Abstract
Purpose
To explore the influence of circulating lymphocyte subsets, serum markers, clinical factors, and their impact on overall survival (OS) in locally advanced nasopharyngeal carcinoma (LA-NPC). Additionally, to construct a nomogram predicting OS for LA-NPC patients using independent prognostic factors.
Methods
A total of 530 patients with LA-NPC were included in this study. In the training cohort, Cox regression analysis was utilized to identify independent prognostic factors, which were then integrated into the nomogram. The concordance index (C-index) was calculated for both training and validation cohorts. Schoenfeld residual analysis, calibration curves, and decision curve analysis (DCA) were employed to evaluate the nomogram. Kaplan-Meier methods was performed based on risk stratification using the nomogram.
Results
A total of 530 LA-NPC patients were included. Multivariate Cox regression analysis revealed that the circulating CD8+T cell, platelet-to-lymphocyte ratio (PLR), lactate dehydrogenase (LDH), albumin (ALB), gender, and clinical stage were independent prognostic factors for LA-NPC (p < 0.05). Schoenfeld residual analysis indicated overall satisfaction of the proportional hazards assumption for the Cox regression model. The C-index of the nomogram was 0.724 (95% CI: 0.669–0.779) for the training cohort and 0.718 (95% CI: 0.636-0.800) for the validation cohort. Calibration curves demonstrated good correlation between the model and actual survival outcomes. DCA confirmed the clinical utility enhancement of the nomogram over the TNM staging system. Significant differences were observed in OS among different risk stratifications.
Conclusion
Circulating CD8+ T cell, PLR, LDH, ALB, gender and clinical stage are independent prognostic factors for LA-NPC. The nomogram and risk stratification constructed in this study effectively predict OS in LA-NPC.
Similar content being viewed by others
Introduction
Nasopharyngeal carcinoma (NPC) is a common malignant tumor of the nasopharynx, particularly prevalent in East Asia and Southeast Asia, with the highest incidence rates in Southern China [1, 2]. Due to its unique biological and anatomical characteristics, early symptoms and signs of NPC are often subtle, leading many patients to be diagnosed at an advanced stage when they are first diagnosed. Locally advanced NPC (LA-NPC) is defined at stage III or IVa. Platinum-based concurrent chemoradiotherapy (CCRT) combined with induction chemotherapy (IC) or adjuvant chemotherapy (AC) has become the standard treatment modality for LA-NPC [3,4,5]. With the advent of intensity-modulated radiotherapy (IMRT), the survival rates of LA-NPC patients have significantly improved. However, recurrence, metastasis, or mortality still occur in some patients [6]. Currently, clinicians primarily rely on the TNM staging system to guide treatment decisions for NPC patients. However, the TNM system primarily reflects the anatomical characteristics of the tumor at a macroscopic level and may not finely distinguish high-risk prognostic groups within LA-NPC patients. Predictive models developed prior to treatment hold promise in identifying patients with poor prognoses, thereby guiding clinicians in making individualized treatment decisions and ultimately benefiting patients.
The occurrence and progression of NPC are closely associated with tumor cell immune escape mechanisms [7]. Non-keratinizing squamous cell carcinoma (NK-NPC) accounts for over 95% of endemic NPC and is widely believed to be associated with Epstein-Barr virus (EBV) infection1. Studies have shown that EBV-induced LMP1 and IFN-γ pathways jointly regulate high expression of PD-L1 in tumor tissues of NPC patients, accompanied by strong lymphocyte infiltration [8]. This suggests that immunotherapy is a promising treatment modality for NPC. Currently, tumor immunotherapy is rapidly advancing and being applied in clinical practice, aiming to stimulate the body’s immune system to control tumors. Clinical studies such as CAPTAIN-1st [9] and JUPITER-02 [10] have demonstrated the potential benefits of immunotherapy for more NPC patients, although specific biomarkers are needed to identify potential beneficiaries. CD8+ T cells are crucial immune cells responsible for killing tumor cells [11]. Circulating immune cells can be measured in peripheral blood, making them easily accessible in clinical practice. Some studies have indicated that circulating immune cells are prognostic factors for NPC [12,13,14], yet they have been less systematically integrated into comprehensive clinical prognostic models.
