Abstract
Enterovirus 71 (EV-71) has strong neurotropism, and it is the main pathogen causing severe hand, foot, and mouth disease (HFMD). In clinical observations, significant differences were observed in the severity and prognosis of HFMD among children who were also infected with EV-71. Genetic differences among individuals could be one of the important causes of differences in susceptibility to EV-71–induced HFMD. As P-selectin glycoprotein ligand-1 (PSGL-1) is an important receptor of EV-71, the correlation between single-nucleotide polymorphisms (SNPs) in PSGL-1 and the susceptibility to severe HFMD following EV-71 infection is worth studying. Given the role of PSGL-1 in immunity, the correlations between PSGL-1 SNPs and the immune status after EV-71 infection are also worth studying. Meanwhile, PSGL-1 variable number of tandem repeats (VNTR) represents a research hotspot in cardiovascular and cerebrovascular diseases, but PSGL-1 VNTR polymorphism has not been investigated in HFMD caused by EV-71 infection. In this study, specific gene fragments were amplified by polymerase chain reaction, and PSGL-1 VNTR sequences were genotyped using an automatic nucleic acid analyzer. The correlations of PSGL-1 VNTR polymorphism with the susceptibility to EV-71–associated severe HFMD and the post-infection immune status were analyzed. The PSGL-1 VNTR A allele was identified as a susceptible SNP for severe HFMD. The risk of severe HFMD was higher for AA + AB genotype carriers than for BB genotype carriers. The counts of peripheral blood lymphocyte subsets were lower in AA + AB genotype carries than in BB genotype carries. In conclusion, PSGL-1 VNTR polymorphism is associated with the susceptibility to EV-71–induced severe HFMD and the immune status after infection. PSGL-1 VNTR might play a certain role in the pathogenesis of severe cases.
Similar content being viewed by others
Introduction
Hand, foot, and mouth disease (HFMD) is more common in children younger than 5 years. It was first reported in New Zealand in 1957 and named according to its clinical symptoms [1]. In the past 30 years, HFMD has been prevalent in the Asia–Pacific region, and it has caused several outbreaks worldwide, becoming a global public health issue. HFMD can be classified as general or severe HFMD. General HFMD is mild, and the course of the disease is limited to the eruption period. The disease can generally be cured within 1 week, and its prognosis is good. Conversely, severe HFMD progresses rapidly after onset, it involves the nervous system, and it carries a high fatality rate.
HFMD is an acute infectious disease caused by various intestinal viruses [2]. These viruses are mainly transmitted through the digestive tract or respiratory droplets. Infection can also occur through contact with an infected person’s skin or mucous membranes or from discharge from blisters. The main clinical manifestations after infection are rashes on the hands and feet and oral blisters [3, 4]. A small number of pediatric patients progress rapidly, and they can experience critical symptoms such as encephalitis, meningoencephalitis, neurogenic pulmonary edema, circulatory system disorders, and even death within 1–5 days of onset [5,6,7].
Similarly as poliovirus, enterovirus 71 (EV-71) is a neurotropic virus [8,9,10]. As one of the main pathogens causing severe and fatal cases of HFMD, EV-71 has received extensive academic attention. In clinical observation, significant differences in the severity of clinical symptoms, disease outcomes, and prognosis were observed among children who were also infected with EV-71. As the first important gateway for viruses to enter the human body, virus receptors determine the host range and specificity of infected tissues [11]. Genetic differences among individuals lead to varying sensitivity of receptors to EV-71, which could be an important cause of differences in the susceptibility to severe EV-71-associated HFMD [9]. Yamayoushi and Nishimura confirmed in cell experiments that scavenger receptor class B member 2 (SCARB2) and P-selectin glycoprotein ligand-1 (PSGL-1) are receptors for EV-71 [12, 13]. In the 2018 edition of the HFMD diagnosis and treatment guidelines, SCARB2 and PSGL-1 were clearly identified as the major receptors of EV-71 [14]. SCARB2 is widely expressed on various cell surfaces, and it plays important roles in viral infection and replication processes. We previously speculated that SCARB2 is related to the susceptibility to EV-71–associated severe HFMD, but our study found that SCARB2 single-nucleotide polymorphisms (SNPs) were not sufficient to cause severe HFMD [15]. This is consistent with the findings of Yen et al. [9]. Nishimura et al. revealed that PSGL-1 is not the receptor for all EV-71 strains, which can be divided into two distinct types based on their affinity for PSGL-1: PSGL-1–binding (PB) and non-PSGL-1–binding [12]. In recent years, the dominant circulating strains in China are mainly PBC4 subtypes belonging to the PB type [16,17,18,19,20]. As an important receptor of PB EV-71, the correlation between PSGL-1 SNPs and the susceptibility to severe HFMD in patients infected with PB EV-71 is worth studying. PSGL-1 is expressed on the surface of almost all white blood cells, it participates in inflammatory responses, and it has a certain correlation with the immune status. Therefore, the correlation between PSGL-1 SNPs and the immune status after PB EV-71 infection is worth studying.
