Abstract
Background
There is a conceptual overlap between negative and depressive symptoms, requiring further exploration to advance the understanding of negative symptoms. The aim of this study was to examine psychometric properties of the Clinical Assessment Interview for Negative Symptoms (CAINS) in patients with depression, and to explore the relationship between the negative and affective symptoms domains.
Methods
Fifty-one patients with a depressive episode were included and interviewed with the CAINS and the Brief Psychiatric Rating Scale—Expanded (BPRS-E). Self-reported depressive symptoms were collected with the Montgomery-Asberg Depression Rating Scale (MADRS-S). Inter-rater agreement, internal consistency and validity measures were examined, as were correlations between negative and affective symptoms.
Results
The intraclass correlation for the CAINS motivation and pleasure subscale (CAINS-MAP) was 0.98 (95% CI 0.96–0.99) and that for the expressional subscale (CAINS-EXP) was 0.81 (95% CI 0.67–0.89). Cronbach’s alpha was 0.71 (95% CI 0.57–0.82) for the CAINS-MAP and 0.86 (95% CI 0.79–0.92) for the CAINS-EXP. The correlation with the negative symptoms subscale of the BPRS-E was 0.35 (p = 0.011, blinded/different raters) or 0.55 (p < 0.001, not blinded/same rater). The CAINS-MAP correlated with the affective symptoms subscale of the BPRS-E (r = 0.39, p = 0.005) and the MADRS-S total score (r = 0.50, p < 0.001), but not with anxiety symptoms.
Conclusions
Negative symptoms in depression can be assessed with the CAINS with good inter-rater agreement and acceptable internal consistency and validity. There are associations between negative and depressive symptoms that call for further exploration.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Negative symptoms, including anhedonia, avolition, asociality, alogia and blunted affect, are usually considered to be part of schizophrenia [1]. There has been growing interest in the negative symptoms domain of schizophrenia in the recent decades [2]. One issue of special interest has been the conceptual overlap between negative symptoms and depressive symptoms and consensus has been reached on the importance of distinguishing between them [3]. This is relevant partly because of the need to diagnose depression in patients with schizophrenia [4], but also because this line of research can promote better characterization of the concept of negative symptoms [2, 3, 5]. This is crucial for several fields: neurobiological research on mechanistic pathways [6, 7], studying the influence of pharmacological effects on negative symptoms [8], but also because there are findings showing that clinicians tend to assign the same information different meanings when they already know a patient’s diagnosis, thus introducing a risk of bias in defining the concept [9]. Thus, if a patient has a schizophrenia diagnosis the bias may lean towards labelling certain behaviours and symptoms as negative symptoms, whereas if the patient has a depressive disorder the similar phenomenology might be interpreted and labelled as depressive symptoms.
To address these issues, some studies have investigated negative symptoms in patients with depression, or in mixed samples of depression or schizophrenia. The emerging picture is that patients with depression often exhibit some level of negative symptoms [10, 11]. When investigating mixed samples, there is indeed an overlap, but it may be possible to distinguish negative symptoms from depressive symptoms [12,13,14]. In other words, the overlap is incomplete, and expressional features have been suggested as a possible marker to distinguish between the two constructs in mixed samples [14]. In studies of individuals with a primary diagnosis of schizophrenia, it has also been suggested that it is possible to distinguish between negative symptoms and depressive symptoms, albeit still acknowledging that the phenomenology is overlapping [15]. This is corroborated by findings that expressional features such as motor retardation, blunted affect and alogia have been found to have the weakest correlations with depressive symptoms in a large sample of patients with schizophrenia [5]. A challenge to this line of research is also the diversity of the depression diagnosis [16].
Several rating scales have been developed to assess negative symptoms, though mainly in patients with schizophrenia [8]. The Clinical Assessment Interview for Negative Symptoms (CAINS) was developed to address conceptual and psychometric limitations of existing instruments [17]. The CAINS is a semi-structured interview estimating the patient’s motivation for and pleasure in social interactions and engagement in social/recreational activities and working/studying. Emotional expression is assessed through observations during the interview. As the CAINS is now one of the recommended tools for assessing negative symptoms in schizophrenia [8], there is a need for studies in patients with depression, to validate if it can be used in this population as well. This would enable further exploration of the overlap between negative symptoms and depressive symptoms, both in depression only but also in transdiagnostic samples. One earlier study using the CAINS in patients with depression and schizophrenia concluded that reduced expression can be used to distinguish between the two diagnostic constructs [14]. As the overlap between negative symptoms and depressive symptoms might complicate the delineation of negative symptoms, the possibility to use the same rating scale transdiagnostically may be of help for disentangling the constructs [18].
The aim of this study was to examine inter-rater agreement, internal consistency and validity measures of the CAINS in patients with depression. A further aim was to explore the relationship between the negative symptoms domain and the depressive and anxiety symptoms domains, as well as measures of treatment resistance, global clinical impression, functional and cognitive features. Our hypothesis was that inter-rater agreement and consistency measures would resemble earlier reports from populations of patients with schizophrenia. Regarding validity, we hypothesized that established assessments of negative symptoms would correlate to the CAINS also in our population of patients with depression. We also hypothesized that there would be correlations between negative and affective symptom domains, indicating an overlap between these.
