Abstract
Objective
This randomized controlled and double-blind study aimed to investigate whether the analgesic effect of the adductor canal block (ACB) combined with the genicular nerve block (GNB) after total knee arthroplasty is noninferior to that of the adductor canal block combined with local infiltration analgesia (LIA).
Methods
A total of 102 patients undergoing total knee arthroplasty under general anesthesia were included and randomly divided into: ACB + GNB and ACB + LIA groups; the ACB + LIA group received 80 mL of 0.2% ropivacaine with adrenaline 10 µg/mL for LIA, whereas the ACB + GNB group received 4 mL of 0.2% ropivacaine for the blockade of five peri-knee nerves. The primary outcome was the median difference in the visual analog scale scores at rest at 24 h between the two groups. Secondary outcomes involved the median differences in the pain scores at other time points. Other outcomes included the cumulative dosage of opioids calculated in morphine equivalents in the first 24 h and indicators related to knee joint functional recovery.
Results
In total, 36 and 38 patients were included in the ACB + GNB and ACB + LIA groups, respectively. We found that the median difference (95% confidence internal) in postoperative rest pain at 24 h (noninferiority criteria, △ = 1) was − 0.5 (− 1 to 0, p = 0.002). The median difference in cumulative opioid consumption was 1 mg (− 1 to 3, p = 0.019), meeting the noninferiority criteria, △ = 7.7 mg.
Conclusions
ACB combined with GNB provides noninferior analgesia compared to ACB with LIA on the first day after total knee arthroplasty while significantly reducing local anesthetic use.
Trial registration
Name of the Registry: Chinese Clinical Trial Registry; Trial Registration Number: ChiCTR2300074274; Date of Registration. August 2, 2023.
Similar content being viewed by others
Introduction
Background
Total knee arthroplasty (TKA) is one of the most common surgical procedures, and effective postoperative pain management has become increasingly important for patients within the framework of enhanced recovery after surgery [1, 2]. Regional anesthesia is an important method in postoperative pain management as it promotes early mobilization and contributes to faster patient recovery [3].
The latest PROSPECT guidelines [4] recommend combining a single-shot adductor canal block (ACB) with local infiltration analgesia (LIA) for managing postoperative pain after TKA. LIA compensates for the limited analgesic effect of ACB on the lateral and posterior aspects of the knee, and the ACB + LIA technique provides superior pain relief than using either ACB or LIA alone [5, 6]. However, LIA often requires high doses of local anesthetics, which may increase the risk of systemic anesthetic toxicity [7].
Ultrasound-guided genicular nerve blocks (GNB) effectively treat acute or chronic knee pain by selectively targeting the terminal sensory nerves. Compared with LIA, GNB allows the anesthetist to provide analgesia by ultrasound-guided injection of small doses of local anesthetic into three, four, or five key nerves (superior medial genicular nerve [SMGN], inferior medial genicular nerve [IMGN], superior lateral genicular nerve [SLGN], inferior lateral genicular nerve [ILGN], and recurrent tibial genicular nerve [RTGN]) to provide analgesia with a reduced dose of local anesthetic [8,9,10]. Genicular nerves are terminal branches of the femoral, saphenous, and obturator nerves and may also include branches from the sciatic nerve, carrying afferent fibers from the knee capsule [11, 12]. From an anatomical perspective, LIA blocks the posterior capsule of the knee more comprehensively than GNB. However, the main areas of pain after TKA are concentrated in the patellar region and the medial joint line [13]. Additionally, blocking the posterior capsule of the knee may affect the movement of the calf or foot muscles, and ultrasound-guided GNB is more precise with small doses of local anesthetic, making this a viable alternative to LIA. Previous studies have shown that GNB provides analgesia comparable with that of LIA [10]. However, no randomized controlled trials have compared the efficacy of the two combined analgesic regimens, ACB + LIA versus ACB + GNB, for postoperative analgesia after TKA.
Objective
This noninferiority, randomized controlled trial was intended to evaluate the combined analgesic efficacy of ACB + GNB in comparison with that of ACB + LIA to explore equally effective but safer techniques for postoperative analgesia after TKA. We hypothesized that the combined ACB + GNB could provide analgesia as effective as the combined ACB + LIA but with a significant reduction in the required local anesthetic dose.
