Abstract
Background
Different risk factors affect the intensive care unit (ICU) stay after cardiac surgery. This study aimed to evaluate these risk factors.
Patients and methods
A retrospective analysis was conducted on clinical, operative, and outcome data from 1070 patients (mean age: 59 ± 9.8 years) who underwent isolated coronary bypass grafting CABG surgery with cardiopulmonary bypass. The outcome variable was prolonged length of stay LOS in the CICU stay (> 3 nights after CABG).
Results
Univariate predictors of prolonged ICU stays included a left atrial diameter of > 4 cm (P < 0.001),chronic obstructive airway disease COPD (P = 0.005), hypertension (P = 0.006), diabetes mellitus (P = 0.009), having coronary stents (P = 0.006), B-blockers use before surgery (either because the surgery was done on urgent or emergency basis or the patients have contraindication to B-blockers use) (P = 0.005), receiving blood transfusion during surgery (P = 0.001), post-operative acute kidney injury (AKI) (P < 0.001), prolonged inotropic support of > 12 h (P < 0.001), and ventilation support of > 12 h (P < 0.001), post-operative sepsis or pneumonia (P < 0.001), post-operative stroke/TIA (P = 0.001), sternal wound infection (P = 0.002), and postoperative atrial fibrillation POAF (P < 0.001).
Multivariate regression revealed that patients with anleft atrial LA diameter of > 4 cm (AOR 2.531, P = 0.003), patients who did not take B-blockers before surgery (AOR 1.1 P = 0.011), patients on ventilation support > 12 h (AOR 3.931, P = < 0.001), patients who developed pneumonia (AOR 20.363, P = < 0.001), and patients who developed post-operative atrial fibrillation (AOR 30.683, P = < 0.001) were more likely to stay in the ICU for > 3 nights after CABG.
Conclusion
Our results showed that LA diameter > 4 cm, patients who did not take beta-blockers before surgery, on ventilation support > 12 h, developed pneumonia post-operatively, and developed POAF were more likely to have stays lasting > 3 nights. Efforts should be directed toward reducing these postoperative complications to shorten the duration of CICU stay, thereby reducing costs and improving bed availability.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Coronary artery bypass grafting (CABG) is the most commonly performed type of cardiac surgery worldwide. CABG aims to improve the quality of life of patients by alleviating angina and heart failure symptoms and increasing survival rates [1]. However, CABG is associated with risk of morbidity and mortality [2]. Previous studies reported mortality rates after an isolated CABG ranging from 2.6 to 12.2% [3,4,5]. Predictors of post-surgical mortality and morbidity have been studied thoroughly in various countries [3,4,5,6]. In Jordan, we previously studied the determinants of three complications after isolated CABG surgery (renal impairment, pneumonia, and sternal wound infection). We found that age, female sex, history of diabetes mellitus, COPD, peripheral vascular disease, renal impairment, emergency surgery, perioperative blood transfusion, mechanical ventilation of > 12 h, and prolonged inotropic support were associated with 30-day complications after on-pump isolated CABG surgery [6].
Cardiac intensive care units (CICUs) are specialized units that provide care to patients after cardiac surgery or critically ill patients. However, the care provided by intensive care units is costly and labor-intensive. Compounded by a limited number of ICU beds, most ICUs operate at or near full capacity [7]. Thus, bed unavailability has become a critical issue that can significantly impact other services, including operating theatres. Extending ICU capacity may not always be feasible due to physical constrains, resources limitations, or government regulations [8]. For these reasons, the duration of ICU stay is of major importance following cardiac surgery, as well as other types of surgery.
Perioperative management of patients undergoing (CABG) has been improving recently, but the duration of LOS in the CICU stay varies from one to several days for various reasons. Prolonged LOS in the CICU stay in these patients increases both overall hospital and CICU costs [9] and reduces the availability of CICU beds for other critically ill patients. Therefore, the ability to predict the duration of CICU stay in patients undergoing CABG is invaluable. Many studies [10, 11] have reported perioperative risk factors for prolonged ICU stay, with prolonged mechanical ventilation considered one of the most critical factors. Other studies have indicated that prolonged inotrope use and blood transfusion in the CICU can predict the duration of LOS [12].
