Abstract
Background
Posterolateral decompression and fusion with internal fixation is a commonly used surgical approach for treating degenerative lumbar spinal stenosis (DLSS). This study aims to evaluate the impact of preserving a portion of the unilateral facet joint during decompression on surgical outcomes and long-term recovery in patients.
Methods
This study analyzed 73 patients with DLSS accompanied by bilateral lower limb neurological symptoms who underwent single-level L4/5 posterolateral decompression and fusion surgery from January 2022 to March 2023. Patients were categorized into two groups based on the type of surgery received: Group A comprised 31 patients who underwent neural decompression without facet joint preservation, while Group B consisted of 42 patients who underwent neural decompression with preservation of partial facet joints on one side. Regular follow-up evaluations were conducted, including clinical and radiological assessments immediately postoperatively, and at 3 and 12 months thereafter. Key patient information was documented through retrospective chart reviews.
Results
Most patients in both groups experienced favorable surgical outcomes. However, four cases encountered complications. Notably, during follow-up, Group B demonstrated superior 1-year postoperative interbody fusion outcomes (P < 0.05), along with a trend towards less interbody cage subsidence and slower postoperative intervertebral disc height loss. Additionally, Group B showed significantly reduced postoperative hospital stay (P < 0.05).
Conclusion
Under strict adherence to surgical indications, the posterior lateral lumbar fusion surgery, which preserves partial facet joint unilaterally during neural decompression, can offer greater benefits to patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
DLSS is characterized by degenerative changes in the central vertebral canal, neural root canal, lateral recesses, or intervertebral foramina of the lumbar spine. These changes result in abnormal morphology and volume of bony and/or fibrous structures, leading to narrowing of the lumbar spinal canal. This narrowing reduces the space available for neural and vascular tissue activity, resulting in a clinical syndrome characterized by pain in the lumbosacral region or lower extremities, with or without accompanying radicular symptoms [1, 2]. This disease is more common in middle-aged and elderly individuals over the age of 40, with a gradual onset. Patients often have a history of chronic low back pain, with pain recurring frequently. Central type spinal canal stenosis primarily manifests as pain in the lumbosacral or gluteal region, with rarely any radiating pain in the lower limbs. The most typical presentation in this type of patient is neurogenic intermittent claudication. While, symptoms of lateral recess stenosis and neural foraminal stenosis are generally similar, presenting as corresponding symptoms of nerve root irritation or compression. Radicular pain is often more severe than that seen in lumbar disc herniation, radiating from the lower back and buttocks downwards, often being continuous, exacerbated after activity, with less pronounced effects from changes in posture compared to the central type, and intermittent claudication being atypical [3, 4]. For patients with lumbar spinal stenosis presenting with radiating pain or numbness in both lower extremities, the majority exhibit more severe symptoms on one side compared to the other. This study focuses on surgical interventions and their efficacy in such patients.
Early-stage lumbar spinal stenosis patients are typically advised conservative treatment. However, for those who do not respond well to conservative measures, common surgical options at present include posterior lumbar interbody fusion (PLIF), transforaminal lumbar interbody fusion (TLIF), and spinal endoscopic surgery [5]. In recent years, with the continuous advancement of spinal endoscopic technology, the scope of surgical indications has gradually expanded. Some patients with lumbar spinal stenosis are able to choose spinal endoscopic surgery and achieve desirable outcomes [6, 7]. However, not all patients with lumbar spinal stenosis are suitable candidates for spinal endoscopic surgery, such as those with spinal instability, multi-level lesions, severe neural compression, or vertebral fractures [8]. For patients with lumbar spinal stenosis requiring spinal fusion surgery and presenting with significant bilateral lower limb pain and numbness, surgeons typically employ thorough laminectomy and complete facetectomy techniques to achieve optimal neural decompression of the intervertebral foramina and central spinal canal. However, extensive bony structure resection inevitably results in more loss of spinal stability. Although robust pedicle screw fixation systems and interbody fusion can provide effective postoperative spinal stability [9], theoretically preserving unilateral facet joint structures as much as possible is likely to benefit patients’ postoperative recovery.
The aim of this study is to investigate the impact of preserving partial facet joint on the less symptomatic side while performing central canal and bilateral neural foraminal decompression in patients with severe DLSS accompanied by significant bilateral lower limb neurological symptoms, primarily on one side. This investigation aims to assess its effect on the surgical outcome and long-term recovery efficacy.
