Abstract
Background
Previous observational studies have highlighted potential relationships between the telomerase reverse transcriptase (TERT) gene, short leukocyte telomere length (LTL), and cerebrovascular disease. However, it remains to be established as to whether TERT gene variants are associated with an elevated risk of cerebral small vessel disease (CSVD), and whether there is a causal relationship between LTL and CSVD.
Methods
Five TERT single nucleotide polymorphisms (SNPs) were analyzed in 307 CSVD patients and 320 healthy controls in whom LTL values were quantified. Allele models and four genetic models were used to explore the relationship between these SNP genotypes and CSVD risk. A Mendelian randomization analysis of CSVD risk was then performed using LTL-related SNPs and the polygenic risk score (PRS) constructed from these SNPs as genetic instrumental variables to predict the causal relationship between LTL and CSVD risk.
Results
Model association analyses identified two SNPs that were significantly associated with CSVD risk. LTL was significantly correlated with age (P < 0.001), and the MR analysis revealed an association between short LTL and an elevated risk of CSVD. PRS-based genetic prediction of short LTLs was also significantly related to an elevated CSVD risk.
Conclusion
Multiple genetic models and MR results indicate that TERT gene SNPs may be related to an elevated risk of CSVD, and that shorter LTL may be causally linked to such CSVD risk.
Similar content being viewed by others
Introduction
Cerebral small vessel disease (CSVD) refers to a common group of cerebrovascular diseases exhibiting varying imaging features [1]. Prior evidence suggests that CSVD is a complex polygenetic disease influenced by several risk factors, yet the precise genetic basis for CSVD risk remains to be fully elucidated [2, 3].
The telomerase reverse transcriptase functions to continuously extend or maintain the length of telomeres in response to activation by a telomerase RNA template. Components of the telomerase complex include telomerase-associated protein, telomerase reverse transcriptase (TERT), and telomerase RNA component. Of these, TERT is an essential regulator of telomerase activity [4, 5], and observational analyses suggest that TERT gene variants are related to ischemic stroke (IS) risk [6]. We thus hypothesized that TERT gene variants may also be associated with patient susceptibility to CSVD.
Leukocyte telomere length (LTL) has long been analyzed as an aging-related biomarker [7]. Several single nucleotide polymorphisms (SNPs) proximal to the TERT gene have been reported to be associated with LTL, but whether these TERT variants play any functional role in disease pathogenesis remains uncertain [8, 9]. While IS risk has been linked with LTL shortening, no similar evidence regarding a link between LTL and CSVD risk has been published to date. Traditional observational studies are limited in their ability to assess causal relationships between LTL and CSVD owing to bias stemming from the inability to fully control for confounding variables, reverse causality, minor exposure factors, and multiple testing. To address these issues, epidemiological research has increasingly employed Mendelian randomization (MR) studies in which select genetic mutations are treated as instrumental variables (IVs). While MR studies of the causal relationship between LTL and several diseases have been performed in recent years, there have not been any specific MR analyses of the interplay between LTL and CSVD risk [10, 11].
Here, an MR approach was used to explore the relationship between TERT gene variants, LTL, and CSVD by correcting for confounding factors and other biases. These efforts and a further exploration of the causal effect of LTL on CSVD incidence offer a new foundation for assessing CSVD risk.
Materials and methods
Study population
In total, 307 consecutive CVSD patients 45–75 years old that were admitted to the outpatient department and wards of the Liaoning Provincial People’s Hospital between October 2018 and August 2020 whose CVSD diagnosis was consistent with the 2021 Chinese Consensus for the Diagnosis and Treatment of Cerebral Small Vascular Diseases were enrolled in this study. In addition, 320 healthy controls were recruited. All participants were unrelated individuals of Han ethnicity. This study was carried out in accordance with the Helsinki Declaration and approved by the Ethics Committee of Liaoning Provincial People’s Hospital (No. (2021)HS007). Participants gave informed consent to participate in the study before taking part.
All subjects signed the informed consent form. The specific research process is illustrated in Fig. 1.