Methods
Participants
The sample included 51 outpatients diagnosed with major depressive disorder or bipolar disorder, with a current depressive episode. The diagnoses were confirmed using the Mini-International Neuropsychiatric Interview [19]. All participants had participated in a transdiagnostic randomized controlled trial of repetitive transcranial magnetic stimulation for treating negative symptoms in schizophrenia and depression [20] or an add-on brain imaging study [21]. The current study included subjects from these studies who had depression. Inclusion criteria were: (1) having a diagnosis of a major depressive disorder or bipolar disorder, with an ongoing depressive episode, as defined in the 10th revision of the International Statistical Classification of Diseases and Related Health Problems, (2) age 18–59 years and (3) scoring ≤ 40 on the Motivation and Pleasure Scale-Self Report (MAP-SR) [22]. The last criterion was due to the design of the aforementioned trial, where a certain level of negative symptom burden was required (see also the "Discussion" section). Exclusion criteria were (1) a severe medical condition, (2) epilepsy, (3) metal or cochlear implant in the head, (4) changes in medication during the preceding month, (5) current substance use disorder (illicit drugs or alcohol), (6) regular treatment with benzodiazepines, (7) pregnancy and (8) insufficient proficiency in Swedish. Patients were recruited from the affective disorder clinic at Uppsala University Hospital in 2016–2020.
Assessments
The CAINS is a semi-structured interview consisting of 13 items divided into two parts: the CAINS motivation and pleasure subscale (CAINS-MAP) and the CAINS expression subscale (CAINS-EXP). The CAINS-MAP comprises nine items assessing the patient’s motivation and pleasure in social interactions and engagement in social and recreational activities/working/studying. In the CAINS-EXP, the interviewer assesses the patient’s facial and vocal expressions, expressive gestures and quantity of speech in four items. All items are scored 0–4, where 0 is described as ‘No impairment’ and 4 as ‘Severe deficit’.
The Brief Psychiatric Rating Scale—Expanded (BPRS-E) is one of several rating scales widely used for assessing negative symptoms [8]. It is a clinician-rated global rating scale where all 24 items are scored 1–7, with 1 being ‘Not present’ and 7 is ‘Extremely severe’. The items yield a relatively comprehensive description of major psychiatric symptom characteristics. In earlier studies, several subscales of the BPRS have been used [23]. In this study, we opted for the negative symptoms subscale consisting of the sum of the items Blunted affect, Emotional Withdrawal and Motor retardation. The positive symptoms subscale used in this study consisted of the sum of the items Suspiciousness, Hallucinations and Unusual Thought Content. For the affective symptoms subscale, we used the sum of the items Depression, Suicidality and Guilt [23]. We also analysed anxiety symptoms using the sum of the two items Anxiety and Tension.
The Clinical Global Impression (CGI) is a clinician-rated Likert-type scale 1–7, with 1 being ‘normal or not at all ill’ and 7 being ‘severe’ [24, 25].
The self-assessment instrument Montgomery-Asberg Depression Rating Scale (MADRS-S) comprises nine items that are scored from 0 (no symptoms) to 6 (very severe) [26]. The MADRS-S has been validated in Swedish patients with depression in comparison with the Beck Depression Inventory [26]. In addition to using the total sum of MADRS-S, we analysed the sum of the items Lassitude and Inability to feel, calling this entity ‘MADRS-S anhedonia’. There is no established consensus on a validated factor structure for assessing anhedonia using the MADRS-S, but there are several earlier approaches, and they all include at least one of these items [27,28,29,30]. Since we also used the total MADRS-S score, we opted for the aforementioned combination of items, in order to avoid redundancy. We also examined anxiety symptoms with the item Inner tension.
The Maudsley Staging Method (MSM) is a tool used to stage severity of treatment resistance in depression [31]. The MSM assesses duration (scored 1 to 3) and severity (scored 1 to 5) of the current depressive episode. The MSM also assesses number of antidepressant treatment failures (categorized and scored 0 to 5), augmentation (scored 0 or 1), and electroconvulsive therapy (scored 0 or 1) in the current episode. It was included because highly treatment-resistant patients might differ in regard to both motivational and expressional features. The MSM has not been explicitly validated in Swedish patients with depression, but has shown predictive value for treatment-resistant depression [31].
The EuroQol Group Visual Analogue Scale (EQ-VAS) is a self-rated instrument where the patient rates their overall health on a visual analogue scale. The endpoints of the scale are 0 ‘The worst health you can imagine’ and 100 ‘The best health you can imagine’ [32].” The EQ-VAS has been used in Swedish populations of the general population including groups with suspected depression [33,34,35].
The Sheehan Disability Scale (SDS) [36, 37] is a self-rated instrument measuring functional impairment through a total of five items. In the SDS, the patient assesses the degree to which symptoms have affected their work/studies, social life and family interactions. The score ranges from 0 to 10, with 10 being ‘Very much’.
The Alcohol Use Disorders Identification Test (AUDIT) assesses alcohol drinking habits and consequences and was used to gather the clinical characteristics of the sample [38]. The psychometric properties of the Swedish version of the AUDIT have been investigated [39].
Cognitive functioning was assessed with two tests. In the Animal Naming Test, which assesses semantic verbal fluency, the subject is asked to name as many animals as possible during one minute [40]. In the Digit Symbol Substitution Test (DSST) [41], the subject does coding exercises and their processing speed is measured. In both these tests, a higher score indicates higher cognitive functioning.