Methods
Trial design and participants
This study was a double-blind, prospective, randomized controlled trial that was approved by the Clinical Medical Research Ethics Committee of the First Affiliated Hospital of Chongqing Medical University on April 26, 2023 (Approval No.: 2023 − 196). The trial was registered with the Clinical Trials Registry on August 2, 2023 (Registration No.: ChiCTR2300074274). Before surgery, all participants provided their informed consent. We assessed the eligibility of patients undergoing their first unilateral TKA at the First Affiliated Hospital of Chongqing Medical University from August 2023 to February 2024. The study adhered to the ethical standards of the Declaration of Helsinki and the Consort Guidelines. Patients were included who were aged 18 to 75, of any gender, scheduled for unilateral TK, had agreed to participate and signed the consent form, and who had an American Society of Anesthesiologists (ASA) degree of I–III and a body mass index (BMI) between 18 and 40 kg/m². We excluded patients with allergies to opioids or amide local anesthetics, a history of neurological or coagulation disorders, previous knee surgery, long-term opioid or significant alcohol use, cognitive impairments, or who declined to participate or chose to withdraw from the study. A researcher conducted preoperative interviews with all patients to ensure compliance with the study criteria.
Interventions
Preoperative management
The data collector documented the preoperative baseline characteristics of patients, including gender, age, BMI, ASA degree, the visual analog scale (VAS) score, range of motion of knee (ROM), quadriceps strength, and The Knee Society Score (the Function Score) [14]. After admission, all patients received an intravenous injection of parecoxib (40 mg, twice daily) for pain management. All TKAs were performed by the same team of orthopedic surgeons using a medial patellar approach, with pneumatic tourniquets and controlled blood pressure measures during the operation.
Anesthesia, ACB, GNB, and LIA
Anesthesia induction was achieved through the intravenous administration of midazolam at 0.04 mg/kg, propofol at 1–2 mg/kg, sufentanil at 0.3–0.5 µg/kg, and vecuronium at 0.08–0.1 mg/kg. Anesthesia was maintained using 1–2.5% sevoflurane, propofol at 2 mg/kg/h, remifentanil at 0.15 µg/kg/h, and vecuronium at 0.02–0.03 mg/kg. The concentration of sevoflurane in alveolar gas was monitored intraoperatively to maintain bispectral index values between 40 and 60. Following the release of the tourniquet, 1.0 g of tranexamic acid was administered intravenously.
Before surgery, all ACBs and GNBs were performed by the same experienced anesthesiologist (HKH) involved in this study. For ACB, the patient was placed in a supine position, with the operative limb externally rotated and the knee slightly flexed. A high-frequency ultrasound probe (HFL38x/13–6 MHz Transducer, SonoSite Inc., Bothell, WA, USA) was placed transversely at the midpoint of the line connecting the patella and the anterior superior iliac spine. The femoral artery, vein, sartorius muscle, vastus medialis, and adductor longus were first identified. The hyperechogenic lateral to the femoral artery, identified as the saphenous nerve, was targeted (Fig. 1). An in-plane approach was used to advance the needle (USG TYPE CCR φ0.8(21G)× 50 mm, HAKKO Medical, Nagano, Japan) to this area. Both groups of patients received an injection of 0.33% ropivacaine (20 mL), ensuring uniform spread of the solution laterally to the femoral artery under ultrasound guidance to guarantee complete blockade.
Following the ACB, the same anesthesiologist proceeded with the GNB. In line with the latest studies [10, 15], the GNE targeted five peri-knee nerve branches: SMGN, IMGN, SLGN, ILGN, and RTGN. In the ACB + GNE group, 4 mL of 0.2% ropivacaine was administered to each nerve, whereas in the ACB + LIA group, 4 mL of saline was administered to each nerve. The ultrasound probe was placed laterally around the medial supracondylar area of the femur and the medial vastus muscle, and femoral echogenicity became visible. The superior medial genicular artery, lying superficial to the femur, was identified, with the SMGN typically located near this artery. The local anesthetic was injected adjacent to the artery (Fig. 2a).
IMGN: The ultrasound probe was placed over the medial condyle of the tibia, and the inferior medial genicular artery was located near the neck of the tibia and under the medial collateral ligament. The IMGN typically runs alongside this artery, and the local anesthetic was injected adjacent to the artery (Fig. 2b).
SLGN: The ultrasound probe was placed over the lateral condyle of the femur, and the superior lateral genicular artery was found just beneath the surface, deep within the lateral vastus muscle. The SLGN is typically located near this artery, and the local anesthetic was injected adjacent to the artery (Fig. 2c).
ILGN: The ultrasound probe was placed over the lateral condyle of the tibia. At the level of the knee joint line and just beneath the surface of the tibia, the inferior lateral genicular artery was located deep to the lateral collateral ligament. The ILGN typically runs alongside this artery, and the local anesthetic was injected adjacent to the artery (Fig. 2d).
