Abstract
Background
The correlation between lipid profiles and sepsis has received increasing attention. The ratio of non-high-density lipoprotein cholesterol to high-density lipoprotein cholesterol (NHHR) is one of the key lipid profiles. However, in-depth exploration of the correlation between NHHR and the mortality risk of patients with sepsis is limited.
Methods
Data from the MIMIC-IV (v2.2) database, we review the NHHR relevance and the sepsis severity index using Spearman’s correlation analysis. Additionally, we research NHHR associated with sepsis patients’ survival rate of 28 days using Cox regression analyses of continuous and categorical models. To further validate our findings, we conducted subgroup and sensitivity analyses.
Results
The study involved 3,142 patients diagnosed with sepsis, according to 28 days after in-hospital survival condition, divided into two groups. In this study, 2932 patients were in the survival group and 210 patients died within 28 days (mortality group). Of note, the mean NHHR of patients in the mortality group exceeded that of the survival group (3.5 vs. 2.9). Additionally, NHHR was positively correlated with the severity index. After adjusting for demographic and laboratory data, an increased NHHR was positively correlated with higher sepsis mortality risk (OR = 1.06; 95% CI: 1.02–1.11; P = 0.013). Subgroup analysis shown the same results. Contributors were be categorized into two groups based on NHHR levels, with a threshold of 2.61. Contrast the mortality risk between low-NHHR group and high-NHHR group, high-NHHR show greater mortality risk on 28-day, 60-day, 90-day, in ICU, and in hospital.
Conclusion
Elevated NHHR is to be correlated with an increased risk of mortality in patients with sepsis. Further research on NHHR may contribute to advancements in sepsis prevention and treatment.
Similar content being viewed by others
Introduction
Sepsis, an urgent medical condition that can be life-threatening, ranks among the leading causes of death globally [1]. Sepsis patients can suffer from tissue damage, organ failure, and even death, particularly among high-risk groups such as the elderly [2, 3]. Despite advancements in treatment, sepsis still carries a high mortality rate, with approximately 270,000 deaths occurring annually in the United States due to sepsis-related complications [4]. Sepsis can arise suddenly and progress quickly, making it challenging to recognize and treat in its early stages [5]. Immediate medical attention is crucial, as the risk of death from sepsis increases with each passing hour [6]. Hence, early detection and effective treatment are essential in managing sepsis and improving patient outcomes.
Recently, the correlation between sepsis and lipid metabolism has attracted increasing attention. Daniel et al. found that hypocholesterolemia in sepsis is a strong predictor of poor outcomes [7]. Rory et al. identified an inverse correlation between total cholesterol (TC), high-density lipoprotein (HDL), and low-density lipoprotein (LDL) concentrations upon admission to critical care and mortality [9]. Alexander et al. found that HDL can protect against sepsis through a variety of processes, including steroid production, eliminating bacteria toxins, maintaining the integrity of the endothelial barrier, and antioxidant and anti-inflammatory properties [10]. Moreover, an observational study revealed that among septic patients admitted to the emergency department, HDL levels on admission predict multiple organ dysfunction syndrome [11]. In another trial involving 64 patients with severe sepsis, we noted that none of the patients with HDL levels of 25 mg/dL on day 3 died, whereas those who did not survive showed a consistent trend toward lower HDL levels [11].
An increasing number of diseases are being linked to NHHR, non-HDL /HDL ratio is emerging as a novel lipid composite biomarker for arteriosclerosis predisposition [12]. Wang et al. found that higher NHHR had a higher risk of nonalcoholic steatohepatitis [13]. Qing et al. discovered a significant correlation between higher NHHR levels and an elevated risk of suicidal ideation [14]. Likely, le et al. discovered that a higher or lower NHHR was linked to an increased risk of 28-day death by analysis of 724 sepsis patients [15]. Research on the correlation between NHHR and sepsis is relatively limited, requiring further clarification of their clinical importance by a larger sample population. Hence, this study aimed to seek out the potential correlation of the NHHR with sepsis mortality risk, aiming to offer more accurate evidence for prognosis assessment and personalized treatment in clinical practice.