In this study, we assessed the factors influencing the length of ICU stay in patients following CABG by analyzing pre-operative, intra-operative, and immediate postoperative variables.
Patients and methods
This retrospective cohort study included all patients who underwent isolated CABG at the Princess Mona Heart Institute/King Abdullah University Hospital in northern Jordan between January 2005 and June 2022. This study was approved by the Institutional Review Board of King Abdullah University Hospital. The exclusion criteria included repeat surgery, valve surgery, and combined CABG and valve surgery. A total of 1070 consecutive patients were included in this study. Patients are typically transferred to the CICU immediately after surgery. The CICU, specializing in cardiac surgery, is a well-equipped unit with six beds and a patient to nurse ratio of 1:1. Patients were transferred to the ward once they achieved hemodynamic stability, were successfully weaned from the ventilator, were able to ambulate, and no longer required inotropes and vasopressors. This transfer occurred either until the removal of chest drains or their output remained consistently low (5–6 consecutive hours with no drainage). The criteria for weaning from the ventilator included hemodynamic stability, adequate urine output, regaining full consciousness (including obeying commands), minimal chest tube drainage (< 50 cc/hour), normal chest X-ray findings, and normal arterial blood gases on continuous positive airway pressure CPAP and T-piece. All patients were transferred from the CICU after ensuring that they did not require reexploration for bleeding. Staying for ≤ 3 nights in the CICU was considered normal, whereas staying for > 3 nights was considered prolonged. The average stay of three nights struck a balance between patient stabilization, cost consideration, and limited resources of the CICU. In this study, patients were categorized into two groups: normal (n = 276) and prolonged (n = 794) stays. Of the patients with prolonged ICU stay, clinical, laboratory, and demographic data were obtained retrospectively from the patients’ medical records. Data on plasma glucose, low-density lipoprotein, high-density lipoprotein, triglyceride, and total cholesterol levels were obtained from the King Abdullah University Hospital Information Registry. Preoperative medication use was collected from all the patient data and assessed in relation to the duration of ICU stay following CABG.
Myocardial infarction (MI) was defined according to the fourth universal definition of MI. It entails an elevation or drop in cardiac enzymes (specifically troponin) beyond the 99th percentile of the upper reference limit, combined with at least one of the following: MI symptoms, new electrocardiogram (ECG) ischemic changes, the presence of pathological Q wave, or imaging evidence consistent with ischemia [13].
ST-elevation myocardial infarction STEMI was defined according to the European Society of Cardiology (ESC) guidelines: at least two contiguous leads with ST-segment elevation of ≥ 2.5 mm in men < 40 years, ≥ 2 mm in men ≥ 40 years, or ≥ 1.5 mm in women, particularly in leads V2–V3, and/or ≥ 1 mm in the other leads in the absence of left ventricular (LV) hypertrophy or left bundle branch block (LBBB) [14].
Recent myocardial infarction was defined as MI within 28 days after CABG. Heart failure was considered if the patient was symptomatic or undergoing anti-failure treatment. Diabetes status (taking either oral hypoglycemic agents or insulin), hypertension status (being on treatment), renal dysfunction (having creatinine serum level of 2.0 mg/dl or on chronic dialysis), post-operative acute kidney injury AKI(having serum creatinine doubled after surgery), COPD (having diagnosed by pulmonogist at any time before surgery), peripheral vascular disease (having a positive history of intermittent claudication or having a documented clinical or radiological evidence of ischemia) were all recorded. Left ventricular ejection fraction was obtained from transthoracic echocardiography measurements. Left ventricular ejection fraction (LVEF) was classified into three groups according to the degree of dysfunction: normal (LVEF ≥ 50%), mild to moderate impairment (LVEF between 36 and 49%), and severe impairment (LVEF ≤ 35%). The number of diseased coronary arteries was obtained from the coronary angiography report. Patients with significant coronary artery disease underwent CABG according to American College of Cardiology (ACC) and American Heart Association (AHA) guidelines [15,16,17]. Surgery was considered emergency or urgent if the patient was sent to the operating room within 24 h from the time of cardiac catheterization, typically due to unstable angina, hemodynamic instability, or an untoward event in the catheterization suite. Preoperative trans-thoracic echocardiography studies were performed to evaluate left ventricular ejection fraction LVEF, the degree of mitral/aortic/tricuspid valve regurgitation, and left atrial LA size (diameter). MR was graded from 0 to 4, with 0 = competent, 0–1 = trace MR, 1–2 = mild MR, 2–3 = moderate MR, and 3–4 = severe MR. Left atrial diameter was calculated using the long axis view, measuring the anteroposterior dimension in M-mode. Cardiopulmonary bypass time (pump time) was considered prolonged if > 120 min, and cross clamp time was considered prolonged if > 90 min. Inotropic support was considered prolonged if it continues for 48 h or more, and ventilation support was considered prolonged if it stayed > 12 h. Pneumonia was diagnosed based on symptoms (cough, fever, and SOB), and radiological or microbiological evidence was diagnosed from sputum culture. Sternal wound infection was defined based on presence of purulent discharge from the wound, positive wound culture, or radiological evidence of mediastinitis. Stroke was defined as a permanent neurological deficit by clinical examination and with radiological evidence by brain CT scan or MRI. Pre-, peri-, and postoperative measurements were evaluated as possible independent risk factors for prolonged ICU stay after CABG.