Recently, serum inflammatory markers have been considered to be associated with the prognosis of various cancers [15,16,17]. Elevated levels of lactate dehydrogenase (LDH) and alkaline phosphatase (ALP) have been confirmed as tumor risk factors and widely used in prognostic prediction [9, 18,19,20]. Albumin (ALB), as a nutritional marker, may also reflect the prognosis of patients, as nutritional deficiency can lead to poor outcomes [21]. A nomogram for predicting overall survival (OS) in LA-NPC was constructed, and further risk stratification of patients was performed, aiming to provide a basis for personalized treatment of NPC.
Materials and methods
Study population
LA-NPC patients without distant metastasis, admitted to the Guangxi Medical University Cancer Hospital from 2010 to 2014, were included in this study. Inclusion criteria were as follows: (1) Pathologically confirmed diagnosis of NPC. (2) Retrospective staging according to the 8th edition of the American Joint Committee on Cancer (AJCC) staging system, classified as stage III to IVa. (3) No previous history of chemotherapy or radiotherapy; (4) patients received CCRT with or without IC and AC after diagnosis of NPC. (4) Generally good condition (karnofsky performance status score ≥ 70). (5) Complete clinical data available. Exclusion criteria were as follows: (1) Severe infection or other severe medical conditions that might affect survival. (2) Immunological disorders or recent use of medications that might affect immune function. (3) Presence of other malignant tumors. This study was retrospective in nature, and all patient data were anonymized, thereby exempting the need for informed consent.
Observational parameters and follow-up
Baseline data collected included gender, age, smoking history, TNM stage, percentages of serum circulating lymphocyte subpopulations, complete blood count, LDH, ALP, ALB, pathological classifications (the 5th edition of the WHO classification), treatment modalities, radiation doses. Inflammation biomarkers were calculated according to the following formula:
The endpoint event was OS, defined as the time from the date of diagnosis of NPC until the date of death from any cause. Follow-up was conducted via telephone calls, outpatient visits, and hospital re-examinations. Within the first 2 years after treatment, follow-up occurred every 3 months; from the 3rd to the 4th year, follow-up was conducted every 6 months, and thereafter, annually.
Treatment methods
All patients received CCRT with or without induction or adjuvant chemotherapy. Target delineation for radiotherapy target areas and organs at risk followed the guidelines of International Commission on Radiation Units and Measurements (ICRU) Reports 50 and 62 and was reviewed by at least two associate chief radiation oncologists. Prescription doses for target areas were as follows: GTVnx received 69.0–75.2 Gy (30–33 fractions), GTVnd or CTVnd received 60.0–73.92 Gy (30–33 fractions), CTV1 received 60.0–64.0 Gy (30–32 fractions), and CTV2 received 54–57.6 Gy (30–32 fractions). Chemotherapy regimens included TP (docetaxel 75 mg/m2 on day 1; cisplatin 75 mg/m2 on day 1), PF (cisplatin 80 mg/m2 on days 1–3; fluorouracil 750 mg/m2 continuous intravenous infusion over 120 h), and TPF (docetaxel 60 mg/m2 on day 1; cisplatin 60 mg/m2 on day 1; fluorouracil 600 mg/m2 continuous intravenous infusion over 120 h) administered every 3 weeks for 1–4 cycles for induction and adjuvant chemotherapy. Concurrent chemotherapy consisted of cisplatin (100 mg/m2 on days 1–3), carboplatin (300 mg/m2 on day 1), or nedaplatin (100 mg/m2 on days 1–3) every 3 weeks for 1–3 cycles.
