Abstract
With the accelerated aging tendency, osteoarthritis (OA) has become an intractable global public health challenge. Stem cells and their derivative exosome (Exo) have shown great potential in OA treatment. Research in this area tends to develop functional microcarriers for stem cell and Exo delivery to improve the therapeutic effect. Herein, we develop a novel system of Exo-encapsulated stem cell-recruitment hydrogel microcarriers from liquid nitrogen-assisted microfluidic electrospray for OA treatment. Benefited from the advanced droplet generation capability of microfluidics and mild cryogelation procedure, the resultant particles show uniform size dispersion and excellent biocompatibility. Moreover, acryloylated stem cell recruitment peptides SKPPGTSS are directly crosslinked within the particles by ultraviolet irradiation, thus simplifying the peptide coupling process and preventing its premature release. The SKPPGTSS-modified particles can recruit endogenous stem cells to promote cartilage repair and the released Exo from the particles further enhances the cartilage repair performance through synergistic effects. These features suggest that the proposed hydrogel microcarrier delivery system is a promising candidate for OA treatment.
Similar content being viewed by others
Introduction
With the accelerated aging tendency of the population, osteoarthritis (OA) affects over 240 million people globally, posing a significant public health challenge and inflicting immense mental distress and economic burdens [1,2,3]. The main conventional therapies for OA, such as pharmacotherapy and surgery [4,5,6], primarily manage symptoms and are associated with complications, side effects, and a lack of regenerative capability, leading to limited long-term effectiveness [7, 8]. Stem cell therapy has emerged as a promising alternative for OA treatment in recent years [9,10,11]. They have demonstrated the capacity to modulate inflammation and promote cartilage repair in OA joints [12,13,14]. However, the application of exogenous stem cells is constrained by challenges such as maintaining cell viability during transplantation, immune rejection, substantial individual variation in response, complicated processes [15], and even ethical controversies [16]. Therefore, novel bioactive treatment methods that induce endogenous stem cell therapy is expected.
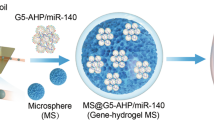
To address the above challenges, we propose an innovative approach involving stem cell-recruitable polypeptide hydrogel microcarriers with exosome (Exo) delivery for OA treatment (Fig. 1). Stem cell-derived Exo can treat OA by mimicking the therapeutic effects of stem cells [17,18,19], while avoiding the risks of immunological rejection [20], microvasculature occlusion [21] and tumor formation [22]. By encapsulating in hydrogel microcarriers, Exo can be released in a sustained way and exert a better therapeutic effect [23,24,25]. Although promising results have been demonstrated, long-term efficacy is still hard to achieve using Exo alone, due to rapid clearance of Exo from the joint cavity [26,27,28]. Stem cell recruitment peptide (Pep) SKPPGTSS can recruit endogenous stem cells [29, 30], which are expected to show long-term efficacy in promoting cartilage tissue repair [31, 32], and can overcome the challenges of exogenous stem cell therapy in both preparation and bioactivity. Hyaluronic acid methacryloyl (HAMA), as a natural polysaccharide material, has excellent bioactivity and lubricity [33, 34]. Gelatin methacryloyl (GelMA), as a natural protein biomaterial, provides favorable microenvironment [35, 36]. Combining the both can effectively improve the functional performances of the microcarriers. Therefore, we envisioned that by constructing HAMA/GelMA hydrogel microcarriers encapsulating Pep and Exo together, a systematic and temporally controlled therapeutic effect of OA can be accomplished.
In this study, we developed such HAMA/GelMA hydrogel microcarriers from microfluidic electrospray technology. A liquid nitrogen treatment procedure was adopted to render the particles with a porous structure, by which stem cell-derived Exo were facilely encapsulated in the particles without the use of organic solvents and thus keeping their biological activity. The microfluidic-derived particles had controllable size and good monodispersity, and were beneficial for subsequent Exo release. Moreover, acyloylated modified SKPPGTSS Pep was directly incorporated into the particles by ultraviolet (UV)-induced crosslinking during the generation process, thus simplifying the Pep coupling process and preventing its premature release. To facilitate description of different kinds of microcarriers in this work, the microfluidic electrospray-generated hydrogel particles were named as (Par), Par modified by SKPPGTSS Pep was named as Par@Pep, Par loaded with Exo was named as Par@Exo, and Par@Pep loaded with Exo was named as Par@Pep&Exo. When Par@Pep&Exo particles were applied for OA treatment, the hydrogel microcarriers release Exo, providing rapid therapeutic effects at the early stage. Simultaneously, the SKPPGTSS Pep recruits endogenous stem cells for sustained cartilage repair, ensuring continuous treatment and improved long-term efficacy. These features demonstrate that Exo and Pep-encapsulated hydrogel microcarriers offer coherent and synergistic OA treatment effects and may pave the way for advanced therapies in regenerative medicine for various other diseases.