Statistical analysis
SPSS version 22 was used for data analysis. Frequencies and percentages were used to summarize categorical variables, while mean ± standard deviation was used for continuous variables. Duration of ICU stay was dichotomized into ≤ 3 nights or > 3 nights. Independent sample t-tests or χ2 tests were used to analyze independent variables for prolonged ICU stay (> 3 days), as appropriate. P-values are reported for bivariate analyses. All independent variables that were significantly associated with a prolonged ICU stay (P < 0.05) were included in the backward conditional logistic regression model (entry at P = 0.05, removal at P = 0.2). Adjusted odds ratios (AOR) and P values are reported. The alpha level for all analyses was set at 0.05. A logistic regression model was used to include variables that were significantly associated with a prolonged ICU stay at the bivariate level. Variable collinearity was tested using a multicollinearity diagnostic test, and the VIF was inspected accordingly. None of the VIF values were greater than 1.2.
Results
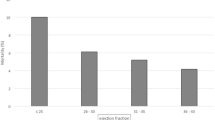
The mean age of the study participants was 59 years, and males comprised approximately three quarters of the cohort (77.8%). Approximately two-thirds of the participants had hypertension, half had diabetes mellitus, and only 12.1% had heart failure. Table 1 shows the main preoperative demographic and clinical characteristics, while Table 2 shows the intra- and postoperative demographic and clinical characteristics of the study participants (N = 1070), as well as the unadjusted risks of clinical variables on the duration of ICU stay. As expected for a CABG population, 80% had stable angina, while approximately 20% had experienced a recent (≤ 28 days) myocardial infarction. Most patients (76%, 794 patients) had LOS in the ICU for ≤ 3 nights, while about one-fourth of the participants had > 3 days of ICU stay (26%, 276 patients). Preoperatively, most patients received statins, B-blockers, clopidogrel, and angiotensin-converting enzyme inhibitors, while 27.3% received diuretics. Approximately 16% of patients reported stopping clopidogrel for at least a week before surgery. Most participants underwent 4–6 bypass grafts, from the left internal mammary artery to the left anterior descending artery used in the majority of patients. Extended pump time (≥ 120 min) and aortic clamp time (≥ 90 min) were documented in 15.5% and 7.2% of patients, respectively. Sternal wound infections and pneumonia were diagnosed in 3.3% and 5.1% of patients, respectively, while 6.0% of patients had an ICU stay of a week or more. The prevalence of postoperative AKI was 8.1%. Incidence of postoperative atrial fibrillation was documented in 25.5% of the patients. Of the patients’ category with prolonged stay in the CICU, only 20 were discharged and readmitted to the ICU due to arrhythmia (nine patients), hemodynamic instability (six patients), and wound infection (five patients), while in the early discharge group from the CICU, only six patients were readmitted due to atrial fibrillation (four patients) and hemodynamic instability (two patients).