Statistical analysis
Age was dichotomized using the median age as the cut-off value. Continuous laboratory variables were categorized into binary variables using the X-tile software (Chicago, Rim Laboratory) to determine the optimal cut-off value via enumeration method. Patients were randomly divided into training and validation cohorts at a ratio of 7:3 using simple random sampling. Baseline characteristics were compared using the chi-square test. Statistical analyses were performed using SPSS 25 for Windows (SPSS, Chicago, IL) software. In the training cohort, univariate and multivariate Cox regression analysis were used to select independent prognostic factors, with multicategorical unordered variables set as dummy variables. Variance inflation factor (VIF) was calculated to assess multicollinearity in the multivariate Cox regression model. The proportional hazards assumption in the multivariate Cox regression analysis based on independent prognostic factors was assessed using the schoenfeld residual test. The Kaplan-Meier method was used to calculate survival rates and plot survival curves, and differences in survival rates were evaluated using the Log-rank test. Median follow-up time was calculated using the reverse Kaplan-Meier method. Independent prognostic factors were incorporated into the nomogram using R 4.0.3 software. The concordance index (C-index) of the nomogram was calculated in both training and validation cohorts and compared with the TNM stage to assess model discrimination. Calibration curves were plotted to test the accuracy of the model, and decision curve analysis (DCA) was performed to evaluate whether the nomogram improved the clinical utility of the TNM stage. Total points of nomogram for each patients were calculated, then risk stratification was conducted using the X-tile software. Survival analysis was further performed for patients with different risks by the Kaplan-Meier method. P-values < 0.05 were considered statistically significant.
Results
Patient characteristics
A total of 530 LA-NPC patients were included in this study based on the inclusion and exclusion criteria. The median follow-up time for the entire cohort was 86 months (range: 3-126 months). The 3-year, 5-year, and 7-year overall survival rates (%) were 88.1%, 77.1%, and 70.6%, respectively. Patients were randomly allocated to training cohort (n = 371) and validation cohort (n = 159), with baseline characteristics presented in Table 1. There were no statistically significant differences between the two cohorts in terms of age, gender, pathological type, serum markers, treatment modalities, or overall survival rates (p > 0.05).
Prognostic factor analysis
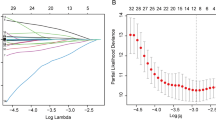
Prognostic analysis was conducted in the training cohort. Univariate Cox regression analysis indicated that gender, age, NLR, PLR, LMR, SII, SIRI, ALB, ALP, LDH, CD3+ T cells, CD8+ T cells, CD4/CD8 ratio, B cells, NK cells, and clinical stage were prognostic factors for LA-NPC patients (p < 0.05). However, smoking history, CD4+ T cells, T stage, N stage, and treatment modalities were not statistically significant in this study (p ≥ 0.05). Significant factors were included in the multivariate Cox regression model, which revealed that gender, PLR, ALB, LDH, percentage of CD8+ T cells, and clinical stage were independent prognostic factors (p < 0.05), as shown in Table 2. Collinearity analysis showed that VIF for each independent prognostic factor was < 5, indicating no significant multicollinearity. The Schoenfeld residual plot (Fig. 1) indicated that the multivariate Cox regression analysis based on independent prognostic factors satisfied the proportional hazards assumption overall (p = 0.141). There were no time-dependent trends observed for each covariate in the model, all of which met the proportional hazards assumption (p > 0.05).
Establishment and validation of the nomogram
The independent prognostic factors were incorporated into the nomogram for predicting OS (Fig. 2). Similarly, we constructed a TNM staging model, which is currently the most widely used method for making treatment decisions for NPC. The C-index of the nomogram in the training cohort and validation cohort were 0.724 (95% CI: 0.669–0.779) and 0.718 (95% CI: 0.636-0.800), respectively, which were higher than the C-index of the TNM staging model in the training cohort (0.565, 95% CI: 0.520–0.610) and validation cohort (0.601, 95% CI: 0.532–0.670). Calibration curves of the nomogram in the training and validation cohorts showed small deviations between predicted and actual results, indicating good calibration (Fig. 3A, B). DCA showed that the clinical utility of the nomogram in both the training and validation cohorts was higher than that of the TNM staging model (Fig. 3C, D).
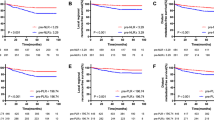
Risk Stratification and Survival Analysis Using X-tile software, patients were stratified into low-risk (score ≤ 252.4), medium-risk (252.4 < score ≤ 316.9), and high-risk (score > 316.9) groups based on the nomogram scores. Kaplan-Meier curves showed that patients in the low-risk group had the best prognosis, while those in the high-risk group had the worst prognosis, in the overall population as well as in the training and validation cohorts (Fig. 4). The Log-rank test indicated significant differences in survival among different risk groups in each cohorts (p < 0.0001). In the overall population, the 3-year, 5-year, and 7-year overall survival rates were 95.4%, 89.0%, and 82.7% in the low-risk group, 81.5%, 63.0%, and 59.0% in the medium-risk group, and 65.8%, 41.1%, and 30.6% in the high-risk group, respectively.