Procedures
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. All procedures were approved by regional ethical review board at Uppsala University. All participants provided written informed consent. The raters were a psychiatrist (RB), two residents in psychiatry (JB and PR) and a clinical psychologist (MC). All were trained in administration of the CAINS under the supervision of the most senior psychiatrist (RB). For training, nine videotaped interviews of both the CAINS (some of which was provided by the original developers through https://redcap.med.upenn.edu/surveys/?s=3794388R39RYEDC7&referrer=120) and the BPRS were watched and assessed by the raters. The inter-rater agreement after training was high for both the CAINS and the BPRS, including the subscales (all intraclass correlation coefficients (ICCs) above 0.80, see Additional file 1: Table S1). In the study, the participants were interviewed with the CAINS and the BPRS, in that order, while being videotaped. These interviews were performed by either author JB or RB. A second rater watched the taped interviews in the opposite order. This rater could be any of the authors JB, PR or MC (JB only if he had not performed the live interview). The video raters were given instructions to avoid rewinding or pausing the recording, in so far as possible. In order to enable a blinded design where assessment of one scale was blinded in assessment of the other, the CAINS scores from the live interview and the BPRS scores from the video rating were used in the validity analyses. This procedure was due to the importance of not being aware of the result from the first interview (CAINS) when conducting the second (BPRS), as recommended by validation guidelines [42].
The negative subscale of the BPRS was used as the reference test to analyse construct validity. Correlations with other affective domains were computed using the BPRS affective subscale, the total score of the MADRS-S and the MADRS-S anhedonia items (Lassitude and Inability to feel). We also analysed the anxiety symptom items of the BPRS and the MADRS-S. The rater who carried out the CAINS live rating also scored the CGI. The EQ-VAS questionnaire was used to assess correlation with self-rated health. The SDS was used to calculate the correlation between the CAINS and disability. Further, the Animal Naming Test and the DSST were administered by a research nurse; these tests were used to determine cognitive function. The patients were also assessed regarding treatment resistance using the MSM.
Statistics
All data were visually inspected for normality distribution, using histograms. For variables where the distribution was somewhat skewed, the mean and median values were compared. As these values did not differ substantially, means are reported throughout. The ICC was used to estimate inter-rater agreement (two-way random effects, consistency) [43]. Cronbach’s alpha with a 95% confidence interval (CI) was used to calculate internal consistency [44]. Scatterplots were visually inspected for linearity between correlation variables. Pearson’s correlation coefficients were used in the validity analyses. Differences in correlations between ratings of the CAINS and blinded versus unblinded ratings of the BPRS negative symptoms subscale were investigated using the r.test function in the psych package for R (Revelle, W. 2020. psych: Procedures for Personality and Psychological Research. Northwestern University, Evanston, https://CRAN.r-project.org/package=psych. R package version 2.0.8). JASP (JASP Team 2022. Version 0.11.1) was used for the remaining statistical analyses.
Results
Demographic and clinical characteristics
Descriptive data are presented in Table 1. About half of the participants were female and a vast majority had unipolar depression as their primary diagnosis. More than a third had a comorbid anxiety disorder and just over a fifth had been diagnosed with attention deficit hyperactivity disorder. Serotonin-norepinephrine reuptake inhibitors were the type of medication most frequently prescribed. A quarter of the participants were treated with mood stabilizers. Mean CAINS total score was 29.2 (standard deviation (SD) 7.7) and mean BPRS total score was 46.6 (SD 6.3). Mean MADRS-S total score was 29.9 (SD 7.7).
Inter-rater agreement
Regarding the inter-rater agreement between live and video interviews, all ICCs were also high (all above 0.80). The ICC for the CAINS total score was 0.93 (95% CI 0.88–0.96). For the CAINS-MAP, the ICC was 0.98 (95% CI 0.96–0.99). The CI for expressional items was wider (CAINS-EXP ICC 0.81, 95% CI 0.67–0.89). For the BPRS, the ICC for the negative symptoms subscale was 0.81 (95% CI 0.67–0.89) and that for the affective symptoms subscale was 0.94 (95% CI 0.89–0.96). The ICC for the CGI was somewhat lower (ICC 0.71, 95% CI 0.50–0.84). See Additional file 1: Table S1 for all ICCs.
Internal consistency
Cronbach’s alpha for the CAINS was 0.75 (95% CI 0.64–0.84), that for the CAINS-MAP was 0.71 (95% CI 0.57–0.82) and that for the CAINS-EXP was 0.86 (95% CI 0.79–0.92). The item-total correlation ranged from 0.32 to 0.46. All internal consistency data are presented in Table 2.
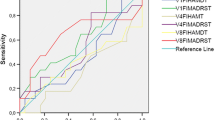
Construct validity
Construct validity measures are presented in Table 3. The CAINS total score correlated significantly with both the blinded and the non-blinded BPRS negative symptoms subscale, but more strongly with the latter; there was a significant difference between correlations (z = 4.82, p < 0.001). A similar result was seen for the CAINS-EXP, with a significant difference between correlations (z = 9.08, p < 0.001), where the strongest correlation was with the non-blinded BPRS negative symptoms subscale. There was no significant correlation between the CAINS-MAP and the BPRS negative symptoms subscale and no significant difference between correlations (z = 1.23, p = 0.22).