RTGN: The ultrasound probe was placed transversely between the tibial tuberosity and the Gerdy’s tubercle, and the anterior recurrent tibial artery was located just beneath the surface, deep to the tibialis anterior muscle. The RTGN typically runs alongside this artery, and the local anesthetic was injected adjacent to the artery (Fig. 2e).
Most of the time, these nerves are not clearly visible; thus, the areas near the corresponding genicular arteries are often targeted instead. If the genicular arteries cannot be located, the anesthetic solution is injected along the bone surface, based on the anatomical positions of bones and muscles.
Ultrasound landmarks for GNB (genicular nerves block). SMGN, superior medial genicular nerve ; IMGN, inferior medial genicular nerve; SLGN, superior lateral genicular nerve ; ILGN, inferior lateral genicular nerve ; RTGN, recurrent tibial genicular nerve; T, tibia; TT, tuberositas tibiae; GT, Gerdy’s tubercles; VL, vastus lateralis; VM, vastus medialis; MFC, medial femoral condyle; MTC, medial tibial condyle ; LFC, lateral femoral condyle
The standard LIA was performed intraoperatively by the same orthopedic surgeon. In the ACB + LIA group, an initial injection of 40 mL of 0.2% ropivacaine with epinephrine at a concentration of 10 µg/mL was administered into the posterior fascial plane of the posterior joint capsule following osteotomy. Then, after prosthesis implantation, 10 mL of the same solution was injected into the fascial plane surrounding each collateral ligament. Finally, 20 mL of the same solution was used for subcutaneous infiltration analgesia along the superficial fascial plane and was completed before skin closure. The ACB + GNB group received 80 mL of saline with the same performance.
Postoperative management
After surgery, each patient was administered 4 mg of ondansetron to prevent postoperative nausea and vomiting. Patients were transferred to the post-anesthesia care unit (PACU) for care and patient-controlled intravenous analgesia (PCIA) was used with all patients. Patients were discharged to the general ward when PACU discharge criteria were met. The PCIA formulation was as follows: 800 mg of tramadol was diluted with normal saline to a total volume of 80 mL. The electronic pump parameters were an initial dose of 1 mL, bolus dose of 1 mL, and lockout of 10 min. Otherwise, all patients received a standard postoperative analgesia regimen, including 40 mg of parecoxib twice daily and 100 mg of flurbiprofen axetil twice daily. All patients began physical training of the knee joint at 2 h postoperatively and were encouraged to leave their bed as early as possible.
Outcome
Data collection was performed by the data collector who was blinded to the randomization. The duration of the intraoperative tourniquet use and of operation were recorded. The primary outcome was the median difference in the VAS scores at rest at 24 h between the two groups.
Secondary outcomes involved the median differences in rest VAS scores at PACU and 6 and 12 h after surgery, as well as the median differences in the VAS scores on movement at 6, 12, and 24 h after surgery between the groups. Other outcomes included ROM and quadriceps strength on the first postoperative day; cumulative dosage of opioid calculated in morphine equivalents at the first 24 h; [16] time to first mobilization; time to first press (PCIA); duration of postoperative hospital stay; time to perform the blocks; incidence rates of postoperative nausea and vomiting (PONV); and rates of adverse events.
Sample size
This study aimed to assess whether the postoperative analgesic effect of ACB + GNB is noninferior to that of ACB + LIA, with the median difference in rest VAS scores at 24 h after surgery between the two groups as the primary outcome. Considering the previous studies and the minimum clinically important difference, this study set the noninferiority margin at 1 [17]. Based on pilot data with 20 patients, who received ACB + GNB and ACB + LIA, the mean ± standard deviations (SDs) of 2.36 ± 1.50 and 2.64 ± 1.62 were assumed for the 24-h postoperative VAS score distributions at rest. Using an α of 0.025 and a power of 90%, the study required 33 patients per group, and assuming a 20% dropout rate, we enrolled 42 patients per group. Based on a previous LIA study using PCIA for postoperative analgesia, the noninferiority margin of total intravenous morphine consumption was set at 7.7 mg in this study [18].
Randomization
Herein, a computer-generated random number table and corresponding group assignments were created. To ensure allocation concealment, all random numbers were sealed in opaque, numbered envelopes. Then, after participants were enrolled, researchers sequentially drew the envelopes in the order of enrollment to determine the treatment group that participants were assigned to. The allocation of pain-relief techniques and group assignments remained blinded to surgeons, anesthesiologists, nurses, physiotherapists, data collectors, and statistical analysts. All local anesthetic solutions were prepared by the investigator, who was the only individual aware of group assignments.