Overall, 60 patients (5.6%) died within 30 days. Most mortalities occurred in those who stayed for > 3 nights. Among those who stayed for > 3 nights, mortality rate was 12.5%, compared to 4.8% among those who reported staying ≤ 3 nights (P < 0.001). Those who reported to stay > 3 nights were 2.87 times as likely to die compared to those who stayed ≤ 3 nights (95% CI 1.78–4.65).
Mean (SD) ICU stay was 3.34 (2.05) nights with a range between 0 and 23 nights (median and IQR are 3.00 and 2.00, respectively). More than one quarter of participants (25.8%, n = 276) had an ICU stay of > 3 nights.
Univariate predictors of prolonged ICU stay included left atrial diameter > 4 cm, COPD, hypertension, diabetes mellitus, history of coronary stents, beta-blockers use before surgery, receiving blood transfusion during surgery, postoperative AKI, prolonged inotropic support for > 12 h, ventilation support for > 12 h, postoperative sepsis or pneumonia, post-operative stroke/TIA, sternal wound infection, and postoperative atrial fibrillation.
The multivariate logistic regression model included all variables that were associated with postoperative prolonged ICU stay (P < 0.2), along with variables of clinical significance: age, sex, and body mass index (Table 3). Patients with LA diameter > 4 cm (AOR 2.531, P = 0.003), patients who did not take beta-blockers before surgery (AOR 1.1, 2.7, P = 0.011), patients on ventilation support > 12 h (AOR 3.931, P = < 0.001), patients who developed pneumonia (AOR 20.363, P = < 0.001), and patients who developed post-operative atrial fibrillation (AOR 30.683, P = < 0.001) were more likely to stay for > 3 nights in the ICU after CABG.
Discussion
The treatment process for cardiac surgery patients is complex and involves pre-, intra-, and postoperative care provided by different multidisciplinary teams at each stage. The cardiac surgeon who performs the operation should serve as the central figure responsible for coordinating and connecting the various stages of the process. Postoperative complications, which influence hospitalization in the ICU, are the results of events occurring at all three perioperative stages; frequently, the ICU is the last stage, where shortcomings and errors of earlier stages, which determine the length of ICU stay, guarantee the quality of the result of cardiac surgery.
In this study, we present our low-volume, single-center experience of the duration of CICU stays after CABG at our center. Pre-, intra-, and postoperative variables were included in a multivariate regression model to predict duration of ICU stay in 1070 patients who underwent isolated CABG surgery.
Advanced age has been shown in some studies to predict prolonged ICU stay and other morbidities after CABG and other cardiac surgeries [6, 9]. In this study, age was not a predictor of prolonged stay after isolated CABG. We believe that this is related to the fact that our cohort was relatively young (mean age, 59 years).
We have previously reported a strong association between left atrial enlargement and mortality after isolated CABG and valve surgery [18, 19]. Our study also showed an association between left atrial enlargement and prolonged ICU stay. Other reports have also shown a relationship between LA size and prolonged ICU stay [20]. LA enlargement may indicate poor LV function and disease chronicity, particularly mitral valve disease.
Borzak et al. [21] showed that post-operative atrial fibrillation (POAF) is an independent predictor of prolonged ICU stay independent of advanced age. Our finding that POAF is an independent predictor of prolonged ICU stay confirms that POAF by itself is a strong predictor of prolonged ICU stay after CABG. In our CICU, POAF is considered as an indication for keeping patients in the unit.
Ventilator support of > 12 h was shown to be a predictor of prolonged ICU stay after isolated CABG in this study cohort. Many studies [22, 23] have published similar results. Prolonged ventilatory support may reflect poor lung function before surgery or a complicated course intra- or postoperatively.
Despite numerous preventive measures, pneumonia remains the most common major infection after cardiac surgery. It is associated with high mortality and morbidity and length of stay in the ICU as evidenced in many studies [24]. In this study, postoperative pneumonia was shown to strongly predict postoperative ICU stay. Pneumonia may prolong the time of ventilation or even mandate reintubation of these patients, which may prolong their stay in the CICU.
