, et al. Associations between a mixture of phenols and phthalates and child behaviour in a French mother–child cohort with repeated assessment of exposure. Environ Int. 2021;156:106697.
van den Dries MA, Ferguson KK, Keil AP, Pronk A, Spaan S, Ghassabian A, et al. Prenatal exposure to nonpersistent chemical mixtures and offspring IQ and emotional and behavioral problems. Environ Sci Technol. 2021;55:16502–14.
Darbre PD. How could endocrine disrupters affect human health? Endocrine Disruption and Human Health: Elsevier; 2022.
Schug TT, Blawas AM, Gray K, Heindel JJ, Lawler CP. Elucidating the links between endocrine disruptors and neurodevelopment. Endocrinol. 2015;156:1941–51.
Kalloo G, Wellenius GA, McCandless L, Calafat AM, Sjodin A, Karagas M, et al. Profiles and predictors of environmental chemical mixture exposure among pregnant women: the health outcomes and measures of the environment study. Environ Sci Technol. 2018;52:10104–13.
Lee W-C, Fisher M, Davis K, Arbuckle TE, Sinha SK. Identification of chemical mixtures to which Canadian pregnant women are exposed: the MIREC study. Environ Int. 2017;99:321–30.
Bradman A, Kogut K, Eisen EA, Jewell NP, Quirós-Alcalá L, Castorina R, et al. Variability of organophosphorous pesticide metabolite levels in spot and 24-hr urine samples collected from young children during 1 week. Environ Health Perspect. 2013;121:118–24.
Casas M, Basagaña X, Sakhi AK, Haug LS, Philippat C, Granum B, et al. Variability of urinary concentrations of non-persistent chemicals in pregnant women and school-aged children. Environ Int. 2018;121:561–73.
Stacy SL, Eliot M, Calafat AM, Chen A, Lanphear BP, Hauser R, et al. Patterns, variability, and predictors of urinary bisphenol a concentrations during childhood. Environ Sci Technol. 2016;50:5981–90.
Stacy SL, Eliot M, Etzel T, Papandonatos G, Calafat AM, Chen A, et al. Patterns, variability, and predictors of urinary triclosan concentrations during pregnancy and childhood. Environ Sci Technol. 2017a;51:6404–13.
Teitelbaum S, Britton J, Calafat A, Ye X, Silva M, Reidy J, et al. Temporal variability in urinary concentrations of phthalate metabolites, phytoestrogens and phenols among minority children in the United States. Environ Res. 2008;106:257–69.
Watkins DJ, Eliot M, Sathyanarayana S, Calafat AM, Yolton K, Lanphear BP, et al. Variability and predictors of urinary concentrations of phthalate metabolites during early childhood. Environ Sci Technol. 2014;48:8881–90.
Yen Y-C, Lin T-Y, Chen M-J, Chen Y-C. Exposure variability and determining factors of urinary metals for schoolchildren in Taiwan. Int J Hyg Environ Health. 2022;243:113976.
Acknowledgements
Authors would like to acknowledge the CHARGE investigators, staff, and most of all, the participants for helping make this research possible.
Disclaimer
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Funding
Research reported in this publication was supported by the Environmental influences on Child Health Outcomes (ECHO) program, Office of The Director, National Institutes of Health (NIH), under Award Number UG3OD023365, UH3OD023365 (Bennett, Hertz-Picciotto, Schweitzer). Lab analysis of serum PFAS was supported by funding from the National Institute of Environmental Health Sciences (NIEHS) to the Wadsworth Center-Children’s Health Exposure Analysis Resource (U2CES026542–01) (Kannan, Parsons). This research was also supported through other NIH grants (R01ES015359, R01ES031701, P30ES023513, U54HD079125, P50HD103526), U. S Environmental Protection Agency (83543201), and the UC Davis MIND Institute.
Author information
Authors and Affiliations
Contributions
J.O., I.H., J.B.S. and D.H.B. conceived the study, and I.H., J.B.S., R.J.S., A.M., and D.H.B. oversaw its coordination and data collection. K. Kannan quantified environmental phenols/parabens, phthalate metabolites, organophosphate and pesticide metabolites, and P.J.P. quantified trace elements in child urine samples. J.O. conducted data analyses and drafted the initial manuscript. K. Kim conducted preliminary data analyses. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The CHARGE study protocol and this study were approved by the institutional review boards (IRB) for the State of California and the University of California-Davis (UC-Davis). Participants provided written informed consent before collection of any data.
Competing interests
Rebecca J. Schmidt consults for the Beasley Law Firm. Rebecca J. Schmidt and Deborah H. Bennett consult for Linus Biotechnology, Inc. Other authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Oh, J., Kim, K., Kannan, K. et al. Early childhood exposure to environmental phenols and parabens, phthalates, organophosphate pesticides, and trace elements in association with attention deficit hyperactivity disorder (ADHD) symptoms in the CHARGE study. Environ Health 23, 27 (2024). https://doi.org/10.1186/s12940-024-01065-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12940-024-01065-3