Abstract
Background
Lipoprotein lipase (LPL) is the rate-limiting enzyme for triglyceride hydrolysis. Homozygous or compound heterozygous LPL variants cause autosomal recessive familial chylomicronemia syndrome (FCS), whereas simple heterozygous LPL variants are associated with hypertriglyceridemia (HTG) and HTG-related disorders. LPL frameshift coding sequence variants usually cause complete functional loss of the affected allele, thereby allowing exploration of the impact of different levels of LPL function in human disease.
Methods
All exons and flanking intronic regions of LPL were Sanger sequenced in patients with HTG-related acute pancreatitis (HTG-AP) or HTG-AP in pregnancy. Previously reported LPL frameshift coding sequence variants were collated from the Human Gene Mutation Database and through PubMed keyword searching. Original reports were manually evaluated for the following information: zygosity status of the variant, plasma LPL activity of the variant carrier, disease referred for genetic analysis, patient’s age at genetic analysis, and patient’s disease history. SpliceAI was employed to predict the potential impact of collated variants on splicing.
Results
Two novel rare variants were identified, and 53 known LPL frameshift coding sequence variants were collated. Of the 51 variants informative for zygosity, 30 were simple heterozygotes, 12 were homozygotes, and 9 were compound heterozygotes. Careful evaluation of the 55 variants with respect to their clinical and genetic data generated several interesting findings. First, we conclude that 6–7% residual LPL function could significantly delay the age of onset of FCS and reduce the prevalence of FCS-associated syndromes. Second, whereas a large majority of LPL frameshift coding sequence variants completely disrupt gene function through their "frameshift" nature, a small fraction of these variants may act wholly or partly as "in-frame" variants, leading to the generation of protein products with some residual LPL function. Third, we identified two candidate LPL frameshift coding sequence variants that may retain residual function based on genotype–phenotype correlation or SpliceAI-predicted data.
Conclusions
This study reported two novel LPL variants and yielded new insights into the genotype–phenotype relationship as it pertains to LPL frameshift coding sequence variants.
Similar content being viewed by others
Background
The lipoprotein lipase (LPL) gene (OMIM #609708) is located on chromosome 8p21.3 and contains 10 exons. The precursor LPL protein comprises 475 amino acids, while the mature LPL protein (excluding the 27-amino-acid signal peptide) comprises 448 amino acids. LPL is the rate-limiting enzyme for triglyceride (TG) hydrolysis [1, 2]. LPL is mainly synthesized in the parenchymal cells of the heart, skeletal muscle and adipose tissues [3]. It is transported by glycosylphosphatidylinositol-anchored high density lipoprotein-binding protein 1 (GPIHBP1) across endothelial cells to the capillary lumen, where it hydrolyses TG in TG-rich lipoproteins (e.g., chylomicrons and very low–density lipoprotein) [4]. Complete or almost complete loss of LPL function due to biallelic (homozygous or compound heterozygous) LPL variants causes autosomal recessive familial chylomicronemia syndrome (FCS; also known as type I hyperlipoproteinemia or LPL deficiency), which is characterized by extremely high plasma TG levels (> 10 mmol/L (880 mg/dL)) [5]. FCS typically develops in infancy or early childhood, manifesting as a failure to thrive, abdominal pain, nausea and vomiting progressing to acute pancreatitis (AP) and various other symptoms (e.g., fatigue, irritability, lipemia retinalis, eruptive xanthomas on trunk, back and gluteal region, and hepatosplenomegaly) [5]. Partial loss of LPL function due to monoallelic (simple heterozygous) LPL variants is associated with hypertriglyceridemia (HTG) [6, 7].
Severe HTG is a frequent cause of AP [8]. Indeed, HTG has become the second most common cause of AP in China, accounting for 14–40% of all AP patients [9,10,11]. HTG-related AP (HTG-AP) is more severe and is associated with poorer outcomes than AP due to other etiologies [9]. Determining the molecular basis of the genetic predisposition to HTG-AP promises to improve our options for both prevention and treatment of the disease. During our routine analysis of genetic risk factors in patients with HTG-AP, including HTG-AP in pregnancy, we identified two novel LPL frameshift coding variants (defined here as simple insertion, simple deletion or complex indel variants that (i) occurred entirely within the coding sequence of the LPL gene AND (ii) resulted in the net addition or deletion of an odd number of nucleotides at the DNA sequence level). LPL frameshift coding variants usually result in the complete functional loss of the affected allele, thereby providing a good model system with which to contrast the complete loss of LPL function (due to biallelic variants) with the partial loss of LPL function (due to monoallelic variants) in human disease. Herein, we describe the identification of two novel LPL frameshift variants together with several new insights into the genotype–phenotype relationship obtained through an exploration of the LPL frameshift coding variants reported to date.
Methods
Ethics statement
This study was approved by the Ethics Committee of Jinling Hostipal, Nanjing, China. Informed consent was obtained from each participant.
Patient description
Diagnoses of HTG-AP and HTG-AP in pregnancy were made as previously described [12, 13]. Patients #1 and #2 both suffered from HTG-AP during pregnancy.
Patient #1 was a 33-year-old pregnant woman (31+4 weeks of gestation). She was admitted to the emergency department due to heavy paroxysmal upper abdominal pain and vomiting. Blood examination revealed chylomicronemia, while the TG level was too high to measure accurately. The serum level of amylase was 1235 U/L, and ultrasound examination noted the presence of peripancreatic fluid collection. On the second day, she received an emergency cesarean section for fetal distress, while 200 mL of chylous abdominal exudate was noted during the operation. After delivery, the patient underwent abdominal computed tomography, revealing typical morphology of AP. On the fifth day, she retained a TG level as high as 23.80 mmol/L (2106.3 mg/dL). She was discharged 17 days later, by which time her fasting TG level had decreased to 4.86 mmol/L (430.11 mg/dL). The patient did not report either a personal or a family history of any disease, with the exception of gestational diabetes mellitus being diagnosed at 28 weeks of gestation.
Patient #2 was a 28-year-old female. She experienced an episode of AP at 38+4 weeks of gestation, with a fasting plasma TG level of 35.35 mmol/L (3128.48 mg/dL). She had received symptomatic and organ function support treatments at a local hospital, but her condition did not improve. She was then transferred to our acute pancreatitis center, where she was diagnosed with moderately severe AP with the complication of acute pancreatic necrosis collection. She received comprehensive treatments, including nutritional support and paracentesis drainage. She was discharged 16 days later, by which time her fasting TG level had decreased to 2.59 mmol/L (229.22 mg/dL). The patient did not report any personal or family history of any disease.
