Abstract
Objective
Our aim was to explore the relationship between serum uric acid (UA) levels in early pregnancy and the development of gestational diabetes mellitus (GDM), and to further explore whether there is a causal relationship.
Methods
684 pregnant women with GDM and 1162 pregnant women without GDM participated in this study. 311 pregnant women with GDM and 311 matched controls were enrolled in a 1:1 case-control study. We used conditional logistic regression to explore the relationship between UA levels and the risk of developing GDM. The causal relationship between the two was examined by two-sample Mendelian randomization (MR) analysis.
Results
In the 1:1 matched population, the odds ratio (OR) of developing GDM compared with the extreme tertiles of UA levels was 1.967 (95% confidence interval [CI]: 1.475–2.625; P < 0.001). Restricted cubic spline analyses showed a linear relationship between UA and GDM when UA exceeded 222 µmol/L. GDM and UA levels maintained a statistically significant positive correlation in different stratified regression analyses (P < 0.001). However, no evidence of a causal relationship between uric acid and GDM was found by MR analyses with an OR of 1.06 (95% CI: 0.91–1.25) per unit increase in UA.
Conclusion
There is a positive correlation between UA levels in early pregnancy and the subsequent risk of developing GDM. However, no genetic evidence was found to support a cause-effect relationship between UA and GDM.
Highlights
λ The positive correlation between serum uric acid level and gestational diabetes mellitus persisted after a 1:1 case-control matching program.
λ High uric acid level remained an independent risk factor for developing gestational diabetes mellitus in the stratified analyses.
λ The positive correlation between serum uric acid level and the development of gestational diabetes mellitus increased when serum uric acid exceeded 222 µmol/L.
λ Our two-sample mendelian randomization analysis did not produce genetic evidence of a causal relationship between uric acid and gestational diabetes mellitus.
Similar content being viewed by others
Introduction
GDM is a disease characterized by elevated blood glucose during pregnancy that increases adverse pregnancy outcomes and poses a significant risk to mother and child [1]. GDM is a key risk factor for postpartum type 2 diabetes in pregnant women [2]. Although early diagnosis and treatment of GDM can reduce the risk of adverse pregnancy outcomes, many of the current diagnostic and management approaches remain controversial. There is a lot of evidence suggesting that the mechanisms and clinical biomarkers of GDM deserve further investigation for the early prevention of GDM [3]. Given that blood glucose levels during pregnancy are affected by a variety of factors, including diet, mood, stress, and medications and that the diagnosis of GDM using a single oral glucose tolerance test (OGTT) is subject to a certain degree of underdiagnosis and misdiagnosis, there is an urgent need to explore novel biomarkers, mechanisms, and targeted measures for GDM.
UA was once overlooked except for gout and kidney stones, but the results of large quantities of recent researches suggest that it is one of the most important metabolized substances [4]. Some studies have demonstrated that hyperuricemia is positively related to metabolic syndrome and diabetes mellitus [5]. Although studies have reported that excessive serum uric acid levels are positively associated with insulin resistance and risk of type 2 diabetes, the relationship between serum uric acid and risk of GDM has been inconsistent and relatively limited [6].
Mendelian randomization (MR) analyses assess the causal effect of genes to predict the relationship between exposure and outcome through gene-based instrumental variables [7]. Mendelian and other genetic studies have been conducted to eliminate potential confounders and reverse causality [8]. Several MR analyses have explored the causal relation between serum UA levels and type 2 diabetes, but all have reported negative results [9, 10]. We are aware that no MR studies have been conducted on the relationship between serum UA levels and the risk of GDM. Therefore, it is essential to explore whether there is a causal relationship between the two.
We hypothesized that elevated UA in early pregnancy is a risk factor for t developing GDM. We analyzed data from a case-control study to examine the association between early gestational UA levels and subsequent GDM risk in pregnant Chinese women. We analyzed data from the International Consortium to further explore the possible causal relationship between uric acid and GDM by two-sample MR analysis.
Methods
Study design and participants
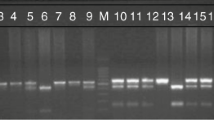
Our case-control study included 1908 singleton pregnant women. Pregnant women were recruited from the obstetrics departments of the Shanghai Fifth People’s Hospital affiliated with Fudan University between February 2018 and June 2022. The procedure of this retrospective study was described in Fig. 1.
