Abstract
Background and purpose
The systemic immune-inflammation index (SII), a novel inflammation index derived from the counts of circulating platelets, neutrophils and lymphocytes, has been studied in the treatment of acute cancer and ischemic stroke (AIS). However, the clinical value of the SII in postoperative delirium patients has not been further investigated. The purpose of our research was to study the incidence and preoperative risk factors for postoperative delirium (POD) and verify whether the SII could serve as a potential marker for POD in older intertrochanteric fracture patients. Finally, we created a novel nomogram for predicting POD in older patients with intertrochanteric fractures.
Methods
We enrolled elderly patients with intertrochanteric fractures who underwent proximal femoral nail antirotation (PFNA) between February 2021 and April 2023. Univariate and multivariate logistic analyses were subsequently performed to confirm the risk factors and construct a nomogram model.Calibration curve and clinical decision curve analysis (DCA) were used to assess the model’s fitting performance. The performance of the nomogram was evaluated for discrimination, calibration, and clinical utility.
Results
A total of 293 patients were eligible for inclusion in the study, 25.6% (75/293) of whom had POD. The POD patients had higher SII values than the non-POD patients. The SII was strongly correlated with POD in older intertrochanteric fracture patients, and the optimal cutoff value was 752.6 × 109. Multivariate analysis revealed that age, diabetes, total albumin, SII > 752.6 × 109 and a CRP > 20.25 mg/L were independent risk factors for POD patients. By incorporating these 5 factors, the model achieved a concordance index of 0.745 (95% CI, 0.683–0.808) and had a well-fitted calibration curve and good clinical application value.
Conclusion
The SII is a simple and valuable biomarker for POD, and the new nomogram model can be used to accurately predict the occurrence of POD. They can be utilized in clinical practice to identify those at high risk of POD in older intertrochanteric fracture patients.
Similar content being viewed by others
Introduction
Hip fracture is one of the most common and potentially devastating injuries in the elderly population. The incidence of this condition sharply increases in most areas of the world due to the aging of the population and the age-related increase in fractures [1, 2]. Specifically, femoral intertrochanteric fracture is the most common type of hip fracture. Surgical intervention, particularly proximal femoral nail antirotation (PFNA), is the preferred treatment for these fractures [3]. Previous studies have shown that intramedullary nails from various manufacturers provide comparable treatment outcomes [4]. In the context of elderly patients with intertrochanteric fractures, the primary challenge lies not in the surgical procedure itself but rather in perioperative management aimed at mitigating the risk of complications, such as pulmonary embolism, pneumonia, and delirium [1]. Delirium is characterized by disturbed attention, consciousness and other cognitive abilities. Postoperative delirium (POD) is one of the most common complications following surgery. POD has a negative effect on postoperative recovery, increases the nursing burden of caregivers, extends the length of hospital stay, increases hospitalization costs and hospitalization mortality, and may even lead to long-term cognitive impairment [5,6,7,8]. POD usually occurs within the first 72 h after surgery and lasts for several days [9]. Studies have shown that the incidence of POD is between 15.7 and 48% in elderly patients after hip fractures [5, 10, 11]. There is much evidence suggesting that POD is associated with neuroinflammatory processes [12]. Several inflammatory markers in serum or cerebrospinal fluid have been proven to be closely associated with POD [13]. The systemic immune-inflammation index (SII), a relatively novel inflammatory index that combines peripheral lymphocyte, neutrophil, and platelet counts, can be obtained without any additional financial burden. A growing body of studies has shown the potential prognostic value of POD for head and neck free-flap reconstruction, abdominal surgery, esophagectomy, carotid endarterectomy and cardiac surgery [14,15,16,17,18]. However, few studies have shown that the SII can be used to predict postoperative delirium (POD) in older hip fracture patients, particularly those with intertrochanteric fractures. It is crucial to establish a specialized model to identify high risk patients as early as possible and further reduce the incidence of POD with intertrochanteric fracture for PFNA. In our single-center retrospective cohort study, we investigated the value of the SII in predicting POD in older intertrochanteric fracture patients. Ultimately, we aimed to create a nomogram prediction model to assist clinicians in accurately identifying POD in elderly patients with intertrochanteric fractures who under PFNA.