Patient #3 was a 43-year-old female. She suffered from sudden and heavy postprandial abdominal pain with nausea and vomiting. She was immediately referred to a local hospital, where a diagnosis of HTG-AP was made (TG level, 33 mmol/L (2920.5 mg/dL)). Twelve days later, she was transferred to our center due to dyspnea and hyperpyrexia and was diagnosed with severe AP. She was discharged 18 days after admission to our hospital with a fasting TG level of 4.94 mmol/L (437.19 mg/dL)). The patient reported a three-year history of HTG. No other personal or family histories of any disease were documented.
Genetic analysis
Genomic DNA was prepared from peripheral blood cells by means of a Gentra Puregene Blood kit (Qiagen, Dusseldorf, Germany). All exons and flanking intronic regions of five primary HTG-related genes, LPL, APOA5 (apolipoprotein A5; OMIM #606368), APOC2 (apolipoprotein C2; OMIM #608083), LMF1 (lipase maturation factor 1; OMIM #611761) and GPIHBP1 (OMIM #612757), were amplified by polymerase chain reaction (PCR) and subsequently Sanger sequenced as previously described [14, 15]. The two novel LPL variants reported in this study were confirmed by independent PCR amplification and Sanger sequencing and have been deposited in the ClinVar database (https://www.ncbi.nlm.nih.gov/clinvar/).
Collation and evaluation of previously reported LPL frameshift coding sequence variants
Previously reported LPL frameshift coding sequence variants were derived primarily from the Human Gene Mutation Database (HGMD; https://www.hgmd.cf.ac.uk) [16]. This was complemented by a combination of a keyword search (“LPL” or “lipoprotein lipase” plus “frameshift variant”, “frameshift mutation”, “truncation variant”, “truncation mutation”, “termination variant” or “termination mutation”) in PubMed and cross-reference examination. Corresponding original reports were manually evaluated for the following information: zygosity status of the variant, plasma LPL activity of the variant carrier, disease referred for genetic analysis, patient’s age at genetic analysis, and patient’s disease history. Whenever a variant was detected as simple heterozygotes and homozygotes or compound heterozygotes, only the homozygous or compound heterozygous state was considered in this study, the underlying logic being that homozygotes or compound heterozygotes were usually more extensively described in terms of their accompanying clinical genetic data and hence potentially more informative with respect to the genotype–phenotype relationship. Moreover, whenever an included variant was reported in ≥ 2 publications, only the first publication was cited. Furthermore, whenever a variant of interest was coinherited with an LPL missense variant in trans, the LPL activity of the missense variant determined by cell transfection experiments was collated by means of a literature search. Variant collation and literature review were frozen on 15 March 2023.
SpliceAI prediction
SpliceAI, a 32-layer deep neural network [17] and currently the most accurate tool for predicting splicing variants, was employed to predict the impact of LPL frameshift coding variants and a common LPL intronic variant (i.e., c.1428-11C > T) on mRNA splicing. The prediction was performed at https://spliceailookup.broadinstitute.org/ (last accessed on July 26, 2023) using the following parameters: Genome version, hg38; Score type, masked; Max distance, 10000. The Δ score ranges from 0 to 1; the higher the score, the more likely the variant is to affect splicing. A variant with a Δ score of ≤ 0.20 was considered unlikely to affect splicing.
Reference sequences and variant nomenclature
NM_000237.3 and NC_000008.11 were used as reference LPL mRNA and DNA sequences, respectively. All variants were named in accordance with Human Genome Variation Society (HGVS) recommendations (http://varnomen.hgvs.org/) [18], with the A of the translation initiation ATG codon of the LPL gene being counted as nucleotide + 1. All variant names at the coding DNA level were verified/normalized at the Leiden University Medical Center (LUMC) Mutalyzer 3 website (https://mutalyzer.nl/) [19]. Variant names at the protein level also followed LUMC Mutalyzer 3 except for one variant (i.e., c.767_768insTAAATATT) that was experimentally determined to result in a transcript with an in-frame deletion [20]. It is also worth mentioning that variants reported in the early literature were described in the context of the 448-amino-acid mature LPL protein (N.B. The first nucleotide of the mature LPL protein-coding sequence corresponds to position c.82 of NM_000237.3; c.1_81 of NM_000237.3 encodes the 27-amino-acid signal peptide of the LPL preprotein).
Results
Identification of two novel LPL frameshift coding sequence variants
We first focused on rare (allele frequency of < 1% in all gnomAD (Genome Aggregation Database; https://gnomad.broadinstitute.org/) populations) missense, frameshift, nonsense or splice site variants in the five primary HTG-related genes, LPL, APOA5, APOC2, LMF1 and GPIHBP1. In patients #1 and #2, we identified the same heterozygous single-nucleotide duplication in exon 1 of the LPL gene, c.32dup (Fig. 1). This variant was deemed to cause a complete functional loss of the affected allele by virtue of its frameshift nature; at the protein level, it was termed p.(Ala12Glyfs*29). The two patients were not known to be related. However, it remains possible that the disease alleles were identical by descent.
In patient #3, we identified a heterozygous 13-bp deletion in the LPL gene (Fig. 2a). The 13-bp deletion was termed c.77_88 + 1del in accordance with HGVS recommendations, but it could alternatively be described as c.76_88del (Fig. 2b), thereby fulfilling the definition of a frameshift coding sequence variant (N.B. The HGVS recommends that “for deletions, duplications and insertions, the most 3’ position possible is arbitrarily assigned to have been changed”). For ease of discussion, this latter description was used here to explore the functional consequences of the 13-bp deletion. As illustrated in Fig. 2c, the sequence spanning the junction of c.76_88del appeared to concur with the 5’ splice site consensus sequence (see [21] and references therein). This suggested that the mutant pre-mRNA would not differ from the wild-type pre-mRNA in terms of intron 1 splicing. As such, the 13-bp deletion would also cause a complete functional loss of the affected allele by virtue of its frameshift nature; at the protein level, it was termed p.(Ala26Lysfs*13).
Identification of a heterozygous 13-bp deletion in the LPL gene and in silico prediction of its impact on splicing. a Sanger sequencing electropherogram showing the 13-bp deletion c.77_88 + 1del (nomenclature in accordance with Human Genome Variation Society (HGVS) recommendations). The variant has been submitted to the ClinVar database. b Illustration showing that c.77_88 + 1del can be alternatively described as c.76_88del. The exon 1 sequence is shown in the upper case, whereas the intron 1 sequence is shown in the lower case. The canonical 5′ splice site GT dinucleotide is highlighted in bold and blue. The start and end positions of the 13-bp deletion in the two alternative nomenclature versions are indicated by red arrows. c Presumed splicing of the c.76_88del LPL pre-mRNA. Normal splicing of the wild-type LPL pre-mRNA is shown for comparison. The DNA sequence was used here instead of the RNA sequence for illustrative purposes. The obligate dinucleotides from the donor and acceptor splice sites, gt and ag, are highlighted in bold and blue. It should be noted that the sequence spanning the junction of the c.76_88del allele conformed to the 5′ splice site consensus sequence. The position weight matrix of the 9‐bp 5′ splice site signal sequence was taken from [22], an Open Access article distributed under the terms of the Creative Commons Attribution Noncommercial License. d SpliceAI predicted impact of c.76_88del on splicing. See text for data interpretation
Neither c.32dup nor c.77_88 + 1del has previously been reported in the literature. Neither of them is present in gnomAD or ClinVar (https://www.ncbi.nlm.nih.gov/clinvar) (as of 25 May 2023). We did not identify any other rare missense, frameshift, nonsense or splice site variants in the five primary HTG-related genes, LPL, APOA5, APOC2, LMF1 and GPIHBP1, in any of the three patients.