Inclusion criteria: (1) residents of Liaoning Province for ≥ 30 years; (2) 45–75 years old; (3) unrelated to other enrolled patients; (4) confirmed CSVD diagnosis as per the “China Consensus on Diagnosis and Treatment of Cerebral Small Vascular Diseases” (2021), with typical imaging findings and consistent acute or subacute clinical manifestations.
Exclusion criteria: (1) atherosclerotic thrombosis, or a history of transient ischemic attack (TIA) or intracranial hemorrhage; (2) cervical vascular ultrasound or head MRA results consistent with the moderate-to-severe occlusion or stenosis of vessels in the head and neck; (3) other neurological diseases including epilepsy, multiple sclerosis, hydrocephalus, or intracranial infectious diseases; (4) white matter lesions of known etiology, including neurosyphilis, carbon monoxide positioning, or degenerative disease; (5) history of serious heart diseases including coronary heart disease, atrial fibrillation, myocardial infarction within the past 6 months, or heart failure; (6) severe liver and kidney diseases or malignant tumors; (7) severe coagulation disorders or active bleeding.
Data collection
Medical records or in-person questionnaires were used to collect data including age, sex, height, weight, systolic blood pressure (SBP), diastolic blood pressure, smoking history, alcohol consumption, and history of physical activity from all participants. Standard methods were used to analyze laboratory parameters including levels of fasting blood glucose, triglycerides, total cholesterol, high-density lipoprotein cholesterol, low-density lipoprotein cholesterol (LDL-C), and homocysteine (Hcy) in the clinical laboratory of Liaoning Provincial People’s Hospital. Both cases and controls underwent TERT genotyping and LTL measurements.
SNP selection and genotyping
Five SNPs with a minor allele frequency ≥ 5% were selected based on the GWAS database (https://www.ebi.ac.uk/gwas) and published research: rs2853676, rs2242652, rs2075786, rs2736100, rs2736122. Fasting venous blood (3 mL) was collected from all subjects in EDTA-containing tubes. Shanghai Sangon Company extracted whole genomic DNA from these samples and synthesized appropriate SNP locus primers. DNA amplification was performed with the following settings: 95 °C for 5 min; 38 cycles of 94 °C for 30 s, 58 °C for 30 s, and 72 °C for 60 s; 72 °C for 10 min. Then, 1% agarose gel electrophoresis (10–20 min, 150 V, 100 mA) was used to separate 5 µl of amplified DNA per sample, followed by visualization with a UV gel imaging system. A3730XL sequencer (ABI Company, US) was then used to sequence these amplified samples for genotyping.
LTL measurements
A qPCR approach was used to measure LTL using the following primers (5’-3’) specific for the human telomere and β-globin genes:
TEL (forward): GGTTTTTGAGGGTGAGGGTGAGGGTGAGGGTGAGGGT;
TEL (reverse): TCCCGACTATCCCTATCCCTATCCCTATCCCTATCCCTA;
HBG1 (forward): TCTGACACAACTGTGTTCACTAGC;
HBG1 (reverse): CACCAACTTCATCCACGTTCACC.
Cycle threshold (Ct) values were used to establish a standard curve as follows: T/S = [2 Ct (telomeres) / 2 Ct (single copy gene)] − 1 = Δ Ct, Δ Ct 1 T/S ratio for each sample, Δ Ct 2 T/S ratio for the reference gene; Δ Δ Ct = Δ Ct1 - Δ Ct 2, with the relative T/S ratio 2 − Δ Δ Ct representing relative LTL length.
Statistical analysis
Data were analyzed with SPSS 26.0, R 4.0.3, and Stata 11. Normally distributed data are given as means ± standard deviation, whereas they were otherwise reported as medians. Qualitative data are reported as rates (%). Results were compared with independent sample t-tests of Fisher’s exact test, with Bonferroni correction for subsequent pairwise comparisons. The χ2 test was used to evaluate the Hardy-Weinberg equilibrium (HWE) of genotype distributions between the control and case groups. CSVD risk and associated 95% confidence interval (CI) values were estimated through a multivariate logistic regression analysis, with P < 0.05 as the significance threshold. Linkage disequilibrium analyses were performed with Haploview 4.2 (https://www.broadinstitute.org/Haploview), and SNP genetic correlation analysis modeling was performed using SNPStats (https://www.snpstats.net/start.htm).