Our analysis population is the per-protocol (PP) population. Patients who were lost to follow-up or withdrew from the study were not included in statistical analyses. Statistical analyses were conducted using IBM SPSS 23.0 (IBM Corporation, Armonk, NY, USA), and noninferiority tests were performed with SAS 9.4 software. Normally distributed continuous data are expressed as mean ± standard deviation, while non-normally distributed measures are expressed as median (M) and interquartile range (IQR). Repeated measures data were analyzed using a generalized linear mixed model (GLMM) to compare group effects, time effects, and group-time interaction effects. For the remaining measures, group comparisons were made using the t-test or Mann-Whitney U test. Categorical data are presented as the number or cases (%), and the χ2 test was used for comparison between groups. In these tests, p < 0.05 was considered significant. In the noninferiority test, the comparison of VAS scores and opioid consumption in the first 24 h was conducted using the Hodges–Lehmann method to calculate the 95% confidence interval (95% CI), while a one-sided Wilcoxon rank-sum test was used to verify noninferiority, with p < 0.025 considered statistically significant.
Result
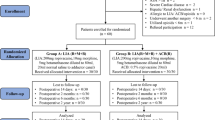
A total of 102 patients scheduled for elective primary TKA were assessed for eligibility, and 18 patients were excluded. All enrolled patients (n = 84) were randomized into two groups. In total, 74 patients were included in the final analysis, with 36 in the ACB + GNB group and 38 in the ACB + LIA group (Fig. 3). No significant differences were found in the baseline characteristics between the two groups (Table 1). The time to perform GNE for both groups was around 5 min. In five patients, at least one artery was not observed, and the block was performed according to the corresponding anatomical landmarks.
Primary, secondary, and other outcomes are shown in Table 2. The median (IQR) VAS scores at rest at 24 h for the ACB + GNB and ACB + LIA groups were 3 (1.25–4) and 3 (2–4.25), respectively (Fig. 4). The 95% CI for the median difference was − 0.5 (− 1 to 0), with the upper limit being less than the noninferiority margin of 1, meeting the criteria for noninferiority (p<0.01). The group t-test at this time point indicated that the VAS scores for the ACB + GNE were not superior to those for the ACB + LIA group (p>0.05). At other time points as well, the ACB + GNB group showed noninferior pain relief to that of the ACB + LIA group, both at rest and during activity (Fig. 5). The median (IQR) cumulative opioid consumption in intravenous morphine equivalents during the first 24 h was 10.5 mg (7–12.5) for ACB + GNB versus 8 mg (5.75–10.5) for ACB + LIA. The 95% CI for median differences for postoperative 0–12 and the entire first day were 0 (− 1 to 1) and 1 (− 1 to 3), respectively, fulfilling the noninferiority standard of △ = 7.7 mg (Table 2). No significant differences were found between the two groups in time to first mobilization, time to first press (PCIA), incidence rates of PONV at first 24 h, as well as duration of postoperative hospital stay (Table 2). No patient experienced foot drop or any other adverse event.
Table 3 presents the results of the GLMM analysis for repeated measures data (postoperative VAS scores, postoperative quadriceps strength, and knee ROM). At 12 and 24 h postoperatively, the resting VAS scores were significantly influenced by the time effect. The group effect, time effect, and group-time interaction had no impact on the movement VAS scores. At 12 and 24 h postoperatively, quadriceps strength was significantly influenced by the time effect. At 24 h postoperatively, knee ROM was significantly influenced by the time effect.
Box plots for VAS(visual analogue scale) scores at PACU; 6 h; 12 h; and 24 h. The blue lines represent group ACB + GNB; The red lines represent group ACB + LIA. The thin lines represent the scores at rest; The thick lines represent the scores on movement. ACB, adductor canal block; GNB, genicular nerves block; LIA, local infiltration analgesia.
VAS (visual analogue scale) scores on median differences for with the non-inferiority margin Δ of 1. Error bars representing 95% CIs. The blue lines represents median differences at rest; The red lines represents median differences on movement. ACB, adductor canal block; GNB, genicular nerves block; LIA, local infiltration analgesia
Discussion
Our results demonstrate that ACB + GNB indeed showed noninferior analgesic effects for postoperative 24-h VAS scores, which was also reflected at other time points in the first 24 h. Additionally, both groups exhibited noninferiority for opioid consumption over 24 h after surgery. In the GLMM analysis, the results indicated that VAS scores, quadriceps strength, and knee ROM were all affected by the time effect, with the most significant impact observed at 24 h postoperatively. These findings suggest that paying attention to pain levels and knee function recovery at this time point is particularly important, and also confirm that selecting 24 h postoperatively as the primary time point in this study was appropriate.