Variable number of tandem repeats (VNTR) in PSGL-1 represents a research hotspot in cardiovascular and cerebrovascular diseases, but to our knowledge, there is currently no research related to PSGL-1 VNTR polymorphism in HFMD. This study analyzed the correlation between PSGL-1 VNTR polymorphism and the susceptibility to PB EV-71–associated severe HFMD, as well as the immune status after infection, to clarify individual differences in the mechanisms of EV-71–induced severe and fatal disease and provide a research basis for prevention and personalized treatment.
Materials and methods
Clinical data and sample collection
Two hundred children with HFMD who were positive for EV-71 infection based on a nucleic acid test in our hospital were identified. Based on the “Guidelines for the Diagnosis and Treatment of Hand, Foot, and Mouth Disease” (2018) [14], the disease was limited to stage 1 (eruption stage: most cases manifested as rashes on the hands, feet, mouth, hips, and other parts, some cases only manifested as herpetic pharyngitis, and a few individuals lacked rashes) in 100 patients, who recovered during this stage. These 100 patients with general HFMD were enrolled as the control group. Meanwhile, the disease progressed to stage 2 (nervous system involvement stage: manifested as poor mental state, lethargy, skittish, headache, vomiting, limb shaking, stiff neck, and other symptoms), stage 3 (early stage of cardiopulmonary failure: manifested as increased heart rate and respiration, cold sweat, cool extremities, skin discoloration, and elevated blood pressure), or stage 4 (cardiopulmonary failure stage: manifested as tachycardia or bradycardia, tachypnea, cyanosis of lips, cough of pink foam sputum or bloody fluid, decreased blood pressure, shock, convulsion, and serious disturbance of consciousness) in 100 patients. These patients with severe HFMD were enrolled as the case group.All patients participated in the study voluntarily, and all enrolled patients met the inclusion criteria. Informed consent was obtained from all subjects and their parent(s)/legal guardian(s). The data on peripheral blood lymphocyte subsets and immunoglobulin assays were collected on the day of admission before patients were treated. Peripheral venous blood (3 mL) and feces (5 g) were collected from each patient and stored at − 80 °C for later use [15].
EV-71 VP1 nucleotide sequence detection
RNA extraction and polymerase chain reaction (PCR) targeting VP1 of EV-71 were performed using fecal samples and an EV-71 nucleic acid assay kit (Shanghai ZJ Bio-Tech Co., Ltd., Shanghai, China). PCR products sent for sequencing (Sangon Biotech Co., Ltd., Shanghai, China). The sequencing results were compared with those in the GenBank database, and the typing results were obtained.
DNA extraction from peripheral venous blood
DNA was extracted from blood samples using a TIANamp Blood DNA Kit (Tiangen, Beijing, China). DNA samples were analyzed using a NanoDrop 2000, and 1.25% agarose gel electrophoresis was performed. DNA was quantified and transferred to a 96-well plate for storage at − 20 °C for later use [15].
VNTR SNP typing
Primer design and synthesis
The primers were designed as described previously [21] and synthesized by biological companies. The primer sequences are presented in Table 1.
PCR targeting VNTR
PCR was conducted in 30-µL mixtures containing 1 µL of DNA (20 ng/µL), 27 µL of Easy Mix, and 1 µL each of primers F and 1 R. The PCR conditions were as follows: one cycle at 96 °C for 5 min; 10 cycles at 96 °C for 20 s, 62 °C for 30 s, and 72 °C for 60 s; 35 cycles at 96 °C for 20 s, 52 °C for 30 s, and 72 °C for 60 s; and a final extension step at 72 °C for 5 min.
VNTR PCR product analysis
PCR products were analyzed using a Bioptic Qsep100 automatic nucleic acid analyzer (Guangding Company, Taiwan, China).