Results and discussion
Generation of Exo-encapsulated stem cells recruitment particles
Hydrogel pre-gel solution consisting of 5 wt% HAMA, 10 wt% GelMA, and 0.1 wt% LAP was applied for the fabrication of particles via microfluidic electrospray. The reduction of unreacted C = C bonds at 1653 cm− 1 of the HAMA/GelMA sample after UV-crosslinking was confirmed by FTIR (Figure S1). The generated particles had good spherical morphology and excellent monodispersity due to the outstanding droplet manipulation capabilities of microfluidics (Fig. 2a-c). The good spherical morphology facilitates drug administration via intra-articular injection, and the excellent monodispersity ensures the stability of drug release. The scanning electron microscopy (SEM) results showed that the particles had rich three-dimensional pores (Fig. 2d-f), which is conducive to the release of bioactive substances. Additionally, the Exo was determined by a transmission electron microscope (TEM) (Fig. 2g). The TEM results showed the characteristic vesicle-like structure of Exo with a diameter of ~ 100 nm after uranyl acetate negative staining. Western blot confirmed the high expression of Exo markers such as CD9, CD63, TSG101, validating that Exo from human umbilical cord mesenchymal stem cells (hucMSCs) can be used for further research (Fig. 2h). The fluorescence images indicated that the Dio-labeled Exo with green fluorescence were successfully encapsulated into the particles uniformly (Fig. 2i). To further confirm the Exo release ability of the particles, the released Exo was confirmed by protein quantitative kit. The results indicated that the particles can continuously release Exo, and ~ 60% Exo was released into PBS within 8 days (Fig. 2i). Moreover, the degradation profile of the particles was investigated in vitro by placing the particles in a physiological-mimicking environment. The results indicated that ~ 50% degradation occurred in 6 days and complete degradation took about 12 days (Figure S2).
Characterization of particles and Exo. (a) Microscopic image of the particles. (b) The enlarged view of (a). (c) The size distribution of the particles. (d-f) SEM result of (d) the particle, (e) the enlarged view of particle and (f) the surface morphology. (g) TEM result of the Exo from hucMSCs. (h) Western blot of Exo markers CD63, CD63 and TSG101. (i) Release profile of Exo from day 0 to day 16. The inserted image is the particles encapsulated with Dio-labeled Exo. Scale bars are 200 μm in (a), 100 μm in (b), 50 μm in (d), 25 μm in (e), 10 μm in (f), 200 nm in (g), and 200 μm in (i), respectively
Biocompatibility test of the particles
Next, different kinds of particles were cultured with chondrocytes and bone marrow mesenchymal stem cells (BMSCs) of rats to examine their biocompatibility using Calcein-AM staining and CCK8 analysis. The Calcein-AM/PI staining results indicated that the chondrocytes and BMSCs in all groups maintained good morphology and high cell confluence on day 5. In addition, there were no obvious differences in dead cells among different groups (Figure S3a and S3b). CCK8 analysis indicated that all kinds of particles have good biocompatibility from day 1 to day 5. In particular, the Exo-encapsulated particles (Par@Exo and Par@Pep&Exo particles) exhibited better cell proliferation activity (Figure S3 c and S3d). In order to analyze the effect of direct contact of the particles on cells, BMSCs were cultured on the surface of the particles and then stained by Calcein-AM. The results indicated that the BMSCs can adhere and proliferate well on the particles with good cellular morphology from 1 to 7 days (Figure S4). In addition, the hemocompatibility test indicated that the particles had excellent hemocompatibility (Figure S5).
Stem cell recruitment and chondrogenic differentiation activities
BMSCs were co-cultured with different kinds of particles using the Transwell culture system to investigate the stem cell recruitment activities of the particles. After being cultured for 24 h, the Transwell results indicated larger number of BMSCs in Par@Pep and Par@Pep&Exo groups than other groups. Besides, the BMSCs number in Par@Exo group was larger than the control group, and the Par@Pep&Exo group had more cells than Par@Pep group. These results suggested that both SKPPGTSS Pep and Exo encapsulated in particles can stimulate BMSCs migration (Fig. 3a and d). These bio-activities were further confirmed by cell scratch experiments. The results showed that Par@Pep, Par@Exo and Par@Pep&Exo groups all had better cell migration activity than the control and Par groups, and the migration activity of the Par@Exo was better than that of the control group (Fig. 3b and e). To evaluate the activity of the particles on chondrogenic differentiation, BMSCs were co-cultured with different kinds of particles during the process of chondrogenic induction. After 3 weeks’ induction, Alcian blue was used to stain glycosaminoglycan (GAG, a marker of chondrocytes) for its expressions (Fig. 3c and f). The results indicated that the GAG expressions were significantly higher in Exo-encapsulated particles (Par@Pep&Exo and Par@Exo particles) than other groups, indicating that the Exo can effectively promote stem cells differentiation into chondrocytes.