Methods
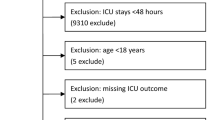
Study population
A flowchart was provided in Fig. 1. This study used data from the period of 2008–2019 at Beth Israel Deaconess Medical Center (BIDMC) of all patients, which is be recorded in the MIMIC IV database (https://physionet.org/content/mimiciv/2.2/). It includes abundant information, such as vital signs, treatments, laboratory results, etc. Personal information is anonymized using random numbers to protect patient privacy (informed permission and ethical approval are not required). Data extraction was performed by one author (Yue Zhang), who complied with access requirements (ID: 53,049,076). In the MIMIC-IV database (v2.2), 76,943 ICU admissions were recorded. Furthermore, 3.0 diagnostic criteria for sepsis, 34,677 patients were be recognized [16]. The exclusion criteria are: (1) age below 18 years or above 80 years (n = 7,813); (2) ICU stay duration of less than 24 h (n = 2,497); (3) records other than the first admission and records from outside the first ICU (n = 7,789); and (4) lack of TC and HDL information (n = 13,466). Finally, 3,142 patients were included in this investigation, which was split into two groups according to whether they died within 28 days.
Data selection
Demographic information (age, sex, race, body mass index (BMI)), vital signs data (respiratory rate (RR), heart rate (HR1), mean blood pressure (MBP), laboratory test results (white blood cell (WBC) count, red blood cell (RBC) count, platelet count, serum creatinine (Scr), blood urea nitrogen (BUN), lactate), comorbidities (hypertension, chronic heart disease (CHD), congestive heart failure (CHF), diabetes, acute kidney injury (AKI), chronic pulmonary disease (COPD), septic shock), treatments (renal replacement therapy (RRT), vasopressor use, albumin use, mechanical ventilation), and risk scoring systems (Charlson Comorbidity Index (CCI), Systemic Inflammatory Response Syndrome (SIRS) score, Oxford Acute Severity of Illness Score (OASIS), Glasgow Coma Scale (GCS), Simplified Acute Physiological Score II (SAPSII), Sequential Organ Failure Assessment (SOFA)) within the first 24 h of ICU admission. Serum lipid indexes of patients on the first day of ICU admission were collected, including TC, HDL, LDL, TG, and non-HDL levels. Data extraction utilized Navicat Premium (version 15) and PostgreSQL (v13.7.1). GitHub code was used to calculate severity scores, assess comorbidities, analyze laboratory markers, and evaluate demographics.
NHHR
The serum lipid data were used to calculate NHHR, and the formula was expressed as NHHR = non-HDL/HDL, where non-HDL refers to the value of TC minus HDL.
Statistical analysis
The report methods for variables are: (1) continuous variable: (1) normally distributed: mean (standard error, SD); (2) not normally distributed: median (interquartile); (2) Categorical variables: Percentages (%). Contrast differences between groups using the t-test, the Mann-Whitney U test, and Chi-square test. To eliminate bias, moving averages were used to calculate variables with missing rates of less than 5% and various interpolation techniques to estimate variables with missing rates of 5 to 15%.
The association between NHHR and the sepsis severity index was explored using Spearman correlation analysis. Cox regression model was be used to assess NHHR with sepsis mortality risk, and the connection between the hazard ratios (HRs) and its 95% confidence interval (CI) was obtained. The NHHR numerical size is divided into four groups, such that one of the lowest quartile arrays sets the benchmark for groups using both a continuous and a categorical model. Without any adjustment in models 1 and 2 to age, race, BMI, RR, MBP, WBC count, RBC count, BUN, and lactate, the correction has carried on. Model 3 added adjustments for diabetes, hypertension, and chronic kidney disease, and Model 4 went a step further by adjusting the treatments for vasoactive medications, albumin, mechanical ventilation, and RRT. The restricted cubic spline model (RCS) was used to set the 5th, 50th, and 95th percentiles of the corresponding distribution of the three nodes to explore the potential nonlinear association between NHHR and the risk of 28-day mortality in patients with sepsis. By subgroup analysis, systematically verified in different BUN, lactate, hypertension, diabetes, RR, MBP, WBC count, RBC count, albumin use, vasopressor use, mechanical ventilation use, and RRT, to validate the consistency of these variables to conclude. Receiver operating characteristic (ROC) curves of NHHR, TC, HDL, non-HDL, LDL, and TG were be analyzed. A binary variable was be created according to the ROC curve cutoff of 2.61 for NHHR. Cox regression models were used to estimate HRs between the two groups. At the same time, the Kaplan-Meier (K-M) survival curves are be performed to contrast the low-NHHR and high-NHHR groups. The studies were undertaken by R software (4.3.2), and values of P under 0.05 are viewed as to be significant.