We did not identify any rare synonymous or intronic variants in the five primary HTG-related genes in any of the three patients. Variants with an allele frequency of ≥ 1% found in the three patients are listed in Supplementary Table 1. With the exception of LPL c.1428-11C > T (N.B. this variant was predicted here, by means of SpliceAI, to have no effect on splicing), all these variants were annotated as “benign” in terms of their likely clinical significance by gnomAD. This notwithstanding, some of these variants may have functional consequences and may therefore predispose to or protect against HTG or HTG-related disorders. However, such situations would not affect the pathological relevance of the two novel LPL frameshift coding variants and hence would not alter the main conclusions of this study. Consequently, those variants with an allele frequency of ≥ 1% will not be discussed further in the manuscript.
Exploration of the LPL frameshift coding variants reported thus far
We collated 53 previously reported LPL frameshift coding variants (Table 1) through a combination of data acquired from HGMD, PubMed keyword search and cross-reference examination. Here, it should be emphasized that c.247_249 + 1del was included as a frameshift coding variant since it could be alternatively described as c.246_249del (i.e., deletion of the last four nucleotides of exon 2; Supplementary Fig. 1).
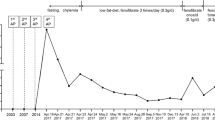
The 53 previously reported LPL variants, together with the 2 newly reported events, were spatially positioned according to their affected exons (Fig. 3). Allowing for variable exon size, a paucity of frameshift coding variants was evident in exon 9 compared to the preceding exons. However, this may represent a chance finding owing to the small sample size.
Exon locations of the 55 LPL frameshift coding variants reported to date. The two novel variants reported in the present study are highlighted in bold. c.77_88 + 1del and c.247_249 + 1del were included because they can be alternatively described as c.76_88del and c.246_249del, respectively. Bars indicate exons. Note that for exons 1 and 10, only the coding sequences are shown. c.positions, start and end coding positions of each exon in accordance with NM_000237.3
We reviewed the corresponding original reports with respect to variant zygosity and the patient’s clinical and laboratory characteristics for each variant (Table 1). Two variants (c.247_249 + 1del [33] and c.384delinsTGGGCT [40]) were “unknown” for zygosity status since we were unable to access the full texts of the original publications. The zygosity status of two other variants (c.438del [41] and c.708del [46]) was “uninformative” due to the lack of relevant information in the original publications. These four variants were therefore excluded from further discussion in terms of genotype–phenotype relationships. Of the 51 variants informative for zygosity, 30 were detected as simple heterozygotes, 12 were detected as homozygotes, and 9 were detected as compound heterozygotes.
Genotype–phenotype correlations in individuals with simple heterozygous variants
Simple heterozygous LPL frameshift coding variants were almost invariably reported in patients with severe HTG and HTG-related diseases such as HTG-AP or HTG-AP in pregnancy. Ages at genetic analysis in these patients, whenever informative, were almost invariably > 20 years. c.483delA represents a notable exception: it was identified in a 5-month-old girl with glycogen storage disease type Ib, and the carrier was found to have severe HTG during laboratory tests in relation to her primary disease [42]. It is possible that glycogen storage disease type Ib may have precipitated the early-onset occurrence of severe HTG in this particular case. Alternatively, this patient may harbor additional as yet undiscovered pathogenic variant(s) in the LPL gene or other HTG-related genes.
Genotype–phenotype correlations in individuals with homozygous variants
Of the 12 homozygous variants identified, 11 can be assigned as causative for typical FCS or LPL deficiency based upon disease phenotype, age of disease onset and/or in vivo LPL activity (Table 1). However, the remaining variant, c.767_768insTAAATATT, was identified in a 25-year-old woman with HTG-AP [20]. The patient reported abdominal pain on two occasions in the previous two years but otherwise had no symptoms of FCS. This rather mild phenotype (by reference to typical FCS) was accounted for by the fact that c.767_768insTAAATATT turned out to be an in-frame variant at the mRNA level, as revealed by RT‒PCR analysis of RNA prepared from the patient’s peripheral blood cells. Specifically, c.767_768insTAAATATT abolished the physiological GT donor site of intron 5 while creating a new splice donor site spanning the 5’ insertion junction, resulting in the generation of a transcript with a 9-bp in-frame deletion (precisely, the deletion of the last 9 nucleotides of exon 5 of the wild-type LPL gene); the mutant transcript would encode a protein with an in-frame deletion of 3 amino acids (i.e., Gly256, Leu257 and Gly258); the mutant protein lacking the three amino acids has been considered to be partially functional [20]. Thanks to the availability of the RT‒PCR analysis data, c.767_768insTAAATATT could confidently be termed p.Gly256_Gly258del at the protein level. Otherwise, it would have been termed p.(Leu257Lysfs*10) in accordance with LUMC Mutalyzer 3.
In summary, of the 12 frameshift coding variants identified in the homozygous state, one (c.767_768insTAAATATT) was conclusively demonstrated to retain residual LPL function based upon both a combination of clinical information and functional analysis data.