ACB, GNB, and LIA are all distal nerve blocks for the lower limb that preserve motor function, making them popular choices among anesthesiologists and surgeons [19]. In previous studies, the median pain score during activity for patients undergoing TKA with ACB alone often ranged between 5 and 6 [5, 20], although, this ranged between 2 and 4 in both groups in this study. Beyond the analgesic effects of GNB and LIA on the lateral aspect of the knee, their nerve innervation also overlaps with the medial aspect covered by ACB. However, the presence of the nerve to vastus medialis, which significantly contributes to the anterior medial joint capsule, within the adductor canal has been a subject of ongoing debate [21, 22]. Therefore, the addition of LIA or GNB is necessary.
The volume range selected for LIA varies between 20 and 300 mL, and is often combined with other medications such as epinephrine and nonsteroidal anti-inflammatory drugs [23, 24]. Although some studies on the application of LIA in lower limb surgeries have shown that high doses of ropivacaine infiltration do not induce elevated free plasma ropivacaine concentrations associated with local anesthetic toxicity, some patients still experience symptoms of potential local anesthetic toxicity, such as nausea, vomiting, dizziness, and arrhythmia [25, 26]. In our study, no differences were present in the incidence of adverse reactions between the two groups, which may be due to the relatively low dose of LIA used (80 mL of 0.2% ropivacaine). Our study also found that the median VAS scores at rest on the first postoperative day were similar in both groups, whereas the ACB + GNB group had lower VAS scores during knee joint activity from 0 to 12 h postoperatively. This difference may be attributed to the limitations of LIA. Since the primary steps of LIA involve infiltration at the surgical incision site, this mainly targets the areas innervated by the medial femoral cutaneous nerve and the intermediate femoral cutaneous nerve [27]. However, previous studies have shown that blocking these nerves is unlikely to produce significant clinical effects [28].
GNB, as an innovative intervention, is primarily used to alleviate pain associated with chronic knee osteoarthritis. Although Yasar et al. noted that the positions of SMGN, IMGN, SLGN, and ILGN are relatively fixed and run along small arteries on the bone cortex [12, 29], the most commonly used technique is the three-point injection method (excluding ILGN) owing to the proximity of ILGN to the common peroneal nerve, which poses a risk of foot drop [30]. However, in our study, despite using a larger volume than that used in chronic pain treatment (4 vs. 1 mL), patients in the ACB + GNE group did not experience foot drop or other adverse events, which is consistent with the findings of Cuñat [10]. This may be because we accurately located the inferior lateral genicular artery in each patient and used a lower concentration of local anesthetic [31]. Therefore, we recommend avoiding the use of excessively high concentrations of local anesthetics for GNE and monitoring for any clinical signs of foot drop. According to Franco’s study, our study also blocked the RTGN, a branch of the peroneal nerve closely associated with the anterior tibial recurrent artery, to ensure analgesia on the lower lateral side [12, 32]. This five-point GNB technique provided more comprehensive analgesia and only took approximately 5 min to perform.
When using two or more nerve block techniques, vigilance must be maintained for local anesthetic toxicity in TKA patients over the long term. This is not only because the combination of techniques means an increase in the dose of local anesthetic but also because advanced age and female gender are high-risk factors for local anesthetic toxicity, characteristics that are also common among TKA patients [33]. Conversely, GNE relies on ultrasound identification of relevant vascular or bony structures, significantly reducing the amount of local anesthetic required (20 vs. 80 mL of 0.2% ropivacaine), making this safer and more precise when combined with ACB and provided clear imaging in obese patients. A recent cadaveric study showed that, in knee radiofrequency ablation, GNE can achieve 100% accuracy using only bony landmarks, even without arterial pulsation [34].
We did not add epinephrine to the GNB as we did with LIA to prolong the block duration [35], primarily because the regions innervated by the genicular nerves have a relatively low blood, which already results in a slower absorption rate of the local anesthetic. However, the ACB + LIA group showed an advantage in opioid consumption with a lower overall consumption at 24 h, with totals of 10.5 mg (7–12.5) and 8 mg (5.75–10.5) in the two groups, respectively, although the result did not exhibit a significant difference in Mann-Whitney U test. It is consistent with those of previous studies comparing GNB and LIA [10], possibly because of the higher dosage of local anesthetics in LIA and the addition of epinephrine, which prolongs the duration of the block, thereby promoting greater tolerance during knee exercises and reducing the number of PCIA presses postoperatively. But this difference may require an experiment with a larger sample size and higher statistical power to prove.
