Abstract
Objective
The aim of this retrospective study is to review our experience in the diagnosis and role of transforaminal percutaneous endoscopic discectomy (TPED) for symptomatic gas-filled discal cysts.
Methods
Between May 2014 and June 2017, 3 patients from Lishui Center Hospital (Lishui China), who underwent TPED for symptomatic gas-filled discal cysts, were analyzed. The clinical features, imaging findings, operative findings, and treatment outcomes are presented. In addition, relevant literature regarding gas-filled discal cysts was searched using PubMed, and their characteristics, clinical features, therapeutic strategies, and survival outcomes were reviewed.
Results
The median age of the patients was 56.7 years (range, 55–60 years). In all patients, a discal cyst was located in the lumbar region, and the patients presented with backache and numbness in the lower extremities. The diagnosis was made by lumbar 3-dimensional computed tomography (3D-CT) or magnetic resonance imaging (MRI). All patients underwent TPED. All patients recovered successfully and were eventually discharged. Eighteen articles were identified from the searches of the database, and a total of 42 patients were included. There were 28 males and 14 females. The mean age was 56.8 years, ranging from 27 to 85 years. Lower back pain was the major symptom. Twenty-two patients underwent surgery, 4 patients underwent percutaneous needle aspiration, 2 patients underwent drug therapy, 13 patients received nonoperative treatment, and 1 patient was unknown.
Conclusion
TPED for gas-filled discal cysts is feasible, effective, and successful, although it should be performed by an experienced surgeon with awareness of the potential risk of severe nerve root injury.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Lumbar radiculopathy can be the result of many different and complicated pathogeneses that cause severe compression of the nerve root [1]. A rare cause of lumbar radiculopathy is discal cyst [1]. Discal cysts are intraspinal extradural cysts with a direct connection with the corresponding intervertebral disc [2]. To the best of our acknowledge, discal cysts of the lumbar spine are rare lesions. Furthermore, discal cysts that contain gas are extremely rare. Forty-three articles have been published describing approximately 105 cases of discal cysts in the available literature [3]. There are no detailed case reports concerning clinical course, imaging findings, diagnosis, and management strategies of gas-filled discal cysts. The main aims of the present study were to assess transforaminal percutaneous endoscopic discectomy (TPED) of symptomatic gas-filled discal cysts and to systematically review the previously reported cases in the literature.
Patients and methods
We retrospectively reviewed the records of 3 patients with symptomatic gas-filled discal cysts who had undergone TPED at the Department of Spinal Surgery, Lishui Center Hospital, Lishui, China, between January 2014 and January 2018. Age, sex, medical history, location of lesions, clinical presentation, diagnostic methods, intraoperative findings, postoperative complications, and outcomes were retrieved from hospital records. Relevant literature and studies regarding gas-filled discal cysts were searched in “PubMed” and “Web of Science” from January 1990 to January 2019. The text words and MESH terms “gas,” “cyst,” “disc,” and “intraspinal” were used. Disease characteristics, clinicopathologic features, therapeutic strategies, and survival outcomes were reviewed, and the data were tabulated.
Surgical strategy
The patient underwent TPED under local anesthesia, in the right lateral decubitus position. To increase the space of the interlaminar window, the hip and knee were flexed at 90° and 45°, respectively. A 7-mm incision was made on the skin. A catheter was inserted into the left intervertebral foramen at level 4/5, and a C-arm X-ray machine was positioned to obtain the proper views. After placing the dilated catheter, the working channel was established and connected with the light source of the endoscope. Normal saline flowed continuously to rinse the area. Following hemostasis, a bipolar radiofrequency knife head under the working channel was used to remove the discal cyst with the nucleus pulposus. A lumbar 5 nerve root canal expansion was performed.