Genotype–phenotype correlations in individuals with compound heterozygous variants
Of the 9 variants identified as components of compound heterozygotes, c.287_288del and c.440_443del were identified in the same subject with FCS, who manifested with failure to thrive and abdominal pain at 3 weeks of age [34]. A third variant, c.840del, which was coinherited with a gross deletion of the LPL gene, was identified in a one-month-old subject with typical FCS [35]. The typical FCS associated with these three frameshift coding variants implied that all three of these variants should result in the complete or almost complete loss of LPL function. For the remaining 6 variants, the LPL variants inherited in trans were invariably missense variants. These six compound heterozygous variants will now be addressed individually.
c.128dup and p.Asn318Ser: these two variants were found in a 29-year-old patient with eruptive cutaneous xanthomata and an elevated plasma TG concentration [26]. This late onset of disease could in principle be accounted for by the residual function of p.Asn318Ser, which had been experimentally determined to exhibit 60% wild-type activity [27].
c.133_143del and p.Gly215Glu: their carrier had barely detectable LPL activity (< 1% of control levels), exhibited marked HTG at birth and was diagnosed as having FCS in childhood [28]. Consistent with this picture, p.Gly215Glu was experimentally determined to lead to a near complete functional loss of LPL [29, 30].
c.290_293delinsGG and p.Leu313Pro: the male carrier was described to have FCS [36]. However, he was subjected to genetic analysis at the age of 67, having previously reported eruptive xanthomata and chylomicronemia during an episode of AP at the age of 53. Moreover, the patient’s plasma LPL activity was found to be 6.6% of that of controls. These pieces of clinical and biological evidence converged with the conclusion that the patient had a milder phenotype than typical FCS. However, this comparatively mild phenotype would be at odds with p.Leu313Pro’s experimentally determined LPL activity (i.e., < 1% of wild-type [36]). To account for this discrepancy, we speculate either that c.290_293delinsGG may retain some residual LPL function or that the in vitro determined functional loss of the p.Leu313Pro missense variant may not reflect the variant’s in vivo properties.
c.334dup and p.Arg102Thr: these variants were found in a one-month-old baby exhibiting severe HTG [38]. Consistent with this phenotype, both variants were experimentally shown to result in the complete functional loss of the affected LPL allele [38].
c.373dup and p.His273Arg: these variants were identified in a 3-year-old child with severe HTG [39]. Consistent with this early onset of disease, p.His273Arg was experimentally determined to exhibit 2% wild-type activity [39].
c.953del and p.Ile221Thr: the male carrier of these variants exhibited a relatively mild clinical phenotype compared to typical FCS [50]. First, he was genetically tested for severe HTG at the age of 33, having not previously reported any other symptoms of FCS. Second, his plasma LPL activity was 7.5% of that of controls. However, p.Ile221Thr was experimentally shown to be associated with an almost complete loss of LPL activity by two different studies [51, 52], a finding supported by two clinical findings. First, p.Ile221Thr homozygosity was found in a patient with LPL deficiency (patient presented at the age of 4 years with a history of hepatosplenomegaly and abdominal pain; plasma lipid analysis revealed chylomicronemia with TG levels in excess of 30 mmol/L; plasma LPL activity in this patient was undetectable) [51]. Second, p.Ile221Thr and another missense variant, p.Arg270His (experimentally shown to be associated with a complete functional loss variant), were identified in a typical FCS patient who exhibited HTG at birth, had recurrent episodes of abdominal pain and pancreatitis and was noted to have eruptive xanthomas, lipemia retinalis, and splenomegaly throughout childhood [52]. The in vitro functional analysis data and clinical information firmly established that p.Ile221Thr caused complete functional loss of the affected allele. Consequently, the mild phenotype of the c.953del and p.Ile221Thr compound heterozygote should be conferred by the c.953del allele, which might retain some residual LPL function.
In short, of the 9 frameshift coding variants identified in the compound heterozygous state, one (c.953del) was reasoned to retain some residual LPL function.
Exploring the possibility that some LPL frameshift coding variants may generate “in-frame” transcripts
As mentioned earlier, c.767_768insTAAATATT homozygosity was associated with a mild phenotype. Consistent with this, c.767_768insTAAATATT has been experimentally shown to affect splicing, thereby generating a transcript with a 9-bp in-frame deletion [20]. This prompted us to explore whether some other LPL frameshift coding variants could have a similar effect. To this end, we predicted the potential impact of all 55 LPL variants by means of SpliceAI (Supplementary Fig. 2). Seven variants were predicted to have at least one Δ score of > 0.20. These seven variants will be addressed first.
c.767_768insTAAATATT
This variant was predicted both to disrupt the physiological splice donor site of intron 5 (Δ score of donor loss, 0.85; premRNA position, 8 bp) and to create a new splice donor site spanning the 5’ insertion junction (Δ score of donor gain, 1.0; premRNA position, -1 bp) (Supplementary Fig. 2). These predictions are entirely consistent with the findings from the RT‒PCR analysis of patient-derived blood cells [20].
Three variants with high Δ scores but with no impact on splicing
Three variants (i.e., c.76_88 (HGVS name, c.77_88 + 1del), c.246_249del (HGVS name, c.247_249 + 1del) and c.1138_1139del) were similar in two respects. First, all variants served to delete the last nucleotides of the exons they affected. Second, they were predicted to have the highest Δ scores in terms of both splicing types (i.e., donor loss and donor gain) and values (0.99 to 1.00) (Supplementary Fig. 2). Evaluations of the corresponding donor gain and loss positions, however, revealed that their respective wild-type and mutant pre-mRNA sequences did not differ in terms of their consequences for splicing. Taking c.76_88 as an example (Fig. 2d), a Δ score of 0.99 for donor loss and a Δ score of 0.99 for donor gain suggested that the deletion allele had the same potential for splicing as the wild-type allele. The donor loss at the pre-mRNA position 13 bp in the context of the wild-type allele refers to c.88, whereas the donor gain at pre-mRNA position 0 bp in the context of the deletion allele refers to c.75. This indicates that the wild-type and c.76_88 pre-mRNAs were identical in terms of intron 1 splicing, as depicted in Fig. 2c. The mutant c.76_88del mRNA sequence (lacking the last 13 nucleotides of exon 1 compared to the wild-type transcript) would thus be predicted to encode a significantly truncated and nonfunctional protein, p.(Ala26Lysfs*14).
In short, the three variants did not affect splicing despite their very high Δ scores, thereby excluding the possibility of generating aberrantly spliced but “in-frame” transcripts. In other words, all three variants are expected to result in the complete functional loss of their affected alleles. Here, it should be noted that one of these variants was informative with respect to in vivo LPL activity; consistent with our predictions, both c.1138_1139del homozygotes exhibited zero plasma LPL activity [54].
One variant potentially affects splicing and leads to the generation of some “in-frame” transcripts
C.94_98del can be alternatively described as c.93_97del, c.92_96del or c.91_95del (Fig. 4a). Using c.91_95del for prediction, the variant had an acceptor gain Δ score of 0.53 (at position 8 bp) (Fig. 4b), indicating the activation of a cryptic acceptor site immediately after the deleted nucleotides (Fig. 4c). The aberrantly spliced transcript would be predicted to lack the first 9 nucleotides of exon 2 (Fig. 4c), thereby encoding a protein with a missense variant (p.Gln30His) followed by the deletion of three amino acids (p.Arg31_Asp33del) (Fig. 4d). Given that these changes are located within the amino terminus of the mature LPL protein (starting at p.Ala28), it is highly likely that the mutant protein would retain some residual function. Unfortunately, this postulate cannot be confirmed (or refuted) by available clinical genetics data because c.94_98del was reported in a subject with HTG in the heterozygous state [25]. HTG, unlike autosomal recessive FCS, is a complex and quantitative trait. Finally, it should be noted that c.94_98del was not predicted by SpliceAI to disrupt any physiological splice donor or acceptor sites (Fig. 4b). Consequently, c.94_98del may generate a mixture of “normally spliced but frameshift transcripts” and “aberrantly spliced but in-frame transcripts”.