A one-sample MR analysis was performed, with SNPs and telomere length-related PRS values being selected as IVs if they satisfied the following criteria: (1) selected SNPs were correlated with LTL; (2) the correlation between SNPs, LTL, and CSVD was not affected by confounding factors; (3) selected SNPs only affected CSVD via LTL and not via an alternative pathway. Direct correlation and causal relationships between LTL and CSVD were obtained with a two-stage least square regression model (2SLS) after eliminating confounders and reverse causality, after which the following were performed:
Step 1: Establish a G-X regression model to obtain the predicted value (P) for exposure factors.
Step 2: Construct a P-Y regression model, and derive the regression equation for the relationship between the predicted value of exposure factors P and outcome variable Y.
Quantitative estimates of the magnitude of the relationship between LTL and CSVD were made with a logistic regression model (θx = logOR), using P < 0.05 as the threshold for significance.
Results
Participant characteristics
This study enrolled 307 CSVD patients (156 female, 151 male; mean age 60.98 ± 8.165 years) and 320 healthy controls (148 female, 172 male; mean age 61.45 ± 8.280 years). CSVD patients exhibited significantly higher mean age, weight, body mass index (BMI) smoking status, blood pressure, blood glucose, LDL-C, and Hcy levels relative to controls (P < 0.05), whereas gender, height, triglyceride levels, cholesterol levels, physical activity, and alcohol consumption were comparable in these groups (Table 1).
Linkage disequilibrium analysis
Linkage disequilibrium refers to the non-random association of different alleles in a population. Linkage disequilibrium analyses of these five SNPs did not reveal the formation of a haplotype block, and there was no evidence of strong linkage disequilibrium (Fig. 2).
Relationship between SNPs and CSVD susceptibility
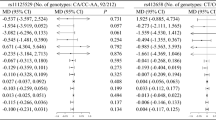
The relationship between individual SNPs and CSVD risk was next assessed. Using an allele model, the frequencies of the TERT rs2853676 and rs2075786 alleles differed significantly between CSVD patients and controls (OR = 1.43, 95%CI: 1.09–1.89, P = 0.001, and OR = 1.37, 95%CI: 1.09–1.73, P = 0.006 for the rs2853676 and rs2075786 allele, respectively). None of the analyzed SNPs deviated from the HWE in the control group (Table 2).
The relationship between TERT gene polymorphisms and CSVD risk was further assessed using various genetic models (Table 3). Elevated CSVD risk was related to the rs2853676 C/T genotype under the codominant model (OR = 1.65, 95% CI: 1.11–2.43; P = 0.018), and the C/T and T/T genotypes under the dominant model (OR = 1.69, 95% CI: 1.17 to 2.46; P = 0.005) and log-additive model (OR = 1.53, 95% CI: 1.13–2.08; P = 0.006). Similarly, higher CSVD risk was related to the rs2075786 A/A genotype under the codominant model (OR = 2.01, 95% CI: 1.15–3.52; P = 0.021), and to the A/G and A/A genotypes under the dominant model (OR = 1.61, 95%CI: 1.12–2.33; P = 0.010) and log-additive model (OR = 1.44, 95% CI: 1.11–1.88; P = 0.006). For the rs2853676 SNP, higher CSVD risk was associated with the C/T genotype under the overdominant model (OR = 1.57, 95% CI: 1.07–2.31; P = 0.022), as was the rs2075786 A/G genotype under the co-dominant model (OR = 1.52, 95% CI: 1.03–2.23; P = 0.021) and rs2736122 with the A/G genotype under the overdominance model (OR = 0.59, 95% CI: 0.36–0.98; P = 0.042) after strictly adjusting for age, sex, BMI, smoking history, and alcohol consumption history.