Correlations with affective domains and related measures
Correlations with affective domains are presented in Table 4. Only small and non-significant differences between the blinded versus non-blinded values of the BPRS and the CAINS were seen (data not shown), for which reason only the non-blinded values are presented. There were medium to strong correlations between the CAINS-MAP and the BPRS affective symptoms subscale, the MADRS-S total score and the MADRS-S anhedonia score, respectively. No significant correlations were found between the BPRS affective symptoms subscale and the CAINS total score or the CAINS-EXP. Both the MADRS-S total score and the MADRS-S anhedonia score correlated weakly to moderately with the CAINS total score. The MADRS-S total score did not correlate significantly with the CAINS-EXP. No significant correlations were found between either of the CAINS subscales and the MADRS-S anxiety symptoms or the BPRS anxiety symptoms. The MSM correlated significantly with the CAINS-EXP, but not with the CAINS-MAP. Both CAINS subscales correlated significantly, to a moderate or high degree, with the CGI. The EQ-VAS scores correlated significantly with the CAINS-MAP, but not with the CAINS-EXP. No significant correlations were found between the CAINS score and the SDS score. There was a weak but significant correlation between verbal fluency and the CAINS-EXP. This seemed to originate from correlations between verbal fluency and item 12 Expressive gestures (r = -– 0.35, p = 0.013) and item 13 Quantity of Speech (r = -– 0.31, p = 0.029). There were no correlations with the DSST.
Discussion
In this study of negative symptoms in patients with depressive disorder, we examined the reliability and validity of the CAINS. We also explored the relationships between negative symptoms and affective symptoms. Our main result indicated that the inter-rater agreement was acceptable, which is in accordance with previous studies in schizophrenia [17]. We found the Cronbach’s alpha of the CAINS to be 0.75. This has previously been regarded as an acceptable level of internal consistency [17], though a higher level would be preferable if firm conclusions are to be drawn about the assessment of negative symptoms in depressive disorders. Our recently published findings from a study with the same design found the Cronbach’s alpha to be 0.84 in a group of 34 patients with schizophrenia [45]. Interestingly, the Cronbach’s alpha for the expression subscale CAINS-EXP was higher in our sample of patients with depressive disorder (0.86) than in the aforementioned study of patients with schizophrenia (0.75). The patients in the current study presented a mean CAINS total score of 29.2, compared with 22.0 in the schizophrenia study. In another study of the CAINS in a sample of 22 patients with depression, the mean value of the total score was 11.9 [14]. This difference probably reflects that our sample was recruited for a study of treatment of negative symptoms, with an inclusion criterion being exhibiting a certain level of self-assessed negative symptoms.
Validity
Regarding validity, both the CAINS total score and the CAINS-EXP correlated significantly with the BPRS Negative Symptoms Subscale, regardless of blinding. However, the non-blinded results correlated more strongly. The differences between the blinded results and the non-blinded results might reflect the difficulties in obtaining high inter-rater reliability for expressional items. In other words, the blinding might not in itself be the cause of the lower coefficients for the blinded values, but rather that the second rater watched a video as opposed to a live interview, or that the values will always differ more when using two different raters for two interviews than when using the same rater for both interviews. However, a blinded study design is still recommended [42]. The CAINS-MAP did not correlate significantly with the BPRS Negative Symptoms Subscale. These results are rather logical, as both the CAINS-EXP and the BPRS negative symptoms subscale are observational measures, while the CAINS-MAP is based on a patient’s reported experience. Notably, the BPRS negative symptoms subscale contains no measures of motivation and/or experienced pleasure. In our recent similar study of patients with schizophrenia, the correlation coefficient between the CAINS-EXP and the BPRS Negative Symptoms Subscale was 0.48 [45]. Given the correlation coefficient of 0.56 for the depressed population in our study, it can be argued that the CAINS-EXP might be well-suited for rating negative symptoms also in patients with depression.
Negative and affective symptoms domains
When analysing relationships between negative symptoms and affective symptoms, we found moderate correlations between the CAINS-MAP and the BPRS Affective Symptoms Subscale, as well as between the CAINS-MAP and the MADRS-S total score. Given the suggested overlap between depressive and negative symptoms, we do not regard this as surprising [14]. Some validation studies of the CAINS in patients with schizophrenia found only weak and non-significant correlations between the CAINS and the Calgary Depression Scale for Schizophrenia (CDSS) [17, 46, 47], whereas others found significant associations [48]. Regarding the correlation with MADRS-S, our findings in patients with schizophrenia resulted in a correlation coefficient of 0.67, i.e. even stronger than the 0.50 in the current study. Notably, it seems that it was mainly the anhedonia items of the MADRS-S that contributed to this correlation. We are not aware of any other study comparing the CAINS and the MADRS-S. The negative symptoms construct has been suggested to reflect an entity distinct from depressive symptoms [5]. However, our results support the notion that there is an overlap between negative symptoms and depressive symptoms [14]. Yet, this overlap is not total, which is supported by our findings that the CAINS-EXP is more strongly correlated to the BPRS negative symptoms subscale than to the BPRS affective symptoms subscale. Also the CAINS-EXP did not correlate to MADRS-S. These results indicate that negative and depressive symptoms are indeed different constructs, albeit being partly overlapped. To further distinguish the negative symptoms in schizophrenia from depressive symptoms, more research is needed to establish which features can differentiate between schizophrenia and depressive disorders. There have been suggestions that expressional items might constitute such a feature [14]. One study that argued for a clearly distinct negative symptom cluster used the Positive and Negative Syndrome Scale [49] and the CDSS. These scales may be more suited for distinguishing between the disorders. Even if reliance on expressional features as a basis for distinction is a feasible way forward in a clinical setting, our study does not lend support to this notion, as our sample of patients with depression exhibited scores on the CAINS-EXP comparable to those in some studies of schizophrenia [46, 48, 50]. However, in this study we studied only patients with depression, and further studies could merit from including transdiagnostic samples. There is also a need to investigate symptom levels in the general population, especially of the volitional items, in order to establish a more accurate and valid pathological construct. Some research has been conducted on this topic [51]. However, from a clinical perspective, the CAINS might constitute a valuable tool in the assessment of the depressive symptom burden. Notably, some contents of the CAINS are lacking in most established symptom rating scales for depression, for example the purely behavioural items. Focusing on such items might be helpful for patients with activation agendas, for instance.