Possible residual function of the LPL c.94_98del variant. a Illustration showing that c.94_98del (nomenclature in accordance with Human Genome Variation Society (HGVS) recommendations) can be alternatively described as c.93_97del, c.92_96del or c.91_95del. The exon 1 sequence is shown in uppercase letters, whereas the intron 1 sequence is shown in lowercase letters. The canonical 3′ splice site ag dinucleotide is highlighted in bold and blue. Deleted nucleotides in the different nomenclature versions are barred and red. b SpliceAI-predicted results for c.91_95del. c LPL exon 2 and flanking intronic sequences. The exon 1 sequence is shown in uppercase letters, whereas intronic sequences are shown in lowercase letters. The physiological obligate acceptor and donor dinucleotides (ag and gt) are highlighted in blue. The c.91_95del variant (red and barred) was predicted by SpliceAI to activate a downstream cryptic splice acceptor site (highlighted in blue and underlined). The use of this cryptic splice acceptor site would result in a transcript lacking the first 9 bp of exon 2. d Alignment of the mutant and wild-type LPL preproteins
Two variants potentially affecting splicing but that do not generate “in-frame” transcripts
C.899_921dup had a donor loss score of 0.25 and a donor gain score of 0.41 (Supplementary Fig. 3). This suggested that the variant allele might generate an aberrantly spliced transcript in addition to the “normally spliced but frameshift transcript”. However, this aberrantly spliced transcript is unlikely to encode a protein product with any LPL function due to the splicing out of the last 149 (not divisible by 3) nucleotides of exon 6 (Supplementary Fig. 3).
c.1160_1161insT had an acceptor gain score of 0.43 (Supplementary Fig. 4). The aberrantly spliced transcript is also unlikely to encode a protein product with any LPL function due to its splicing out of the first 47 (not divisible by 3) nucleotides of exon 8 (Supplementary Fig. 4).
c.953del is among the variants that were not predicted to affect splicing
None of the remaining 48 variants were predicted to have a Δ score of > 0.20 (Supplementary Fig. 2). Interestingly, c.953del, which was previously thought to retain some residual LPL function, was among these variants. c.953del had very low donor loss and gain scores (0.07 and 0.08, respectively; Supplementary Fig. 2).
Discussion
LPL is one of the most extensively studied human disease genes. Hundreds of loss-of-function LPL variants resulting from the study of FCS, HTG or HTG-related diseases have been reported in the literature in different combinations and permutations [16]. Herein, subsequent to the identification of two novel LPL frameshift coding variants in Chinese patients with HTG-AP or HTG-AP in pregnancy, we embarked on an exploration of the genotype–phenotype relationship in relation to the LPL frameshift coding variants reported to date. This analysis generated some interesting findings. First, the study of biallelic variants involving LPL frameshift coding variants in cases with typical FCS or milder forms of the disease generated important insights into the clinical importance of the residual function of LPL. Based upon current data on genotype–phenotype correlations, we conclude that 6–7% residual LPL function could significantly delay the disease onset age of FCS as well as reduce the occurrence rate of FCS-associated syndromes. This is comparable to the situation evident with autosomal recessive cystic fibrosis, where 5% normal CFTR gene expression is sufficient to prevent the pulmonary manifestations of the disease [59]. Second, whereas a large majority of LPL frameshift coding variants completely disrupt gene function through their "frameshift" nature, a small fraction of these variants may act wholly or partly as "in-frame" variants, leading to the generation of protein products with some LPL function. Third, SpliceAI has been widely used to predict the potential effects of different types of variants in many disease genes. For example, we have recently employed it to aid the classification of pancreatitis-associated PRSS1 [60] and PNLIP [61]variants. Herein, SpliceAI perfectly predicted the splicing effect of c.767_768insTAAATATT and suggested that c.94_98del may be capable of generating some “in-frame” transcripts. In contrast, c.953del, which was reasoned by us to retain residual function, was not predicted by SpliceAI to be capable of generating “in-frame” transcripts. These latter two variants would be interesting candidates for in vitro functional analysis.
The frameshift coding sequence variants studied here were defined solely on the basis of their DNA sequence change (see Introduction). Given that this type of variant is not limited to LPL, insights generated from this study could have implications for the genotype–phenotype relationship of frameshift coding sequence variants in other disease genes. Herein, it is worth noting that other types of variants, such as missense and synonymous variants, may also lead to "frameshift" or "in-frame" changes at the RNA level by affecting pre-mRNA splicing, but this lies out within the scope of the current study.
Study strengths and limitations
The strengths of our study were that (i) we reported two novel variants and (ii) we performed the first comprehensive exploration of genotype–phenotype relationships for the LPL frameshift coding variants reported thus far. One limitation of our study was the relatively small sample size.
Conclusions
In this study, we reported 2 novel LPL frameshift coding variants, followed by an exploration of genotype–phenotype relationships for the LPL frameshift coding variants reported to date. Careful evaluation of the 55 LPL frameshift coding variants with respect to their clinical and genetic data generated several novel insights, especially in relation to the importance of residual LPL function in modifying the age of disease onset and subsequent clinical expression in the context of autosomal recessive FCS.
Availability of data and materials
All supporting data are available within the article or its supplemental material.
Abbreviations
- AP:
-
Acute pancreatitis
- APOA5:
-
Apolipoprotein A5
- APOC2:
-
Apolipoprotein C2
- FCS:
-
Familial chylomicronemia syndrome
- gnomAD:
-
The Genome Aggregation Database
- GPIHBP1:
-
Glycosylphosphatidylinositol-anchored high density lipoprotein-binding protein 1
- HGMD:
-
Human Gene Mutation Database
- HGVS:
-
Human Genome Variation Society
- HTG:
-
Hypertriglyceridemia
- HTG-AP:
-
Hypertriglyceridemia-related acute pancreatitis
- LMF1:
-
Lipase maturation factor 1
- LPL:
-
Lipoprotein lipase
- LUMC:
-
Leiden University Medical Center
- NI:
-
Not informative
- PCR:
-
Polymerase chain reaction
- TG:
-
Triglyceride
References
Wion KL, Kirchgessner TG, Lusis AJ, Schotz MC, Lawn RM. Human lipoprotein lipase complementary DNA sequence. Science. 1987;235:1638–41.
Deeb SS, Peng RL. Structure of the human lipoprotein lipase gene. Biochemistry. 1989;28:4131–5.
Kersten S. Physiological regulation of lipoprotein lipase. Biochim Biophys Acta. 2014;1841:919–33.