Stem cell recruitment and chondrogenic activities in vitro. (a) The transwell results of BMSCs after 24 h of induction. (b) The migration results of BMSCs after 24 h of treatment. (c) Alcian blue staining results of BMSCs after 3 weeks of induction. (d-f) Quantitative analysis of (d) cell number, (e) cell migration area, and (f) GAG expression. Scale bars are 100 μm in (a) and 200 μm in (b) and (c), respectively. *:compared with the control group
Therapeutic effect test in vitro
During the pathological development of OA, reactive oxygen species (ROS) is a major factor to induce cartilage degradation [37,38,39]. Hence, we simulate oxidative stress microenvironment of OA by pretreating chondrocytes with H2O2 to examine the protective effect of the particles. The results validated that H2O2 can decrease the proliferative activity of chondrocytes. However, such decreased proliferative activity can be reversed by using particles. Notably, even particle itself also had the chondro-protection effect to a certain extent, although not as pronounced as that in the Pep-encapsulated and Exo-encapsulated groups. This might be because the particle microcarriers were composed of hyaluronic acid- and gelatin-based hydrogels, which have natural bioactive and chondroprotective effects [40, 41]. The Par@Pep&Exo group had the most pronounced protective effect on chondrocytes (Fig. 4a and c). In order to further verify the therapeutic effect of the particles on chondrocytes, immunofluorescence staining was used to detect cartilage marker protein expression, including collagen II (Col II) and aggrecan (Agg). The results showed that H2O2 treatment significantly decreased Col II and Agg expression compared with the control group. The Pep-encapsulated and Exo-encapsulated groups (Par@Pep, Par@Pep&Exo and Par@Exo) shown increased expression levels of Col II and Agg. SKPPGTSS Pep may indirectly promote the expression of Col II and Agg by promoting cell proliferation [42,43,44,45]. In addition, our result was consist with the previous reports that Exo can increase the expression of Agg and Col II in chondrocyte [46,47,48]. However, no obvious difference in the H2O2 and Par groups were observed. The above results indicated that both Exo and Pep can regulate the expression of Col II and Agg, with the Par@Pep&Exo group showing the best therapeutic effect in vitro (Fig. 4b, d, and e).
Therapeutic effect test in vitro. (a) Cell morphology of H2O2-induced chondrocyte cells after the particles treatment. (b) Immunofluorescence staining of Agg and Col II in H2O2-induced chondrocyte cells after the particles treatment. (c) CCK8 assay of H2O2-induced chondrocyte cells after the particles treatment. (d) Agg expression in H2O2-induced chondrocyte cells after the particles treatment. (e) Col II expression in H2O2-induced chondrocyte cells after the particles treatment. Scale bars are 200 μm in (a) and 50 μm in (b). *: compared with the control group; #: compared with the H2O2 group
H&E and safranin O-fast green staining after treatment in vivo
The rat OA model was constructed by surgical method beforehand as the previous reports [39, 49, 50]. After 8 weeks of treatment via articular injection of particles, hematoxylin and eosin (H&E) and Safranin O-fast green staining were performed for pathologic analysis. The results indicated that the typical OA features, such as surface irregularities and erosive cracks, were observed in control group and bare particles treated group (Fig. 5a, b). In contrast, the Pep-encapsulated and Exo-encapsulated particle treatments reduced erosion and destruction of cartilage and improved morphological integrity. Among them, the Par@Pep&Exo treated group had the best therapeutic effect. This result was further confirmed by the OA Research Society International (OARSI) score [51, 52]. The OARSI score indicated that Par@Pep&Exo, Par@Pep&Exo, and Par@Exo effectively inhibited the progression of OA (Fig. 5c), and Par@Pep&Exo had the lowest OARSI score, indicating the combined utilization of Pep and Exo achieved more effective therapeutic outcome than single use of either agent. In addition, the Safranin O-fast green staining also indicated that GAG (stained in red) was the highest in the Par@Pep&Exo group (Fig. 5d), suggesting that Par@Pep&Exo particles could inhibit OA via promoting GAG deposition. Based on this results, the Par@Pep&Exo group had the best performance with regard to OARSI and GAG deposition, indicating its effectiveness in inhibiting articular cartilage degeneration.
H&E and Safranin O-fast green staining results. (a) H&E results after different particles treatment. (b) Safranin O-fast green staining results after the particles treatment. (c) OARSI score after the particles treatment. (d) Relative GAG content after the particles treatment. All the scale bars are 100 μm. *: compared with the sham group; #: compared with the control group
Cartilage marker protein expression after treatment in vivo
Agg and Col II are the marker protein of healthy chondrocytes [49]. To further evaluate the therapeutic effect of particles on OA, the expression of Agg and Col II were examined by Immunohistochemistry. The results indicated that Agg and Col II were widely distributed in the articular cartilage in the Sham group. However, the localization and expression of Agg and Col II in the control group were seriously disturbed. After the Pep-encapsulated and Exo-encapsulated particles treatment, the expression of Agg (Fig. 6a, c) and Col II (Fig. 6b, d) were significantly increased compared with the PBS and bare particle groups. Although bare particle treatment had no obvious effect on cartilage marker proteins expression compared with the control group, there were no significant side effects such as inflammatory cell infiltration and tissue necrosis, as validated through H&E staining of the main organs (Figure S6), indicating that the particles have good biocompatibility in vivo. Overall, these results demonstrated that the Par@Pep&Exo particles could effectively inhibit cartilage degeneration by promoting the Agg and Col II expression.