Results
Demographic information
The baseline data for the mortality groups and survival groups are shown in Table 1. BMI was higher in survivors (29.1 vs. 30.0), while the age (61.2 vs. 64.4), RR (19.3 vs. 20.5), MBP (79.0 vs. 81.9), WBC count (10.1 vs. 11.8), RBC count (3.8 vs. 3.9), BUN (22.5 vs. 26.0), lactate (2.1 vs. 2.7), TC (144.9 vs. 167.0), HDL (38.2 vs. 46.2), TG (141.6 vs.160.6), and non-HDL (106.7 vs. 120.8) were lower in the survival group. However, LDL (3.4 vs. 3.1) was higher in the survival group. The percentages of Asian, White, and Black patients were also lower in the mortality group (Asian: 1.9% vs. 3.9%; White: 51.4% vs. 65.5%; Black: 4.3% vs. 11.7%). The patients of mortality group were less likely to have hypertension (47.4% vs. 29.5%) and diabetes (24.5% vs. 15.7%). On the contrary, the survival group had a low proportion of patients with CKD (6.7% vs. 15.9%). On treatment, the use of vasoactive drugs (6.6% vs. 32.9%), who received mechanical ventilation (90.5% vs. 96.2%) and RRT (8.2% vs. 21.0%) was lower in the survival group. Of note, however, the use of albumin was lower in the mortality group (26.7% vs. 36.8%). Likewise, the NHHR was lower than that of the survival group (3.5 vs. 2.9).
The correlation of NHHR and the severity indices of sepsis
Spearman correlation analysis revealed correlations between NHHR and various severity indices (Table 2). NHHR exhibited a negative correlation with the CCI (P = 0.0003) and GCS (P < 0.0001), and positive correlations with SIRS (P < 0.0001), OASIS (P = 0.0002), and SOFA scores (P < 0.0001). However, its correlation with the SAPSII score was no significant (P = 0.8369).
The correlation of NHHR and the 28-day mortality of sepsis
Through the continuous variable model and category variable model, we assessed the NHHR correlation with mortality risk in patients with sepsis. Higher NHHR is positively correlated with the aggravation of the mortality risk of sepsis. This outcome was significant in the original unadjusted model 1 (HR = 1.07; P = 0.001) and remained significant in model 2 (HR = 1.06; P = 0.006) and model 3 (HR = 1.06; P = 0.013). However, after further adjustments, the statistical significance was weak (HR = 1.05; P = 0.058). Likewise, the categorical models also showed the same results. Further details are provided in Table 3. A nonlinear correlation wasn’t found between NHHR and the 28-day mortality risk of sepsis (P nonlinearity = 0.890) (Supplementary Fig. 1).
Subgroup analysis
As depicted in Fig. 2, subgroup analysis was be used to check on the stability of above results. All of these factors, such as age, ethnicity, BMI, RR, MBP, WBC count, RBC count, BUN, lactate, hypertension, diabetes, use of vasopressors, albumin use, mechanical ventilation use, and RRT, the interaction of the P values was greater than 0.05, which means that the interaction between them is not significant statistically. This conclusion reveals that NHHR the connection between the patients with sepsis mortality, maintains consistency in each population segment.
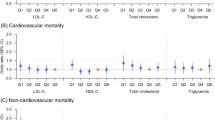
Sensitivity analysis
Given the current body of literature on the impact of various lipid markers on sepsis prognosis, we conducted individual ROC curve analyses for NHHR, TC, HDL, non-HDL, LDL, and TG to determine their predictive value for 28-day mortality. Supplementary Figs. 2–7 displays the six blood lipid indexes of the area under the curve (AUC), including the NHHR (0.621), HDL (0.616), TG (0.605), non-HDL (0.590), TC (0.552), and LDL (0.530). Furthermore, to assess the robustness of the correlation between NHHR and the mortality risk of sepsis patients, according to the threshold point (2.61) determined by the ROC curve, the patients with sepsis were divided into the group with a lower NHHR value and the group with a higher NHHR value (Supplementary Fig. 2). The more data information of the two groups is shown in Supplementary Table 1. As shown in Table 4, we analyzed the correlation between NHHR and the mortality risk of sepsis patients at different time points: (1) 28-day (HR = 1.46; P = 0.006); (2) 60-day (HR = 1.64; P < 0.001); (3) 90-day (HR = 1.54; P < 0.001); (4) ICU mortality (HR = 1.39; P = 0.047); (5) Hospital mortality (HR = 1.61; P = 0.001). Furthermore, the low-NHHR group had a higher survival rate by the K-M curve (Fig. 3).