Young SG, Fong LG, Beigneux AP, Allan CM, He C, Jiang H, Nakajima K, Meiyappan M, Birrane G, Ploug M. GPIHBP1 and lipoprotein lipase, partners in plasma triglyceride metabolism. Cell Metab. 2019;30:51–65.
Baass A, Paquette M, Bernard S, Hegele RA. Familial chylomicronemia syndrome: an under-recognized cause of severe hypertriglyceridaemia. J Intern Med. 2020;287:340–8.
Nordestgaard BG, Abildgaard S, Wittrup HH, Steffensen R, Jensen G, Tybjaerg-Hansen A. Heterozygous lipoprotein lipase deficiency: frequency in the general population, effect on plasma lipid levels, and risk of ischemic heart disease. Circulation. 1997;96:1737–44.
Perera SD, Wang J, McIntyre AD, Dron JS, Hegele RA. The longitudinal triglyceride phenotype in heterozygotes with LPL pathogenic variants. J Clin Lipidol. 2023;17:87–93.
Laufs U, Parhofer KG, Ginsberg HN, Hegele RA. Clinical review on triglycerides. Eur Heart J. 2020;41:99–109c.
Pu W, Luo G, Chen T, Jing L, Hu Q, Li X, Xia H, Deng M, Lu M, Chen X. A 5-year retrospective cohort study: epidemiology, etiology, severity, and outcomes of acute pancreatitis. Pancreas. 2020;49:1161–7.
Li X, Ke L, Dong J, Ye B, Meng L, Mao W, Yang Q, Li W, Li J. Significantly different clinical features between hypertriglyceridemia and biliary acute pancreatitis: a retrospective study of 730 patients from a tertiary center. BMC Gastroenterol. 2018;18:89.
Jin M, Bai X, Chen X, Zhang H, Lu B, Li Y, Lai Y, Qian J, Yang H. A 16-year trend of etiology in acute pancreatitis: The increasing proportion of hypertriglyceridemia-associated acute pancreatitis and its adverse effect on prognosis. J Clin Lipidol. 2019;13(947–953):e941.
Yang Q, Pu N, Li XY, Shi XL, Chen WW, Zhang GF, Hu YP, Zhou J, Chen FX, Li BQ, et al. Digenic inheritance and gene-environment interaction in a patient with hypertriglyceridemia and acute pancreatitis. Front Genet. 2021;12:640859.
Pu N, Yang Q, Shi XL, Chen WW, Li XY, Zhang GF, Li G, Li BQ, Ke L, Tong ZH, et al. Gene-environment interaction between APOA5 c.553G>T and pregnancy in hypertriglyceridemia-induced acute pancreatitis. J Clin Lipidol. 2020;14:498–506.
Chen WW, Yang Q, Li XY, Shi XL, Pu N, Lu GT, Tong ZH, Chen JM, Li WQ. Identification of a novel and heterozygous LMF1 nonsense mutation in an acute pancreatitis patient with severe hypertriglyceridemia, severe obesity and heavy smoking. Lipids Health Dis. 2019;18:68.
Li XY, Pu N, Chen WW, Shi XL, Zhang GF, Ke L, Ye B, Tong ZH, Wang YH, Liu G, et al. Identification of a novel LPL nonsense variant and further insights into the complex etiology and expression of hypertriglyceridemia-induced acute pancreatitis. Lipids Health Dis. 2020;19:63.
Stenson PD, Mort M, Ball EV, Chapman M, Evans K, Azevedo L, Hayden M, Heywood S, Millar DS, Phillips AD, Cooper DN. The Human Gene Mutation Database (HGMD®): optimizing its use in a clinical diagnostic or research setting. Hum Genet. 2020;139:1197–207.
Jaganathan K, Kyriazopoulou Panagiotopoulou S, McRae JF, Darbandi SF, Knowles D, Li YI, Kosmicki JA, Arbelaez J, Cui W, Schwartz GB, et al. Predicting splicing from primary sequence with deep learning. Cell. 2019;176:535–48.
den Dunnen JT, Dalgleish R, Maglott DR, Hart RK, Greenblatt MS, McGowan-Jordan J, Roux AF, Smith T, Antonarakis SE, Taschner PE. HGVS recommendations for the description of sequence variants: 2016 update. Hum Mutat. 2016;37:564–9.
Lefter M, Vis JK, Vermaat M, den Dunnen JT, Taschner PEM, Laros JFJ. Mutalyzer 2: next generation HGVS nomenclature checker. Bioinformatics. 2021;37:2811–7.
Laurie AD, Kyle CV. A novel frameshift mutation in the lipoprotein lipase gene is rescued by alternative messenger RNA splicing. J Clin Lipidol. 2017;11:357–61.
Lin JH, Tang XY, Boulling A, Zou WB, Masson E, Fichou Y, Raud L, Le Tertre M, Deng SJ, Berlivet I, et al. First estimate of the scale of canonical 5’ splice site GT>GC variants capable of generating wild-type transcripts. Hum Mutat. 2019;40:1856–73.
Leman R, Gaildrat P, Le Gac G, Ka C, Fichou Y, Audrezet MP, Caux-Moncoutier V, Caputo SM, Boutry-Kryza N, Leone M, et al. Novel diagnostic tool for prediction of variant spliceogenicity derived from a set of 395 combined in silico/in vitro studies: an international collaborative effort. Nucleic Acids Res. 2018;46:7913–23.
Jin JL, Sun D, Cao YX, Zhang HW, Guo YL, Wu NQ, Zhu CG, Gao Y, Dong QT, Liu G, et al. Intensive genetic analysis for Chinese patients with very high triglyceride levels: Relations of mutations to triglyceride levels and acute pancreatitis. EBioMedicine. 2018;38:171–7.
Wang J, Cao H, Ban MR, Kennedy BA, Zhu S, Anand S, Yusuf S, Pollex RL, Hegele RA. Resequencing genomic DNA of patients with severe hypertriglyceridemia (MIM 144650). Arterioscler Thromb Vasc Biol. 2007;27:2450–5.
Hou YC, Yu HC, Martin R, Cirulli ET, Schenker-Ahmed NM, Hicks M, Cohen IV, Jonsson TJ, Heister R, Napier L, et al. Precision medicine integrating whole-genome sequencing, comprehensive metabolomics, and advanced imaging. Proc Natl Acad Sci U S A. 2020;117:3053–62.
Overgaard M, Brasen CL, Svaneby D, Feddersen S, Nybo M. Familial lipoprotein lipase deficiency: a case of compound heterozygosity of a novel duplication (R44Kfs*4) and a common mutation (N291S) in the lipoprotein lipase gene. Ann Clin Biochem. 2013;50:374–9.