Cartilage marker protein expression. (a) Agg expression after the particles treatment. (b) Col II protein expression after the particles treatment. (c) Agg expression analysis after the particles treatment. (d) Col II expression analysis after the particles treatment. All the scale bars are 100 μm. *: compared with the sham group; #: compared with the control group
Conclusion
In summary, we prepared an Exo-encapsulated particles with stem cell recruitment activities via microfluidic electrospray technology for OA treatment. The generated particles exhibited uniform spherical shape and good monodispersity. The rapid preparation process by liquid nitrogen treatment and UV irradiation avoided the reduction of drug activity and biocompatibility caused by the use of organic solvents in the traditional particle production process. The acryloylated SKPPGTSS Pep were co-crosslinked into the particles by UV irradiation during generation, simplifying the Pep coupling process and prolonging the Pep release time, which in turn improved the efficiency of stem cells recruitment. Furthermore, the addition of stem cell-derived Exo to the particles further enhanced the therapeutic performance through synergistic effects. Finally, in vitro and in vivo experiments showed that the present particles with excellent biocompatibility can effectively delay the progression of OA. These features suggested that the stem cell recruitment polypeptide hydrogel particle is a promising candidate for OA treatment and related biomedical applications.
Although our work provides an innovative approach for the treatment of OA, the mechanism underlying this microcarrier for OA treatment needs to be further explored with the assistance of bioinformatics data analysis, cellular experiments and animal experiments. In addition, a comprehensive biosafety and biotoxicity analysis of the microcarrier is necessary before its clinical application.
Materials and methods
Materials
LAP, AC-PEG-NHS-2 K, GelMA, and HAMA were acquired from EFL (Suzhou, China). Stem cells recruitment Pep SKPPGTSS were obtained from QyaoBio (Shanghai, China). The staining kits for H&E and Safranin O-fast green were purchased from Servicebio (Wuhan, China). Exo of hucMSCs were obtained from CytoNiche (Beijing, China). Alcian blue staining kits were obtained from Beyotime (Nanjing, China). All the antibodies purchased from Abcam (Cambridge, UK). H2O2 were obtained from Sigma-Aldrich (MO, USA). Calcein-AM/PI were purchased from YaJi (Shanghai, China). BCA protein Assay Kit was obtained from KeyGEN (Nanjing, China). Transwell was obtained from Corning (Shanghai, China). BMSCs and chondrocytes of rats were kept in our laboratory. Cartilage induction medium was obtained from Cyagen Biosciences (Guangzhou, China). Hyaluronidase and collagenase were purchased from Aladdin (Shanghai, China). α-MEM, FBS, DMEM and Trypsin-EDTA were obtained from Gibco (Grand Island, NY). Dio (3,3-dioctadecyloxacarbocyanine perchlorate) was purchased from Yeasen (Shanghai, China). The male SD rats at 8–10 weeks were obtained from Beijing Vital River (Beijing, China).
Preparation of particles
In a typical experiment, hydrogel pre-gel solution consisting of 10 wt% GelMA, 5 wt% HAMA, and 0.1 wt% LAP was applied for the fabrication of particles via microfluidic electrospray. Briefly, the pregel solution was injected into the glass capillary microfluidic chip. The tip diameter of the capillary chip was 200 μm, the liquid flow rate was 1 mL/h, and the electric field voltage was 6 kV. The generated droplets were collected in liquid nitrogen and then photo-crosslinked. Before the fabrication of the Exo-encapsulated stem cells recruitment particle, 1 mg/ml SKPPGTSS and 0.1 mg/mL AC-PEG-NHS-2 K were mixed to form the acrylylated SKPPGTSS, which can be photo-crosslinked under UV irradiation. Then, the acrylylated SKPPGTSS and 2 mg/mL Exo was added to the pregel solution for the fabrication of the particles.
Characterization of particles
The optical morphology and diameter of particles were captured and determined by an optical microscope (Jiangnan, JSZ6S, China). The particles loaded with Dio labeled Exo were observed and captured by an inverted fluorescence microscope (OLYMPUS, BX51, Japan). TEM (JSM-7500 F, Japan) was applied for the observation of Exo morphology. The surface morphology and microstructure of lyophilized particles were investigated by SEM (Hitachi, Japan). The content of C = C in methacrylates of HAMA/GelMA hydrogel before and after UV crosslinking was examined by FTIR (Thermo, USA).
Degradation of particles
To assess degradation of the particles in vitro, the dried particles were placed in PBS with 2 U/mL of collagenase and 1U/mL hyaluronidase at 37 °C. Then, the supernatant was replaced with fresh PBS with the same concentration of collagenase and hyaluronidase every 2 days. The remaining weight of particles after vacuum freeze-drying was weighed and compared to the initial weight.
Exo encapsuling and release ability of particle
During the fabrication process of the particles, 2 mg/mL Exo was added to the pregel solution for the fabrications of Exo-encapsulated particles. The loading efficiency of the Exo into hydrogel is about 90%. The Exo release ability of the particles was measured by BCA protein quantitative kit. Briefly, the Exo-encapsulated particles were immersed in PBS. At each point, the soaking solution was collected for measuring the released Exo and the fresh PBS was added. Besides, to visualize the Exo loading and release of the particles, Dio with green fluorescence was used to label Exo, which allows for easy observation of the Exo loading and release in particles under a fluorescence microscope.