Statistical analysis
SPSS v23.0 software was used for statistical processing and analysis. The chi-squared test was used to compare the characteristics of the subjects, and the differences in age and sex between the case and control groups were analyzed. Hardy–Weinberg equilibrium was used to calculate whether the selected sample was taken from a random population. Fisher’s exact test was used to compare VNTR allele frequencies between the groups. The differences in VNTR genotypes and alleles were compared by logistic regression analysis. Odds ratios (ORs) were presented with their 95% confidence intervals (CIs). OR > 1 indicated a pathogenic effect, whereas OR < 1 indicated a protective effect. Peripheral blood lymphocyte subsets and immunoglobulin assay data were normally distributed, and they were expressed as the mean ± standard deviation and compared between the groups using an independent-samples t-test. Non-normally distributed data were presented as the median (interquartile range) and compared between the groups using the Mann–Whitney U test. P < 0.05 indicated statistical difference.
Results
EV-71 VP1 nucleotide sequence analysis
The VP1 nucleotide sequence of five samples were compared with the NCBI (HQ882182) VP1 nucleotide sequence. The similarities of the sequences with the NCBI sequence were 95.96%, 96.07%, 95.96%, 96.18%, and 95.63%, respectively. The infecting strain of EV-71 in the study population was the C4 subtype, conforming to the epidemic strain status in Mainland China. A comparison of nucleotide sequences is presented in Fig. 1.
Characteristics
Table 2 presents the characteristics of the subjects. No differences in sex and age were observed between the case and control groups (P > 0.05).
VNTR Genotyping
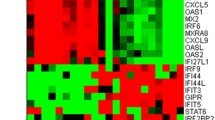
Alleles A, B, and C of PSGL-1 VNTR were 558, 538, and 498 bp, respectively, in length. Four genotypes were identified, namely AA (558 and 558 bp), AB (558 and 538 bp), BB (538 and 538 bp), and BC (538 and 498 bp), as presented in Fig. 2.
Hardy–Weinberg equilibrium
Table 3 presents the frequency distribution and comparison of PSGL-1 VNTR alleles and genotypes between the case and control groups. No significant difference in the distribution of alleles or genotypes was observed between the two groups (P > 0.05), which was consistent with Hardy–Weinberg equilibrium, illustrating that the selected sample was a random population. Because of the small numbers of patients with the BC genotype and C allele, statistical analysis was not conducted.
Analysis of VNTR allele frequencies using fisher’s exact test
The frequencies of the VNTR A and B alleles were analyzed, as presented in Table 4. A significant difference in their frequencies was observed between the groups (P = 0.037), indicating that VNTR alleles might be related to the pathogenicity of EV-71.
Logistic regression analysis of VNTR alleles
As presented in Table 5, the VNTR A allele appeared to be related to the pathogenicity of EV-71 (OR = 1.558, 95% CI = 1.025–2.367, P = 0.038).
Logistic regression analysis of VNTR genotypes
In the recessive models, AA + AB genotype carriers had an increased risk of severe disease than BB genotype carriers (OR = 0.37, 95% CI = 0.15–0.88, P = 0.025, Table 6).
Association of the PSGL-1 VNTR genotype with the immune status
As illustrated in Table 7, the mean counts of peripheral blood CD3+, CD4+, and CD8+ T cells were all lower for the AA + AB genotype than for the BB genotype (P < 0.05), indicating a high correlation between PSGL-1 VNTR and peripheral blood lymphocyte subsets. However, IgA, IgG, and IgM levels did not differ between the genotypes.