None of the anxiety measures correlated with the CAINS. As assessments of anxiety are lacking in most validation studies of the CAINS, it is difficult to compare this result to others. None of the items in the CAINS explicitly address feelings of worry or anxiety, for which reason we do not regard the lack of an association as surprising.
Other measures
We observed a weak correlation between the MSM and the CAINS-EXP. There are many ways to define treatment-resistant depression, and our finding could be an argument for using a continuous measure rather than a dichotomous one. Though the correlation was weak, this finding also suggests that expressional factors can be linked to increased levels of treatment resistance in depression. Further, there was a moderate correlation with the CGI, indicating that expressional deficits are important for the impression of severity in the global clinical picture. These results were virtually identical to our findings in the population with schizophrenia [45]. For self-assessed health, there was a weak correlation with the CAINS-MAP only, reflecting that patients who experience decreased motivation and pleasure will rate their overall health as worse. This indicates that motivational deficits and anhedonia are connected to something that matters to patients, which should encourage further exploration. The CAINS has been associated with functioning measures in schizophrenia [17, 50, 52], although we did not replicate this finding in our study of schizophrenia [45]. In the current study of patients with depression, we did not find a correlation between functioning (as assessed with the SDS) and CAINS total score. This might have many reasons, but it is known that functional deficits are not only explained by symptom severity [53]. The weak correlation between verbal fluency and the CAINS-EXP most likely reflects mainly the Quantity of speech item. Apart from that, our results are similar to those of other studies using the CAINS in schizophrenia, i.e. the CAINS does not seem to reflect cognitive functioning only.
Limitations
Some limitations of the current study need to be addressed. The small and heterogenous sample size prevents drawing firm conclusions and our findings need to be replicated in larger samples. The sample size also precludes factor structure analyses. A sample size calculation was performed in the original treatment study from where the current sample was recruited [20]. Since our sample consisted of patients with treatment-resistant depression, the results might not be generalizable to a wider population of patients with depressive disorders. Indeed, our patients were recruited to a treatment study of negative symptoms, and one of the inclusion criteria was exhibiting a certain level of self-rated negative symptoms. Nevertheless, as the correlation between our measure of treatment resistance and CAINS total score was weak, there is room for less treatment-resistant patients to exhibit negative symptoms. The high comorbidity with anxiety disorders is a rule rather than an exception in depression [54] and does not limit generalizability to the same extent. Further, anxiety did not correlate with CAINS total score, indicating that the presence of an anxiety disorder is of limited importance here. Around one-fifth of the patients had a diagnosis of attention deficit hyperactivity disorder, which should be kept in mind when assessing generalizability. A wide range of psychopharmacological agents was used by the study participants. Antipsychotics, which were prescribed to around one-fifth of the sample, are of some relevance for negative symptoms. However, the olanzapine equivalent dose was rather low. Thus, the antidopaminergic effect probably did not contribute to negative symptoms to any greater extent. Although the training procedures resulted in an acceptable level of inter-rater agreement (all ICCs above 0.80), we acknowledge that there might still be a qualitative difference between rating a participant’s score during a live interview as opposed to a video recording, and maybe especially so for the expressional items. This might contribute to the differences noted between the live and video ratings in Table 3. Lastly, adding other scales for negative symptoms and/or anhedonia could have strengthened the study. The BPRS negative symptoms subscale might not capture the full range of negative symptoms domains, but it has nevertheless been used in many validation studies. Most notably, the domains of asociality and avolition might not be entirely covered by the BPRS negative symptoms subscale. The Positive and Negative Syndrome Scale [49] and the Scale for the Assessment of Negative Symptoms [55] are also widely used. The negative symptoms construct is ultimately defined by the rating scale used and will therefore always differ somewhat across studies. The CAINS was constructed to deal with some of the shortcomings observed in earlier scales and is supposed to have better face validity [1].
Clinical utility
Negative symptoms are burdensome for the patients, and often also implicate hardships in relation to peers and counsellors. The notion that patients with depression also exhibit negative symptoms call for attention in clinical practice. Our experience from interviewing patients with depression with the CAINS is that both patients and their relatives appreciated the slightly different questions than what they were used to be asked. The feedback given was often that the questions addressed key issues regarding their behaviour and function, which they found valuable and accurate.