In this study, patients who did not use beta-blockers before surgery stayed in the ICU longer than those who used them preoperatively. This might be due to the fact that B-blockers decrease POAF [25] which, as discussed earlier, can prolong stay in the ICU after CABG. Patients who did not use beta-blockers were those who underwent urgent or emergency surgery with no time period between diagnosis and surgery; therefore, the prolongation might be due to this factor. In our ICU, beta-blockers were started or resumed the day after surgery in all patients, except those who were on beta-agonist inotropes.
Female gender was found by some researches to be a risk factor for prolonged stay in the CICU after CABG [26]. In our study, this result was not repeated. It could be due to differences in risk factors for this cohort.
Hypertension, DM, dyslipidemia and smoking [27, 28] have not been associated with a prolonged LOS in patients undergoing CABG, which was also observed in our results. Other study [26] found that smoking is a predictor of prolonged stay in the CICU.
Through its activating effect on the complement system and release of cytokines, blood transfusions can cause lung problems and increase the incidence of lung infection and so increases the mortality and morbidity rates and consequently the length of CICU stay after CABG. Cardiopulmonary bypass machine is known to reduce total peripheral resistance specially if used for long times which usually needs prolonged use of vasopressors to treat it. This adds to the duration of stay in the ICU after cardiac surgeries [12]. In our study, neither intraoperative blood transfusion nor prolonged CPB time were associated with prolonged stay in the CICU.
Studying the factors that affect the length of stay in the ICU aims to highlight the importance of reducing or eliminating them to reduce the duration of ICU stay, thus reducing costs and increasing the availability of beds for patients who need them.
Limitations of the study
This was a retrospective study. It was done over a long time and by many surgeons in a relatively small sized center, all these limitations make drawing solid universal conclusions difficult. However, we have presented our center’s results and, to our knowledge, this is the first report from Jordan to discuss this issue. A larger prospective multicenter study is required to confirm these findings.
Conclusion
CICUs management is a continuation of pre- and intraoperative care management, and the length of stay is usually determined by complications that reflect events occurring in the pre- or intra- operative era. Our results showed that LA diameter > 4 cm, patients who did not take beta-blockers before, patients on ventilation support > 12 h, patients who developed pneumonia postoperatively, and patients who developed post-operative atrial fibrillation were more likely to stay for > 3 nights in the ICU after CABG. Efforts should be made to reduce these postoperative complications to reduce the duration of ICU stay, thereby reducing costs and improving bed availability.
Availability of data and materials
Available upon request.
Abbreviations
- CABG:
-
Coronary artery bypass grafting
- ICU:
-
Intensive care unit
- AKI:
-
Acute kidney injury
- BMI:
-
Body mass index
- LA:
-
Left atrium
- AOR:
-
Adjusted odds ratio
- HF:
-
Heart failure
- EF:
-
Ejection fraction
- LVEF:
-
Left ventricular ejection fraction
- LIMA:
-
Left internal mammary artery
- LAD:
-
Left anterior descending
- CAD:
-
Coronary artery disease
- ACE-i:
-
Angiotensin-converting enzyme inhibitor
- ET-1:
-
Endothelin 1
- IRB:
-
Institutional Research Board
References
Velazquez EJ, Lee KL, Jones RH, Al-Khalidi HR, Hill JA, Panza JA, Michler RE, Bonow RO, Doenst T, Petrie MC, Oh JK, She L, Moore VL, Desvigne-Nickens P, Sopko G, Rouleau JL, Investigators STICHES. Coronary-artery bypass surgery in patients with ischemic cardiomyopathy. N Engl J Med. 2016;74(16):1511–20.
Okrainec K, Banerjee DK, Eisenberg MJ. Coronary artery disease in the developing world. Am Heart. 2004;148:7–15.
Sá MP, Soares EF, Santos CA, Figueredo OJ, Lima RO, Escobar RR, Silva FP, Lima Rde C. EuroSCORE and mortality in coronary artery bypass graft surgery at pernambuco cardiologic emergency medical services [pronto socorro cardiologico de pernambuco]. Rev Bras Cir Cardiovasc. 2010;25:474–82.
Seccareccia F, Perucci CA, D’Errigo P, Arcà M, Fusco D, Rosato S, Greco D, Research Group of the Italian CABG Outcome. The Italian CABG outcome study: short-term outcomes in patients with coronary artery bypass graft surgery. Eur J Cardiothorac Surg. 2006;29:56–62 (discussion 62-4).