Results
Report of cases
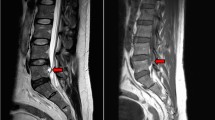
Of the three patients with gas-filled discal cysts at our hospital, two were females and one was male, with a mean age of 56.7 years (range, 55–60 years). Patient no. 2 had a history of hepatitis. The remaining two patients had no history of any disease. All three patients presented with backache and numbness of the left limb (Table 1). A physical examination found paresthesia of the L5 dermatome of the left foot. The straight leg-raising test was positive in two patients (no. 1 and no. 3). All lesions occurred at the level of L4/5. The preoperative 3-dimensional computed tomography (3D-CT) with discogram and magnetic resonance image (MRI) showed the cyst connected to the corresponding intervertebral disc in all cases (Fig. 1). Gas-filled discal cysts show low-density shadows on 3D-CT. Gas-filled discal cysts are round to oval, extradural masses with low signal intensity on T1-weighted images and T2-weighted images (Fig. 2). Other examinations, including echocardiogram, electrocardiogram, coagulation function, and routine blood examination, were normal. All patients underwent TPED. The mean operative duration was 91.6 min (range, 65–115 min), and the mean blood loss was 26.7 ml (range, 10–50 ml). The mean length of hospital stay was 7.3 days (range, 7–8 days). All patients recovered successfully and were eventually discharged. The median postoperative follow-up duration was 26 months (range, 12–36 months). An MRI scan 3 years postoperative showed a complete absence of a gas-filled discal cyst at the site of treatment in one patient (Fig. 3). Two patients were lost to follow-up.
Published case report findings
We searched the literature from January 1990 to January 2019. According to the titles and abstracts, a total of 20 articles were related. One article was not included in the analysis because there were no relevant data [4, 5]. One article, a letter to the editor, was not included in the analysis [6]. In this letter to the editor, more than 200 cases of intraspinal gas were described. However, this letter contained little or no clinical outcomes. Because of the lack of data, this letter was not included. Eighteen articles were identified from the database searches, and a total of 42 patients were included [7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23] (Table 2). There were 28 males and 14 females. The mean age was 56.8 years, ranging from 27 to 85 years. Lower back pain was the major symptom. Twenty-two patients underwent surgery, 4 patients underwent percutaneous needle aspiration, 2 patients underwent drug therapy, 13 patients received nonoperative treatment, and 1 patient was unknown. Cysts recurred in 2 patients who underwent percutaneous needle aspiration, and they later underwent surgical treatment.
Discussion
Discal cysts are extremely rare lesions, described as cysts with a direct connection with the corresponding intervertebral disc [2]. Discal cysts that contain gas are even more rare. The etiology and pathogenesis of discal cysts remain unknown, but several hypotheses have been proposed [24]. The vascular theory hypothesizes that it is an organized epidural hematoma result of hemorrhage of the epidural venous plexus resulting from disc herniation or preceding discal injury, which develops acutely and later acquires a pseudomembrane [2]. Jeong and Bendo [25] hypothesized that the formation of discal cysts was not a vascular phenomenon but resulted from a change in a herniated disc. Some scholars support the theory that a discal cyst is due to focal degeneration or annular injury of an intervertebral disc producing a corresponding herniated disc with subsequent spilling of fluid from the herniated disc tissue that triggers an abacterial inflammatory response, resulting in the formation of a pseudomembrane and development of a discal cyst [26]. Based on our intraoperative findings, we agree that the underlying etiology and pathogenesis results from an annular injury or focal degeneration, leading to a herniated disc with a subsequent series of reactions resulting in the formation of a reactive pseudomembrane that finally becomes a discal cyst.
Chief complaints, symptoms and signs of discal cysts can be similar to those of patients with typical lumbar disc herniation [1]. The early stage of discal cyst formation is asymptomatic, and no treatment is necessary because the discal cyst puts only small pressure on the canalis spinalis. However, as the discal cyst grows, patients present with different symptoms, including backache and numbness. Other diseases, which can present with similar clinical symptoms including lower back pain and radiculopathy are perineural or Tarlov cysts, epidural hematomas, ligamentum flavum cysts, arachnoid cysts, and synovial cysts [27].