Materials and methods
Patient population
Following institutional review board approval, we conducted a retrospective analysis of data collected from patients with DLSS who underwent lumbar fusion surgery at the Department of Spinal Surgery, Affiliated Hospital of Qingdao University, between January 2022 and March 2023. Due to the retrospective nature of the study, written informed consent was waived. The inclusion criteria for this study were as follows: (1) age > 40 years, (2) single-segment lumbar fusion surgery performed at the L4/5 level, (3) preoperative presence of bilateral lower limb neurological symptoms, with one side being more severe, (4) a minimum follow-up period of 1 year postoperatively, and (5) preoperative magnetic resonance imaging (MRI) showing Schizas Grade C or D (severe spinal stenosis, with the cross-sectional area of the spinal canal between 25% and 50% or less than 25%) [10]. The exclusion criteria for this study included: (1) revision surgery, (2) lack of complete preoperative and postoperative imaging data (preoperative X-ray, 3D CT, MRI, postoperative X-ray), (3) absence of clinical assessments at preoperative or 3 months or 1 year postoperatively, (4) presence of scoliosis, and (5) presence of spondylolisthesis. According to the aforementioned criteria, this study enrolled a total of 73 patients, all of whom underwent posterior approach lumbar decompression, interbody fusion, and instrumentation. Based on the extent of neural decompression, patients were categorized into two groups: 31 patients underwent complete removal of the spinous process, lamina, and bilateral facet joints (Group A, bilateral facetectomy group), while the remaining 42 patients underwent complete removal of the spinous process, lamina, and unilateral facet joints, with simultaneous partial resection of the contralateral facet joints (Group B, unilateral facetectomy group). The facetectomies were performed according to the TLIF. All surgeries employed a single interbody fusion cage and underwent thorough interbody bone grafting.
Demographic and perioperative data collection
This study acquired patient demographic profiles, perioperative data, and radiological records by querying our hospital’s internal medical records management system. The demographic characteristics of the patients included in this study encompassed age, gender, height, weight, body mass index (BMI), and the degree of lumbar spinal canal stenosis. Perioperative variables include preoperative symptom duration, surgical duration, estimated intraoperative blood loss, drainage volume within the first three days postoperatively, time of drainage tube removal, postoperative hospital stay duration, as well as complications occurring both intraoperatively and within one year postoperatively.
Surgical procedures
Before the surgery, all participants were fully informed about the procedural steps and provided their informed consent for the surgical interventions.
Group A: These patients all underwent complete spinous process and lamina resection, as well as bilateral resection of the inferior articular processes. The superior edge and medial edge of the superior articular processes were also removed. Additionally, we performed internal fixation with a pedicle screw and rod system, and fully grafted bone into the intervertebral space along with the insertion of a single interbody fusion cage (Fig. 1). After surgery, patients were permitted to walk once the drainage tubes were removed. They were instructed to wear lumbar braces for three months to support the surgical site during the initial healing phase.
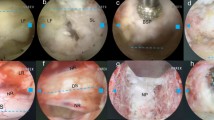
Group B: We performed complete resection of the spinous process for these patients, followed by the removal of the entire lamina, inferior articular process, and the superior edge and medial edge of the superior articular process on the side with more severe lower limb nerve symptoms. On the other side, we removed part of the lamina, inferior articular process, and the medial edge of the superior articular process, while preserving the lateral part of the lamina isthmus and part of the facet joint. Additionally, internal fixation with a pedicle screw and rod system was performed, and the intervertebral space was fully grafted with bone along with the insertion of a single interbody fusion cage (Fig. 2). Following surgery, patients were allowed to begin walking once the drainage tubes were removed. They were advised to wear lumbar braces for three months to support the surgical site during the initial healing phase.