Our study has several limitations. First, this study used general anesthesia instead of spinal anesthesia, considering intraoperative anxiety, of patients, which does not align with recommendations and daily clinical practice in Europe/United States. Additionally, the use of parecoxib, flurbiprofen axetil, and tramadol for postoperative pain management in PCIA is uncommon in other European medical institutions, limiting the generalizability of our findings. Second, this study selected the 24-h postoperative pain score as the primary endpoint because many patients begin more extensive and active rehabilitation activities at this time. We believe that the pain level at 24 h postoperatively remains an important determinant of the ability of the patient to engage in postoperative activities. However, pain assessment in the early postoperative period (at 6 and 12 h) as well as beyond 24 his equally important, and future studies should aim to evaluate postoperative pain more comprehensively. Third, as previously mentioned, a standardized protocol is not currently available for LIA, and the dosages and compositions of drugs vary across institutions. The LIA protocol used in this study is not representative. Fourth, the VAS score is a subjective measure that can be influenced by emotional, social, cultural, and other factors [36]. Lastly, noninferiority trials are recommended to demonstrate noninferiority in both the intention-to-treat and PP populations [37]. However, we only demonstrated the noninferiority of ACB + GNB in the PP population.
The results of our study suggest that combining ACB with GNB for postoperative analgesia in TKA may produce effects similar to those achieved with the commonly used ACB + LIA regimen on the first postoperative day while also reducing the use of local anesthetics, making this a potentially valuable pain-management strategy. However, these results only apply to the initial 24 h postoperatively, and further research is needed to evaluate the effects of this regimen over a longer period. Additionally, future studies could explore differences in ACB sites, variations in drug formulations and volumes in LIA, and changes in the number of blocked nerves in GNB to understand the role of combined nerve block strategies in balancing postoperative analgesia and lower limb function recovery in more depth.
Data availability
No datasets were generated or analysed during the current study.
References
Kester B, Minhas S, Vigdorchik J, et al. Total knee arthroplasty for posttraumatic osteoarthritis: is it Time for a new classification? J Arthroplasty. 2016;31(8):1649–e16531641. https://doi.org/10.1016/j.arth.2016.02.001.
Tan M, Law LS, Gan TJ. Optimizing pain management to facilitate enhanced recovery after surgery pathways. Can J Anaesth. 2015;62(2):203–18. https://doi.org/10.1007/s12630-014-0275-x.
Terkawi A, Mavridis D, Sessler D, et al. Pain Management modalities after total knee arthroplasty: a Network Meta-analysis of 170. Randomized Controlled Trials Anesthesiology. 2017;126(5):923–37. https://doi.org/10.1097/ALN.0000000000001607.
Lavand’homme PM, Kehlet H, Rawal N, PROSPECT Working Group of the European Society of Regional Anaesthesia and Pain Therapy (ESRA), et al. Pain management after total knee arthroplasty: PROcedure SPEcific Postoperative Pain ManagemenT recommendations. Eur J Anaesthesiol. 2022;39(9):743–57. https://doi.org/10.1097/EJA.0000000000001691.
Seo SS, Kim OG, Seo JH, et al. Comparison of the Effect of continuous femoral nerve Block and Adductor Canal Block after primary total knee arthroplasty. Clin Orthop Surg. 2017;9(3):303–9. https://doi.org/10.4055/cios.2017.9.3.303.
Marya SKS, Arora D, Singh C, et al. A prospective comparative study of local infiltration versus adductor block versus combined use of the two techniques following knee arthroplasty. J Arthroplasty. 2020;2(1):15. https://doi.org/10.1186/s42836-020-00034-8.
Mitchell K, Cai E, Miller B et al. Local anesthetic systemic toxicity from local infiltration anesthesia in total joint arthroplasty: a single center retrospective study. Reg Anesth Pain Med 2023:rapm-2023-104880. https://doi.org/10.1136/rapm-2023-104880
Shanahan EM, Robinson L, Lyne S, et al. Genicular nerve block for Pain Management in patients with knee osteoarthritis: a randomized placebo-controlled trial. Arthritis Rheumatol. 2023;75(2):201–9. https://doi.org/10.1002/art.42384.
González Sotelo V, Maculé F, Minguell J, et al. Ultrasound-guided genicular nerve block for pain control after total knee replacement: preliminary case series and technical note. Rev Esp Anestesiol Reanim. 2017;64(10):568–76. https://doi.org/10.1016/j.redar.2017.04.001.