Methods
Study population
This study was a retrospective cohort study. All the data were obtained from patients at the Third Affiliated Hospital of Wenzhou Medical University from February 2021 to April 2023.
Patients were included in the study only if they met all the following criteria: 1) aged ≥ 60 years; 2) had clinically and radiographically confirmed intertrochanteric fractures and agreed to participate in PFNA surgery; 3) American Society of Anesthesiologists’ physical status I–III; 4) had spinal anesthesia.
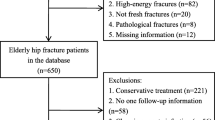
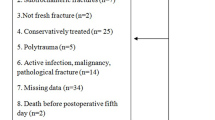
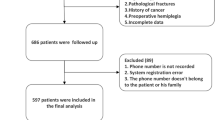
The exclusion criteria were as follows: 1) an infection at admission; 2) postoperative infections; 3) multiple injuries or multiple fractures; 4) a history of dementia or mental illness; 5) patients who had undergone other surgeries within 6 months; 6) cardiac disease (including acute myocardial infarction, congestive heart failure, a history of tachyarrhythmia/bradyarrhythmia or atrial fibrillation), pulmonary disease and impaired renal function (estimated glomerular filtration rate < 60 mL/min per 1.73 m2); 7) using antipsychotic medications; 8) alcohol or drug abuse; 9) incapable of appropriate communication; 10) preoperative delirium, stroke after surgery and in-hospital mortality. Overall, 293 patients were included in our study. Figure 1 presents the selection of patients in a flow chart.
This study was approved by the Ethics Committee of the Third Affiliated Hospital of Wenzhou Medical University (LZM2023005) and was carried out in accordance with the Declaration of Helsinki. Because this study was retrospectively designed, the ethics committee granted a waiver of the requirement for informed consent regarding the use of existing data in accordance with the national legislation and the institutional requirements. For the purpose of privacy protection in this study, personal identification information of the enrolled participants was anonymized and replaced with a coding system.
Data collection
Patient data such as age, sex, smoking status, body mass index, education degree level, hypertension, diabetes, postoperative analgesic pump use and American Society of Anesthesiologists (ASA) physical score were obtained at the preoperative visit. Surgical information, including surgical duration and blood loss was recorded.
Laboratory data, including hematocrit, neutrophil count, lymphocyte count, platelet count, total albumin and C-reactive protein (CRP) level, which were most recently measured prior to surgery and measured within 24 h after admission, were collected.SII was defined as platelet neutrophil/lymphocyte ratio.
Symptoms and signs of infection were estimated, and white blood cell count, procalcitonin (PCT) level, urine screening, chest CT, and body temperature (at least 3 times a day) were monitored within 7 days after admission.Patients with infections such as urinary tract infection, pulmonary infection, or infections in other locations were excluded.
Definitions of outcomes
The primary outcome was the incidence of POD within seven days postoperatively. It was captured through descriptive words documented in the medical records and confirmed by the neurologist. The inclusion criteria were as follows: (1) postoperative medical records containing “mental status change,” “confusion,” “disorientation,” “agitation,” “delirium,” “inappropriate behavior,” “inattention,” “hallucinations,” and “combative behavior“ [19]; and (2) postoperative drug regimens including “quetiapine,” “olanzapine,” “haloperidol,” “haloperidol,” and “risperidone.” Neurologists rechecked all the delirium patients’ medical records for diagnosing POD using the Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV) criteria [14].
Statistical analysis
Patients were classified into non-POD and POD groups. We used the mean ± standard deviation (SD) to describe continuous variables with a normal distribution and the median to describe continuous variables with a nonnormal distribution. To identify differences between non-POD and POD groups, the Pearson χ2 test was used for categorical variables. Student’s t test was used to compare normally distributed variables. Mann‒Whitney U tests were used to compare non-normally distributed variables. These variables were included in multivariate logistic regression analysis to determine whether the SII was an independent predictor of POD. Variables associated with POD in the univariate analyses with a P value < 0.05 were included in the multivariate analysis. The results are expressed as the adjusted odds ratio (aOR) with the corresponding 95% confidence interval (CI). A nomogram model was constructed based on multivariate analysis through the “R” package. Receiver operating characteristic (ROC) curve analysis, calibration curve analysis, and clinical decision curve analysis (DCA) were conducted using the “proc,” “resource selection,” and “rmda” packages. A P value < 0.05 indicated that the difference was statistically significant. The data were analyzed using IBM SPSS Statistics (26.0) and R software (4.1.3).