Analyses of LTL in cases and control
LTL was negatively correlated with age in both the cases and controls (P < 0.001, Fig. 3A), with significantly different respective LTL values of 1.278 ± 0.634 and 1.492 ± 0.618 in these two groups (P < 0.001, Fig. 3B). No significant difference between the average LTL of males (1.405 ± 0.631; n = 323) and females (1.368 ± 0.638; n = 304) was observed (P = 0.463). However, CSVD patients exhibited a shorter LTL than controls among both males and females (males: 1.258 ± 0.621 vs. 1.534 ± 0.641, P < 0.001; females: 1.297 ± 0.649 vs. 1.442 ± 0.62, P = 0.048, Fig. 3B). Given the observed relationships between the rs2853786 and rs2075676 alleles in the TERT gene and CSVD risk, LTL was next compared for different genotypes in both the case and control populations. The respective LTL values for the rs2853786 C/C, C/T and T/T genotypes in the case group were 1.385 ± 0.669, 1.054 ± 0.510, and 1.427 ± 0.595 (P < 0.001), while those in controls were 1.577 ± 0.614, 1.283 ± 0.580, and 1.404 ± 0.632, respectively (P = 0.001, Fig. 3C). The LTL values associated with the rs2075786 A/A, A/G, and G/G genotypes among cases were 0.680 ± 0.357, 1.370 ± 0.620, and 1.433 ± 0.597, respectively (P < 0.001), while those for controls were 0.773 ± 0.394, 1.554 ± 0.550, and 1.603 ± 0.620, respectively (P < 0.001, Fig. 3D).
Estimates of the relationship between individual SNPs and LTL, and instrumental variable selection
Correlations between individual SNPs, CSVD, and LTL are summarized in Table 4. Following Bonferroni adjustment for age, sex, BMI, smoking history, and alcohol consumption history, three SNPs were significantly correlated with LTL (rs2853676, P = 1.09 × 10− 5; rs2242652, P = 1.38 × 10− 4; rs2075786, P = 7.12 × 10 − 21). These results, together with the genetic model analyses performed above, led to the selection of rs2853676 and rs2075786 for further analyses examining associations between genotype and potential confounding factors (Fig. 4A-B). These analyses revealed no correlation between genotype and age, height, weight BMI, blood lipids, Hcy, or other analyzed risk factors (P > 0.05), although SBP did differ among rs2075786 genotypes (P = 0.037). This may be due to the limited sample size, which precluded the simultaneous satisfaction of multiple independent hypotheses. Accordingly, rs2853676, rs2242652, and rs2075786 were selected as IVs for a subsequent MR analysis.
Mendelian randomization analysis of the link between LTL and CSVD
The causal effects of LTL on CSVD were assessed using a one-sample MR approach using a 2SLS. A PRS for telomere length was constructed from rs2853676, rs2242652, and rs2075786, and this PRS as well as the three individual SNPs were selected as IVs. Following Bonferroni correction, LTL values for different rs2853676 and rs2075786 genotypes remained strongly correlated with CSVD (Table 5). LTL was also significantly negatively correlated with the PRS (Beta = 0.991, P < 2 × 10− 16), while the PRS was significantly correlated with CSVD (Beta= -1.207, P = 1.84 × 10− 4). No significant confounding relationship was detected when exploring associations between the PRS and CSVD-associated risk factors, although LDL-C levels were related to the PRS (Beta = 0.419, P = 0.005, Table 6). Even so, following Bonferroni adjustment for LDL-C, a significant association between LTL and PRS remained evident (Beta =-1.066, P = 0.001). These results suggested that short LTL may have a causal impact on CSVD incidence. Leave-one-out sensitivity testing was used to confirm the accuracy of these results, with correlation analyses revealing that a significant correlation between IVs and CSVD remained present under these conditions, supporting the causal link between LTL and CSVD (Table 5; Fig. 5C).
A: Scatterplot of the association of SNPs with LTL and CSVD risk; Each point in the scatter plot represents an instrumental variable. The vertical and horizontal black lines show the 95% CI for each SNP, with the horizontal axis illustrating the effect of the SNP on the exposure (telomere length), and the vertical axis highlighting the effect of the SNP on outcome (cerebrovascular disease), while the solid blue line shows the MR fitting results. B: Forest diagram of the risk relationship between LTL and CSVD, showing the odds ratio (OR), with the horizontal line representing the 95%CI of the risk of CSVD occurring in LTL-associated SNPs. The red line illustrates that shortening of LTLs increases the risk of CSVD. C: The sensitivity analysis of MR results was carried out by removing SNPs one by one
Discussion
The present case-control study was constructed as the first analysis of the associations between SNPs in the TERT gene, LTL, and the risk of CSVD. LTL-associated SNPs were used as IVs for a one-sample MR analysis supplemented by the PRS method to fully explore potential causal relationships between LTL and CSVD. Five SNPs exhibiting a MAF greater than 5% were selected to ensure that these analyses were sufficiently powered. In the Chinese Han population, these analyses revealed a significant relationship between TERT gene variants and CSVD susceptibility, supporting a causal association between LTL and CSVD. These findings support the hypothesis that the TERT gene may contribute to elevated CSVD risk through LTL shortening.