A 72-year-old male was diagnosed with DLSS at the L4/5 level with bilateral lower limb neurological symptoms. He underwent traditional posterior lateral lumbar decompression, bone grafting, and internal fixation without facet joint preservation. A, B Preoperative X-rays showed no lumbar spondylolisthesis or scoliosis. C, D, E, F Preoperative MRI and CT showed severe DLSS at the L4/5 level, compressing the dural sac and L5 nerve root. G, H Postoperative X-rays showed posterolateral decompression and fixation surgery at L4/5 without preserving the facet joints. A single interbody cage was inserted, and extensive bone grafting was performed in the intervertebral space. I, J Postoperative X-ray at 1-year follow-up showed excellent outcomes with evidence of bony fusion in the intervertebral space, and no signs of instrumentation failure or displacement
A 67-year-old female was diagnosed with DLSS at the L4/5 level with bilateral lower limb neurological symptoms. She underwent posterior lateral lumbar decompression, bone grafting, and internal fixation, with preservation of partial facet joint on the side with milder neurological symptoms. A, B Preoperative X-rays showed no lumbar spondylolisthesis or scoliosis. C, D, E, F Preoperative MRI and CT showed severe DLSS at the L4/5 level, compressing the dural sac and L5 nerve root. G, H Postoperative X-rays revealed posterolateral decompression and fixation surgery at the L4/5 level, with partial preservation of the facet joint on one side during the procedure. A single interbody fusion cage was implanted in the intervertebral space, accompanied by extensive interbody bone grafting. I, J At 1-year postoperative follow-up, X-rays demonstrated excellent outcome with evidence of intervertebral bony fusion, and no signs of failure or displacement of the pedicle screw instrumentation
Clinical and radiological outcomes
In assessing clinical outcomes, the Oswestry disability index (ODI) was utilized to evaluate lumbar degenerative diseases. The ODI score was measured preoperatively, immediately postoperatively, at 3 months postoperatively, and at 1 year postoperatively. Additionally, patients’ lumbar visual analog scale (VAS) scores and lower limb VAS scores were assessed preoperatively, immediately postoperatively, at 3 months postoperatively, and at 1 year postoperatively.
The radiographic assessment includes an evaluation of spinal canal stenosis based on preoperative MRI, as well as assessment of intervertebral disc height, lumbar lordosis angle, and fusion status based on preoperative, immediate postoperative, 3-month follow-up, and 1-year follow-up X-ray examinations. The average intervertebral disc height is obtained by measuring the anterior and posterior disc heights separately at the fusion segment while the patient is in a standing position, and then calculating the average [11]. The segmental lordotic angle (SLA) of the lumbar spine was measured via lateral lumbar X-rays, defined as the angle formed between the lines passing through the inferior endplate of the upper vertebra and the superior endplate of the lower vertebra within the target intervertebral space [12]. Postoperative intervertebral fusion status is evaluated on X-ray images obtained at the 1-year follow-up, assessed by a board-certified spine surgeon trained in specialized procedures. “Fusion” indicates the presence of a continuous bony bridge at the surgical segment. “Doubtful fusion” refers to suboptimal fusion quality at the surgical segment, including fusion masses obscured by instrumentation. “Nonunion” signifies a definite lack of fusion at the surgical segment [13]. Additionally, the study investigates intervertebral cage subsidence. Cage subsidence is defined as a descent of the intervertebral cage into the vertebral endplates by more than 2 millimeters on lateral X-ray images taken at 1 year postoperatively compared to immediate postoperative X-ray images [5].
Consistency verification
Imaging parameters were independently measured by two spine surgeons. The results from both measurers were thoroughly examined to ensure inter-rater consistency.
Statistical analysis
All data are presented as mean ± standard deviation. Intra-class correlation coefficients (ICCs) were used to assess the consistency between measurements by different raters, with consistency results categorized into poor (0 − 0.39), fair (0.4 − 0.74), and excellent (0.75 − 1) levels. For continuous variables, intergroup comparisons between the two patient groups were first performed by assessing normality using the Shapiro-Wilk test and evaluating homogeneity of variances using Levene’s test. Upon confirmation of normal distribution and equal variances, the standard independent samples t-test was conducted to compare the two groups. For data that do not follow a normal distribution (duration of preoperative symptoms, estimated intraoperative blood loss, drainage volume in the first three postoperative days, timing of drainage tube removal, and postoperative hospital stays), the Mann-Whitney U test was used to compare differences between the two groups. Although the preoperative lumbar segmental lordosis angle data from the two groups conformed to normal distribution, they did not meet the homogeneity of variances assumption; therefore, Welch’s t-test was used for comparison. For comparing data obtained from different follow-up time points within the same group of patients, repeated measures ANOVA was used to analyze differences among multiple variables. For pairwise comparisons of data with homogeneous variances, the Bonferroni test was used; for data with non-homogeneous variances (lumbar segmental lordosis angle), the Tamhane’s T2 test was employed. For categorical variables, the chi-square test was employed. A statistical significance level was set at p < 0.05. All analyses were performed using SPSS version 23.0 (IBM Corporation, Armonk, NY, USA).