Discussion
Currently, NPC is entering a new era where IMRT is the mainstay treatment, leading to improved local control of NPC. However, reducing recurrence and metastasis of LA-NPC has become a significant challenge. Relying solely on TNM stage is insufficient to distinguish the heterogeneity of LA-NPC patients, as individuals receiving the same treatment may still have different prognostic outcomes. A reliable prognostic model can guide clinical decisions and potentially enhance patient outcomes. We are the first to analyse the prediction of OS in LA-NPC by combining circulating CD8+ T cell percentage and inflammatory markers, which showed superior efficacy compared to TNM stag2 alone.
The immune system plays a crucial role in immune surveillance and destruction of cancer cells [22]. CD8+ T cells are pivotal immune cells for tumor killing, however, tumors expressing highly immunogenic neoantigens may still progress despite their presence [23]. Testing for circulating lymphocyte subsets is cost-effective and convenient, yet studies on its prognostic role in NPC are limited. In this study, a high proportion of circulating CD8+ T cells was identified as an independent risk factor for OS in LA-NPC, possibly indicating CD8+ T cell dysfunction in these patients. CD8+CD28−T cells are senescent T cells with immunosuppressive functions, activated under prolonged stimulation from inflammation, infection, and tumors [24]. Previous research has shown that untreated NPC patients have significantly higher peripheral blood CD8+CD28−T cell percentages than healthy individuals, and it is an independent risk factor for NPC [25]. Another study found similar results, with the percentage of CD8+CD28−T cells being higher in untreated or recurrent NPC patients compared to healthy individuals and those in complete remission [26]. Based on the above, we conclude that in patients with LA-NPC in the context of long-standing tumor and potential EBV infection, the increase in the percentage of CD8+T cells does not necessarily reflect an enhancement of the patients’ anti-tumor immune function. Instead, it is more likely indicative of immune suppression. Our study suggests that CD8+T cells can serve as a novel prognostic factor for LA-NPC, and immunotherapy targeting the reversal of T cell dysfunction may be an effective treatment strategy.
Inflammation and immune responses are implicated in the initiation, promotion, and metastasis of tumors [27]. Numerous studies have indicated that inflammatory markers such as NLR and PLR are prognostic factors for NPC [28, 29]. In our study, PLR > 151.6 emerged as an independent risk factor for OS in LA-NPC. Consistent with our research findings, a meta-analysis incorporating data from 9 studies revealed that an elevated PLR is significantly associated with poorer OS, PFS, and DMFS in patients with NPC. Furthermore, subgroup analysis suggests that regardless of sample size, cut-off values, and treatment modalities, elevated PLR predicts worse OS [29]. The definitive reasons for the prognostic impact of PLR remain unclear, but potential mechanisms may be multifaceted. Platelets are involved in several steps of tumor hematogenous metastasis. Platelet-derived extracellular vesicles from patients with NPC transfer from platelets to NPC tumor cells, inducing cell-to-cell communication by upregulating ITGB3 expression, thus promoting NPC metastasis [30]. Lymphocytes also play crucial roles in tumor immunity. Hence, PLR may represent a balance between tumor promotion and anti-tumor immune response.