Discussion
This study explores the correlation between lipid profiles and sepsis mortality risk, focusing particularly on NHHR. Sepsis patients’ NHHR level rise indicates a higher risk of death, which remains consistent across various subgroups. NHHR demonstrates greater potential as a predictive indicator for sepsis patients’ mortality risk than other lipid profiles. To further assess the robustness of the NHHR-sepsis connection, according to the cut-off point determined by the ROC curve, these participants were divided into two groups. Cox model and K-M curve indicated that higher NHHR levels faced a greater risk of death in sepsis patients.
Sepsis is a serious public health challenge, its characteristic is associated with physiology, pathology, and significant abnormal metabolic activity [17]. Sepsis can deteriorate rapidly and become septic shock, the two are closely associated with a significantly increased risk of death [18]. When clinical identification of patients with septic shock, focus on the following indicators: even without obvious loss of blood volume, also need to rely on the blood pressure agents to ensure that not less than 65 mm hg, mean arterial pressure and serum lactic acid concentration is beyond 2 millimoles/l (or > 18 mg/dl) [16]. According to the global estimation, each year about 49 million people suffer from sepsis, including as many as 11 million people unfortunately die due to sepsis-related reasons [19]. A study analyzing data from 2010 to 2016 revealed that the overall mortality rate for sepsis patients in U.S. hospitals was 12.5% [20]. Among adults aged 65 and older in the U.S. in 2019, the sepsis-related death rate was 277.4 per 100,000 population [21]. Meanwhile, survivors of sepsis often face long-term complications and an elevated risk of rehospitalization and death [22]. However, the treatment of sepsis patients typically involves prompt antibiotic administration and supportive care [23]. As an urgent and serious medical condition, sepsis needs immediate attention. Delay in treatment may lead to organ failure and even fatal consequences [24]. Therefore, early detection and treatment are crucial in managing sepsis and preventing serious consequences, such as septic shock and organ failure.
The study revealed a lipid and lipoprotein metabolism imbalance in sepsis disease plays a key role in the process of development [7]. Sepsis-induced disturbances in lipid and lipoprotein metabolism lead to alterations in the composition, concentration, and clearance of plasma fatty acids and triglycerides [25]. Proteomic studies have shown that sepsis induced by community-acquired pneumonia alters lipid metabolism [26]. Research suggests that patients with sepsis in TC, HDL, LDL, and apolipoprotein ApoA1, ApoB100 and 1 (PON1) levels of oxygen phosphorus enzyme were showing abnormal changes [27]. Elevated triglyceride levels have been correlated with a poorer prognosis and higher mortality rates in sepsis patients, and they have been identified as an independent predictor of death in sepsis [28]. HDL levels significantly decrease in septic patients, and lower HDL levels are correlated with worse clinical outcomes and higher mortality rates [29]. HDL has several protective mechanisms against sepsis, including binding and neutralizing bacterial toxins like lipopolysaccharide (LPS), promoting clearance of LPS from the body, reducing inflammation and oxidative stress, and maintaining endothelial barrier integrity [10, 30]. Dysfunctional HDL (dysHDL) lacks these protective qualities and has been correlated with worse outcomes and organ failure in sepsis [31]. In conclusion, high-density lipoprotein (HDL) plays a key protective effect in sepsis, and its metabolic disturbance is considered to be a central feature in the pathophysiological process of sepsis.