Busca R, Peinado J, Vilella E, Auwerx J, Deeb SS, Vilaro S, Reina M. The mutant Asn291–>Ser human lipoprotein lipase is associated with reduced catalytic activity and does not influence binding to heparin. FEBS Lett. 1995;367:257–62.
Reina M, Brunzell JD, Deeb SS. Molecular basis of familial chylomicronemia: mutations in the lipoprotein lipase and apolipoprotein C-II genes. J Lipid Res. 1992;33:1823–32.
Emi M, Wilson DE, Iverius PH, Wu L, Hata A, Hegele R, Williams RR, Lalouel JM. Missense mutation (Gly––Glu188) of human lipoprotein lipase imparting functional deficiency. J Biol Chem. 1990;265:5910–6.
Peterson J, Ayyobi AF, Ma Y, Henderson H, Reina M, Deeb SS, Santamarina-Fojo S, Hayden MR, Brunzell JD. Structural and functional consequences of missense mutations in exon 5 of the lipoprotein lipase gene. J Lipid Res. 2002;43:398–406.
Evans D, Arzer J, Aberle J, Beil FU. Rare variants in the lipoprotein lipase (LPL) gene are common in hypertriglyceridemia but rare in Type III hyperlipidemia. Atherosclerosis. 2011;214:386–90.
Benlian P, Foubert L, Gagne E, Bernard L, De Gennes JL, Langlois S, Robinson W, Hayden M. Complete paternal isodisomy for chromosome 8 unmasked by lipoprotein lipase deficiency. Am J Hum Genet. 1996;59:431–6.
Rahalkar AR, Giffen F, Har B, Ho J, Morrison KM, Hill J, Wang J, Hegele RA, Joy T. Novel LPL mutations associated with lipoprotein lipase deficiency: two case reports and a literature review. Can J Physiol Pharmacol. 2009;87:151–60.
Foubert L, De Gennes JL, Benlian P, Truffert J, Miao L, Hayden MR. Compound heterozygosity for frameshift mutations in the gene for lipoprotein lipase in a patient with early-onset chylomicronemia. Hum Mutat. 1998;(1):141–4.
Rabacchi C, Pisciotta L, Cefalu AB, Noto D, Fresa R, Tarugi P, Averna M, Bertolini S, Calandra S. Spectrum of mutations of the LPL gene identified in Italy in patients with severe hypertriglyceridemia. Atherosclerosis. 2015;241:79–86.
Benlian P, De Gennes JL, Foubert L, Zhang H, Gagne SE, Hayden M. Premature atherosclerosis in patients with familial chylomicronemia caused by mutations in the lipoprotein lipase gene. N Engl J Med. 1996;335:848–54.
Ariza MJ, Rioja J, Ibarretxe D, Camacho A, Diaz-Diaz JL, Mangas A, Carbayo-Herencia JA, Ruiz-Ocana P, Lamiquiz-Moneo I, Mosquera D, et al. Molecular basis of the familial chylomicronemia syndrome in patients from the National Dyslipidemia Registry of the Spanish Atherosclerosis Society. J Clin Lipidol. 2018;12(1482–1492): e1483.
Hu X, Chen L, Gong C, Guo J, Chen Y, Wang Q, Guo R, Li W, Hao C. Whole exome sequencing for non-selective pediatric patients with hyperlipidemia. Gene. 2021;768:145310.
Martin-Campos JM, Julve J, Roig R, Martinez S, Errico TL, Martinez-Couselo S, Escola-Gil JC, Mendez-Gonzalez J, Blanco-Vaca F. Molecular analysis of chylomicronemia in a clinical laboratory setting: diagnosis of 13 cases of lipoprotein lipase deficiency. Clin Chim Acta. 2014;429:61–8.
Henderson HE, Devlin R, Peterson J, Brunzell JD, Hayden MR. Frameshift mutation in exon 3 of the lipoprotein lipase gene causes a premature stop codon and lipoprotein lipase deficiency. Mol Biol Med. 1990;7:511–7.
Marmontel O, Charriere S, Simonet T, Bonnet V, Dumont S, Mahl M, Jacobs C, Nony S, Chabane K, Bozon D, et al. Single, short in-del, and copy number variations detection in monogenic dyslipidemia using a next-generation sequencing strategy. Clin Genet. 2018;94:132–40.
Wang F, Wang F, Zhou X, Yi Y, Zhao J. A novel lipoprotein lipase mutation in an infant with glycogen storage disease type-Ib and severe hypertriglyceridemia. Front Pediatr. 2021;9: 671536.
Pruneta-Deloche V, Marcais C, Perrot L, Sassolas A, Delay M, Estour B, Lagarde M, Moulin P. Combination of circulating antilipoprotein lipase (Anti-LPL) antibody and heterozygous S172 fsX179 mutation of LPL gene leading to chronic hyperchylomicronemia. J Clin Endocrinol Metab. 2005;90:3995–8.
Di Filippo M, Marcais C, Charriere S, Marmontel O, Broyer M, Delay M, Merlin M, Nollace A, Valero R, Lagarde M, et al. Post-heparin LPL activity measurement using VLDL as a substrate: a new robust method for routine assessment of plasma triglyceride lipolysis defects. PLoS ONE. 2014;9: e96482.
Marmontel O, Rollat-Farnier PA, Wozny AS, Charriere S, Vanhoye X, Simonet T, Chatron N, Collin-Chavagnac D, Nony S, Dumont S, et al. Development of a new expanded next-generation sequencing panel for genetic diseases involved in dyslipidemia. Clin Genet. 2020;98:589–94.
Murthy V, Julien P, Gagne C. Molecular pathobiology of the human lipoprotein lipase gene. Pharmacol Ther. 1996;70:101–35.
Takagi A, Ikeda Y, Tsutsumi Z, Shoji T, Yamamoto A. Molecular studies on primary lipoprotein lipase (LPL) deficiency. One base deletion (G916) in exon 5 of LPL gene causes no detectable LPL protein due to the absence of LPL mRNA transcript. J Clin Invest. 1992;89:581–91.
Pingitore P, Lepore SM, Pirazzi C, Mancina RM, Motta BM, Valenti L, Berge KE, Retterstol K, Leren TP, Wiklund O, Romeo S. Identification and characterization of two novel mutations in the LPL gene causing type I hyperlipoproteinemia. J Clin Lipidol. 2016;10:816–23.
Surendran RP, Visser ME, Heemelaar S, Wang J, Peter J, Defesche JC, Kuivenhoven JA, Hosseini M, Peterfy M, Kastelein JJ, et al. Mutations in LPL, APOC2, APOA5, GPIHBP1 and LMF1 in patients with severe hypertriglyceridaemia. J Intern Med. 2012;272:185–96.