Biocompatibility test of particle
The primary chondrocytes (identified by Alcian blue staining in Figure S7) and BMSCs from rats were applied for biocompatibility test of particle. For the observation of cell morphology and density, the chondrocytes and BMSCs (6 × 104/mL) were seeded on a 24-well plate and the particles were placed in Transwell. On day 3, the cells were stained with Calcein-AM/PI and then observed the cell morphology. For cell activity analysis, the cells were seeded on a 96-well plate and the soaked solution from 5% particles or 5% PBS (as control) were added in the cell culture medium. After treatment for 3 days, he cells activity was measured by CCK-8.
Hemolysis tests of particle
The red blood cells (RBCs) of rats were used for hemolysis tests of particle. Briefly, the whole blood of rats was collected in anticoagulation tube. Then, the RBCs were collected and washed by PBS. Subsequently, the collected RBC suspension was then diluted to 5% and then incubated with different kinds of Particles for 4 h. At last, hemolysis in each group including positive control (ddH2O) and negative control (PBS) were observed and analyzed.
Cells migration test of particle
To assess the effect of particles on stem cells migration, cell scratch experiments were performed using Transwell culture system. Simply, 6 × 104/mL BMSCs were inoculated in a 24-well plate. After 48 h of cultivation, BMSCs reached 70–80% confluence and a straight line was scratched using a 200 µL pipette tip. Then, the detached cells were rinsed with PBS for 2 times and 5% particles from different groups were added to the upper chamber. After continued incubation for 24 h, cells migration was observed after crystal violet staining.
Stem cell recruitment test of particle
Stem cell recruitment experiments were conducted using the Transwell culture system. Briefly, 5 × 104/mL BMSCs were inoculated into the upper chamber and different kinds of particles were added to the lower chamber. After 24 h of incubation, the the cells on the membrane of Transwell were fixed by paraformaldehyde. Subsequently, cells of the membrane were stained by crystal violet staining solution to observe and count the cells recruitment capacity.
Chondrogenic differentiation test of particle
Different kinds of particles were cocultured with the BMSCs during the chondrogenic differentiation process. 6 × 104/mL BMSCs were cultured in α-MEM and seeded into a 24-well plate for 24 h cultivation. When the BMSCs will reach 30–50% confluence, the α-MEM was replaced with cartilage induction medium and the particles were added to the upper chamber of the Transwell. After 3 weeks’ of chondrogenic differentiation, the differentiated cells were fixed and then stained with Alcian blue to observe chondrogenic differentiation.
Therapeutic effect of particles in vitro
We stimulated rat chondrocytes by H2O2 to mimic the microenvironment of oxidative stress of OA as the previous reports [38, 39]. The passage 3 − 4 chondrocytes (6 × 104/mL) were used for this test. When the chondrocytes reached 60–80% confluence, 500 µM H2O2 was used to pretreat cells for 6 h to induce oxidative stress. After that, the cells were washed by fresh cells culture medium and different kinds of particles were added. After treatment for 24 h, the cells were stained by Calcein-AM to observe cell morphology and cell density. At the same time, the treated chondrocytes were performed for immunofluorescence staining of Agg and Col II.
Construction of rat OA model
The male SD rat OA model (10 weeks old, n = 5 for each group) was constructed by surgical operation as previous reports [39, 49, 50]. Briefly, after anesthetizing the rats with sodium pentobarbital, the joint cavity was opened, the anterior cruciate ligament was transected, a portion of the medial meniscus was incised, and then the muscle and skin layers were sutured sequentially. One week after the model was established, the rats were intraarticularly injected with 100 µl PBS (as control) or with different kinds of particles every 2 weeks. After 8 weeks’ treatment, the knee joints and organ were collected for next experiment.
Histochemical analysis of therapeutic effect
The collected arthrosis and organs were sequentially fixed, decalcified (only for arthrosis), embedded, and tissue sectioned. Then, the 5 μm thick paraffin sections of organs were stained with H&E for pathological analysis. The collected knee joint samples were fixed for 1 week and then decalcified for 2 months. Subsequently, the samples were stained for H&E and safranin O-fast green. The OARSI based on safranin O-fast green result was evaluated by two assessors as the previous reports [51, 52]. Twenty tissue sections per group (4 tissue sections per rat, 5 rats per group) were scored. In addition, the paraffin sections were stained with the primary antibodies of Col II (1:100 dilutions) and Agg (1:200 dilutions) for histochemical analysis of Agg and Col II expression. The relative expression levels of Agg and Col II were analyzed by image processing.
Statistical analysis
All the data in this work were presented as mean ± standard deviation (n ≥ 3). All experiments were repeated at least three times in this work. Statistical differences of the of results were performed and analyzed using ANOVA or Student’s t-test. P < 0.05 was considered as statistically significant.
Data availability
No datasets were generated or analysed during the current study.
References
Coryell PR, Diekman BO, Loeser RF. Mechanisms and therapeutic implications of Cellular Senescence in Osteoarthritis. Nat Rev Rheumatol. 2021;17(1):47–57.