The NHHR, a recently incorporated metric, outperforms standard lipid indicators in assessing the severity of atherosclerosis [32]. The latest research results show that the combined detection of non-HDL and HDL, in predict atherosclerosis disease better than traditional lipid indicators [33]. Kwok, put forward by compared with other indicators of lipids, NHHR in the prediction of nonalcoholic fatty liver disease (NAFLD) shows a higher potential [34]. The high NHHR has also been correlated with the risk and severity of other conditions like gallbladder polyp formation [35] and abdominal aortic aneurysm [36]. The study found that patients with sepsis of HDL/HDL ratio on the high side and adverse clinical outcomes and a higher risk of death are closely related [15]. Consistent with our study, we found that sepsis patients with higher NHHR levels experienced higher all-cause mortality, and higher NHHR levels are correlated with more severe sepsis. In addition, in terms of predicting the prognosis of patients with sepsis, NHHR is particularly prominent, and its predictive utility exceeds other conventional lipid measurements. This study further confirmed that NHHR for evaluating sepsis patients of the risk for all-cause mortality indicators has better performance. Mark et al. Studies have shown that inhibiting cholesterol ester transfer protein can effectively maintain HDL levels, and positive influence on the prognosis of patients with sepsis [37]. Adrian and others through the study revealed a reorganization of the high-density lipoprotein (rHDL) can successfully prevent kidney damage in rats induced by endotoxin and dysfunction [38]. Moreover, rHDL is expected to pass directly combined with LPS weaken the active, and reduce the expression of CD14 monocyte surface, to effectively reduce the negative effects of LPS in the human body [39]. Zhang et al. found that apolipoprotein A-I mimetic peptide 4 F can reduce mortality and improve the cardiac output of sepsis rats [40]. More and more research reported that cholesterol supplementation and lipoprotein therapies show great potential for treating sepsis patients. However, human studies are limited, so it is necessary to further implement the extensive experiment in vitro and in vivo studies, aims to verify its feasibility explore suitable doses, and identify any potential adverse reaction.
Study strengths and limitations
This study has many obvious advantages. The first is the large-scale, comprehensive sample group and nationally representative data obtained through the MIMIC-IV database, ensuring a consistent approach. Second, this study was extremely rigorous in the selection and adjustment of confounding variables, and the association of these variables with sepsis and other risk factors based on previous studies enhanced the accuracy of the analysis. Moreover, the NHHR value can be directly calculated from the conventional blood lipid test results; there is no additional testing cost. Additionally, our results indicate that NHHR has significant potential as a predictive indicator for sepsis patient mortality compared to other lipid indicators. Lastly, we employed various methods to strengthen the correlation between NHHR and sepsis, including subgroup analysis, Cox analysis, and K-M curve analysis, enhancing the reliability and validity of the findings.
However, there are limitations to this research. Firstly, the cross-sectional design of the study introduces the possibility of reverse causality, making it challenging to establish a causal correlation. Therefore, larger studies are needed to confirm causality. Even though we have tried to adjust the number of known confounding factors, because of the limitations of the research design, it still cannot be ruled out that all potential is not affected by the adjustment for confounding factors. Thirdly, the study only analyzed the correlation between sepsis and NHHR using the MIMIC-IV database, and additional databases may be necessary to further validate the results. Lastly, most of the MIMIC-IV database’s included population was of European descent, suggesting the need for validation in different ethnic groups.
Conclusion
This study reveals the sepsis mortality risk is significantly associated with elevated NHHR, highlighting the clinical significance of lipid metabolism in the treatment of sepsis. This new finding provides a powerful auxiliary tool for the early identification of patients with severe sepsis, enabling healthcare providers to closely monitor high-risk patients and enhance overall care efficacy.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
- NHHR:
-
Non-high-density lipoprotein cholesterol to high-density lipoprotein cholesterol ratio
- MIMIC-IV:
-
The Medical Information Mart for Intensive Care database IV
- HDL:
-
High-density lipoprotein
- Apo-A-I:
-
Apolipoprotein A-I
- Apo-A-II:
-
Apolipoprotein A-II
- ED:
-
Emergency department
- ROC:
-
Receiver-operator curve
- MIT:
-
Massachusetts Institute of Technology
- BIDMC:
-
The Beth Israel Deaconess Medical Center
- TC:
-
Total cholesterol
- HR:
-
Hazard ratio
- CI:
-
Confidence interval
- BMI:
-
Body mass index
- WBC:
-
White blood cell
- RBC:
-
Red blood cell
- Scr:
-
Serum creatinine
- BUN:
-
Blood urea nitrogen
- RRT:
-
Renal replacement therapy
- CCI:
-
Charlson Comorbidity Index
- SIRS:
-
Inflammatory response syndrome score
- OASIS:
-
Oxford acute severity of illness score
- GCS:
-
Glasgow coma scale
- SAPSII:
-
Simplified acute physiological score II
- SOFA:
-
Sequential organ failure assessment
- LPS:
-
Lipopolysaccharide
References
Cecconi M, et al. Sepsis and septic shock. Lancet. 2018;392(10141):75–87.