Pregnant women who have a record of pregnancy in this institution are included. The exclusion criteria were twin or multiple pregnancies, diagnosis of diabetes mellitus or other metabolic or infectious diseases, UA testing beyond the 24th week of gestation, or incomplete maternal and fetal records. Ultimately, 1846 women (1162 without and 684 with GDM) were included in the analysis.
GDM is diagnosed if at least one of the following thresholds is reached in the 2-hour 75-g OGTT: fasting plasma glucose ≥ 5.1 mmol/L, 1-hour plasma glucose ≥ 10.0 mmol/L, or 2-hour plasma glucose ≥ 8.5 mmol/L [11]. All 1846 participants had no significant pre-pregnancy diabetes and 684 women were diagnosed with GDM.
Pregnancy data collection and laboratory evaluation
After fasting overnight for 12 h, blood samples were collected for biochemical parameter testing (Cobas 8000 Automatic Biochemical Analyzer; Roche, Basel, Switzerland). We measured blood pressure and anthropometric parameters.
Sources of data for MR analysis
Genetic variants related to uric acid were screened based on a genome-wide association study of 162,255 Japanese, of which the number of participants related to UA was 109,029 [12]. The study retrieved single-nucleotide polymorphisms (SNPs) associated with UA with genome-wide significance (P < 5 × 10− 8) and linkage disequilibrium between SNPs were estimated using the clumping method (r2 < 0.001, window size = 10,000 kb) using European samples from the 1000 Genomes Project. Forty-three SNPs associated with UA were identified, and we researched these SNPs in the PhenoScanner database to examine whether these genetic variants were associated with potential confounders of GDM. Finally, 35 SNPs were enrolled in the main MR analysis.
Data from the FinnGen consortium were used to analyze the relationship between the selected SNPs and GDM. The analysis included 6033 GDM cases in approximately 123,000 women [13]. Detailed data are shown in the Supplementary Tables.
Statistical analyses
Continuous variables are expressed as mean ± standard deviation or median (interquartile range), and for categorical variables frequencies or percentiles are used. To avoid potential bias, we used a case-control matching method to match the variables of age, family history of diabetes mellitus, parity, and BMI, with matching tolerances of 0, 0, 0, 0, 0, and 0.25. To further validate the relationship between UA and GDM, we created a retrospective cohort that included the same subjects, in which participants were divided into three groups according to the tertiles of UA: the lowest group (< 199 µmol/L), middle group (199–243 µmol/L), and highest group (> 243 µmol/L). We used conditional logistic regression analysis to estimate the independent association between UA levels and GDM risk in the case-control study. In the retrospective cohort, we adjusted for UA in Model 1 and made additional adjustments for lifestyle and metabolic risk factors, including maternal age, pre-pregnancy BMI, history of diabetes, and history of GDM in Model 2. In Model 3, we further adjusted for alanine aminotransferase (ALT), creatinine (Cr), low-density lipoprotein (LDL), triglyceride (TG), fasting blood glucose (FBG) levels and diastolic blood pressure (DBP). In the cohort study, a restricted cubic spline was used to estimate the relationship between UA and GDM, and subject operating characteristic curves were plotted.
Two-sample MR analysis was performed using the “TwoSampleMR” R package [14]. In the main analysis, we used MR inverse variance weighting (IVW), which is a regression weighted by the inverse of the SNP-outcome association variances [15]. The MR-Egger intercept test [16] and MR-PRESSO test [17] were used to identify and account for potential horizontal pleiotropy. The Cochran’s Q test [18] was used to detect heterogeneity.
All statistical analyses were performed using SPSS software (version 25.0; IBM SPSS Inc., Chicago, IL, USA) and R software version 4.0.2. All P-values were two-tailed, and statistical significance was set at P < 0.05.