ALB is a commonly used clinical nutritional indicator. Low levels of albumin can weaken the body’s immune defense mechanisms and activate DNA replication in tumor cells [31]. Our study also observed that low ALB levels are an independent risk factor for LA-NPC. This suggests that providing appropriate nutritional support before treatment may improve prognosis. Additionally, we found that LDH > 179 U/L indicates a shorter OS. Due to the unique metabolic characteristics of tumors leading to abnormal enzyme synthesis in the body, serum enzymes may serve as prognostic markers for tumors. LDH is an enzyme in the glycolytic pathway, increased due to anaerobic release in malignant tumors [32]. Elevated LDH levels have been widely reported to indicate poor prognosis for various tumors [33,34,35]. In our study, being female was a favorable prognostic factor. Previous studies have suggested that females have a favorable OS in NPC patients [36,37,38]. Some studies also indicate that males are unfavorable for other prognostic endpoints such as distant metastasis, disease-free survival, and local control [39,40,41]. This suggests possible biological differences in tumor behavior between female and male patients, perhaps related to hormonal influences. In our study, clinical stage emerged as an independent prognostic factor, whereas individual T and N stage did not. This may be attributed to our study cohort consisting predominantly of locally advanced patients, where isolated T or N stage may not effectively discern the specificity within these staged patients. Certain indicators such as NLR, LMR, and ALP have been shown by multiple studies to be prognostic factors for nasopharyngeal carcinoma (NPC). However, in our study, they did not emerge as independent prognostic factors. This could be attributed to several reasons: (1) Differences in follow-up time. Our study had a longer follow-up duration, with a median follow-up time of 86 months. (2)The factors included in the multivariable Cox regression analysis differed among studies, and our study encompassed a broad range of factors. (3) Different studies may employ varied methods for determining cut-off values for these indicators, which could impact their prognostic significance. (4) Selection of NPC patients at different stages. We specifically focused on LA-NPC patients. The inclusion of patients at different stages of NPC across studies may affect the prognostic relevance of these indicators.
In recent years, nomograms have been widely utilized in tumor prognosis decision-making. In this study, we analyzed the impact of circulating immune cell subsets, inflammatory markers, and other serum and clinical prognostic factors on long-term survival in LA-NPC. We established a nomogram incorporating the percentages of CD8+T cells, PLR, ALB, LDH, gender, and clinical stage to further stratify prognostic risks among LA-NPC patients. The nomogram we constructed encompasses a wide range of clinical and laboratory feature types, enabling the reflection of biological differences among different patients comprehensively. The C-index of our nomogram in the training and validation cohorts was 0.724 (95% CI: 0.669–0.779) and 0.718 (95% CI: 0.636-0.800), indicating good discrimination. Nomograms constructed using radiomics are also among the current hot topics. A radiomics nomogram based on deep learning for predicting OS in LA-NPC achieved C-indexes of 0.888 and 0.899 in the training and validation cohorts, respectively, surpassing ours [42]. However, radiomics data parameters are complex, making widespread clinical application challenging. Our nomogram includes indicators that are easily detectable in clinical settings and are cost-effective to obtain, making it more convenient for clinical use. A review article suggested that evaluating a nomogram not only involves examining the C-index for model discrimination but also considering calibration curves and clinical utility assessment [43]. Combining these evaluation metrics, our nomogram demonstrates good predictive performance and clinical utility.
Schoenfeld residuals plot. The regression coefficients of each independent prognostic factors in the multivariate Cox regression model fitted by the nomogram remain stable over time, hovering near the 0 line and exhibiting basic symmetry. The multivariate Cox model and all covariates satisfy the proportional hazards assumption (p ≥ 0.05)
Validation of the nomogram. Calibration curves for the 3, 5, and 7-year OS in the training (A) and validation cohorts (B) closely align with the standard curve, indicating good model accuracy. (C) and (D) depict decision curve analysis (DCA) for the training and validation cohorts, demonstrating that the nomogram provides more net benefit compared to the TNM staging alone in both cohorts
This study has several limitations. Firstly, it is a single-center retrospective study, inevitably prone to patient selection bias. Secondly, further external data are needed to validate the practicality of our nomogram. Thirdly, although EBV-DNA is considered to have a significant impact on the prognosis of NPC, we did not include EBV-DNA as a prognostic factor because it was not a routine test item in our center in the early years. Fourthly, the CD8+T cells we measured did not further determine their functional cell subsets. These shortcomings need to be addressed in future studies.