Xie R, Yao H, Mao AS, Zhu Y, Qi D, Jia Y, Gao M, Chen Y, Wang L, Wang D-A. Biomimetic cartilage-lubricating polymers regenerate cartilage in rats with early osteoarthritis. Nat Rev Eng. 2021;5(10):1189–201.
Chen H, Ye T, Hu F, Chen K, Li B, Qiu M, Chen Z, Sun Y, Ye W, Wang H. Urchin-like Ceria nanoparticles for enhanced gene therapy of Osteoarthritis. Sci Adv. 2023;9(24):eadf0988.
Sharma L. Osteoarthritis of the knee. New Engl J Med. 2021;384(1):51–9.
Li G, Liu S, Chen Y, Zhao J, Xu H, Weng J, Yu F, Xiong A, Udduttula A, Wang D. An Injectable Liposome-Anchored Teriparatide Incorporated gallic acid-grafted gelatin hydrogel for Osteoarthritis Treatment. Nat Commu. 2023;14(1):3159.
Lei Y, Zhang Q, Kuang G, Wang X, Fan Q, Ye F. Functional biomaterials for Osteoarthritis Treatment: from research to application. Smart Med. 2022;1(1):e20220014.
Latourte A, Kloppenburg M, Richette P. Emerging Pharmaceutical therapies for osteoarthritis. Nat Rev Rheumatol. 2020;16(12):673–88.
Lei C, Song J-H, Li S, Zhu Y-N, Liu M-Y, Wan M-C, Mu Z, Tay FR, Niu L-N. Adv Materials-Based Therapeutic Strategies against Osteoporos Biomaterials. 2023;296:122066.
Wiggers TG, Winters M, Van den Boom NA, Haisma HJ, Moen MH. Autologous stem cell therapy in knee osteoarthritis: a systematic review of Randomised controlled trials. Brit J Sport Med. 2021;55(20):1161–9.
Zhao X, Liu S, Yildirimer L, Zhao H, Ding R, Wang H, Cui W, Weitz D. Injectable Stem Cell-Laden Photocrosslinkable microspheres fabricated using Microfluidics for Rapid Generation of osteogenic tissue constructs. Adv Funct Mater. 2016;26(17):2809–19.
Mianehsaz E, Mirzaei HR, Mahjoubin-Tehran M, Rezaee A, Sahebnasagh R, Pourhanifeh MH, Mirzaei H, Hamblin MR. Mesenchymal stem cell-derived exosomes: a New Therapeutic Approach to Osteoarthritis? Stem. Cell Res the. 2019;10:1–13.
Bhattacharjee M, Escobar Ivirico JL, Kan H-M, Shah S, Otsuka T, Bordett R, Barajaa M, Nagiah N, Pandey R, Nair LS. Injectable Amnion hydrogel-mediated delivery of adipose-derived stem cells for Osteoarthritis Treatment, P. Natl Acad Sci. 2022;119(4):e2120968119.
Maumus M, Manferdini C, Toupet K, Peyrafitte J-A, Ferreira R, Facchini A, Gabusi E, Bourin P, Jorgensen C, Lisignoli G. Adipose mesenchymal stem cells protect chondrocytes from Degeneration Associated with Osteoarthritis, Stem. Cell Res. 2013;11(2):834–44.
Wang B, Liu W, Li JJ, Chai S, Xing D, Yu H, Zhang Y, Yan W, Xu Z, Zhao B. A low dose cell therapy system for treating osteoarthritis: in vivo study and in Vitro mechanistic investigations. Bioact Mater. 2022;7:478–90.
Yang L, Liu Y, Sun L, Zhao C, Chen G, Zhao Y. Biomass microcapsules with Stem Cell Encapsulation for Bone Repair. Nano-Micro Lett. 2022;14:1–12.
Master Z, Crowley AP, Smith C, Wigle D, Terzic A, Sharp RR. Stem cell preservation for regenerative therapies: ethical and governance considerations for the Health Care Sector. NPJ Regen Med. 2020;5(1):23.
Jin Y, Xu M, Zhu H, Dong C, Ji J, Liu Y, Deng A, Gu Z. Therapeutic effects of Bone Marrow mesenchymal stem cells-derived exosomes on Osteoarthritis. Int J Mol Cell Med. 2021;25(19):9281–94.
Yu H, Huang Y, Yang L. Research Progress in the use of mesenchymal stem cells and their derived exosomes in the treatment of Osteoarthritis. Ageing Res Rev. 2022;80:101684.
Liu Z, Zhuang Y, Fang L, Yuan C, Wang X, Lin K. Breakthrough of Extracellular vesicles in Pathogenesis, diagnosis and treatment of Osteoarthritis. Bioact Mater. 2023;22:423–52.
Zhai M, Zhu Y, Yang M, Mao C. Human mesenchymal stem cell derived exosomes enhance cell-free bone regeneration by altering their miRNAs profiles. Adv Sci. 2020;7(19):2001334.