Cuñat T, Mejía J, Tatjer I et al. Ultrasound-guided genicular nerves block vs. local infiltration analgesia for total knee arthroplasty: a randomised controlled non-inferiority trial. Anaesth 2023:78(2):188–96. https://doi.org/10.1111/anae.15909
Franco CD, Buvanendran A, Petersohn JD, et al. Innervation of the Anterior Capsule of the human knee: implications for Radiofrequency ablation. Reg Anesth Pain Med. 2015;40(4):363–8. https://doi.org/10.1097/AAP.0000000000000269.
Tran J, Peng PWH, Lam K, et al. Anatomical study of the innervation of anterior knee Joint Capsule: implication for image-guided intervention. Reg Anesth Pain Med. 2018;43(4):407–14. https://doi.org/10.1097/AAP.0000000000000778.
Mekkawy KL, Zhang B, Wenzel A, et al. Mapping the course to recovery: a prospective study on the anatomic distribution of early postoperative pain after total knee arthroplasty. Arthroplasty. 2023;5:37. https://doi.org/10.1186/s42836-023-00194-3.
Miralles-Muñoz FA, Gonzalez-Parreño S, Martinez-Mendez D, et al. A validated outcome categorization of the knee society score for total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2022;30(4):1266–72. https://doi.org/10.1007/s00167-021-06563-2.
Pietrantoni P, Cuñat T, Nuevo-Gayoso M, et al. Ultrasound-guided genicular nerves block: an analgesic alternative to local infiltration analgesia for total knee arthroplasty: a noninferiority, matched cohort study. Eur J Anaesthesiol. 2021;38(Suppl 2):S130–7. https://doi.org/10.1097/EJA.0000000000001546.
Nielsen S, Degenhardt L, Hoban B, et al. A synthesis of oral morphine equivalents (OME) for opioid utilisation studies. Pharmacoepidemiol Drug Saf. 2016;25(6):733–7. https://doi.org/10.1002/pds.3945.
Myles PS, Myles DB, Galagher W, et al. Measuring acute postoperative pain using the visual analog scale: the minimal clinically important difference and patient acceptable symptom state. Br J Anaesth. 2017;118(3):424–9. https://doi.org/10.1093/bja/aew466.
Unver B, Yuksel E, Eymir M, et al. Effect of Local Infiltration Analgesia on functional outcomes in total knee arthroplasty: a Randomized, Placebo-Controlled, double-blind clinical trial. J Knee Surg. 2022;35(4):367–74. https://doi.org/10.1055/s-0040-1715103.
Layera S, Aliste J, Bravo D, et al. Motor-sparing nerve blocks for total knee replacement: a scoping review. J Clin Anesth. 2021;68:110076. https://doi.org/10.1016/j.jclinane.2020.110076.
Hanson NA, Allen CJ, Hostetter LS, et al. Continuous ultrasound-guided adductor canal block for total knee arthroplasty: a randomized, double-blind trial. Anesth Analg. 2014;118(6):1370–7. https://doi.org/10.1213/ANE.0000000000000197.
Burckett-St Laurant D, Peng P, Girón Arango L, et al. The nerves of the Adductor Canal and the innervation of the knee: an anatomic study. Reg Anesth Pain Med. 2016;41(3):321–7. https://doi.org/10.1097/AAP.0000000000000389.
Andersen HL, Andersen SL, Tranum-Jensen J. The spread of injectate during saphenous nerve block at the adductor canal: a cadaver study. Acta Anaesthesiol Scand. 2015;59(2):238–45. https://doi.org/10.1111/aas.12451.
Li C, Qu J, Pan S, et al. Local infiltration anesthesia versus epidural analgesia for postoperative pain control in total knee arthroplasty: a systematic review and meta-analysis. J Orthop Surg Res. 2018;13(1):112. https://doi.org/10.1186/s13018-018-0770-9.
Marques EM, Jones HE, Elvers KT, et al. Local anaesthetic infiltration for peri-operative pain control in total hip and knee replacement: systematic review and meta-analyses of short- and long-term effectiveness. BMC Musculoskelet Disord. 2014;15:220. https://doi.org/10.1186/1471-2474-15-220.
Brydone AS, Souvatzoglou R, Abbas M, et al. Ropivacaine plasma levels following high-dose local infiltration analgesia for total knee arthroplasty. Anaesthesia. 2015;70(7):784–90. https://doi.org/10.1111/anae.13017.