Major pathogenic factors involved in the development of CSVD are thought to include inflammation, poor blood perfusion, blood-brain barrier impairment, and genetic susceptibility [12, 13]. In line with prior reports, CSVD risk was herein found to be associated with age, BMI, hypertension, hyperglycemia, dyslipidemia, smoking, and Hcy levels [12, 13]. Males have also been suggested to be at a higher risk of CSVD than females, potentially owing to sex-related differences in exposure to risk factors including smoking and drinking. The present results do not support a role for sex as a CSVD-related risk factor, although the limited study sample size limits further analyses of this relationship. In our study, we performed a correlation analysis of confounding risk factors associated with PRS and CSVD, the results showed that only LDL was associated with constructed PRS (Beta = 0.419, P = 0.005). After Bonferroni correction for LDL, we found that LTL and PRS were still statistically significant (Beta = -1.066, P = 0.001). Therefore, although there were differences in baseline data between the case and control groups, genetic factors were significantly associated with the development of LTL and CSVD.
TERT expression plays a key role in regulating telomerase activity [14]. Few studies to date, however, have assessed correlations between TERT polymorphisms and cerebrovascular diseases, and studies that have been completed have yielded inconsistent results among populations of different ethnicities. The ARIC study of 15,792 IS patients revealed an association between TERT gene polymorphisms and IS risk among African Americans, but found that this relationship was weaker when the regression model incorporated hypertension, diabetes, BMI, and smoking history in the regression model. Among Caucasians, no such link between TERT gene polymorphisms and IS risk has been observed [15]. In the population-based GWAS study by Wei et al. [16] the TERT rs2736100 SNP was reportedly significantly associated with LTL, while another report indicated that the TERT C and G alleles of the rs2853691 and rs33954691 genotypes were associated with shorter LTL. When studying TERT polymorphisms in the Chinese population, Zhang et al. [6]. found that the TERT rs224652 G/A (superdominant model) and A/A (dominant model) genotypes were associated with elevated IS risk. In our initial genetic analyses, TERT rs2242652 genotypes were not significantly correlated with CSVD but were significantly correlated with LTL (Beta=-0.168, Se = 0.044, P = 1.38 × 10− 4). In a study of African Americans, Bresler et al. [15]. found a significant association between the additive model of rs2853668 and ischemic stroke (HRR = 1.17, p = 0.05, 95% CI = 1.00–1.38).Han et al. [17] showed that the T/G and G/G genotypes of rs2736100 and the G/A and A/A genotypes of rs2853676 were associated with stroke risk (P < 0.05).This study was the first to assess the link between TERT SNPs and CSVD risk, ultimately revealing that rs2853676 and rs2075786 were significantly associated with CSVD even following Bonferroni correction. The rs2853676 C/T (co-dominant model) and C/T and T/T (dominant model and logarithmic additive model) genotypes were significantly associated with CSVD risk. Moreover, the rs2075786 A/A (co-dominant model) and A/G and A/A (dominant model and logarithmic additive model) genotypes were associated with elevated CSVD risk. Additionally, the rs2853676 C/T genotype (overdominant model), the rs2075786 A/G genotype (co-dominant model), and the rs2736122 A/G genotype (overdominant model) were significantly related to CSVD risk following strict adjustment for age, sex, BMI, smoking history, and alcohol consumption history. The level of significance declined following the correction of the logarithmic additive model for rs2736100, potentially indicating that rs2736100 may be correlated with the risk of CSVD but that further large-scale prospective analyses will be necessary to explore this possibility.