Discussion
PSGL-1 is a transmembrane glycoprotein with a homologous dimer structure. The protein has a molecular weight of 120 kDa and a length of 412 amino acids [22, 23]. The PSGL-1 gene is located on human chromosome 12 (12q24). VNTR polymorphism of the PSGL-1 gene includes the A, B, and C alleles. The A allele contains repeats 1–16, the B allele lacks repeats 2 (QTTQPVPTEA), and the C allele lacks repeats 9 (QTTAPAAMEA) and 10 (QTTPPAAMEA). There are significant differences in the distribution of VNTR polymorphism and genotypes among different regions and races. Bugert et al. [24] conducted PSGL1 VNTR genotyping in 5071 white German individuals. The frequencies of alleles A, B, and C were 81.9%, 16.9%, and 1.2%, respectively, and genotypes AA (66.7%), AB (28.3%), AC (2.1%), BB (2.6%), BC (0.3%), and CC (0.05%) were detected. Hancer et al. [25] found that the frequencies of the A, B, and C alleles in 175 Turkish individuals were 79.4%, 19.2%, and 1.4% respectively, and genotypes AA (64%), AB (29.1%), AC (1.7%), BB (4.6%), and CC (0.6%), but not BC, were found. Afshar-Kharghan et al. [26] reported that the frequencies of the A, B, and C alleles were 65%, 35%, and 0%, respectively, among 68 Japanese individuals. The AA (38.0%), AB (55.0%), and BB genotypes (7.0%) were found, but no individuals carried the AC, BC, or CC genotype. The current study genotyped 200 children with HFMD, and the frequencies of PSGL-1 VNTR alleles A, B, and C were 65.75%, 34%, and 0.25%, respectively. Genotypes AA (45.5%), AB (40.5%), BB (13.5%), and BC (0.5%) were observed, but the AC and CC genotypes were not found. These comparative data illustrated that the A allele is most common in human PSGL-1 VNTR, followed by allele B, and allele C is the least common. The distribution of VNTR alleles and genotypes in Türkiye is similar to that in Germany. However, Japanese and Chinese people are Asian by ethnicity. Compared with the findings in Germany and Türkiye, the rates of the A allele and AA genotype were lower in Asians, whereas those of the B allele and AB genotype were higher. In addition, the AC and CC genotypes were not found in Asians. PSGL-1 VNTR is a research hotspot in cardiovascular and cerebrovascular diseases. Bugert and colleagues found that alleles B and C had a protective effect against cerebrovascular disease but not against coronary heart disease or deep vein thrombosis. Lozano et al. [27] reported that the short PSGL1 allele significantly reduced the ability of neutrophils to bind to platelets. Short alleles are associated with a reduced risk of cerebrovascular disease but not coronary heart disease or deep vein thrombosis. Roldan et al. [28] indicated that the short PSGL-1 allele has a protective effect against coronary artery thrombosis. PSGL-1 VNTR has not been reported in patients with HFMD caused by EV-71 infection. By comparing the allele frequencies between the case and control groups using Fisher’s exact test and comparing the differences between genotypes and alleles using logistic regression analysis, we found that the PSGL-1 VNTR A allele is a susceptible SNP for HFMD. Compared with BB genotype carriers, AA + AB genotype carriers exhibited an increased risk of serious disease. PSGL-1, as an important receptor for PB EV-71, is associated with susceptibility to severe HFMD, in line with previous reports [10, 29,30,31,32].
PSGL-1 is continuously expressed on human leukocytes, and it is a ligand for SELP. In the early stage of inflammation, platelet α-granules and the Weibel–Palade bodies of endothelial cells rapidly fuse with the plasma membrane after stimulation by viruses, thrombin, histamine, complement, and oxygen free radicals, leading to SELP expression on their surfaces. PSGL-1 on the surface of white blood cells interacts with SELP to rapidly initiate mutual adhesion among white blood cells, endothelial cells, and platelets. Stimulated vascular endothelial cells and platelet Weibel–Palade bodies release SELP, whereas vascular endothelial cells release a series of inflammatory and chemotactic factors to recruit more white blood cells, further promoting the inflammatory response [33,34,35]. Numerous studies have illustrated that multiple immune function indicators are abnormal in children with HFMD [10, 21, 36]. Cosan et al. [21] found that VNTR polymorphism of the PSGL-1 gene can lead to differences in the length of its extracellular region, affecting the distance from its SELP-binding site to the cell surface and leading to individual differences in immune response. The VNTR polymorphism of PSGL-1 is located downstream of the SELP-binding region. The length of the PSGL-1 extracellular domain could be the key factor affecting SELP binding [21, 37, 38]. Allele A is the longest allele, and it is associated with the greatest binding affinity for SELP, which activates platelets and endothelial cells. The shorter B and C alleles lead to lower affinity for SELP. These differences might affect post-infection immunity through the interaction between SELP and PSGL-1. The CD3+ T cell count mainly refers to the total number of mature T cells in peripheral blood, whereas CD4+ and CD8+ T cells play immunomodulatory roles. Among them, CD4+ T cells mainly play an inducing role, and an increase in their count represents enhanced cellular immunity. CD8+ T cells mainly exert inhibitory effects, and an increase in their count indicates the occurrence of immune suppression. IgA is a secreted antibody that plays a major role in local anti-infection responses in the body’s mucosa. IgM helps to clear viruses in the early stages of infection. IgG is the only antibody that can pass through the placenta, and it plays an important role in neonatal anti-infection activity. This study analyzed the correlation between PSGL-1 VNTR polymorphism and the immune status after PB EV-71 infection. The results illustrated that peripheral blood CD3+, CD4+, and CD8+ T cell counts were significantly lower in patients with the AA + AB genotype than in those with the BB genotype. During the EV-71 outbreak in Taiwan, several studies [30, 39] found that children with severe HFMD exhibited significant T cell depletion. There was no statistically significant difference in peripheral blood immunoglobulin levels between children with the AA + AB genotype children and those with the BB genotype, suggesting immune dysfunction in children infected with EV-71. As PSGL-1 is a ligand for SELP, PSGL-1 VNTR polymorphism is associated with the immune status after PB EV-71-associated HFMD.