Results
Characteristics of the study subjects
Our study enrolled 293 intertrochanteric fracture patients; the mean age was 80.34 ± 9.61 years (60–98 years), and 49.5% (145) of the patients were women. In the study population, 172 patients had a history of hypertension, 105 had a history of diabetes, and 74 patients were smokers. The mean surgery duration was 55.03 ± 17.33 min, and blood loss was 110.17 ± 19.80 ml. The baseline characteristics are displayed in Table 1.
A total of 75 (25.6%) patients experienced POD, and patients with POD were significantly older (82.24 ± 8.57 vs. 79.68 ± 9.88, P < 0.05), had a greater percentage of diabetes (46.7% vs. 32.1%, P < 0.05), had a greater SII [788.39 ± 528.49 vs. 628.86 ± 616.81, P < 0.05], had a greater CRP level (24.58 ± 11.96 vs. 21.29 ± 12.23, P < 0.05), had a lower lymphocyte count (1.27 ± 0.39 vs. 1.41 ± 0.50, P < 0.05) and had a lower total albumin (34.04 ± 4.51 vs. 35.29 ± 3.65, P < 0.05).
Evaluation of the prognostic value of the SII and CRP for POD
ROC curve analysis revealed that the SII was predictive of POD, with an AUC of 0.64 (95% CI 0.56 to 0.70), and that of CRP was 0.59 (95% CI 0.52 to 0.66) (Fig. 2). The SII cutoff value was 752.6 × 109, the sensitivity was 72.3%, and the specificity was 53.3%; however, the CRP cutoff value was 20.25 mg/L, the sensitivity was 64.00%, and the specificity was 52.5%. The proportion of patients with an SII ≥ 752.6 × 109 was significantly greater than that of patients without delirium (39 [52.0%] vs. 60 [27.5%], P < 0.001).
Multivariate analysis for risk factors
Unadjusted logistic regression analysis revealed that age, diabetes, lymphocyte count, total albumin, the SII and the CRP level were correlated with POD. The 6 variables with P values less than 0.05 were included in the multifactorial analysis, and the results are shown in Table 2.Age (OR = 1.034, 95% CI: 1.002–1.067, P = 0.035), diabetes(OR = 2.450, 95% CI: 1.330–4.511, P = 0.047), total albumin(OR = 0.903, 95% CI: 0.837–0.974, P = 0.004), an SII > 752.6 × 109 (OR = 0.311, 95% CI: 0.158–0.614, P = 0.001) and a CRP concentration > 20.25 mg/L (OR = 0.463, 95% CI: 0.256–0.837, P = 0.011) were found to be independent predictors of POD.
Development and verification of nomogram model
Using multivariate analysis, a nomogram prediction model for POD was built and is displayed in Fig. 3. The corresponding predicted risk of POD was evaluated with a total score of 5 items. A reasonable calibration was confirmed by the Hosmer‒Lemeshow goodness-of-fit test (p = 0.559), and the results are displayed in Fig. 4. The net benefit associated with the use of the nomogram model is presented as a decision curve analysis (DCA) curve in Fig. 5. The bootstrap method (n = 1000) was used for internal validation of the nomogram, and the area under the ROC curve (AUC) was 0.745 (95% CI, 0.683–0.808) as shown in Fig. 6.