Shroyer AL, Coombs LP, Peterson ED, Eiken MC, DeLong ER, Chen A, Ferguson TB Jr, Grover FL, Edwards FH, Society of Thoracic Surgeons. The Society of thoracic surgeons: 30-day operative mortality and morbidity risk models. Ann Thorac Surg. 2003;75:1856–64 (discussion 64-5).
AlWaqfi N, Khader Y, Ibrahim K. Coronary artery bypass: predictors of 30-day operative mortality in Jordanians. Asian Cardiovasc Thorac Ann. 2012;20(3):245–51.
Almashrafi A, Elmontsri M, Aylin P. Systematic review of factors influencing length of stay in ICU after adult cardiac surgery. BMC Health Serv Res. 2016;16:318.
Bazzoli GJ, Brewster LR, May JH, Kuo S. The transition from excess capacity to strained capacity in US hospitals. Milbank Q. 2006;84(2):273–304.
Nakasuji M, Matsushita M, Asada A. Risk factors for prolonged ICU stay in patients following coronary artery bypass grafting with a long duration of cardiopulmonary bypass. J Anesth. 2005;19:118–23.
Tu JV, Jaglal SB, Naylor CD. Multicenter validation of a risk index for mortality, intensive care unit stay, and overall hospital length of stay after cardiac surgery. Circulation. 1995;91:677–84.
Michalopoulos A, Tzelepis G, Pavlides G, Kriaras J, Dafni U, Geroulanos S. Determinants of duration of ICU stay after coronary artery bypass graft surgery. Br J Anaesth. 1996;77:208–12.
Azarfarin R, Ashouri N, Totonchi Z, Bakhshandeh H, Yaghoubi A. Factors influencing prolonged ICU stay after open heart surgery. Res Cardiovasc Med. 2014;3(4):e20159.
Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, White HD. Executive group on behalf of the Joint European Society of cardiology (ESC)/American college of cardiology (ACC)/American heart association (AHA)/world heart federation (WHF) task force for the universal definition of myocardial infarction. J Am Coll Cardiol. 2018;72(18):2231–64.
Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, Caforio ALP, Crea F, Goudevenos JA, Halvorsen S, Hindricks G, Kastrati A, Lenzen MJ, Prescott E, Roffi M, Valgimigli M, Varenhorst C, Vranckx P, Widimský P. ESC scientific document group 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European society of cardiology (ESC). Eur Heart J. 2018;39(2):119–77.
Hillis LD, Smith PK, Anderson JL, Bittl JA, Bridges CR, Byrne JG, Cigarroa JE, Disesa VJ, Hiratzka LF, Hutter AM Jr, Jessen ME, Keeley EC, Lahey SJ, Lange RA, London MJ, Mack MJ, Patel MR, Puskas JD, Sabik JF, Selnes O, Shahian DM, Trost JC, Winniford MD. 2011 ACCF/AHA guideline for coronary artery bypass graft surgery: executive summary: a report of the American college of cardiology foundation/American heart association task force on practice guidelines. Circulation. 2011;124:2610–42.
Eagle KA, Guyton RA, Davidoff R, Edwards FH, Ewy GA, Gardner TJ, Hart JC, Herrmann HC, Hillis LD, Hutter AM Jr, Lytle BW, Marlow RA, Nugent WC, Orszulak TA. ACC/AHA 2004 guideline update for coronary artery bypass graft surgery: a report of the American college of cardiology/American Heart association task force on practice guidelines (committee to update the 1999 guidelines for coronary artery bypass graft surgery). American college of cardiology; American heart association. Circulation. 2004;110(14):e340-437.
Levine GN, Bates ER, Bittl JA, Brindis RG, Fihn SD, Fleisher LA, Granger CB, Lange RA, Mack MJ, Mauri L, Mehran R, Mukherjee D, Newby LK, O’Gara PT, Sabatine MS, Smith PK. Smith SC 2016 ACC/AHA guideline focused update on duration of dual antiplatelet therapy in patients with coronary artery disease: a report of the american college of cardiology/American heart association task force on clinical practice guidelines: an update of the 2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention, 2011 ACCF/AHA guidelinefor coronary artery bypass graft surgery, 2012 ACC/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease, 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction, 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes, and 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery. Circulation. 2016;134(10):e123–55.