Liu D, et al. Sepsis-induced immunosuppression: mechanisms, diagnosis and current treatment options. Mil Med Res. 2022;9(1):56.
Prescott HC, Angus DC. Enhancing recovery from Sepsis: a review. JAMA. 2018;319(1):62–75.
Gauer R, Forbes D, Boyer N. Sepsis: diagnosis and management. Am Fam Physician. 2020;101(7):409–18.
Eubank TA, Long SW, Perez KK. Role of Rapid Diagnostics in diagnosis and management of patients with Sepsis. J Infect Dis. 2020;222(Suppl 2):S103–9.
Wilkins AL, et al. Toxic shock syndrome - the seven rs of management and treatment. J Infect. 2017;74(Suppl 1):S147–52.
Hofmaenner DA, et al. The many roles of cholesterol in Sepsis: a review. Am J Respir Crit Care Med. 2022;205(4):388–96.
Nogueira AC, et al. Changes in plasma free fatty acid levels in septic patients are correlated with cardiac damage and reduction in heart rate variability. Shock. 2008;29(3):342–8.
Taylor R, et al. Low circulatory levels of total cholesterol, HDL-C and LDL-C are correlated with death of patients with sepsis and critical illness: systematic review, meta-analysis, and perspective of observational studies. EBioMedicine. 2024;100:104981.
Reisinger AC, et al. Impact of Sepsis on High-Density Lipoprotein Metabolism. Front Cell Dev Biol. 2021;9:795460.
Cirstea M, et al. Decreased high-density lipoprotein cholesterol level is an early prognostic marker for organ dysfunction and death in patients with suspected sepsis. J Crit Care. 2017;38:289–94.
Sheng G, et al. Utility of Non-high-density Lipoprotein Cholesterol to high-density lipoprotein cholesterol ratio in evaluating Incident Diabetes Risk. Diabetes Metab Syndr Obes. 2022;15:1677–86.
Wang D, et al. Higher non-HDL-cholesterol to HDL-cholesterol ratio linked with increased nonalcoholic steatohepatitis. Lipids Health Dis. 2018;17(1):67.
Qing G, et al. The correlation between non-high-density lipoprotein cholesterol to high-density lipoprotein cholesterol ratio (NHHR) and suicidal ideation in adults: a population-based study in the United States. Lipids Health Dis. 2024;23(1):17.
Chang L, Chen X, Lian C. The correlation between the non-HDL-cholesterol to HDL-cholesterol ratio and 28-day mortality in sepsis patients: a cohort study. Sci Rep. 2022;12(1):3476.
Singer M, et al. The Third International Consensus definitions for Sepsis and septic shock (Sepsis-3). JAMA. 2016;315(8):801–10.
Huang M, Cai S, Su J. The pathogenesis of Sepsis and potential therapeutic targets. Int J Mol Sci, 2019. 20(21).
Esposito S, et al. Sepsis and septic shock: new definitions, new diagnostic and therapeutic approaches. J Glob Antimicrob Resist. 2017;10:204–12.
Tupchong K, Koyfman A, Foran M. Sepsis, severe sepsis, and septic shock: a review of the literature. Afr J Emerg Med. 2015;5(3):127–35.
Paoli CJ et al. Epidemiology and costs of Sepsis in the United States—An analysis based on timing of diagnosis and severity Level*. Crit Care Med, 2018. 46(12).
Prest J, et al. Sepsis-related Mortality Rates and Trends based on site of infection. Crit Care Explor. 2022;4(10):e0775.
Angus DC, van der Poll T. Severe sepsis and septic shock. N Engl J Med. 2013;369(9):840–51.