Imaging examinations, including 3D-CT and MRI, are used for assessing discal cysts. Gassy discal cysts show low-density shadows on 3D-CT. The typical findings for fluid discal cysts are round to oval extradural masses with low signal intensity on T1-weighted images and high signal intensity on T2-weighted images [28]. However, this signal depends on the contents of the fluid. When the discal cysts contain gas and no fluid, masses have low signal intensity on T1-weighted images and T2-weighted images.
According to cases in the literature, partial hemilaminectomy, microscopic excision, or endoscopic excision are generally accepted as the definitive and effective treatment of choice for discal cysts. To our knowledge, the largest single-center experience describing the surgical treatment of discal cysts was described by Wang et al. [29]. This author reported the microscopic surgical outcomes of nine patients with symptomatic radiculopathy caused by discal cysts and believed that the operative indications for discal cysts are similar to those of lumbar disc herniation [29]. Although the majority of cases of discal cysts have been treated with surgical resection, computed tomography-guided aspiration has also been described [30, 31]. Endo [27] described a lumbar discal cyst that was treated with computed tomography-guided aspiration and steroid injection. This author believed that corticosteroid injection into the cyst was important for minimizing the risk of recurrence [27]. However, Kang et al. [32] performed similar aspirations without steroid injections, and no patients reported any recurrence of the cysts. Meanwhile, Cho et al. [13] described a gas-filled intradural cyst that was treated with computed tomography-guided aspiration. Unfortunately, the patient’s symptoms recurred 1 month later, and the CT showed re-accumulation of gas in the intradural cyst. The patient underwent open intradural surgery via the posterior approach. Therefore, steroid injection for discal cysts is still controversial. In addition, Demaerel et al. [33] and Takeshima et al. [34] report cases of spontaneous regression of a discal cyst without intervention. In our study, discal cysts were treated effectively by TPED. However, in order to provide more definitive evidence of standard and effective treatment for discal cysts, more studies on diagnostic and therapeutic strategies for discal cysts are needed, and careful analysis and long-term follow-up are necessary.
Conclusion
Gassy discal cysts are an extremely rare disease and may manifest with symptoms and signs very similar to lumbar disc herniation. TPED is the standard, feasible, effective, and successful treatment of gassy discal cysts, and it should be conducted by an experienced surgeon with awareness of the potential risk of nerve root injury.
Availability of data and materials
We declare that the materials described in the manuscript, including all relevant raw data, will be freely available to any scientist wishing to use them for noncommercial purposes, without breaching participant confidentiality.
Abbreviations
- TPED:
-
Transforaminal percutaneous endoscopic discectomy
- 3D-CT:
-
3-Dimensional computed tomography
- MRI:
-
Magnetic resonance imaging
References
Cho N, Keith J, Pirouzmand F. Lumbar discal cyst as a cause of radiculopathy: case report. Br J Neurosurg. 2016;30(6):675–7. https://doi.org/10.3109/02688697.2015.1100274.
Chiba K, Toyama Y, Matsumoto M, Maruiwa H, Watanabe M, Nishizawa T. Intraspinal cyst communicating with the intervertebral disc in the lumbar spine: discal cyst. Spine. 2001;26(19):2112–8. https://doi.org/10.1097/00007632-200110010-00014.
Sahoo SS. Discal cyst—a rare cause of lumbar radiculopathy in the pediatric population. Neurol India. 2016;64(1):178–80. https://doi.org/10.4103/0028-3886.173652.
Steinberg ML, Rose WS, Ruchman RB. Case report: intraspinal synovial cyst containing gas. N J Med. 1995;92(3):169–71.
Simonetti G, Martino V, Santilli S, Chiappetta F. Lumbar root compression by a gas-containing cyst in the extradural space. Case report. J Neurosurg Sci. 1992;36(2):101–2.
Hidalgo-Ovejero AM, García-Mata S, Otermin-Maya I. Gas-filled cyst. J Neurosurg Spine. 2008 Oct;9(4):400–1. https://doi.org/10.3171/SPI.2008.9.10.400.