Ibrahim KS, Mayyas FA, Kheirallah K, AlWaqfi NR, Van Wagoner DR. Is left atrial size a predictor of mortality after coronary artery bypass surgery? A single center study. Acta Cardiol Sin. 2017;33(2):195–203.
Ibrahim KS, Kheirallah KA, Megdadi MA. Enlargement of the Left atrium strongly predicts postoperative mortality following heart valve surgery. Vasc Health Risk Manag. 2022;18:783–91.
Yu-qi Wu, Min Yu, Yu-lin Zhang, Min Qian, Xin-li Zhang, Chao Yu, Chang-yun Guo, Rui Huang (2013). Cause analysis of prolonged intensive care unit stay after coronary artery bypass grafting Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 25(2):109–111.
Borzak S, Tisdale JE, Amin NB, Goldberg AD, Frank D, Padhi ID, Higgins RS. Atrial fibrillation after bypass surgery: Does the arrhythmia or the characteristics of the patients prolong hospital stay? Chest. 1998;113(6):1489–91.
Zhang X, Zhang W, Lou H, Luo C, Du Q, Meng Y, Wu X, Zhang M. Risk factors for prolonged intensive care unit stays in patients after cardiac surgery with cardiopulmonary bypass: a retrospective observational study. Int J Nurs Sci. 2021;8(4):388–93.
Meziane M, Koundi A, Meskine A, Bensghir M, Hatim A, Ahtil R. Predictors of prolonged ICU stay following elective adult cardiac surgery:monocentric retrospective study on 5 and half years. Ann Cardiol Angeiol [Paris]. 2017;66(2):66–73.
Ailawadi G, Chang HL, O’Gara PT, O’Sullivan K, Woo YJ, Derose JJ Jr, Parides MK, Thourani VH, Robichaud S, Gillinov AM, Taddei-Peters WC. Pneumonia after cardiac surgery: experience of the national institutes of health/canadian institutes of health research cardiothoracic surgical trials network. J Thorac Cardiovasc Surg. 2017;153(6):1384–91.
Osmanovic E, Ostojic M, Avdic S, Djedovic S, Delic A, Kadric N, Terzic A, Avdic-Salihovic A. Pharmacological prophylaxis of atrial fibrillation after surgical myocardial revascularization. Med Arch. 2019;73(1):19–22.
Kao KD, Lee SYKC, Liu CY, Chou NK. Risk factors associated with longer stays in cardiovascular surgical intensive care unit after CABG. J Formos Med Assoc. 2022;121(1):304–13.
Gumus F, Polat A, Yektas A, Totoz T, Bagci M, Erentug V, et al. Prolonged Mechanical ventilation after CABG: risk factor analysis. J Cardiothorac Vasc Anesth. 2015;29(1):52–8.
Piotto RF, Ferreira FB, Colósimo FC, Silva GS, Sousa AG, Braile DM. Fatores preditores independentes de ventilação mecânica prolongada em pacientes submetidos à cirurgia de revascularização miocárdica. Braz J Cardiovasc Surg. 2012;27(4):520–8.
Acknowledgements
None
Funding
NA.
Author information
Authors and Affiliations
Contributions
All authors have contributed sufficiently. KSI: Concept, methods, manuscript writing, final version, and submission. KAK and MAM: Statistical analysis, writing the statistical notes, and preparing the tables. The final version was revised accordingly. ARAM: Concept, data collection, writing, and revision of the final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Approved by the Institutional Review Board at Jordan University of Science and Technology and King Abdullah University Hospital.
Competing interests
The authors have no conflicts of interest to declare.
Informed consent/consent to publish
Waived by IRB.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ibrahim, K.S., Kheirallah, K.A., Al Manasra, A.R.A. et al. Factors affecting duration of stay in the intensive care unit after coronary artery bypass surgery and its impact on in-hospital mortality: a retrospective study. J Cardiothorac Surg 19, 45 (2024). https://doi.org/10.1186/s13019-024-02527-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13019-024-02527-y