Busch CA, Whitehouse MR, Shore BJ, et al. The efficacy of periarticular multimodal drug infiltration in total hip arthroplasty. Clin Orthop Relat Res. 2010;468(8):2152–9. https://doi.org/10.1007/s11999-009-1198-7.
Bjørn S, Nielsen TD, Moriggl B et al. Anesthesia of the anterior femoral cutaneous nerves for total knee arthroplasty incision: randomized volunteer trial. Reg Anesth Pain Med 2019:rapm-2019-100904. https://doi.org/10.1136/rapm-2019-100904
Kampitak W, Tanavalee A, Ngarmukos S, et al. Effect of ultrasound-guided selective sensory nerve blockade of the knee on pain management compared with periarticular injection for patients undergoing total knee arthroplasty: a prospective randomized controlled trial. Knee. 2021;33:1–10. https://doi.org/10.1016/j.knee.2021.08.024.
Yasar E, Kesikburun S, Kılıç C et al. Accuracy of Ultrasound-Guided Genicular Nerve Block: A Cadaveric Study. Pain Physician. 2015;18(5):E899-904. PMID: 26431143.
Rambhia M, Chen A, Kumar AH, et al. Ultrasound-guided genicular nerve blocks following total knee arthroplasty: a randomized, double-blind, placebo-controlled trial. Reg Anesth Pain Med. 2021;46(10):862–6. https://doi.org/10.1136/rapm-2021-102667.
Casati A, Fanelli G, Borghi B, et al. Ropivacaine or 2% mepivacaine for lower limb peripheral nerve blocks. Study Group on Orthopedic Anesthesia of the Italian Society of Anesthesia, Analgesia, and Intensive Care. Anesthesiology. 1999;90(4):1047–52. https://doi.org/10.1097/00000542-199904000-00018.
Van den Bergh FR, Vanhoenacker FM, De Smet E, et al. Peroneal nerve: normal anatomy and pathologic findings on routine MRI of the knee. Insights Imaging. 2013;4(3):287–99. https://doi.org/10.1007/s13244-013-0255-7.
Neal JM, Barrington MJ, Fettiplace MR, et al. The third American Society of Regional Anesthesia and Pain Medicine Practice Advisory on local anesthetic systemic toxicity: executive Summary 2017. Reg Anesth Pain Med. 2018;43(2):113–23. https://doi.org/10.1097/AAP.0000000000000720.
Kolakkanni C, Gonnade NM, Gaur R, et al. Can ultrasound-guided radiofrequency ablation of genicular nerves of the knee, be performed without locating corresponding arterial pulsations-a cadaveric study. BMC Musculoskelet Disord. 2023;24(1):654. https://doi.org/10.1186/s12891-023-06761-8.
Brummett CM, Williams BA. Additives to local anesthetics for peripheral nerve blockade. Int Anesthesiol Clin. 2011;49(4):104–16. https://doi.org/10.1097/AIA.0b013e31820e4a49.
Hawker GA, Mian S, Kendzerska T, et al. Measures of adult pain: visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), short-form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), short Form-36 Bodily Pain Scale (SF-36 BPS), and measure of intermittent and constant Osteoarthritis Pain (ICOAP). Arthritis Care Res (Hoboken). 2011;63(Suppl 11):S240–252. https://doi.org/10.1002/acr.20543.
U.S. Food and Drug Administration. Non-inferiority clinical trials. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/non-inferiority-clinical-trials (2021).
Acknowledgements
The authors express their gratitude to Hong Chen (Orthopedist, Department of Orthopedics, The First Affiliated Hospital of Chongqing Medical University) for assisting with data collection.
Funding
This work was supported by grants from National Key Clinical Specialty Construction Project(2011 − 170) and Chongqing medical scientific research project (Joint project of Chongqing Health Commission and Science and Technology Bureau 2024MSXM025). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
Study conception and design: Tong Mu ; Acquisition of data: Qian Yang and Ke Wei; Analysis and interpretation of data: Tong Mu ; Drafting of manuscript: Tong Mu; Critical revision: Baohong Yuan and Ke Wei. All authors discussed the results and commented on the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This trial was performed in accordance with the Declaration of Helsinki and was approved by the Institutional Ethical Review Committee for Clinical Trials of The First Affiliated Hospital of Chongqing Medical University (NO. 2023 − 196).
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Mu, T., Yuan, B., Wei, K. et al. Adductor canal block combined with genicular nerve block versus local infiltration analgesia for total knee arthroplasty: a randomized noninferiority trial. J Orthop Surg Res 19, 546 (2024). https://doi.org/10.1186/s13018-024-05048-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-024-05048-5