Conclusions
Assessment of negative symptoms in depression can be performed with the CAINS, with good inter-rater agreement and acceptable internal consistency and validity. There are associations between negative and depressive symptoms but the overlap is not total, thus strengthening the notion of two partly different constructs. To more accurately define the negative symptoms construct, we encourage further use of the CAINS in populations with depressive disorders as well as direct comparisons between patients with depression and patients with schizophrenia.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AUDIT:
-
Alcohol Use Disorders Identification Test
- BPRS-E:
-
Brief Psychiatric Rating Scale Expanded
- CAINS:
-
Clinical Assessment Interview for Negative Symptoms
- CAINS-EXP:
-
CAINS Expression Subscale
- CAINS-MAP:
-
CAINS Motivation and Pleasure Subscale
- CGI:
-
Clinical Global Impression
- CI:
-
Confidence interval
- DSST:
-
Digit Symbol Substitution Test
- EQ-VAS:
-
EuroQol Group Visual Analogue Scale
- ICC:
-
Intraclass correlation coefficient
- MADRS-S:
-
Montgomery-Asberg Depression Rating Scale
- MAP-SR:
-
Motivation and Pleasure Scale-Self Report
- MSM:
-
Maudsley staging method
- SD:
-
Standard deviation
- SDS:
-
Sheehan Disability Scale
References
Kirkpatrick B, Fenton WS, Carpenter WT Jr, Marder SR. The NIMH-MATRICS consensus statement on negative symptoms. Schizophr Bull. 2006;32:214–9. https://doi.org/10.1093/schbul/sbj053.
Galderisi S, Mucci A, Buchanan RW, Arango C. Negative symptoms of schizophrenia: new developments and unanswered research questions. Lancet Psychiatry. 2018;5:664–77. https://doi.org/10.1016/S2215-0366(18)30050-6.
Marder SR, Galderisi S. The current conceptualization of negative symptoms in schizophrenia. World Psychiatry. 2017;16:14–24. https://doi.org/10.1002/wps.20385.
Upthegrove R, Marwaha S, Birchwood M. Depression and Schizophrenia: Cause, Consequence, or Trans-diagnostic Issue? Schizophr Bull. 2017;43:240–4. https://doi.org/10.1093/schbul/sbw097.
Demyttenaere K, Anthonis E, Acsai K, Correll CU. Depressive symptoms and panss symptom dimensions in patients with predominant negative symptom schizophrenia: a network analysis. Front Psychiatry. 2022;13: 795866. https://doi.org/10.3389/fpsyt.2022.795866.
Ahangari M, Bustamante D, Kirkpatrick R, Nguyen TH, Verrelli BC, Fanous A, et al. Relationship between polygenic risk scores and symptom dimensions of schizophrenia and schizotypy in multiplex families with schizophrenia. Br J Psychiatry. 2022. https://doi.org/10.1192/bjp.2022.179.
Kirschner M, Schmidt A, Hodzic-Santor B, Burrer A, Manoliu A, Zeighami Y, et al. Orbitofrontal-striatal structural alterations linked to negative symptoms at different stages of the schizophrenia spectrum. Schizophr Bull. 2021;47:849–63. https://doi.org/10.1093/schbul/sbaa169.
Galderisi S, Mucci A, Dollfus S, Nordentoft M, Falkai P, Kaiser S, et al. EPA guidance on assessment of negative symptoms in schizophrenia. Eur Psychiatry. 2021;64: e23. https://doi.org/10.1192/j.eurpsy.2021.11.
Meiseberg J, Moritz S. Biases in diagnostic terminology: clinicians choose different symptom labels depending on whether the same case is framed as depression or schizophrenia. Schizophr Res. 2020;222:444–9. https://doi.org/10.1016/j.schres.2020.03.050.
Chaturvedi SK, Sarmukaddam S. Negative symptoms in depression. Indian J Psychiatry. 1985;27:139–44.
Galynker II, Cohen LJ, Cai J. Negative symptoms in patients with major depressive disorder: a preliminary report. Neuropsychiatry Neuropsychol Behav Neurol. 2000;13:171–6.
Bottlender R, Sato T, Groll C, Jager M, Kunze I, Moller HJ. Negative symptoms in depressed and schizophrenic patients: how do they differ? J Clin Psychiatry. 2003;64:954–8. https://doi.org/10.4088/jcp.v64n0816.
Chuang JY, Murray GK, Metastasio A, Segarra N, Tait R, Spencer J, et al. Brain structural signatures of negative symptoms in depression and schizophrenia. Front Psychiatry. 2014;5:116. https://doi.org/10.3389/fpsyt.2014.00116.
Richter J, Holz L, Hesse K, Wildgruber D, Klingberg S. Measurement of negative and depressive symptoms: Discriminatory relevance of affect and expression. Eur Psychiatry. 2019;55:23–8. https://doi.org/10.1016/j.eurpsy.2018.09.008.
Krynicki CR, Upthegrove R, Deakin JFW, Barnes TRE. The relationship between negative symptoms and depression in schizophrenia: a systematic review. Acta Psychiatr Scand. 2018;137:380–90. https://doi.org/10.1111/acps.12873.
Kim YK, Park SC. An alternative approach to future diagnostic standards for major depressive disorder. Prog Neuropsychopharmacol Biol Psychiatry. 2021;105: 110133. https://doi.org/10.1016/j.pnpbp.2020.110133.
Kring AM, Gur RE, Blanchard JJ, Horan WP, Reise SP. The Clinical Assessment Interview for Negative Symptoms (CAINS): final development and validation. Am J Psychiatry. 2013;170:165–72. https://doi.org/10.1176/appi.ajp.2012.12010109.