Conclusion
In our study, we propose circulating CD8+ T cells as a novel prognostic marker for OS in LA-NPC. Additionally, we validated several biological indicators including PLR, indicating their continued reliability as independent prognostic factors in the era dominated by IMRT. The nomogram we constructed and its associated risk stratification demonstrate robust efficacy, providing clinicians with a valuable tool for pre-treatment assessment and treatment regimen determination for patients with LA-NPC.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
- PLR:
-
Platelet-to-lymphocyte ratio
- NPC:
-
Nasopharyngeal carcinoma
- OS:
-
Overall survival
- LA-NPC:
-
Locally advanced nasopharyngeal carcinoma
- C-index:
-
The concordance index
- DCA:
-
Decision curve analysis
- LDH:
-
Lactate dehydrogenase
- ALB:
-
Albumin
- CCRT:
-
Concurrent chemoradiotherapy
- IC:
-
Induction chemotherapy
- AC:
-
Adjuvant chemotherapy
- IMRT:
-
Intensity-modulated radiotherapy
- EBV:
-
Epstein-Barr virus
- ALP:
-
Alkaline phosphatase
- AJCC:
-
The American Joint Committee on Cancer
- NLR:
-
Neutrophil-to-lymphocyte ratio
- LMR:
-
Lymphocyte-to-Monocyte ratio
- SII:
-
Systemic immune-inflammation Index
- SIRI:
-
Systemic inflammatory response index
- ICRU:
-
International Commission on Radiation Units and Measurements
- VIF:
-
Variance inflation factor
References
Chen YP, Chan ATC, Le QT, et al. Nasopharyngeal carcinoma. Lancet (London England). 2019;394(10192):64–80.
Chang ET, Ye W, Zeng YX, Adami HO. The evolving epidemiology of nasopharyngeal carcinoma. Cancer Epidemiol Biomarkers Prev. 2021;30(6):1035–47.
Li WF, Chen NY, Zhang N, et al. Concurrent chemoradiotherapy with/without induction chemotherapy in locoregionally advanced nasopharyngeal carcinoma: long-term results of phase 3 randomized controlled trial. Int J Cancer. 2019;145(1):295–305.
Wee J, Tan EH, Tai BC, et al. Randomized trial of radiotherapy versus concurrent chemoradiotherapy followed by adjuvant chemotherapy in patients with American joint committee on cancer/international union against cancer stage III and IV nasopharyngeal cancer of the endemic variety. J Clin Oncology Off J Am Soc Clin Oncol. 2005;23(27):6730–8.
Yang J, Liang ZG, Jiang YT, et al. Efficacy and safety of concurrent chemoradiotherapy combined with induction chemotherapy or adjuvant chemotherapy in patients with stage II-IVA nasopharyngeal carcinoma: a propensity score matching analysis and meta-analysis. Front Oncol. 2021;11:778836.
Lee AW, Ma BB, Ng WT, Chan AT. Management of nasopharyngeal carcinoma: current practice and future perspective. J Clin Oncology Off J Am Soc Clin Oncol. 2015;33(29):3356–64.
Su WH, Hildesheim A, Chang YS. Human leukocyte antigens and epstein-barr virus-associated nasopharyngeal carcinoma: old associations offer new clues into the role of immunity in infection-associated cancers. Front Oncol. 2013;3:299.
Larbcharoensub N, Mahaprom K, Jiarpinitnun C, et al. Characterization of PD-L1 and PD-1 expression and CD8 + tumor-infiltrating lymphocyte in Epstein-Barr virus-associated nasopharyngeal carcinoma. Am J Clin Oncol. 2018;41(12):1204–10.
Yang Y, Qu S, Li J, et al. Camrelizumab versus placebo in combination with gemcitabine and cisplatin as first-line treatment for recurrent or metastatic nasopharyngeal carcinoma (CAPTAIN-1st): a multicentre, randomised, double-blind, phase 3 trial. Lancet Oncol. 2021;22(8):1162–74.
Mai HQ, Chen QY, Chen D, et al. Toripalimab or placebo plus chemotherapy as first-line treatment in advanced nasopharyngeal carcinoma: a multicenter randomized phase 3 trial. Nat Med. 2021;27(9):1536–43.
Kato T, Noma K, Ohara T, et al. Cancer-Associated fibroblasts affect Intratumoral CD8(+) and FoxP3(+) T cells Via IL6 in the tumor microenvironment. Clin cancer Res Off J Am Association Cancer Res. 2018;24(19):4820–33.
Huang C, Ding J, Huang C, et al. Abnormal variation and prognostic significance of circulating immune cells in patients with nasopharyngeal carcinoma treated with chemoradiotherapy: a prospective cohort study. Translational cancer Res. 2023;12(12):3718–27.