Results
Association between serum UA levels and GDM in observational study
Table 1 shows the demographic and metabolic characteristics of the participants categorized as women without GDM (control group, n = 1162) and those with GDM (GDM group, n = 684). The control group consisted of women with physiologic pregnancies who were routinely screened for GDM at mid-pregnancy with negative results. The average age of the women with GDM was significantly higher than that of the control group, whereas no differences were found in systolic blood pressure (SBP), diastolic blood pressure (DBP), fasting blood glucose (FBG), aspartate transaminase (AST), and cholesterol. Pre-pregnancy BMI and alanine aminotransferase (ALT), creatinine (Cr), UA, triglycerides (TG), and low-density lipoprotein cholesterol (LDL-C) levels were higher in women who developed GDM than in women in the control group.
A 1:1 case-control matching procedure was used to avoid possible bias. After 1:1 a case-control matching procedure, matching for parameters such as age, family history of diabetes mellitus, parity, and BMI, the results of the conditional logistic regression analysis (enter method) showed a positive association between UA and GDM (OR: 1.967; 95% CI: 1.475–2.625, in the highest tertile vs. the lowest tertile; P < 0.001), as shown in Table 2.
The participants’ characteristics across the tertiles of UA levels were shown in Table 3. There were no differences in SBP, FBG levels or history of GDM across the tertiles of UA levels. Participants with higher levels of UA were likely to have higher DBP and ALT, AST, TG, cholesterol, and LDL-C levels but lower high-density lipoprotein cholesterol (HDL-C) levels. In the fully adjusted model, the OR for the occurrence of GDM comparing with the extreme tertiles of UA levels was 2.788 (95% CI: 2.060–3.772; P < 0.001), and the P-values were stable during the process of adjusting for different models, as shown in Table 4. After regression analysis of the different subgroups, UA still showed a significant correlation with GDM, as shown in Table 5.
Restricted cubic splines showed a positively correlated linear relationship between uric acid levels and GDM risk, especially when uric acid was above 222 µmol/L (P for nonlinearity < 0.001, P overall < 0.001, Fig. 2). The area under the receiver operating characteristic curve (ROC) of UA combined with basal factors (age, GDM history, pre-pregnancy BMI, TG, ALT, Cr, LDL, FBG, and DBP) for predicting GDM was 0.803 (95% CI: 0.781–0.826, P < 0.001, Fig. 3).
Association between genetic variants of UA and GDM
We further performed MR analysis to estimate the causal effect size of genetically determined UA levels on GDM. The characteristics of the selected SNPs and their associations with GDM risk and UA levels are shown in Supplementary Table 1. We detected an outlier SNP (rs1260326) using the MR-PRESSO test and performed MR analysis after deleting this SNP. No evidence of a causal relationship between serum UA and GDM risk was found (OR: 1.06, 95% CI: 0.91–1.25) per standard deviation increase in UA (IVW-MR in Table 6). Similar results were observed for the weighted median method, simple mode, weighted mode, and MR-Egger regression (Table 6). The MR-Egger intercept test suggested no unbalanced horizontal pleiotropy (MR-Egger intercept = -0.007; P = 0.385). Cochran’s Q statistics using separately selected SNPs showed significant heterogeneity (P < 0.05) in UA (Table 7). More Details of the MR analysis were summarized in Supporting Information (Supfig 1-4).
Discussion
Our study found a positive association between elevated serum UA levels and increased risk of GDM. However, MR analysis fails to demonstrate a causal relationship between serum UA levels and GDM risk.
Many observational studies support a positive correlation between serum UA levels and diabetes risk as well as GDM. Rasika et al. [19]. Susan reported that the risk of GDM in pregnant women increases as serum UA levels rise in the first trimester. In a prospective study, Duo et al. [20]. demonstrated that elevated serum UA levels were positively associated with the development of GDM, and the association was enhanced when serum UA exceeded 240 µmol/L. A systematic review and meta-analysis showed that elevated UA levels are positively related to the risk of GDM, especially in early pregnancy [6]. Our results are consistent with these findings. We conducted a 1:1 case-control matching program and found that the significant correlation between UA and GDM persisted after matching.