Discussion
Chronic stress induced by surgery, anesthesia, or trauma often nonspecifically activates the immune system. This activation is characterized by an increase in neutrophil count and a decrease in lymphocyte count, along with a decrease in platelet count in peripheral circulation [20,21,22]. This activation may involve hypercortisolism, disruption of the blood‒brain barrier, activation of microglia, and release of cerebral cytokines, which may contribute to the pathophysiology of delirium [22, 23]. Several recent studies have shown that white-cell-derived inflammatory biomarkers, including the neutrophil-to-lymphocyte ratio (NLR) and the systemic immune-inflammation index (SII), are indeed correlated with postoperative delirium (POD). A prospective multicenter study conducted in three medical centers enrolled 182 patients with POD and revealed a correlation between the NLR and POD in elderly patients who underwent THA for hip fracture. Compared to patients without POD, those with an NLR ≥ 3.50, older age, diabetes, and a higher neutrophil count were associated with an increased risk of POD [24]. Yuxiang Song et al. observed a total of 29,608 patients who did not undergo neurosurgery or cardiac surgery, among whom the SII was an independent predictor. They found that the SII was significantly greater in patients with POD, and the SII was found to be a useful prognostic predictor of POD in patients of different ages, sexes, and ASA classifications [24].To the best of our knowledge, intertrochanteric femoral fracture is the most commonly observed fracture in the elderly population, accounting for 63% of all hip fractures [25]. However, to our knowledge, the SII has not been applied in elderly patients with intertrochanteric fractures, who have a high incidence of POD. Therefore, this retrospective study is the first to investigate the relationship between POD and the SII. In our study, 25.6% (75/293) of older intertrochanteric fracture patients developed POD, similar to previous studies [26,27,28]. The ROC curve indicated an AUC of 0.64 for the preoperative SII, with an optimal cutoff value of 752.6 × 109. This suggests that patients with an SII > 752.6 × 109 are at a greater risk of developing POD. Logistic regression analysis revealed that a high SII, advanced age, diabetes, total albumin, and CRP concentration > 20.25 mg/L were independent risk factors for POD in older patients with intertrochanteric fractures.
The results of this study indicate that age is an independent risk factor for POD, consistent with previous studies [24, 28,29,30]. Wang et al. Conducted multiple logistic regression analysis on 582 patients who underwent joint surgery and found that age was a significant risk factor for postoperative delirium. The risk was significantly greater in patients older than 70 years than in those younger than 70 years [30]. Aging leads to a decline in organ compensatory function and physical fitness, a decrease in the brain’s regulatory ability, increased susceptibility to stressors, and abnormal excitation conduction ability, all of which contribute to the development of delirium. Additionally, aging results in a decrease in brain volume, loss of synapses in nerve cells, elevated cortisol levels, reduced oxyacetylene levels, sleep disturbances, and a gradual decline in memory and attention, all of which can cause POD [31].
Diabetes mellitus has been recognized as a risk factor for postoperative delirium (POD) in previous studies. In our study, patients with diabetes mellitus had a 2.45-fold greater risk of POD than patients without diabetes mellitus. Recent research has revealed a close association between diabetes and cognitive dysfunction, including dementia and Alzheimer’s disease. This association may be driven by factors such as insulin resistance, altered glucose metabolism, vascular changes, and the metabolism of β-amyloid and tau [32,33,34].In our study, the relevant p value (P = 0.047) was unfortunately close to 0.05, which may be attributed to the small sample size.
In our study, we also found that elderly patients with intertrochanteric fractures and hypo-protein status had a relatively high incidence of POD. Quinlan GJ et al. reported that albumin functions as an antioxidant, scavenges metabolites, protects the microcirculation, and promotes drug binding and transport [31], supporting our results. Elderly patients have reduced albumin levels, which reflects their poor nutritional status. In addition, the production process leads to an increase in oxygen free radicals that cannot be efficiently cleared, resulting in damage to brain cells through the blood‒brain barrier. A decrease in albumin levels can weaken the binding ability of drugs, such as those that cause central nervous system side effects. This can increase the concentration of free drugs in the body and potentially lead to mental disorders. Therefore, it is particularly important for doctors to identify the causes of hypoproteinaemia and actively correct the state of hypoalbuminemia to prevent the occurrence of POD.
There is a growing body of evidence supporting a link between CRP levels and postoperative delirium in various settings [35,36,37,38,39]. Chantal J et al. suggested that CRP plays a role in the underlying (inflammatory-vascular) pathological pathway of postoperative delirium [39]. Sarinnapha M et al. conducted a study suggesting that preoperative CRP could serve as an important risk marker for delirium incidence and that CRP measured preoperatively could aid in predicting and monitoring the severity of POD [40]. These findings are consistent with our own research. The SII also represents the systemic immune-inflammation status. In this study, the ROC curve and logistic regression analyses demonstrated that the SII had greater sensitivity and specificity than the CRP. Specifically, the SII was 0.64, while the AUC of CRP was 0.59, proving that the SII showed good predictive power for POD.