Zhu J, Fang R, Pan Z, Qian X. Circulating lymphocyte subsets are prognostic factors in patients with nasopharyngeal carcinoma. BMC Cancer. 2022;22(1):716.
Xu T, Huang Z, Su B, et al. Prognostic significance of circulating CD19 + B lymphocytes in EBV-associated nasopharyngeal carcinoma. Med Oncol (Northwood Lond Engl). 2014;31(10):198.
Kumarasamy C, Tiwary V, Sunil K, et al. Prognostic utility of platelet-lymphocyte ratio, neutrophil-lymphocyte ratio and monocyte-lymphocyte ratio in head and neck cancers: a detailed PRISMA compliant systematic review and meta-analysis. Cancers. 2021;13:16.
Zeng X, Liu G, Pan Y, Li Y. Development and validation of immune inflammation-based index for predicting the clinical outcome in patients with nasopharyngeal carcinoma. J Cell Mol Med. 2020;24(15):8326–49.
Gianni C, Palleschi M, Schepisi G, et al. Circulating inflammatory cells in patients with metastatic breast cancer: implications for treatment. Front Oncol. 2022;12:882896.
Zhou JY, Chen T, Li W, Ye K, Wei ZB. Effect of pretreatment serum LDH and ALP levels on the prognosis of patients with nasopharyngeal carcinoma. Lin chuang er bi yan hou tou jing wai ke za zhi = J Clin Otorhinolaryngology Head Neck Surgery. 2017;31(14):1069–1073.
Lu ZJ, Liu LT, Sun XS, et al. Establishment and validation of a prognostic nomogram to predict early metastasis in nasopharyngeal carcinoma patients within six months after radiotherapy and to guide intensive treatment. Radiotherapy Oncology: J Eur Soc Therapeutic Radiol Oncol. 2021;162:202–11.
Su K, Huang W, Li X, et al. Evaluation of Lactate Dehydrogenase and Alkaline phosphatase as predictive biomarkers in the prognosis of hepatocellular carcinoma and development of a new nomogram. J Hepatocellular Carcinoma. 2023;10:69–79.
Yang H, Wang K, Liang Z, et al. Prognostic role of pre-treatment serum albumin in patients with nasopharyngeal carcinoma: a meta-analysis and systematic review. Clin Otolaryngology Off J ENT-UK Official J Neth Soc Oto-Rhino-Laryngology Cervico-Facial Surg. 2020;45(2):167–76.
Dunn GP, Old LJ, Schreiber RD. The immunobiology of cancer immunosurveillance and immunoediting. Immunity. 2004;21(2):137–48.
Philip M, Schietinger A. CD8(+) T cell differentiation and dysfunction in cancer. Nat Rev Immunol. 2022;22(4):209–23.
Huff WX, Kwon JH, Henriquez M et al. The evolving role of CD8(+)CD28(-) immunosenescent T cells in cancer immunology. Int J Mol Sci 2019;20(11).
Xu X, Wei F, Xiao L, et al. High proportion of circulating CD8 + CD28- senescent T cells is an independent predictor of distant metastasis in nasopharyngeal canrcinoma after radiotherapy. J Translational Med. 2023;21(1):64.
Chen M, Jin F, Ma L. The detection and significance of T cells in nasopharyngeal carcinoma patients. J Cancer Res Ther. 2018;14(Supplement):S331–5.
Grivennikov SI, Greten FR, Karin M. Immunity, inflammation, and cancer. Cell. 2010;140(6):883–99.
Li Q, Yu L, Yang P, Hu Q. Prognostic value of inflammatory markers in nasopharyngeal carcinoma patients in the intensity-modulated radiotherapy era. Cancer Manage Res. 2021;13:6799–810.
Zhang J, Feng W, Ye Z, et al. Prognostic significance of platelet-to-lymphocyte ratio in patients with nasopharyngeal carcinoma: a meta-analysis. Future Oncol (London England). 2020;16(5):117–27.
Xu XR, Zhang D, Oswald BE, et al. Platelets are versatile cells: new discoveries in hemostasis, thrombosis, immune responses, tumor metastasis and beyond. Crit Rev Clin Lab Sci. 2016;53(6):409–30.