Previous studies have identified several potential risk factors for GDM (age, BMI, family history of diabetes, and history of GDM) [21, 22]. To correct these potential consolidating factors, we conducted a stratified regression analysis. Even after adjusting for metabolic risk factors in the model, high UA levels remained an independent risk factor for developing GDM. We used spline regression analysis to explore the relationship between UA levels and the occurrence of GDM. When we examined the association between UA levels and GDM, a J-shaped association was observed. When serum UA exceeded 222 µmol/L, the positive correlation between serum UA levels and the development of GDM increased. Various mechanisms may account for the positive association between UA levels and GDM risk. Firstly, hyperuricemia may potentially cause β-cell dysfunction by inducing oxidative stress, inducible nitric oxide (NO) synthase and inflammation within β-cells [23,24,25,26]. Secondly, insulin resistance plays a critical role in the pathogenesis of GDM, and the results of many researches have shown that hyperuricemia is closely associated with insulin resistance [27,28,29,30,31]. Furthermore, hyperuricemia may induce oxidative stress, which in turn leads to endocrine dysfunction in adipose tissue, leading to the development of metabolic syndrome [32].
Although many studies have indicated that UA is a crucial factor in the development of GDM, evidence reveals that UA may play only a bystander role in the risk of GDM. Maged et al. [33]. reported that the serum UA concentration was not positively related to the development of GDM. Güngör et al. [34]. also proved that UA levels were higher in patients with diabetes; however, this elevation was not statistically significant. Therefore, it remains unknown whether there is a causal relationship between serum UA levels and GDM risk.
Yan et al. [35]. provided evidence of a causal association between UA and macrovascular disease in Chinese diabetic women using MR analysis. Although several MR studies have evaluated the potential causal relationship between serum UA levels and diabetes risk, no positive results have been reported. Three European studies and a Chinese study found no causal association between UA and diabetes risk [9, 10, 36, 37]. We are unaware of any studies that have performed MR analyses of UA and GDM to explore their genetic causality. Therefore, additional MR studies are necessary to explore the causal associations between serum UA levels and GDM risk. Although serum UA levels were significantly correlated with an increased incidence of GDM, our two-sample MR analysis did not produce genetic evidence of a causal relationship between them. There are several possible reasons for these negative results. Firstly, this study used summary-level data, which could lead to potential mediators between genotype and disease risk that may not have been controlled for. Secondly, datasets of exposures and outcomes were obtained from individuals of Japanese and European descent who had varying risks of developing GDM. In addition, the limited number of SNPs included in the MR analysis and the relatively small effect of SNPs on UA levels may lead to negative conclusions. Finally, in observational studies, blood UA may be a secondary factor to adverse metabolic phenotypes, and residual confounders may induce a positive association of UA and GDM in previous studies. Notably, factors such as alcohol consumption, smoking, physical activity, renal function, or diuretic use have all been reported to be associated with GDM and serum uric acid levels, but only a few studies have corrected for them. Therefore, additional MR and prospective cohort studies are necessary to examine the causal relationship between serum UA levels and GDM risk, especially in different populations.
Our study has several advantages. First, our study included a well-matched retrospective design, making it even more compelling. Second, as far as we know, this is the first Mendelian randomized study to investigate the relationship between UA and GDM. The MR design effectively minimizes the potential biases caused by confounding and reverse causality in observational studies. However, this study had certain limitations. Firstly, consistent with previous MR studies, the SNPs employed in the present study explained only a portion of serum UA changes. In future studies, it will be necessary to identify additional UA susceptibility genes to investigate the causal relationship between these two factors. Secondly, our analysis was limited to specific racial populations, which limits its generalization to other populations. Finally, although we considered the possible GDM risk factors, the possibility of residual confounders could not be excluded.
In conclusion, although elevated serum UA levels were significantly related to an increased risk of GDM, the results of the MR study did not provide evidence of a causal relationship between serum UA levels and GDM risk.
Data availability
The datasets during the current study are not publicly available but are available from the corresponding author on reasonable request.
References
Classification and diagnosis of diabetes. Standards of Medical Care in Diabetes-2020 [J]. Diabetes Care. 2020;43(Suppl 1):S14–31.
SWEETING A, WONG J, MURPHY H R, et al. A clinical update on gestational diabetes mellitus [J]. Endocr Rev. 2022;43(5):763–93.