This study had some limitations. The sample size was not large, which might have led to the omission of rare genotypes, making it impossible to conduct a more comprehensive analysis. The lengths of PSGL-1 VNTR alleles differ, and various combinations of these alleles can cause conformational differences within the genotype, which might result in differences in receptor sensitivity to viruses. The configuration difference is greatest for the AC genotype, which might result in extremely low binding efficiency. The CC genotype is the shortest genotype, and its binding efficiency might also be low. It is worth studying the correlation of the AC and CC genotypes of PSGL-1 with the susceptibility to severe HFMD and the immune status after infection. Unfortunately, no patients carried the AC or CC genotype in this study, making it impossible to further analyze these relationships. We will continue to expand the sample size and develop transgenic animal models carrying the AC and CC genotypes to comprehensively clarify the structure and function of PSGL-1. This will help predict and treat critically ill patients infected with EV-71. At the same time, such studies will also provide some ideas for the application of receptor antagonists in clinical treatment.
Conclusion
The PSGL-1 VNTR A allele is a susceptible SNP for severe HFMD. AA + AB genotype carriers had a higher risk of severe HFMD than BB genotype carriers. PSGL-1 VNTR polymorphism was associated with the susceptibility to severe HFMD caused by EV-71 and the immune status after infection.
Data availability
No datasets were generated or analysed during the current study.
References
Sarma N. Hand, foot, and mouth disease: current scenario and Indian perspective. Indian J Dermatol Venereol Leprol. 2013 Mar-Apr;79(2):165 – 75. https://doi.org/10.4103/0378-6323.107631. PMID: 23442455.
Tikute S, Lavania M, Hand. Foot, and Mouth Disease (HFMD) in India: a review on clinical manifestations, Molecular Epidemiology, Pathogenesis, and Prevention. Indian Dermatol Online J. 2023;14(4):475–81. https://doi.org/10.4103/idoj.idoj_423_22. PMID: 37521225; PMCID: PMC10373810.
Lee YP, Yu CK, Wong TW, Chen LC, Huang BM. Cordycepin inhibits Enterovirus A71 Replication and protects host cell from Virus-Induced cytotoxicity through Adenosine Action Pathway. Viruses. 2024;16(3):352. https://doi.org/10.3390/v16030352. PMID: 38543718; PMCID: PMC10974990.
Esposito S, Principi N. Hand, foot and mouth disease: current knowledge on clinical manifestations, epidemiology, aetiology and prevention. Eur J Clin Microbiol Infect Dis. 2018;37(3):391–8. https://doi.org/10.1007/s10096-018-3206-x. Epub 2018 Feb 6. PMID: 29411190.
Fang CY, Liu CC. Novel strategies for the development of hand, foot, and mouth disease vaccines and antiviral therapies. Expert Opin Drug Discov. 2022;17(1):27–39. Epub 2021 Aug 19. PMID: 34382876.
Min N, Ong YHB, Han AX, Ho SX, Yen EWP, Ban KHK, Maurer-Stroh S, Chong CY, Chu JJH. An epidemiological surveillance of hand foot and mouth disease in paediatric patients and in community: a Singapore retrospective cohort study, 2013–2018. PLoS Negl Trop Dis. 2021;15(2):e0008885. https://doi.org/10.1371/journal.pntd.0008885. PMID: 33566802; PMCID: PMC7901731.
Yang A, Luo Y, Yang J, Xie T, Wang W, Wan X, Wang K, Pang D, Yang D, Dai H, Wu J, Meng S, Guo J, Wang Z, Shen S. Quantitation of Enterovirus A71 empty and full particles by Sedimentation Velocity Analytical Ultracentrifugation. Viruses. 2024;16(4):573. https://doi.org/10.3390/v16040573. PMID: 38675915; PMCID: PMC11053756.
Ong KC, Wong KT. Understanding Enterovirus 71 neuropathogenesis and its impact on other Neurotropic enteroviruses. Brain Pathol. 2015;25(5):614–24. https://doi.org/10.1111/bpa.12279. PMID: 26276025; PMCID: PMC8029433.