Laursen I, Briand P, Lykkesfeldt AE. Serum albumin as a modulator on growth of the human breast cancer cell line, MCF-7. Anticancer Res. 1990;10(2a):343–51.
Schwartz MK. Lactic dehydrogenase. An old enzyme reborn as a cancer marker? Am J Clin Pathol. 1991;96(4):441–3.
Zhang Y, Xu T, Wang Y, et al. Prognostic role of Lactate Dehydrogenase expression in urologic cancers: a systematic review and Meta-analysis. Oncol Res Treat. 2016;39(10):592–604.
Petrelli F, Cabiddu M, Coinu A, et al. Prognostic role of lactate dehydrogenase in solid tumors: a systematic review and meta-analysis of 76 studies. Acta Oncol (Stockholm Sweden). 2015;54(7):961–70.
Zhang M, Wei S, Su L, et al. Prognostic significance of pretreated serum lactate dehydrogenase level in nasopharyngeal carcinoma among Chinese population: a meta-analysis. Medicine. 2016;95(35):e4494.
Ng WT, Chan SH, Lee AW, et al. Parapharyngeal extension of nasopharyngeal carcinoma: still a significant factor in era of modern radiotherapy? Int J Radiat Oncol Biol Phys. 2008;72(4):1082–9.
Xiao G, Cao Y, Qiu X, et al. Influence of gender and age on the survival of patients with nasopharyngeal carcinoma. BMC Cancer. 2013;13:226.
Yeh SA, Tang Y, Lui CC, et al. Treatment outcomes and late complications of 849 patients with nasopharyngeal carcinoma treated with radiotherapy alone. Int J Radiat Oncol Biol Phys. 2005;62(3):672–9.
Lee AW, Sze WM, Au JS, et al. Treatment results for nasopharyngeal carcinoma in the modern era: the Hong Kong experience. Int J Radiat Oncol Biol Phys. 2005;61(4):1107–16.
Lai SZ, Li WF, Chen L, et al. How does intensity-modulated radiotherapy versus conventional two-dimensional radiotherapy influence the treatment results in nasopharyngeal carcinoma patients? Int J Radiat Oncol Biol Phys. 2011;80(3):661–8.
Ma J, Mai HQ, Hong MH, et al. Is the 1997 AJCC staging system for nasopharyngeal carcinoma prognostically useful for Chinese patient populations? Int J Radiat Oncol Biol Phys. 2001;50(5):1181–9.
Zhong L, Dong D, Fang X, et al. A deep learning-based radiomic nomogram for prognosis and treatment decision in advanced nasopharyngeal carcinoma: a multicentre study. EBioMedicine. 2021;70:103522.
Balachandran VP, Gonen M, Smith JJ, DeMatteo RP. Nomograms in oncology: more than meets the eye. Lancet Oncol. 2015;16(4):e173–180.
Acknowledgements
We sincerely appreciate the support and contributions of all the authors to this research and manuscript. Additionally, we would like to express our gratitude for the generous support from the funding agencies.
Funding
This study was supported by the Key Research and Development Program Project of Guangxi Zhuang Autonomous Region (GuikeAB23026020), Natural Science Foundation of Guangxi Zhuang Autonomous Region (2023GXNSFBA026012).
Author information
Authors and Affiliations
Contributions
Yan C, Yang GH and Zhu XD were the principal investigators of this study and conceived the research design. Yan C, Yang GH, Lai Lin, Sun YC, Liang ZG, Chen KH contributed to data collection. Yan C and Zhang CJ analyzed the data and prepared the figures. The manuscript was primarily drafted by Yan C. Zhu XD, Li L, Qu S critically reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study involved anonymized patient data and, due to its retrospective nature, was exempt from the requirement for informed consent. This study was approved by the Ethics Committee of Guangxi Medical University Cancer Hospital (LW2024045), in compliance with the Declaration of Helsinki.
Consent for publication
All authors have consented to the publication of this manuscript.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Yan, C., Yang, G., Zhang, C. et al. A nomogram based on circulating CD8+ T cell and platelet-to-lymphocyte ratio to predict overall survival of patients with locally advanced nasopharyngeal carcinoma. Radiat Oncol 19, 108 (2024). https://doi.org/10.1186/s13014-024-02500-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13014-024-02500-y