Results
Between January 2022 and March 2023, following the application of specified inclusion and exclusion criteria, our study examined 73 patients (30 males, 43 females) diagnosed with DLSS who underwent single-segment postero-lateral lumbar decompression and fusion with internal fixation surgery at the L4/5 level in the Spine Surgery Department of the Affiliated Hospital of Qingdao University. The average age of these patients was 60.22 ± 9.38 years, with ages ranging from 41 to 81 years. The patients were divided into two groups based on the surgical methods: Group A consisted of 31 patients, and Group B consisted of 42 patients. Detailed descriptions of the surgical procedures can be found in the Methods section. The baseline characteristics, including age, gender, height, weight, BMI, severity of lumbar spinal canal stenosis, duration of preoperative symptoms, surgical duration, estimated intraoperative blood loss, drainage volume in the first three postoperative days, timing of drainage tube removal, and incidence of complications, were similar between the groups, with no significant differences observed. However, in terms of postoperative hospital stay, Group B was significantly shorter than Group A, with a statistically significant difference between the two groups (P < 0.05) (Table 1).
Most patients experienced positive surgical outcomes, although four cases did encounter complications. Detailed clinical results presented in Table 2 demonstrate significant reduction in postoperative back and leg pain, as well as enhanced functional improvements throughout the follow-up period. There were no statistically significant differences between the two groups in terms of postoperative pain relief and functional scores. The study did not observe any serious neurological complications, infections, or implant fractures. The analysis of the ICC indicates excellent consistency in the radiographic measurements between the two observers. Specifically, the ICC values for intervertebral disc height were 0.890 preoperatively, 0.873 postoperatively, 0.881 at 3 months postoperatively, and 0.834 at 1 year postoperatively. For segmental lordosis angle, the ICC values were 0.935 preoperatively, 0.813 postoperatively, 0.791 at 3 months postoperatively, and 0.791 at 1 year postoperatively. Analysis of radiographic data showed no statistically significant differences between the groups in terms of intervertebral disc height before and after surgery, segmental lordosis angle before and after surgery, and postoperative subsidence of interbody fusion devices. Notably, although not statistically significant, the rate of postoperative subsidence of interbody fusion devices was notably lower in Group B compared to Group A. Meanwhile, although the differences did not reach statistical significance, the disparity in intervertebral disc height between the two groups gradually increased over time postoperatively, with Group B exhibiting greater disc height compared to Group A. Additionally, there was a statistically significant difference between the two groups in the interbody fusion status at one-year follow-up, with Group B demonstrating superior fusion status compared to Group A (P < 0.05) (Table 3).
Furthermore, the within-group comparisons of intervertebral disc height and segmental lordosis angle at various postoperative follow-up points for the two patient groups revealed significant statistical differences in both groups. Subsequent pairwise comparisons within each group were then conducted. For Group A, the pairwise comparisons of intervertebral disc height showed significant statistical differences between the following time points: preoperative vs. immediate postoperative, preoperative vs. 3 months postoperative, preoperative vs. 1 year postoperative, immediate postoperative vs. 3 months postoperative, and immediate postoperative vs. 1 year postoperative. For lumbar segmental lordosis angle in Group A, significant statistical differences were found between the following time points: preoperative vs. immediate postoperative, preoperative vs. 3 months postoperative, preoperative vs. 1 year postoperative, and immediate postoperative vs. 1 year postoperative (Table 4). For Group B, the pairwise comparisons of intervertebral disc height showed significant statistical differences between the following time points: preoperative vs. immediate postoperative, preoperative vs. 3 months postoperative, preoperative vs. 1 year postoperative, immediate postoperative vs. 3 months postoperative, and immediate postoperative vs. 1 year postoperative. For lumbar segmental lordosis angle in Group B, significant statistical differences were found between the following time points: preoperative vs. immediate postoperative, preoperative vs. 3 months postoperative, and preoperative vs. 1 year postoperative (Table 5).