YUE C, YING C, LI X. Elevated serum uric acid is associated with gestational diabetes mellitus: an observational cohort study [J]. J Clin Endocrinol Metab. 2023;108(7):e480–6.
COPUR S, DEMIRAY A. Uric acid in metabolic syndrome: does uric acid have a definitive role? [J]. Eur J Intern Med. 2022;103:4–12.
HARYONO A, NUGRAHANINGSIH D A A, SARI D C R, et al. Reduction of serum uric acid associated with attenuation of renal injury, inflammation and macrophages M1/M2 ratio in hyperuricemic mice model [J]. Kobe J Med Sci. 2018;64(3):E107–14.
SU S, ZHANG E, GAO S, et al. Serum uric acid and the risk of gestational diabetes mellitus: a systematic review and meta-analysis [J]. Gynecol Endocrinol. 2023;39(1):2231101.
LAWLOR D A, HARBORD R M, STERNE JA, et al. Mendelian randomization: using genes as instruments for making causal inferences in epidemiology [J]. Stat Med. 2008;27(8):1133–63.
GHERGHINA ME, PERIDE I. TIGLIS M, Uric acid and oxidative stress-relationship with cardiovascular, metabolic, and renal impairment [J]. Int J Mol Sci, 2022, 23(6).
KEERMAN M, YANG F, HU H et al. Mendelian randomization study of serum uric acid levels and diabetes risk: evidence from the Dongfeng-Tongji cohort [J]. BMJ Open Diabetes Res Care, 2020, 8(1).
PFISTER R, BARNES D, LUBEN R, et al. No evidence for a causal link between uric acid and type 2 diabetes: a mendelian randomisation approach [J]. Diabetologia. 2011;54(10):2561–9.
METZGER B E, GABBE S G, PERSSON B, et al. International association of diabetes and pregnancy study groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy [J]. Diabetes Care. 2010;33(3):676–82.
Kanai M, Akiyama M, Takahashi A, et al. Genetic analysis of quantitative traits in the Japanese population links cell types to complex human diseases. Nat Genet. 2018;50(3):390–400.
FinnGen. FinnGen Documentation of R5 release. Accessed 11. June 2021. https://finngen.gitbook.io/documentation/
Hemani G, Zheng J, Elsworth B, Wade KH, Haberland V, Baird D, et al. The MR-Base platform supports systematic causal inference across the human phenome. Elife. 2018;7:e34408.
Burgess S, Butterworth A, Thompson SG. Mendelian randomization analysis with multiple genetic variants using summarized data. Genet Epidemiol. 2013;37(7):658–65.
Bowden J, Davey Smith G, Burgess S. Mendelian randomization with invalid instruments: effect estimation and bias detection through Egger regression. Int J Epidemiol. 2015;44(2):512–25.
Verbanck M, Chen CY, Neale B, Do R. Detection of widespread horizontal pleiotropy in causal relationships inferred from mendelian randomization between complex traits and diseases. Nat Genet. 2018;50(5):693–8.
Bowden J, Del Greco MF, Minelli C, Zhao Q, Lawlor DA, Sheehan NA, Thompson J, Davey Smith G. Improving the accuracy of two-sample summary-data mendelian randomization: moving beyond the NOME assumption. Int J Epidemiol. 2019;48(3):728–42.
C R, SAMAL S. Association of elevated first trimester serum uric acid levels with development of GDM [J]. J Clin Diagn Res. 2014;8(12):Oc01–5.
DUO Y, SONG S, ZHANG Y et al. Relationship between serum uric acid in early pregnancy and gestational diabetes mellitus: a prospective cohort study [J]. Endocrine, 2023.
Catov JM, Sun B, Bertolet M, et al. Changes in cardiometabolic risk factors before and after gestational diabetes: a prospective life-course analysis in CARDIA women. Obes (Silver Spring). 2020;28(8):1397–404.
Li Y, Ren X, He L, Li J, Zhang S, Chen W. Maternal age and the risk of gestational diabetes mellitus: a systematic review and meta-analysis of over 120 million participants. Diabetes Res Clin Pract. 2020;162:108044.
GHASEMI A. Uric acid-induced pancreatic β-cell dysfunction [J]. BMC Endocr Disord. 2021;21(1):24.