Evans T. Diagnosis and management of sepsis. Clin Med (Lond). 2018;18(2):146–9.
Dellinger RP, et al. Surviving Sepsis Campaign guidelines for management of severe sepsis and septic shock. Crit Care Med. 2004;32(3):858–73.
Cioccari L, Luethi N, Masoodi M. Lipid mediators in critically ill patients: a step towards Precision Medicine. Front Immunol. 2020;11:599853.
Sharma NK, et al. Proteomic study revealed cellular assembly and lipid metabolism dysregulation in sepsis secondary to community-acquired pneumonia. Sci Rep. 2017;7(1):15606.
Sharma NK, et al. Lipid metabolism impairment in patients with sepsis secondary to hospital acquired pneumonia, a proteomic analysis. Clin Proteomics. 2019;16(1):29.
Barker G et al. Lipid and Lipoprotein Dysregulation in Sepsis: clinical and mechanistic insights into chronic critical illness. J Clin Med, 2021. 10(8).
Morin EE, et al. HDL in sepsis - risk factor and therapeutic approach. Front Pharmacol. 2015;6:244.
Jones TK, Wong HR, Meyer NJ. HDL cholesterol: a Pathogen lipid Sink for Sepsis? Am J Respir Crit Care Med. 2019;199(7):812–4.
Guirgis FW, et al. Lipid and lipoprotein predictors of functional outcomes and long-term mortality after surgical sepsis. Ann Intensiv Care. 2021;11(1):82.
Zhao W, et al. Correlation of lipid profiles and the ratios with arterial stiffness in middle-aged and elderly Chinese. Lipids Health Dis. 2014;13:37.
Wen J, et al. Lipoprotein ratios are better than conventional lipid parameters in predicting arterial stiffness in young men. J Clin Hypertens (Greenwich). 2017;19(8):771–6.
Kwok RM, Torres DM, Harrison SA. Vitamin D and nonalcoholic fatty liver disease (NAFLD): is it more than just an correlation? Hepatology. 2013;58(3):1166–74.
Zhao X, et al. Correlation between the non-HDL-cholesterol-to-HDL-cholesterol ratio and the risk of gallbladder polyp formation among men: a retrospective cohort study. Lipids Health Dis. 2020;19(1):146.
Lin W, et al. Correlation between the non-HDL-cholesterol to HDL- cholesterol ratio and abdominal aortic aneurysm from a Chinese screening program. Lipids Health Dis. 2023;22(1):187.
Trinder M, et al. Inhibition of Cholesteryl Ester Transfer Protein Preserves High-Density Lipoprotein Cholesterol and improves survival in Sepsis. Circulation. 2021;143(9):921–34.
McDonald MC, et al. Reconstituted high-density lipoprotein attenuates organ injury and adhesion molecule expression in a rodent model of endotoxic shock. Shock. 2003;20(6):551–7.
Pajkrt D, et al. Antiinflammatory effects of reconstituted high-density lipoprotein during human endotoxemia. J Exp Med. 1996;184(5):1601–8.
Zhang Z, et al. Apolipoprotein A-I mimetic peptide treatment inhibits inflammatory responses and improves survival in septic rats. Am J Physiol Heart Circ Physiol. 2009;297(2):H866–73.
Acknowledgements
Not applicable.
Funding
The Fundamental Research Funds for the Central Universities of Central South University (2023ZZTS0897), the Degree & Postgraduate Education Reform Project of Central South University (2023JGB116), and the National Natural Science Foundation of China (Nos. 82170019) have provided financial support for this work.
Author information
Authors and Affiliations
Contributions
Y. performed the major design and drafted the manuscript. X. conceptualized, supervised, and revised the manuscript. All authors contributed to the article and approved the submitted version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Massachusetts Institute of Technology’s Institutional Review Boards (IRB) approved the use of the MIMIC-IV database for our study, which does not include any protected health information.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhang, Y., Zheng, X. Association of 28-day mortality with non-high-density lipoprotein cholesterol and the high-density lipoprotein cholesterol ratio (NHHR) in patients with sepsis: Results of MIMIC-IV database analysis. Lipids Health Dis 23, 255 (2024). https://doi.org/10.1186/s12944-024-02219-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12944-024-02219-5