The SII was strongly correlated with POD. Unlike in previous studies on risk factors, independent risk factor data were obtained only by combining the Chi-square test, t test and other methods as well as univariate logistic regression analysis. The independent risk factors identified in this study were more accurately analyzed by univariate and multivariate logistic regression. Additionally, we developed a nomogram model and internally validated its excellent diagnostic efficacy. Different scores were obtained for each variable, after which the total scores of the 5 items were assessed for the corresponding POD-predicted risk. The calibration plot and the Hosmer‒Lemeshow goodness-of-fit test indicated that the model’s calibration was reasonable (p = 0.559). The DCA curve in Fig. 5 illustrates that the nomogram model has excellent clinical application. The internal verification of the nomogram was performed through the bootstrap method with 1000 repetitions of sampling, and the AUC was 0. 745, indicating that the model had good prediction performance. The new nomogram score can be derived and used by clinicians to predict the occurrence of POD in older intertrochanteric fracture patients. This tool could be helpful for clinicians by enabling early evaluation of patient outcomes, thereby aiding in the selection of better treatment plans.
However, our study has several limitations as follows. First, our study is a single-center study with a relatively small sample size, which may cause selection bias and inaccuracy to some degree. Patients with POD were identified based on medical and nursing records but not assessment tools. Nurses may have missed delirium because of a lack of knowledge of POD assessment. Second, we investigated only the SII values at admission, while the dynamic variability over time should also be assessed and studied. Third, we tried to reduce the impact of confounding factors on outcomes, but confounding factors could still not be completely ruled out in the multiple logistic regression analysis. Finally, there was a shortage of sufficient external validation targeting the new predictive model. Considering the above limitations, some prospective clinical trials with sufficient samples need to be designed in the future to evaluate the diagnostic and prognostic value of the SII for POD in older intertrochanteric fracture patients.
Conclusion
The SII is a straightforward and valuable predictor of POD in older intertrochanteric fracture patients. The new nomogram model, which consisted of 5 risk factors, provided an intuitive and accurate prediction of POD. It could be used in clinical practice to identify intertrochanteric fracture patients with PFNA who are at high risk of postoperative delirium.
Data availability
No datasets were generated or analysed during the current study.
References
Maffulli N, Aicale R. Proximal femoral fractures in the Elderly: a few things to know, and some to forget [J]. Medicina-Lithuania. 2022;58(10):1314.
Quaranta M, Miranda L, Oliva F, et al. Haemoglobin and transfusions in elderly patients with hip fractures: the effect of a dedicated orthogeriatrician [J]. J Orthop Surg Res. 2021;16(1):387.
Marsillo E, Pintore A, Asparago G, et al. Cephalomedullary nailing for reverse oblique intertrochanteric fractures 31A3 (AO/OTA) [J]. Orthop Rev. 2022;14(6):38560.
Gargano G, Poeta N, Oliva F, et al. Zimmer Natural Nail and ELOS nails in pertrochanteric fractures [J]. J Orthop Surg Res. 2021;16(1):509.
Poeran J, Cozowicz C, Zubizarreta N, et al. Modifiable factors associated with postoperative delirium after hip fracture repair: an age-stratified retrospective cohort study [J]. Eur J Anaesthesiol. 2020;37(8):649–58.
Wang NY, Hirao A, Sieber F. Association between intraoperative blood pressure and postoperative delirium in elderly hip fracture patients [J]. PLoS ONE. 2015;10(4):e0123892.
Zywiel MG, Hurley RT, Perruccio AV, et al. Health economic implications of perioperative delirium in older patients after surgery for a fragility hip fracture [J]. J bone Joint surgery-american Volume. 2015;97(10):829–36.
Ha A, Krasnow RE, Mossanen M, et al. A contemporary population-based analysis of the incidence, cost, and outcomes of postoperative delirium following major urologic cancer surgeries [J]. Urologic oncology-seminars Original Investigations. 2018;36(7):341.e15-.e22.
Krenk L, Rasmussen LS. Postoperative delirium and postoperative cognitive dysfunction in the elderly - what are the differences? [J]. Minerva Anestesiol. 2011;77(7):742–9.
Jin Z, Hu J, Ma D. Postoperative delirium: perioperative assessment, risk reduction, and management [J]. Br J Anaesth. 2020;125(4):492–504.