Haguiara B, Koga G, Diniz E, Fonseca L, Higuchi CH, Kagan S, et al. What is the best latent structure of negative symptoms in schizophrenia? A systematic review. Schizophr Bull Open. 2021;2:sgab013. https://doi.org/10.1093/schizbullopen/sgab013.
Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):22–33 (quiz 4-57).
Boden R, Bengtsson J, Thornblom E, Struckmann W, Persson J. Dorsomedial prefrontal theta burst stimulation to treat anhedonia, avolition, and blunted affect in schizophrenia or depression—a randomized controlled trial. J Affect Disord. 2021;290:308–15. https://doi.org/10.1016/j.jad.2021.04.053.
Persson J, Struckmann W, Gingnell M, Fallmar D, Boden R. Intermittent theta burst stimulation over the dorsomedial prefrontal cortex modulates resting-state connectivity in depressive patients: a sham-controlled study. Behav Brain Res. 2020;394: 112834. https://doi.org/10.1016/j.bbr.2020.112834.
Llerena K, Park SG, McCarthy JM, Couture SM, Bennett ME, Blanchard JJ. The Motivation and Pleasure Scale-Self-Report (MAP-SR): reliability and validity of a self-report measure of negative symptoms. Compr Psychiatry. 2013;54:568–74. https://doi.org/10.1016/j.comppsych.2012.12.001.
Shafer A, Dazzi F, Ventura J. Factor structure of the Brief Psychiatric Rating Scale - Expanded (BPRS-E) in a large hospitalized sample. J Psychiatr Res. 2017;93:79–86. https://doi.org/10.1016/j.jpsychires.2017.05.011.
Guy W. ECDEU assessment manual for psychopharmacology publication. Washington: Department of health, education and welfare; 1976.
Ahmad I, Sandberg M, Brus O, Ekman CJ, Hammar Å, Landén M, et al. Validity of diagnoses, treatment dates, and rating scales in the Swedish national quality register for electroconvulsive therapy. Nord J Psychiatry. 2022;76:96–103. https://doi.org/10.1080/08039488.2021.1939416.
Svanborg P, Asberg M. A comparison between the Beck Depression Inventory (BDI) and the self-rating version of the Montgomery Asberg Depression Rating Scale (MADRS). J Affect Disord. 2001;64:203–16. https://doi.org/10.1016/s0165-0327(00)00242-1.
Parker RD, Flint EP, Bosworth HB, Pieper CF, Steffens DC. A three-factor analytic model of the MADRS in geriatric depression. Int J Geriatr Psychiatry. 2003;18:73–7. https://doi.org/10.1002/gps.776.
Watanabe K, Fujimoto S, Marumoto T, Kitagawa T, Ishida K, Nakajima T, et al. Therapeutic potential of vortioxetine for anhedonia-like symptoms in depression: a post hoc analysis of data from a clinical trial conducted in Japan. Neuropsychiatr Dis Treat. 2022;18:363–73. https://doi.org/10.2147/NDT.S340281.
Diaz AP, Fernandes BS, Teixeira AL, Mwangi B, Hasan KM, Wu MJ, et al. White matter microstructure associated with anhedonia among individuals with bipolar disorders and high-risk for bipolar disorders. J Affect Disord. 2022;300:91–8. https://doi.org/10.1016/j.jad.2021.12.037.
Zheng W, Gu LM, Sun CH, Zhou YL, Wang CY, Lan XF, et al. Comparative effectiveness of repeated ketamine infusions in treating anhedonia in bipolar and unipolar depression. J Affect Disord. 2022;300:109–13. https://doi.org/10.1016/j.jad.2021.12.105.
Fekadu A, Wooderson S, Donaldson C, Markopoulou K, Masterson B, Poon L, et al. A multidimensional tool to quantify treatment resistance in depression: the Maudsley staging method. J Clin Psychiatry. 2009;70:177–84. https://doi.org/10.4088/jcp.08m04309.
The EuroQol Group. A new facility for the measurement of health-related quality of life. Health Policy. 1990;16:199–208.
Teni FS, Burström K, Devlin N, Parkin D, Rolfson O. Experience-based health state valuation using the EQ VAS: a register-based study of the EQ-5D-3L among nine patient groups in Sweden. Health Qual Life Outcomes. 2023;21:34. https://doi.org/10.1186/s12955-023-02115-z.
Burström K, Johannesson M, Diderichsen F. Health-related quality of life by disease and socio-economic group in the general population in Sweden. Health Policy. 2001;55:51–69. https://doi.org/10.1016/S0168-8510(00)00111-1.
Johansson R, Carlbring P, Heedman A, Paxling B, Andersson G. Depression, anxiety and their comorbidity in the Swedish general population: point prevalence and the effect on health-related quality of life. PeerJ. 2013;1: e98. https://doi.org/10.7717/peerj.98.
Sheehan DV, Harnett-Sheehan K, Raj BA. The measurement of disability. Int Clin Psychopharmacol. 1996;11(Suppl 3):89–95.
Hörberg N, Kouros I, Ekselius L, Ramklint M. The Swedish version of the Sheehan Disability Scale: a valid and brief measure of functioning. Eur J Person Centered Healthc. 2016;4:1–7. https://doi.org/10.5750/ejpch.v4i1.1075.