Yen TY, Shih WL, Huang YC, Lee JT, Huang LM, Chang LY. Polymorphisms in enterovirus 71 receptors associated with susceptibility and clinical severity. PLoS ONE. 2018;13(11):e0206769. https://doi.org/10.1371/journal.pone.0206769. PMID: 30395634; PMCID: PMC6218064.
Huang HI, Shih SR. Neurotropic enterovirus infections in the Central Nervous System. Viruses. 2015;7(11):6051–66. https://doi.org/10.3390/v7112920. PMID: 26610549; PMCID: PMC4664993.
Lu MY, Lin YL, Kuo Y, Chuang CF, Wang JR, Liao F. Muscle tissue damage and Recovery after EV71 infection correspond to dynamic macrophage phenotypes. Front Immunol. 2021;12:648184. https://doi.org/10.3389/fimmu.2021.648184. PMID: 34305887; PMCID: PMC8299204.
Nishimura Y, Shimojima M, Tano Y, Miyamura T, Wakita T, Shimizu H. Human P-selectin glycoprotein ligand-1 is a functional receptor for enterovirus 71. Nat Med. 2009;15(7):794–7. https://doi.org/10.1038/nm.1961. Epub 2009 Jun 21. PMID: 19543284.
Yamayoshi S, Iizuka S, Yamashita T, Minagawa H, Mizuta K, Okamoto M, Nishimura H, Sanjoh K, Katsushima N, Itagaki T, Nagai Y, Fujii K, Koike S. Human SCARB2-dependent infection by coxsackievirus A7, A14, and A16 and enterovirus 71. J Virol. 2012;86(10):5686–96. https://doi.org/10.1128/JVI.00020-12. Epub 2012 Mar 21. PMID: 22438546; PMCID: PMC3347270.
Li XW, Ni X, Qian SY, Wang Q, Jiang RM, Xu WB, Zhang YC, Yu GJ, Chen Q, Shang YX, Zhao CS, Yu H, Zhang T, Liu G, Deng HL, Gao J, Ran XG, Yang QZ, Xu BL, Huang XY, Wu XD, Bao YX, Chen YP, Chen ZH, Liu QQ, Lu GP, Liu CF, Wang RB, Zhang GL, Gu F, Xu HM, Li Y, Yang T. Chinese guidelines for the diagnosis and treatment of hand, foot and mouth disease (2018 edition). World J Pediatr. 2018;14(5):437–447. https://doi.org/10.1007/s12519-018-0189-8. Epub 2018 Oct 3. PMID: 30280313.
Wang X, Liu H, Li Y, Su R, Liu Y, Qiao K. Relationship between polymorphism of receptor SCARB2 gene and clinical severity of enterovirus-71 associated hand-foot-mouth disease. Virol J. 2021;18(1):132. https://doi.org/10.1186/s12985-021-01605-0. PMID: 34193186; PMCID: PMC8244142.
Li R, Liu L, Mo Z, Wang X, Xia J, Liang Z, Zhang Y, Li Y, Mao Q, Wang J, Jiang L, Dong C, Che Y, Huang T, Jiang Z, Xie Z, Wang L, Liao Y, Liang Y, Nong Y, Liu J, Zhao H, Na R, Guo L, Pu J, Yang E, Sun L, Cui P, Shi H, Wang J, Li Q. An inactivated enterovirus 71 vaccine in healthy children. N Engl J Med. 2014;370(9):829 – 37. https://doi.org/10.1056/NEJMoa1303224. PMID: 24571755.
Zhu F, Xu W, Xia J, Liang Z, Liu Y, Zhang X, Tan X, Wang L, Mao Q, Wu J, Hu Y, Ji T, Song L, Liang Q, Zhang B, Gao Q, Li J, Wang S, Hu Y, Gu S, Zhang J, Yao G, Gu J, Wang X, Zhou Y, Chen C, Zhang M, Cao M, Wang J, Wang H, Wang N. Efficacy, safety, and immunogenicity of an enterovirus 71 vaccine in China. N Engl J Med. 2014;370(9):818 – 28. https://doi.org/10.1056/NEJMoa1304923. PMID: 24571754.
Liang Z, Mao Q, Gao Q, Li X, Dong C, Yu X, Yao X, Li F, Yin W, Li Q, Shen X, Wang J. Establishing China’s national standards of antigen content and neutralizing antibody responses for evaluation of enterovirus 71 (EV71) vaccines. Vaccine. 2011;29(52):9668–74. https://doi.org/10.1016/j.vaccine.2011.10.018. Epub 2011 Oct 19. PMID: 22015395.