Nikfarjam S, Rezaie J, Zolbanin NM, Jafari R. Mesenchymal stem cell Derived-Exosomes: a Modern Approach in Translational Medicine. J Transl Intern Med. 2020;18(1):1–21.
Lou G, Chen Z, Zheng M, Liu Y. Mesenchymal stem cell-derived exosomes as a New Therapeutic Strategy for Liver diseases. Exp Mol Med. 2017;49(6):e346–346.
Han M, Yang H, Lu X, Li Y, Liu Z, Li F, Shang Z, Wang X, Li X, Li J. Three-dimensional-cultured msc-derived exosome-hydrogel hybrid microneedle array Patch for spinal cord repair. Nano Lett. 2022;22(15):6391–401.
Tang Q, Lu B, He J, Chen X, Fu Q, Han H, Luo C, Yin H, Qin Z, Lyu D. Exosomes-Loaded Thermosensitive Hydrogels for Corneal Epithelium and Stroma Regeneration, Biomaterials 280 (2022) 121320.
Fan L, Liu C, Chen X, Zheng L, Zou Y, Wen H, Guan P, Lu F, Luo Y, Tan G. Exosomes-Loaded Electroconductive Hydrogel synergistically promotes tissue repair after spinal cord Injury via Immunoregulation aand enhancement of Myelinated Axon Growth. Adv Sci. 2022;9(13):2105586.
Zhao Y, Wei C, Chen X, Liu J, Yu Q, Liu Y, Liu J. Drug Delivery System based on Near-Infrared Light-Responsive Molybdenum Disulfide nanosheets controls the high-efficiency release of dexamethasone to inhibit inflammation and treat Osteoarthritis, ACS. Appl Mater Inter. 2019;11(12):11587–601.
Wan J, He Z, Peng R, Wu X, Zhu Z, Cui J, Hao X, Chen A, Zhang J, Cheng P. Injectable Photocrosslinking Spherical Hydrogel-Encapsulated Targeting peptide-modified Engineered exosomes for Osteoarthritis Therapy. J Nanobiotechnol. 2023;21(1):1–21.
Deng S, Cao H, Cui X, Fan Y, Wang Q, Zhang X. Optimization of Exosome-based cell-free strategies to enhance endogenous cell functions in tissue regeneration. Acta Biomater. 2023;171:68–84.
Zhu J, Yang S, Qi Y, Gong Z, Zhang H, Liang K, Shen P, Huang Y-Y, Zhang Z, Ye W. Stem cell-homing hydrogel-based mir-29b-5p delivery promotes cartilage regeneration by suppressing senescence in an Osteoarthritis Rat Model, Sci. Adv. 2022;8(13):eabk0011.
Sun X, Yin H, Wang Y, Lu J, Shen X, Lu C, Tang H, Meng H, Yang S, Yu W. In situ articular cartilage regeneration through endogenous reparative cell homing using a functional bone marrow-specific scaffolding system, ACS. Appl Mater Inter. 2018;10(45):38715–28.
Yang Z, Li H, Yuan Z, Fu L, Jiang S, Gao C, Wang F, Zha K, Tian G, Sun Z. Endogenous cell recruitment strategy for articular cartilage regeneration. Acta Biomater. 2020;114:31–52.
Li Y, Li L, Wang M, Yang B, Huang B, Bai S, Zhang X, Hou N, Wang H, Yang Z. O-alg-THAM/Gel Hydrogels Functionalized with Engineered microspheres based on mesenchymal stem cell secretion Recruit endogenous stem cells for cartilage repair. Bioact Mater. 2023;28:255–72.
Yang L, Liu Y, Shou X, Ni D, Kong T, Zhao Y. Bio-inspired Lubricant Drug Delivery particles for the treatment of Osteoarthritis. Nanoscale. 2020;12(32):17093–102.
Xiang H, Zhang C, Xiong Y, Wang Y, Pu C, He J, Chen L, Jiang K, Zhao W, Yang H. MMP13-Responsive hydrogel microspheres for Osteoarthritis Treatment by Precise Delivery of Celecoxib. Mater Des. 2024;241:112966.
Wan J, He Z, Peng R, Wu X, Zhu Z, Cui J, Hao X, Chen A, Zhang J, Cheng P. Injectable Photocrosslinking Spherical Hydrogel-Encapsulated Targeting peptide-modified Engineered exosomes for Osteoarthritis Therapy. J Nanobiotechnol. 2023;21(1):284.
Pang L, Jin H, Lu Z, Xie F, Shen H, Li X, Zhang X, Jiang X, Wu L, Zhang M. Treatment with mesenchymal stem cell-derived nanovesicle-containing gelatin methacryloyl hydrogels alleviates Osteoarthritis by modulating Chondrogenesis and Macrophage polarization. Adv Healthc Mater. 2023;12(17):2300315.
Wang W, Duan J, Ma W, Xia B, Liu F, Kong Y, Li B, Zhao H, Wang L, Li K. Trimanganese Tetroxide Nanozyme protects cartilage against degeneration by reducing oxidative stress in Osteoarthritis. Adv Sci. 2023;10(17):2205859.