Kobayashi J, Nagashima I, Taira K, Hikita M, Tamura K, Bujo H, Morisaki N, Saito Y. A novel frameshift mutation in exon 6 (the site of Asn 291) of the lipoprotein lipase gene in type I hyperlipidemia. Clin Chim Acta. 1999;285:173–82.
Henderson HE, Ma Y, Hassan MF, Monsalve MV, Marais AD, Winkler F, Gubernator K, Peterson J, Brunzell JD, Hayden MR. Amino acid substitution (Ile194----Thr) in exon 5 of the lipoprotein lipase gene causes lipoprotein lipase deficiency in three unrelated probands. Support for a multicentric origin. J Clin Invest. 1991;87:2005–11.
Dichek HL, Fojo SS, Beg OU, Skarlatos SI, Brunzell JD, Cutler GB Jr, Brewer HB Jr. Identification of two separate allelic mutations in the lipoprotein lipase gene of a patient with the familial hyperchylomicronemia syndrome. J Biol Chem. 1991;266:473–7.
Hu Y, Ren Y, Luo RZ, Mao X, Li X, Cao X, Guan L, Chen X, Li J, Long Y, et al. Novel mutations of the lipoprotein lipase gene associated with hypertriglyceridemia in members of type 2 diabetic pedigrees. J Lipid Res. 2007;48:1681–8.
Nierman MC, Peter J, Khoo KL, Defesche JC. Lipoprotein lipase gene analyses in one Turkish family and three different Chinese families with severe hypertriglyceridaemia: one novel and several established mutations. J Inherit Metab Dis. 2006;29:686.
Cheema H, Bertoli-Avella AM, Skrahina V, Anjum MN, Waheed N, Saeed A, Beetz C, Perez-Lopez J, Rocha ME, Alawbathani S, et al. Genomic testing in 1019 individuals from 349 Pakistani families results in high diagnostic yield and clinical utility. NPJ Genom Med. 2020;5:44.
Kuthiroly S, Yesodharan D, Radhakrishnan N, Ganapathy A, Mannan AU, Hoffmann MM, Nampoothiri S. Lipoprotein lipase deficiency. Indian J Pediatr. 2021;88:147–53.
Rodrigues R, Artieda M, Tejedor D, Martinez A, Konstantinova P, Petry H, Meyer C, Corzo D, Sundgreen C, Klor HU, et al. Pathogenic classification of LPL gene variants reported to be associated with LPL deficiency. J Clin Lipidol. 2016;10:394–409.
Dron JS, Wang J, McIntyre AD, Iacocca MA, Robinson JF, Ban MR, Cao H, Hegele RA. Six years’ experience with LipidSeq: clinical and research learnings from a hybrid, targeted sequencing panel for dyslipidemias. BMC Med Genomics. 2020;13:23.
Raraigh KS, Han ST, Davis E, Evans TA, Pellicore MJ, McCague AF, Joynt AT, Lu Z, Atalar M, Sharma N, et al. Functional assays are essential for interpretation of missense variants associated with variable expressivity. Am J Hum Genet. 2018;102:1062–77.
Masson E, Zou WB, Pu N, Rebours V, Génin E, Wu H, Lin JH, Wang YC, Franco-Chinese GREPAN Study Group, Li ZS, et al. Classification of PRSS1 variants responsible for chronic pancreatitis: An expert perspective from the Franco-Chinese GREPAN Study Group. Pancreatology. 2023;23:491–506.
Masson E, Berthet S, Le Rhun M, Ka C, Autret S, Gourlaouen I, French GREPAN Study Group, Cooper DN, Férec C, et al. Identification of protease-sensitive but not misfolding PNLIP variants in familial and hereditary pancreatitis. Pancreatology. 2023;23:507–11.
Acknowledgements
None.
Funding
This work was supported by the National Natural Science Foundation of China (Nos. 82070669 and 81870441) and the Institut National de la Santé et de la Recherche Médicale (INSERM), France.
Author information
Authors and Affiliations
Contributions
G.Z., Y.H. and Q.Y. designed the study, identified the novel variants, and contributed to mutation collation and manuscript writing. N.P., G.L., J.Z. and Z.T. collected patient data and revised the manuscript. E.M. contributed to mutation collation, SpliceAI prediction and manuscript revision. D.N.C. provided the LPL mutation dataset, analyzed the data, and critically revised the manuscript with important intellectual input. W.L. designed the study, obtained funding and revised the manuscript. J.M.C. designed the study, performed the literature search and SpliceAI predictions, and wrote the manuscript. All authors approved the submitted manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Ethics Committee of Jinling Hospital (2021NZKY-042–01). Written informed consent was obtained from all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplementary Table 1
. Variants with an allele frequency of ≥1% found in the three patients. Supplementary Figure 1. Illustration showing that c.247_249+1del (in accordance with Human Genome Variation Society (HGVS) recommendations) may be alternatively described as c.246_249del. Exon 2 sequence is shown in upper case letters whereas intron 2 sequence is shown in lower case. The canonical 5’ splice site gt dinucleotide is highlighted in bold and blue. The deleted four nucleotides in each nomenclature version are barred. Supplementary Figure 2. SpliceAI predictions for the 55 LPL frameshift coding variants reported to date. Supplementary Figure 3. SpliceAI-predicted impact of the LPL c.899_921dup variant on splicing. (a) SpliceAI predictions. (b) Explanation of the predicted results in the context of the wild-type LPL exon 6 and flanking intronic sequences. Exon 6 sequence is shown in upper case letters whereas intronic sequence is shown in lower case. The physiological obligate acceptor and donor dinucleotides (ag and gt) are highlighted in blue. The 23-bp duplicated sequence is highlighted in red. The LPL c.899_921dup variant was predicted to activate an upstream cryptic donor splice site (highlighted in blue and underlined). The use of this cryptic donor splice site would result in a transcript lacking the last 149 (not divisible by 3) nucleotides (barred) of exon 6. Supplementary Figure 4. SpliceAI-predicted impact of the LPL c.1160_1161insT variant on splicing. (a) SpliceAI predictions. (b) Explanation of the predicted results in the context of the wild-type LPL exon 8 and flanking intronic sequences. Exon 8 sequence is shown in upper case letters whereas intronic sequence is shown in lower case. The physiological obligate splice site acceptor and donor dinucleotides (ag and gt) are highlighted in blue. The LPL c.1160_1161insT variant was predicted to activate a downstream cryptic acceptor splice site (highlighted in red). The use of this cryptic acceptor splice site would result in a transcript lacking the first 47 (not divisible by 3) nucleotides of exon 8.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhang, G., Hu, Y., Yang, Q. et al. Frameshift coding sequence variants in the LPL gene: identification of two novel events and exploration of the genotype–phenotype relationship for variants reported to date. Lipids Health Dis 22, 128 (2023). https://doi.org/10.1186/s12944-023-01898-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12944-023-01898-w