Xie H, Yang E, Wang C, Peng C, Ji L. Targeting HDAC11 activity by FT895 restricts EV71 replication. Virus Res. 2023;330:199108. https://doi.org/10.1016/j.virusres.2023.199108. Epub 2023 Apr 15. PMID: 37024058; PMCID: PMC10194106.
Zhu P, Ji W, Li D, Li Z, Chen Y, Dai B, Han S, Chen S, Jin Y, Duan G. Current status of hand-foot-and-mouth disease. J Biomed Sci. 2023;30(1):15. https://doi.org/10.1186/s12929-023-00908-4. PMID: 36829162; PMCID: PMC9951172.
Cosan F, Oku B, Gedar Totuk OM, Abaci N, Ustek D, Diz Kucukkaya R, Gul A. The association between P selectin glycoprotein ligand 1 gene variable number of tandem repeats polymorphism and risk of thrombosis in Behçet’s disease. Int J Rheum Dis. 2018;21(12):2175–9. Epub 2017 Aug 14. PMID: 28809090.
Carlow DA, Gossens K, Naus S, Veerman KM, Seo W, Ziltener HJ. PSGL-1 function in immunity and steady state homeostasis. Immunol Rev. 2009;230(1):75–96. https://doi.org/10.1111/j.1600-065X.2009.00797.x. PMID: 19594630.
Yamayoshi S, Fujii K, Koike S. Receptors for enterovirus 71. Emerg Microbes Infect. 2014;3(7):e53. https://doi.org/10.1038/emi.2014.49. Epub 2014 Jul 16. PMID: 26038749; PMCID: PMC4126179.
Bugert P, Hoffmann MM, Winkelmann BR, Vosberg M, Jahn J, Entelmann M, Katus HA, März W, Mansmann U, Boehm BO, Goerg S, Klüter H. The variable number of tandem repeat polymorphism in the P-selectin glycoprotein ligand-1 gene is not associated with coronary heart disease. J Mol Med (Berl). 2003;81(8):495–501. https://doi.org/10.1007/s00109-003-0459-2. Epub 2003 Jul 16. PMID: 12879153.
Hancer VS, Diz-Kucukkaya R, Nalcaci M. Turkish population data on the factor XIII Val34Leu,glycoprotein (GP)Ibalpha Kozak and P-selectin glycoprotein ligand 1 (PSGL-1) loci. Cell Biochem Funct. 2005 Jan-Feb;23(1):55 – 8. https://doi.org/10.1002/cbf.1150. PMID: 15386532.
Afshar-Kharghan V, Diz-Küçükkaya R, Ludwig EH, Marian AJ, López JA. Human polymorphism of P-selectin glycoprotein ligand 1 attributable to variable numbers of tandem decameric repeats in the mucinlike region. Blood. 2001;97(10):3306-7. https://doi.org/10.1182/blood.v97.10.3306. PMID: 11342464.
Lozano ML, González-Conejero R, Corral J, Rivera J, Iniesta JA, Martinez C, Vicente V. Polymorphisms of P-selectin glycoprotein ligand-1 are associated with neutrophil-platelet adhesion and with ischaemic cerebrovascular disease. Br J Haematol. 2001;115(4):969 – 76. https://doi.org/10.1046/j.1365-2141.2001.03151.x. PMID: 11843835.
Roldán V, González-Conejero R, Marín F, Pineda J, Vicente V, Corral J. Short alleles of P-selectin glycoprotein ligand-1 protect against premature myocardial infarction. Am Heart J. 2004;148(4):602-5. https://doi.org/10.1016/j.ahj.2004.04.020. PMID: 15459589.
Koyuncu OO, Hogue IB, Enquist LW. Virus infections in the nervous system. Cell Host Microbe. 2013;13(4):379–93. https://doi.org/10.1016/j.chom.2013.03.010. PMID: 23601101; PMCID: PMC3647473.
Lin TY, Hsia SH, Huang YC, Wu CT, Chang LY. Proinflammatory cytokine reactions in enterovirus 71 infections of the central nervous system. Clin Infect Dis. 2003;36(3):269–74. https://doi.org/10.1086/345905. Epub 2003 Jan 13. PMID: 12539066.
Zhang Y, Cui W, Liu L, Wang J, Zhao H, Liao Y, Na R, Dong C, Wang L, Xie Z, Gao J, Cui P, Zhang X, Li Q. Pathogenesis study of enterovirus 71 infection in rhesus monkeys. Lab Invest. 2011;91(9):1337–50. https://doi.org/10.1038/labinvest.2011.82. Epub 2011 May 9. PMID: 21555996.