Bohn MJ, Babor TF, Kranzler HR. The Alcohol Use Disorders Identification Test (AUDIT): validation of a screening instrument for use in medical settings. J Stud Alcohol. 1995;56:423–32. https://doi.org/10.15288/jsa.1995.56.423.
Källmén H, Berman AH, Jayaram-Lindström N, Hammarberg A, Elgán TH. Psychometric properties of the AUDIT, AUDIT-C, CRAFFT and ASSIST-Y among Swedish adolescents. Eur Addict Res. 2019;25:68–77. https://doi.org/10.1159/000496741.
Tombaugh TN, Kozak J, Rees L. Normative data stratified by age and education for two measures of verbal fluency: FAS and animal naming. Arch Clin Neuropsychol. 1999;14:167–77.
Dickinson D, Ramsey ME, Gold JM. Overlooking the obvious: a meta-analytic comparison of digit symbol coding tasks and other cognitive measures in schizophrenia. Arch Gen Psychiatry. 2007;64:532–42. https://doi.org/10.1001/archpsyc.64.5.532.
Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, et al. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 2011;155:529–36. https://doi.org/10.7326/0003-4819-155-8-201110180-00009.
Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15:155–63. https://doi.org/10.1016/j.jcm.2016.02.012.
Cronbach LJ, Warrington WG. Time-limit tests: estimating their reliability and degree of speeding. Psychometrika. 1951;16:167–88. https://doi.org/10.1007/BF02289113.
Bengtsson J, Boden R, Neider D, Cernvall M. A blinded validation of the Swedish version of the Clinical Assessment Interview for Negative Symptoms (CAINS). Nord J Psychiatry. 2022;76:44–51. https://doi.org/10.1080/08039488.2021.1933174.
Jung SI, Woo J, Kim YT, Kwak SG. Validation of the Korean-Version of the Clinical Assessment Interview for Negative Symptoms of Schizophrenia (CAINS). J Korean Med Sci. 2016;31:1114–20. https://doi.org/10.3346/jkms.2016.31.7.1114.
Addington D, Addington J, Schissel B. A depression rating scale for schizophrenics. Schizophr Res. 1990;3:247–51.
Valiente-Gomez A, Mezquida G, Romaguera A, Vilardebo I, Andres H, Granados B, et al. Validation of the Spanish version of the Clinical Assessment for Negative Symptoms (CAINS). Schizophr Res. 2015;166:104–9. https://doi.org/10.1016/j.schres.2015.06.006.
Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13:261–76.
Engel M, Fritzsche A, Lincoln TM. Validation of the German version of the Clinical Assessment Interview for Negative Symptoms (CAINS). Psychiatry Res. 2014. https://doi.org/10.1016/j.psychres.2014.07.070.
Emmerson LC, Ben-Zeev D, Granholm E, Tiffany M, Golshan S, Jeste DV. Prevalence and longitudinal stability of negative symptoms in healthy participants. Int J Geriatr Psychiatry. 2009;24:1438–44. https://doi.org/10.1002/gps.2284.
Chan RC, Shi C, Lui SS, Ho KK, Hung KS, Lam JW, et al. Validation of the Chinese version of the Clinical Assessment Interview for Negative Symptoms (CAINS): a preliminary report. Front Psychol. 2015;6:7. https://doi.org/10.3389/fpsyg.2015.00007.
Porcelli S, Kasper S, Zohar J, Souery D, Montgomery S, Ferentinos P, et al. Social dysfunction in mood disorders and schizophrenia: clinical modulators in four independent samples. Prog Neuropsychopharmacol Biol Psychiatry. 2020;99: 109835. https://doi.org/10.1016/j.pnpbp.2019.109835.
Malhi GS, Mann JJ. Depression. Lancet. 2018;392:2299–312. https://doi.org/10.1016/S0140-6736(18)31948-2.
Andreasen NC. The Scale for the Assessment of Negative Symptoms (SANS): conceptual and theoretical foundations. Br J Psychiatry Suppl. 1989;155:49–58.
Acknowledgements
Not applicable.
Funding
Open access funding provided by Uppsala University. RB was supported by the Swedish Research Council Grant 2016-02362. JB was supported by the Lennander Foundation. The study was also supported by unrestricted grants from the Märta and Nicke Nasvell Foundation and the Professor Bror Gadelius Foundation.
Author information
Authors and Affiliations
Contributions
JB: conceptualization, data curation, formal analysis, methodology, writing—original draft, writing—review and editing. PR: conceptualization, data curation, formal analysis, methodology, writing—original draft, writing—review and editing. MC: conceptualization, data curation, formal analysis, methodology, writing—review and editing. RB: conceptualization, data curation, formal analysis, methodology, supervision, writing—review and editing, funding acquisition. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures were approved by regional ethical review board at Uppsala university. All participants provided written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.Additional file: As per journal requirements, every additional file must have a corresponding caption. In this regard, please be informed that the caption of Additional file 1 was taken from the additional e-file itself. Please advise if action taken appropriate and amend if necessary.Seems appropriate!
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Inter-rater agreement after training and between live and video ratings.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Bengtsson, J., Rad, P., Cernvall, M. et al. Psychometric properties of the Clinical Assessment Interview for Negative Symptoms (CAINS) in patients with depression and its relationship to affective symptoms. Ann Gen Psychiatry 22, 42 (2023). https://doi.org/10.1186/s12991-023-00474-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12991-023-00474-x