Oh ES, Fong TG, Hshieh TT, et al. Delirium in older persons: advances in diagnosis and treatment [J]. Jama-journal Am Med Association. 2017;318(12):1161–74.
Maldonado JR. Neuropathogenesis of delirium: review of current etiologic theories and common pathways [J]. Am j Geriat Psychiat. 2013;21(12):1190–222.
Liu X, Yu Y, Zhu S. Inflammatory markers in postoperative delirium (POD) and cognitive dysfunction (POCD): a meta-analysis of observational studies [J]. PLoS ONE. 2018;13(4):e0195659.
Kinoshita H, Saito J, Takekawa D, et al. Availability of preoperative neutrophil-lymphocyte ratio to predict postoperative delirium after head and neck free-flap reconstruction: a retrospective study [J]. PLoS ONE. 2021;16(7):e0254654.
IDA M, TAKESHITA Y. KAWAGUCHI M. Reply to in reference to preoperative serum biomarkers in the prediction of postoperative delirium following abdominal surgery [J]. Volume 21. Geriatrics & Gerontology International; 2021. pp. 756–7. 8.
Oyama T, Kinoshita H, Takekawa D, et al. Higher neutrophil-to-lymphocyte ratio, mean platelet volume, and platelet distribution width are associated with postoperative delirium in patients undergoing esophagectomy: a retrospective observational study [J]. J Anesth. 2022;36(1):58–67.
Kotfis K, Ślozowska J, Safranow K, et al. The practical use of White Cell inflammatory biomarkers in prediction of postoperative delirium after Cardiac surgery [J]. Brain Sci. 2019;9(11):308.
Kayadibi H, Uyanik M, Sertoglu E. Regarding neutrophil-lymphocyte ratio as a predictor of cognitive dysfunction in carotid endarterectomy patients [J]. J Vasc Surg. 2014;60(1):270–1.
Hornor MA, Ma M, Zhou L, et al. Enhancing the American College of Surgeons NSQIP Surgical Risk Calculator to predict geriatric outcomes [J]. J Am Coll Surg. 2020;230(1):88–e1001.
Dhabhar FS, Malarkey WB, Neri E, et al. Stress-induced redistribution of immune cells–from barracks to boulevards to battlefields: a tale of three hormones–Curt Richter Award winner [J]. Psychoneuroendocrinology. 2012;37(9):1345–68.
Alam A, Hana Z, Jin Z et al. Surgery, neuroinflammation and cognitive impairment [J]. EBioMedicine, 2018; 37: 547–56.
Murray C, Sanderson DJ, Barkus C et al. Systemic inflammation induces acute working memory deficits in the primed brain: relevance for delirium [J]. Neurobiol Aging, 2012, 33(3): 603 – 16.e3.
Hughes CG, Patel MB, Pandharipande PP. Pathophysiology of acute brain dysfunction: what’s the cause of all this confusion? [J]. Curr Opin Crit Care. 2012;18(5):518–26.
Song Y, Luo Y, Zhang F, et al. Systemic immune-inflammation index predicts postoperative delirium in elderly patients after surgery: a retrospective cohort study [J]. BMC Geriatr. 2022;22(1):730.
Schultz KA, Westcott BA, Barber KR, et al. Elevated 1-Year mortality rate in males sustaining low-energy proximal femur fractures and subgroup analysis utilizing age-adjusted Charlson Comorbidity Index [J]. Volume 11. Geriatric Orthopaedic Surgery & Rehabilitation;2020;11:2151459319898644
Eshmawey M, Arlt S, Ledschbor-Frahnert C et al. Preoperative Depression and Plasma Cortisol Levels as Predictors of Delirium after Cardiac Surgery [J]. Dementia and geriatric cognitive disorders, 2019, 48(3–4): 207 – 14.
Sieber FE, Neufeld KJ, Gottschalk A, et al. Effect of depth of Sedation in older patients undergoing hip fracture repair on postoperative delirium: the STRIDE Randomized Clinical trial [J]. JAMA Surg. 2018;153(11):987–95.
Shin JE, Kyeong S, Lee JS, et al. A personality trait contributes to the occurrence of postoperative delirium: a prospective study [J]. BMC Psychiatry. 2016;16(1):371.