Qiu W, Zhao W, Zhang L, Wang H, Li N, Chen K, Zhang H, Wang Y. A solid-liquid Composite Lubricating Nano-Snowboard for Long‐Acting Treatment of Osteoarthritis. Adv Funct Mater. 2022;32(46):2208189.
Yang L, Sun L, Zhang H, Bian F, Zhao Y. Ice-inspired Lubricated Drug Delivery particles from Microfluidic Electrospray for Osteoarthritis Treatment. ACS Nano. 2021;15(12):20600–6.
Kang L-J, Yoon J, Rho JG, Han HS, Lee S, Oh YS, Kim H, Kim E, Kim SJ, Lim YT. Self-assembled Hyaluronic Acid nanoparticles for Osteoarthritis Treatment. Biomaterials. 2021;275:120967.
Maihemuti A, Zhang H, Lin X, Wang Y, Xu Z, Zhang D, Jiang Q. 3D-Printed fish gelatin scaffolds for cartilage tissue Engineering. Bioact Mater. 2023;26:77–87.
Koutsopoulos S. Self-assembling peptide nanofiber hydrogels in tissue Engineering and Regenerative Medicine: Progress, Design guidelines, and applications. J Biomed Mater Res A. 2016;104(4):1002–16.
Gelain F, Bottai D, Vescovi A, Zhang S. Designer self-assembling peptide nanofiber scaffolds for adult mouse neural stem cell 3-Dimensional cultures. PLoS ONE. 2006;1(1):e119.
Zhang ZX, Zheng QX, Wu YC, Hao DJ. Compatibility of neural stem cells with functionalized self-assembling peptide Scaffold in vitro. Biotechnol Bioproc Eng. 2010;15:545–51.
Liu X, Wang X, Wang X, Ren H, He J, Qiao L, Cui F-Z. Functionalized self-assembling peptide Nanofiber Hydrogels Mimic Stem Cell Niche to control human adipose stem cell behavior in vitro. Acta Biomater. 2013;9(6):6798–805.
Cao H, Chen M, Cui X, Liu Y, Liu Y, Deng S, Yuan T, Fan Y, Wang Q, Zhang X. Cell-free Osteoarthritis Treatment with sustained-release of chondrocyte-targeting exosomes from umbilical cord-derived mesenchymal stem cells to rejuvenate aging chondrocytes. ACS Nano. 2023;17(14):13358–76.
He L, He T, Xing J, Zhou Q, Fan L, Liu C, Chen Y, Wu D, Tian Z, Liu B. Bone marrow mesenchymal stem cell-derived exosomes protect cartilage damage and relieve knee Osteoarthritis Pain in a rat model of Osteoarthritis. Stem Cell Res. 2020;11:1–15.
Long L, Zou G, Cheng Y, Li F, Wu H, Shen Y. MATN3 delivered by Exosome from Synovial mesenchymal stem cells relieves knee osteoarthritis: evidence from in vitro and in vivo studies. J Orthop Transl. 2023;41:20–32.
Lei Y, Wang Y, Shen J, Cai Z, Zhao C, Chen H, Luo X, Hu N, Cui W, Huang W. Injectable Hydrogel microspheres with Self-renewable hydration layers alleviate osteoarthritis. Sci Adv. 2022;8(5):eabl6449.
Zuo G, Zhuang P, Yang X, Jia Q, Cai Z, Qi J, Deng L, Zhou Z, Cui W. Xiao, regulating Chondro-Bone metabolism for treatment of Osteoarthritis via High‐Permeability Micro/Nano Hydrogel Microspheres. Adv Sci. 2024;11(5):2305023.
Gerwin N, Bendele A, Glasson S, Carlson C. The OARSI Histopathology Initiative-recommendations for histological assessments of Osteoarthritis in the rat. Osteoarthr Cartil. 2010;18:S24–34.
Yang J, Zhu Y, Wang F, Deng L, Xu X, Cui W. Microfluidic liposomes-anchored microgels as Extended Delivery platform for treatment of Osteoarthritis. Chem Eng J. 2020;400:126004.
Acknowledgements
Not applicable.
Funding
This work was supported by the National Natural Science Foundation of China (No. 82202670 and 82272502), the Zhejiang Provincial Natural Science Foundation of China (No. LQ23H060001), and the Startup Fund of Wenzhou Institute, University of Chinese Academy of Sciences (No. WIUCASQD2022001).
Author information
Authors and Affiliations
Contributions
Y.J. Zhao and L.R. Shang conceived the conceptualization and designed the experiment. L. Yang carried out the experiments. L.R. Shang, W.Z. Li, Y.X. Wang and L. Yang participated in data analysis and discussion. L. Yang, W.Z. Li, and L.R. Shang wrote the paper.
Corresponding authors
Ethics declarations
Ethical approval
All animal experiments were approved by the Animal Care and Use Committee of Wenzhou Institute (WIUCAS22030421).
Consent for publication
All authors agree to be published.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Yang, L., Li, W., Zhao, Y. et al. Stem cell recruitment polypeptide hydrogel microcarriers with exosome delivery for osteoarthritis treatment. J Nanobiotechnol 22, 512 (2024). https://doi.org/10.1186/s12951-024-02765-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12951-024-02765-1