Discussion
DLSS is a common spinal disorder among the elderly population, characterized by narrowing of the lumbar spinal and nerve root canals, resulting in compression of neural and vascular structures within these passageways. Currently, it is the most frequent indication for spinal surgery in elderly patients [14]. If symptoms persist or worsen despite conservative therapy, surgical intervention may be considered [15]. The goal of surgery is decompression of the central spinal canal and nerve foramina to relieve pressure on the nerve roots. The Spine Patient Outcomes Research Trial (SPORT) study has shown that symptomatic patients with lumbar spinal stenosis who undergo surgery experience significantly greater pain relief and functional improvement over a 4-year follow-up compared to those managed non-surgically [16]. The standard surgical procedure is open laminectomy, which involves a single larger incision into the spine, as employed in the SPORT study. This surgical process entails removal of bone, spurs, and ligaments compressing the nerves, and may involve one or multiple spinal segments. Fusion may be necessary based on various factors, including pre-existing spinal instability prior to surgery [16]. Some studies suggest that there may be a risk of iatrogenic spondylolisthesis or increased spondylolisthesis following decompression surgery in patients with degenerative spinal conditions. This risk arises from potential destabilization of spinal segments due to the surgical approach itself, particularly during more extensive decompression procedures where ligamentous disruption is greater or multiple segments are involved, increasing the likelihood of excessive motion. In fact, postoperative instability after laminectomy or spinal fusion is one of the most common reasons for subsequent surgery following decompression procedures [17,18,19,20]. In theory, preserving more of the posterior bony structures of the spine should enhance spinal stability postoperatively and potentially improve patient outcomes, especially for those with bilateral lower limb neurological symptoms due to DLSS. However, current research has yet to focus extensively on this aspect.
In recent years, for patients with preoperative bilateral lower limb neurological symptoms predominantly affecting one side who undergo posterior lateral lumbar fusion surgery, we have increasingly employed a surgical decompression approach that preserves part of the facet joints on the less affected side. However, systematic research and analysis comparing the advantages of this approach to traditional laminectomy with bilateral facet joint resection for decompression have not yet been conducted. Therefore, in this study, we systematically compared the surgical approach that preserves part of the facet joints with the traditional approach that does not preserve the facet joints. This comparison involved various aspects such as operative time, blood loss, length of hospital stays, postoperative symptom recovery, changes in imaging parameters, and postoperative follow-up outcomes. The results of the study showed significant differences between the two groups in terms of postoperative hospital stay and intervertebral fusion status at one-year post-surgery. Patients who had part of their facet joints preserved experienced shorter postoperative hospital stays and better intervertebral fusion status at one year. Additionally, although not statistically significant, patients with partial facet joint preservation had a lower incidence of cage subsidence at one year postoperatively. Furthermore, while both groups showed a gradual decrease in intervertebral height post-surgery, the degree of intervertebral height reduction was less in the group with partial facet joint preservation compared to the control group. Although there were no significant differences between the two groups in terms of postoperative relief of low back pain and lower limb neurological symptoms, and despite the presence of various confounding factors affecting discharge timing, the shorter postoperative hospital stay for patients with partial facet joint preservation suggests that this surgical approach has certain advantages in accelerating postoperative recovery. Notably, the pairwise comparisons of lumbar segmental lordosis angle at various follow-up time points within groups revealed that Group A had a significant difference between immediate postoperative and 1 year postoperative, whereas Group B showed no significant difference between these two time points. Therefore, the differences in imaging measurements both between and within groups indicate that preserving part of the facet joint can effectively enhance postoperative lumbar stability. This, in turn, promotes interbody bone graft fusion and potentially reduces cage subsidence, and may also slow the loss of intervertebral height post-surgery [21, 22]. In addition to the stability of internal fixation devices and the extent of bony structure preservation, several other factors influence the efficiency of lumbar interbody fusion. These factors include postoperative cross-sectional area of the lumbar erector spinae muscles, insulin levels, hormonal factors, vitamins, corticosteroids, anemia, nonsteroidal anti-inflammatory drugs, smoking, vascular factors, osteoporosis, among others [23, 24]. Failure of interbody fusion can lead to persistent low back pain or worsening symptoms, functional impairment of the lumbar spine, and an increased likelihood of reoperation [25]. Therefore, in the absence of significant differences in other factors, preserving part of the facet joint’s bony structure as much as possible plays a crucial role in improving long-term outcomes for patients undergoing lumbar fusion surgery.
Limitations
Several limitations should be noted. First, as a retrospective study, our data collection depended on extraction from electronic medical records. These data were nonrandomized and sourced from a single center, so a larger, multicenter study might produce different results. Second, the decision to discharge patients to their homes may have been influenced by personal preferences or hospital policies related to the severity of their postoperative condition. Third, certain factors, such as the extent of decompression performed, trainee involvement, and the type of implant system used, were not accounted for. These factors could impact operative time, estimated blood loss, and patient-reported outcomes, but were not controlled for in our regression analyses. Future research with larger sample sizes and longer follow-up periods is necessary to validate these results and potentially adjust treatment protocols based on long-term outcomes.