Gu YY, Shi K, Yao S, Yang X, Liu YH, Tang L, Dang YW, Chen G, Feng ZB, Pan HB. Morphological characteristics of fatal pediatric hand, foot and mouth disease: a clinicopathological study with related receptors of EV71. Pathol Res Pract. 2017;213(9):1144–51. Epub 2017 Jul 6. PMID: 28756983.
Dong ZM, Chapman SM, Brown AA, Frenette PS, Hynes RO, Wagner DD. The combined role of P- and E-selectins in atherosclerosis. J Clin Invest. 1998;102(1):145–52. https://doi.org/10.1172/JCI3001. PMID: 9649568; PMCID: PMC509076.
Norman KE, Moore KL, McEver RP, Ley K. Leukocyte rolling in vivo is mediated by P-selectin glycoprotein ligand-1. Blood. 1995;86(12):4417-21. PMID: 8541529.
Klinkhardt U, Dragutinovic I, Harder S. P-selectin (CD62p) and P-selectin glycoprotein ligand-1 (PSGL-1) polymorphisms: minor phenotypic differences in the formation of platelet-leukocyte aggregates and response to clopidogrel. Int J Clin Pharmacol Ther. 2005;43(6):255 – 63. https://doi.org/10.5414/cpp43255. PMID: 15968882.
Tinoco R, Otero DC, Takahashi AA, Bradley LM. PSGL-1: a New Player in the Immune Checkpoint Landscape. Trends Immunol. 2017;38(5):323–35. https://doi.org/10.1016/j.it.2017.02.002. Epub 2017 Mar 2. PMID: 28262471; PMCID: PMC5411281.
Barbaux S, Poirier O, Pincet F, Hermand P, Tiret L, Deterre P. The adhesion mediated by the P-selectin P-selectin glycoprotein ligand-1 (PSGL-1) couple is stronger for shorter PSGL-1 variants. J Leukoc Biol. 2010;87(4):727 – 34. https://doi.org/10.1189/jlb.0609408. Epub 2010 Jan 5. PMID: 20051472.
Ozben B, Diz-Kucukkaya R, Bilge AK, Hancer VS, Oncul A. The association of P-selectin glycoprotein ligand-1 VNTR polymorphisms with coronary stent restenosis. J Thromb Thrombolysis. 2007;23(3):181-7. https://doi.org/10.1007/s11239-006-9020-9. PMID: 17221329.
Wang SM, Lei HY, Huang KJ, Wu JM, Wang JR, Yu CK, Su IJ, Liu CC. Pathogenesis of enterovirus 71 brainstem encephalitis in pediatric patients: roles of cytokines and cellular immune activation in patients with pulmonary edema. J Infect Dis. 2003;188(4):564–70. https://doi.org/10.1086/376998. Epub 2003 Jul 23. PMID: 12898444.
Acknowledgements
The authors gratefully acknowledge the editors and anonymous reviewers for their valuable comments on this manuscript. We thank Medjaden Inc. for its assistance in the preparation of this manuscript.
Funding
This research was funded by the Tianjin Key Medical Discipline (Specialty) Construction Project (grant number: TJYXZDXK-059B to YL, number: ZD04).
Author information
Authors and Affiliations
Contributions
Conceptualization and methodology, Y. L. and Y. M.; software and validation, X. W. and J. Q.; formal analysis, X. W.; investigation, X. W., J. Q., Y. M., Y. L., Y. C., and K. Q.; resources, Y. L. and Y. M.; writing—original draft preparation, X. W.; writing—review and editing, X. W., and J. Q.; supervision, Y. L. and Y. M.; project administration, Y. L.; funding acquisition, Y. L. and X. W. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
All procedures performed in studies involving human participants were in accordance with the guidelines of the Declaration of Helsinki, and the protocol was approved by the Institutional Review Board of Medical Ethics Committee of Tianjin Second People’s Hospital (Approval Certificate of Ethical Review No. 201825, No. 202142). Informed consent was obtained from all subjects and their parents/legal guardian(s).
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wang, X., Qian, J., Mi, Y. et al. Correlations of PSGL-1 VNTR polymorphism with the susceptibility to severe HFMD associated with EV-71 and the immune status after infection. Virol J 21, 187 (2024). https://doi.org/10.1186/s12985-024-02461-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12985-024-02461-4