Cebeci H, Tekin AF, Sivri M, Kıvrak AS. A rare cause of low back pain: intraspinal synovial cyst containing gas. Spine J. 2016;16(8):e495–6. https://doi.org/10.1016/j.spinee.2016.01.175.
Firth RL. Lumbar intraspinal synovial cyst containing gas as a cause for low-back pain. J Manipulative Physiol Ther. 2000;23(4):276–8. https://doi.org/10.1067/mmt.2000.106096.
Jeon CH, Park JU, Choo HS, Chung NS. Increased size of a gas-filled intradural cyst causing acute foot drop: a case report. Skeletal Radiol. 2013;42(12):1747–50. https://doi.org/10.1007/s00256-013-1668-6.
Kakitsubata Y, Theodorou SJ, Theodorou DJ, Yuko M, Ito Y, Yuki Y, et al. Symptomatic epidural gas cyst associated with discal vacuum phenomenon. Spine (Phila Pa 1976). 2009;34(21):E784–9. https://doi.org/10.1097/BRS.0b013e3181b35301.
Kang SS, Kim MS, Ko KM, Park JC, Hong SJ, Yoon YJ, et al. Symptomatic epidural gas cyst treated with epidural block and percutaneous needle aspiration -a case report. Korean J Anesthesiol. 2012;62(4):379–81. https://doi.org/10.4097/kjae.2012.62.4.379.
Ambesi Impiombato F, Lunghi V, Gambacorta D, Zocchi M. Treatment of a symptomatic epidural gas cyst using an angiographic 5F catheter in the epidural space of the spinal cord through the sacral hiatus. A Case Report. Neuroradiol J. 2011;24(6):914–8. https://doi.org/10.1177/197140091102400615.
Cho HL, Lee SH, Kim JS. Gas-filled intradural cyst within the cauda equine. J Korean Neurosurg Soc. 2011;49(3):182–5. https://doi.org/10.3340/jkns.2011.49.3.182.
Yun SM, Suh BS, Park JS. Symptomatic epidural gas-containing cyst from intervertebral vacuum phenomenon. Korean J Spine. 2012;9(4):365–8. https://doi.org/10.14245/kjs.2012.9.4.365.
Chiu LJ, Tsai PC, Chou PC, et al. A gas filled intradural cyst with intradural disc herniation: a case report. Acta Neurol Taiwan. 2008;17(1):36–41.
Kudo Y, Nishijima Y, Mochida K, Sekido Y, Tachibana S. Gas-filled intradural cyst with migration into the nerve root of the cauda equina. J Neurosurg Spine. 2008;8(5):482–6. https://doi.org/10.3171/SPI/2008/8/5/482.
Qasho R, Santoro A, Vangelista T, Cantore G. Nerve root compression by a gas-containing cyst associated with stenotic lateral recess. Case report and review of the literature. J Neurosurg Sci. 2001;45(3):181–4.
Kawaguchi S, Yamashita T, Ida K, Ikeda T, Ohwada O. Gas-filled intradural cyst of the lumbar spine. Case report. J Neurosurg. 2001;95(2 Suppl):257–9. https://doi.org/10.3171/spi.2001.95.2.0257.
Harvey AR, Britton JM, Plant GR. A gas filled intradural cyst associated with disc degeneration. Spinal Cord. 2000;38(11):708–10. https://doi.org/10.1038/sj.sc.3101071.
Fandino J, Garcia J, Garcia-Abeledo M. Radicular compression by gas in a spinal extra dural cyst. Report on two cases. Neurochirurgie. 1994;40(3):179–82.
Lin RM, Wey KL, Tzeng CC. Gas-containing “ganglion” cyst of lumbar posterior longitudinal ligament at L3. Case report. Spine (Phila Pa 1976). 1993;18(16):2528-2532, Gas-Containing “Ganglion” Cyst of Lumbar Posterior Longitudinal Ligament at L3, DOI: https://doi.org/10.1097/00007632-199312000-00026.