Conclusions
This study compared two different surgical approaches for treating DLSS with bilateral lower limb neurological symptoms, predominantly affecting one side: the traditional posterior lateral lumbar fusion without bilateral facet joint preservation and the posterior lateral lumbar fusion preserving part of the facet joint on the less symptomatic side. The results showed that preserving the unilateral partial facet joint not only ensures effective decompression but also has significant clinical benefits, including shorter postoperative hospital stays and improved interbody fusion efficiency. Therefore, under the strict adherence to surgical indications, this approach, which preserves a portion of the facet joint, can provide greater benefits to patients.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- DLSS:
-
Degenerative Lumbar Spinal Stenosis
- PLIF:
-
Posterior Lumbar Interbody Fusion
- TLIF:
-
Transforaminal Lumbar Interbody Fusion
- MRI:
-
Magnetic Resonance Imaging
- BMI:
-
Body Mass Index
- ODI:
-
Oswestry Disability Index
- VAS:
-
Visual Analog Scale
- SLA:
-
Segmental Lordotic Angle
- ICCs:
-
Intra-class Correlation Coefficients
- SPORT:
-
Spine Patient Outcomes Research Trial
References
Katz JN, Zimmerman ZE, Mass H, Makhni MC. Diagnosis and management of lumbar spinal stenosis: a review. JAMA. 2022;327(17):1688–99.
Covaro A, Vila-Canet G, de Frutos AG, Ubierna MT, Ciccolo F, Caceres E. Management of degenerative lumbar spinal stenosis: an evidence-based review. EFORT Open Rev. 2016;1(7):267–74.
Issack PS, Cunningham ME, Pumberger M, Hughes AP, Cammisa FP. Jr. Degenerative lumbar spinal stenosis: evaluation and management. J Am Acad Orthop Surg. 2012;20(8):527–35.
Bagley C, MacAllister M, Dosselman L, Moreno J, Aoun SG, El Ahmadieh TY. Current concepts and recent advances in understanding and managing lumbar spine stenosis. F1000Res. 2019;8.
Shimizu T, Fujibayashi S, Otsuki B, Murata K, Matsuda S. Indirect decompression via oblique lateral interbody fusion for severe degenerative lumbar spinal stenosis: a comparative study with direct decompression transforaminal/posterior lumbar interbody fusion. Spine J. 2021;21(6):963–71.
Ruetten S, Komp M. Endoscopic lumbar decompression. Neurosurg Clin N Am. 2020;31(1):25–32.
Meng H, Su N, Lin J, Fei Q. Comparative efficacy of unilateral biportal endoscopy and micro-endoscopic discectomy in the treatment of degenerative lumbar spinal stenosis: a systematic review and meta-analysis. J Orthop Surg Res. 2023;18(1):814.
Ito F, Ito Z, Shibayama M, Nakamura S, Yamada M, Yoshimatu H, et al. Step-by-step Sublaminar Approach with a newly-designed spinal endoscope for Unilateral-Approach bilateral decompression in spinal stenosis. Neurospine. 2019;16(1):41–51.
Liu H, Xu Y, Yang SD, Wang T, Wang H, Liu FY, et al. Unilateral versus bilateral pedicle screw fixation with posterior lumbar interbody fusion for lumbar degenerative diseases: a meta-analysis. Med (Baltim). 2017;96(21):e6882.
Li J, Li H, Zhang N, Wang ZW, Zhao TF, Chen LW, et al. Radiographic and clinical outcome of lateral lumbar interbody fusion for extreme lumbar spinal stenosis of Schizas grade D: a retrospective study. BMC Musculoskelet Disord. 2020;21(1):259.
Son S, Lee SG, Kim WK, Ahn Y, Jung JM. Disc height discrepancy between supine and standing positions as a screening metric for discogenic back pain in patients with disc degeneration. Spine J. 2021;21(1):71–9.
Hong TH, Cho KJ, Kim YT, Park JW, Seo BH, Kim NC. Does Lordotic Angle of cage determine lumbar lordosis in lumbar Interbody Fusion? Spine (Phila Pa 1976). 2017;42(13):E775–80.