Freter S, Dunbar M, Koller K, et al. Prevalence and characteristics of pre-operative delirium in hip fracture patients [J]. Gerontology. 2016;62(4):396–400.
Wang LH, Xu DJ, Wei XJ, et al. Electrolyte disorders and aging: risk factors for delirium in patients undergoing orthopedic surgeries [J]. BMC Psychiatry. 2016;16(1):418.
Guo Y, Zhang Y, Jia P et al. Preoperative serum metabolites are Associated with Postoperative Delirium in Elderly hip-fracture patients [J]. Journals of gerontology series a-biological sciences and medical sciences, 2017, 72(12): 1689–96.
Liu K, Song Y, Yuan Y, et al. Type 2 diabetes Mellitus with tight glucose control and poor Pre-injury Stair climbing Capacity May Predict Postoperative Delirium: a secondary analysis [J]. Brain Sci. 2022;12(7):951.
Van Keulen K, Knol W, Belitser SV, et al. Glucose variability during delirium in diabetic and non-diabetic intensive care unit patients: a prospective cohort study [J]. PLoS ONE. 2018;13(11):e0205637.
Berger M, Browndyke J, Mathew JP. Intraoperative Glycemic Control to prevent delirium after cardiac surgery: steering a course between Scylla and Charybdis [J]. Anesthesiology. 2015;122(6):1186–8.
Cerejeira J, Batista P, Nogueira V, et al. The stress response to surgery and postoperative delirium: evidence of hypothalamic-pituitary-adrenal axis hyperresponsiveness and decreased suppression of the GH/IGF-1 Axis [J]. J Geriatr Psychiatr Neurol. 2013;26(3):185–94.
Lee HJ, Hwang DS, Wang SK, et al. Early assessment of delirium in elderly patients after hip surgery [J]. Psychiatry Invest. 2011;8(4):340–7.
Macdonald A, Adamis D, Treloar A, et al. Age Ageing. 2007;36(2):222–5. C-reactive protein levels predict the incidence of delirium and recovery from it [J].
Şaşkin H, Özcan KS, Yildirim S. The role of inflammatory parameters in the prediction of postoperative delirium in patients undergoing coronary artery bypass grafting [J]. Cardiovasc J Afr. 2022;33(6):296–303.
Slor CJ, Witlox J, Adamis D, et al. The trajectory of C-reactive protein serum levels in older hip fracture patients with postoperative delirium [J]. Int J Geriatr Psychiatry. 2019;34(10):1438–46.
Vasunilashorn SM, Dillon ST, Inouye SK, et al. High C-Reactive protein predicts Delirium Incidence, Duration, and feature severity after major noncardiac surgery [J]. J Am Geriatr Soc. 2017;65(8):e109–16.
Acknowledgements
We are grateful to the doctors who contributed to this paper.
Funding
None.
Author information
Authors and Affiliations
Contributions
Conception and study design—Xiaoxiao Yan and Mian Lin; data acquisition—Xiachan Chen and Jin Huang; data analysis and interpretation—Xiaoxiao Yan and Mian Lin; drafting the article—Xiaoxiao Yan and Mian Lin; and revising the article—Xiachan Chen and Jin Huang. All the authors have made substantial contributions to the study conception and study design, acquisition of data, or analysis and interpretation of data, taken part in drafting or critically revising the manuscript critically for important intellectual content, agreed to submit to the current journal, reviewed and agreed on all the versions to be published, and agreed to take responsibility and be accountable for the contents of the article.
Corresponding author
Ethics declarations
Ethics approval
This study was approved by the Ethics Committee of the Third Affiliated Hospital of Wenzhou Medical University (LZM2023005) and was carried out in accordance with the Declaration of Helsinki.
Consent to participate
Because this study was retrospectively designed, the ethics committee granted a waiver of the requirement for informed consent to use existing data in accordance with the national legislation and the institutional requirements. For the purpose of privacy protection, personal identification information of the enrolled participants was anonymized and replaced with a coding system in this study.
Consent for publication
All authors consent to publication.
Competing interests
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yan, X., Huang, J., Chen, X. et al. Association between increased systemic immune-inflammation index and postoperative delirium in older intertrochanteric fracture patients. J Orthop Surg Res 19, 219 (2024). https://doi.org/10.1186/s13018-024-04699-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-024-04699-8