CHOI YJ, YOON Y, LEE K Y, et al. Uric acid induces endothelial dysfunction by vascular insulin resistance associated with the impairment of nitric oxide synthesis [J]. Faseb j. 2014;28(7):3197–204.
PARK JH, JIN Y M HWANGS, et al. Uric acid attenuates nitric oxide production by decreasing the interaction between endothelial nitric oxide synthase and calmodulin in human umbilical vein endothelial cells: a mechanism for uric acid-induced cardiovascular disease development [J]. Nitric Oxide. 2013;32:36–42.
MARUHASHI T, HISATOME I, KIHARA Y, et al. Hyperuricemia and endothelial function: from molecular background to clinical perspectives [J]. Atherosclerosis. 2018;278:226–31.
PLOWS J F, STANLEY J L, BAKER P N et al. The pathophysiology of gestational diabetes mellitus [J]. Int J Mol Sci, 2018, 19(11).
YU W, XIE D, YAMAMOTO T, et al. Mechanistic insights of soluble uric acid-induced insulin resistance: insulin signaling and beyond [J]. Rev Endocr Metab Disord. 2023;24(2):327–43.
DU T, SUN X. Associations of serum uric acid levels with cardiovascular health factors: differences by sex, age and body mass index in Chinese participants [J]. Eur J Intern Med. 2014;25(4):388–93.
HU X, WANG RONGS. Association between plasma uric acid and insulin resistance in type 2 diabetes: a mendelian randomization analysis [J]. Diabetes Res Clin Pract. 2021;171:108542.
ZHU Y, HU Y, HUANG T, et al. High uric acid directly inhibits insulin signalling and induces insulin resistance [J]. Biochem Biophys Res Commun. 2014;447(4):707–14.
SAUTIN Y Y, NAKAGAWA T. Adverse effects of the classic antioxidant uric acid in adipocytes: NADPH oxidase-mediated oxidative/nitrosative stress [J]. Am J Physiol Cell Physiol. 2007;293(2):C584–96.
MAGED A M, MOETY G A, MOSTAFA W A, et al. Comparative study between different biomarkers for early prediction of gestational diabetes mellitus [J]. J Matern Fetal Neonatal Med. 2014;27(11):1108–12.
GüNGöR ES, DANIŞMAN N. Relationship between serum uric acid, creatinine, albumin and gestational diabetes mellitus [J]. Clin Chem Lab Med. 2006;44(8):974–7.
Yan D, Wang J, Jiang F, et al. A causal relationship between uric acid and diabetic macrovascular disease in Chinese type 2 diabetes patients: a mendelian randomization analysis. Int J Cardiol. 2016;214:194–9.
Sluijs I, Holmes MV, van der Schouw YT, et al. A mendelian randomization study of circulating uric acid and type 2 diabetes. Diabetes. 2015;64:3028–36.
KEENAN T, ZHAO W. Causal assessment of serum urate levels in cardiometabolic diseases through a mendelian randomization study [J]. J Am Coll Cardiol. 2016;67(4):407–16.
Funding
This study was funded by the Natural Science Foundation of China (82270852), the Science and Technology Innovation Action Plan “Biomedical Technology Support Special Project” of Shanghai (21S31901800).
Author information
Authors and Affiliations
Contributions
Nuerbiya·Xilifu: Clinical data collection, Formal analysis, Writing original draft. Zhang Rui: Data analysis, Supervision, Writing review and editing. Miyeshaer·Maimaiti: Clinical data collection. Li Zhangyan: Clinical data collection. Zang Shufei and Yang Ju: Subject design and supervision. Liu Jun: Conceptualization, Supervision, Writing review and editing. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethical approval
This study was approved by the Ethics Committee of Shanghai Fifth People’s Hospital Fudan University. Informed consent was obtained from patients or their representatives, and the protocol conformed with the Declaration of Helsinki.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Xilifu, N., Zhang, R., Dai, Y. et al. Uric acid and risk of gestational diabetes mellitus: an observational study and mendelian randomization analysis. Reprod Biol Endocrinol 22, 108 (2024). https://doi.org/10.1186/s12958-024-01278-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12958-024-01278-8