Christensen FB, Laursen M, Gelineck J, Eiskjaer SP, Thomsen K, Bunger CE. Interobserver and intraobserver agreement of radiograph interpretation with and without pedicle screw implants: the need for a detailed classification system in posterolateral spinal fusion. Spine (Phila Pa 1976). 2001;26(5):538–43. discussion 43 – 4.
Shamji MF, Mroz T, Hsu W, Chutkan N. Management of degenerative lumbar spinal stenosis in the Elderly. Neurosurgery. 2015;77(Suppl 4):S68–74.
Karlsson T, Forsth P, Skorpil M, Pazarlis K, Ohagen P, Michaelsson K, et al. Decompression alone or decompression with fusion for lumbar spinal stenosis: a randomized clinical trial with two-year MRI follow-up. Bone Joint J. 2022;104–B(12):1343–51.
Weinstein JN, Tosteson TD, Lurie JD, Tosteson A, Blood E, Herkowitz H, et al. Surgical versus nonoperative treatment for lumbar spinal stenosis four-year results of the spine patient outcomes Research Trial. Spine (Phila Pa 1976). 2010;35(14):1329–38.
Fox MW, Onofrio BM, Onofrio BM, Hanssen AD. Clinical outcomes and radiological instability following decompressive lumbar laminectomy for degenerative spinal stenosis: a comparison of patients undergoing concomitant arthrodesis versus decompression alone. J Neurosurg. 1996;85(5):793–802.
Guha D, Heary RF, Shamji MF. Iatrogenic spondylolisthesis following laminectomy for degenerative lumbar stenosis: systematic review and current concepts. Neurosurg Focus. 2015;39(4):E9.
Lee KK, Teo EC, Qiu TX, Yang K. Effect of facetectomy on lumbar spinal stability under sagittal plane loadings. Spine (Phila Pa 1976). 2004;29(15):1624–31.
Hartmann F, Janssen C, Bohm S, Hely H, Rommens PM, Gercek E. Biomechanical effect of graded minimal-invasive decompression procedures on lumbar spinal stability. Arch Orthop Trauma Surg. 2012;132(9):1233–9.
Jun BY. Posterior lumbar interbody fusion with restoration of lamina and facet fusion. Spine (Phila Pa 1976). 2000;25(8):917–22.
Humphreys SC, Hodges SD, Patwardhan AG, Eck JC, Murphy RB, Covington LA. Comparison of posterior and transforaminal approaches to lumbar interbody fusion. Spine (Phila Pa 1976). 2001;26(5):567–71.
Choi MK, Kim SB, Park BJ, Park CK, Kim SM. Do trunk muscles affect the lumbar Interbody Fusion Rate? Correlation of Trunk Muscle Cross Sectional Area and Fusion Rates after posterior lumbar Interbody Fusion using stand-alone cage. J Korean Neurosurg Soc. 2016;59(3):276–81.
Ondra SL, Marzouk S. Revision strategies for lumbar pseudarthrosis. Neurosurg Focus. 2003;15(3):E9.
Bassani R, Morselli C, Cirullo A, Querenghi AM, Mangiavini L. Successful salvage strategy using anterior retroperitoneal approach in failed posterior lumbar interbody fusion. A retrospective analisys on lumbar lordosis and clinical outcome. Eur Spine J. 2022;31(7):1649–57.
Acknowledgements
Not applicable.
Funding
This research was funded by Natural Science Foundation of Shandong Province (grant number ZR2022QH137) and Qingdao Science and Technology Benefit the People Demonstration Project (No. 23-2-8-smjk-7-nsh).
Author information
Authors and Affiliations
Contributions
CS designed and conducted the study, prepared the manuscript and performed statistical analyses. CPQ conducted the study and performed statistical analyses. XXM and HT designed the study and revised the manuscript. CLZ, and KZ revised the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This clinical retrospective study of single center was in accordance with the declaration of Helsinki. The work was compliant with the STROCSS criteria. All the procedures of this study were approved by the ethics committee of the Affiliated Hospital of Qingdao University. Written informed consent was waived.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Sun, C., Qu, C., Zhou, C. et al. Role of unilateral partial facet joint preservation in postero-lateral approach lumbar interbody fusion for patients with degenerative lumbar spinal stenosis presenting bilateral lower limb symptoms: a retrospective study. J Orthop Surg Res 19, 537 (2024). https://doi.org/10.1186/s13018-024-05020-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-024-05020-3