Hidalgo-Ovejero AM, Martinez-Grande M, Garcia-Mata S. Disc herniation with gas. Spine (Phila Pa 1976). 1994;19(19):2210–2. https://doi.org/10.1097/00007632-199410000-00016.
Tobback IG, Parizel PM, Milants W, de Moor J, de Schepper A. Gas-filled intraspinal synovial cyst. Rofo. 1992;156(3):300–1. https://doi.org/10.1055/s-2008-1032889.
Sanjeevan R, Prabu S, Azizul A, Abdul-Halim Y. Discal cyst of the lumbar spine: case report of a rare clinical entity. Malays Orthop J. 2018;12(2):56–8. https://doi.org/10.5704/MOJ.1807.011.
Jeong GK, Bendo JA. Lumbar intervertebral disc cyst as a cause of radiculopathy. Spine J. 2003;3(3):242–6. https://doi.org/10.1016/S1529-9430(02)00445-X.
Kono K, Nakamura H, Inoue Y, et al. Intraspinal extradural cysts communicating with adjacent herniated disks: imaging characteristics and possible pathogenesis. AJNR Am J Neuroradiol. 1999;20(7):1373–7.
Endo Y, Miller TT, Saboeiro GR, Cooke PM. Lumbar discal cyst: diagnostic discography followed by therapeutic computed tomography-guided aspiration and injection. J Radiol Case Rep. 2014;8(12):35–40. https://doi.org/10.3941/jrcr.v8i12.2087.
Kim SY. Radiculopathy caused by discal cyst. Korean J Pain. 2014;27(1):86–9. https://doi.org/10.3344/kjp.2014.27.1.86.
Wang ES, Lee CG, Kim SW, Kim YS, Kim DM. Clinical analysis of microscopic removal of discal cyst. Korean J Spine. 2013;10(2):61–4. https://doi.org/10.14245/kjs.2013.10.2.61.
Dasenbrock HH, Kathuria S, Witham TF, et al. Successful treatment of a symptomatic L5/S1 discal cyst by percutaneous CT-guided aspiration. Surg Neurol Int. 2010;10:1.pii:41.
Norman ER, Beall DP, Kitley CA, Ly JQ. Intervertebral disk cyst: a case report. J Comput Assist Tomogr. 2006;30(2):313–5. https://doi.org/10.1097/00004728-200603000-00029.
Kang H, Liu WC, Lee SH, Paeng SS. Midterm results of percutaneous CT-guided aspiration of symptomatic lumbar discal cysts. AJR Am J Roentgenol. 2008;190(5):W310–4. https://doi.org/10.2214/AJR.07.2195.
Demaerel P, Eerens I, Goffin J, Wilms G. Spontaneous regression of an intraspinal disc cyst. Eur Radiol. 2001;11(11):2317–8. https://doi.org/10.1007/s003300100888.
Takeshima Y, Takahashi T, Hanakita J, et al. Lumbar discal cyst with spontaneous regression and subsequent occurrence of lumbar disc herniation. Neurol Med Chir (Tokyo). 2011;51(11):809–11. https://doi.org/10.2176/nmc.51.809.
Acknowledgements
None
Funding
None
Author information
Authors and Affiliations
Contributions
ZKJ drafted the article. ZKJ and HDW performed the surgery. HDW made critical revisions for important intellectual content. All authors read and approved the final article.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was reviewed and approved by the Clinical College, Lishui Municipal Central Hospital Institutional Review Board.
Consent for publication
Written informed consent was obtained from the patients for the publication of this case report. A copy of the consent form is available for review by the editor-in-chief of this journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhu, K., He, D. Transforaminal percutaneous endoscopic discectomy for symptomatic gas-filled discal cysts—report of three cases and literature review. J Orthop Surg Res 16, 251 (2021). https://doi.org/10.1186/s13018-021-02403-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-021-02403-8