While prior evidence supports a correlative relationship between LTL and cerebrovascular disease risk, large-scale multi-center studies are lacking, and reported results have not been consistent. Gao et al. [18]. observed a significant correlation between LTL and age in a Chinese Han population (P < 0.001), and found shorter LTL to be associated with a higher risk of IS (OR = 8.44, 95%CI: 5.42–13.14, P < 0.001). This correlation between LTL shortening and IS risk was also supported by a meta-analysis of 11 studies [19]. When comparing stroke patients and controls (n = 1309 each), Ding et al. [20]. similarly observed a higher risk of IS among individuals with the shortest LTL relative to those with the longest LTL (OR = 2.12, 95%CI: 1.62–2.77). In contrast, Luo et al. [21]. reported detecting significantly longer LTL values in there is case group relative to their control and high-risk groups, whereas high-risk patients exhibited significantly shorter LTL as compared to controls, suggesting that the correlative relationship between LTL and IS risk may be U-shaped. Moreover, one 29-year Danish cohort study found that LTL was unrelated to IS incidence [22], and a 10-year prospective analysis conducted in the USA observed a positive correlation between shorter telomere length and stroke risk among individuals 65–73 years of age but not in individuals > 73 years old [23]. In the present case-control study, LTL-associated SNPs and PRSs constructed from these SNPs were used as instrumental variables in a one-sample MR analysis exploring the predicted association between LTL and CSVD risk. The results indicated that shorter LTL was associated with an elevated risk of CSVD. These findings align well well two recent GWAS data-based MR studies surveying a range of diseases that identified a possible causal relationship between short LTL and small vessel stroke (OR = 0.72, 95% CI: 0.54–0.97, P = 0.028) [24, 25]. Our results further suggest that LTL may be related to small cerebral vascular lesions.
In traditional observational studies, disease or treatment-related processes have the potential to contribute to LTL shortening, and both LTL and disease risk may be influenced by environmental variables. Under these conditions, establishing causality is challenging. This study exhibits several advantages including the use of a one-sample MR method and supporting sensitivity analyses of possible pluripotency effects, thereby mitigating potential bias stemming from the inability to fully control for confounding factors, reverse causality, minor exposure factors, and multiple testing. This is also the first MR study to explore the causal relationship between LTL and CSVD, as this association was not examined in prior analyses of the interplay between LTL and cerebrovascular disease.
This study is subject to some limitations. For one, the sample size was relatively small relative to other MR studies, increasing the potential risk of type II error. The data used in this study are primarily based on Han Chinese patients, and there is no evidence of a causal relationship between LTL and CSVD in other ethnic populations, so the generalization of our findings to other ethnic groups may be limited.Further studies analyzing representative regional and ethnic populations will thus be necessary to validate these results, together with large-scale multicenter prospective analyses. Second, genetic variation is utilized as an instrumental variable in MR studies to satisfy the required assumptions. As the total elimination of potential confounding factors from MR methods remains challenging, however, it remains possible that the present results are subject to bias from pluripotency effects not identified at present. Many studies have shown that the construction of SNP-related PRSs can predict individualized disease risk, particularly in high-risk populations such as advanced age, hypertension, hyperglycemia, dyslipidemia, smoking, and high Hcy levels [26, 27]. However, other studies have shown that the PRS model is only slightly or not statistically significant compared to the traditional model [28]. The reason for the limited predictive power of the PRS may be related to genetic and environmental factors, as well as the multiple pathogenic mechanisms of the disease. In addition, poor predictive power may also be related to modeling algorithms. In the field of forecasting, the PRS model has also been studied by using machine algorithms, and good prediction efficiency has been achieved [29, 30]. Therefore, optimization algorithms and new machine algorithms can be considered in the future to improve the prediction ability of PRS models.
This study also included a relatively limited number of SNPs, reducing overall MR analysis accuracy such that weaker associations may have been missed. Further studies exploring the causal link between genetic predictors of LTL and CSVD risk that incorporate other LTL-related SNPs will thus be necessary to increase the overall power of these analyses and to further mitigate potential confounding variables. Large-scale analyses will also be vital to fully explore the association between LTL and other CSVD subtypes.
Conclusion
In summary, based on analyses of multiple genetic models and MR methods using LTL-related SNPs as instrumental variables, these results suggest that TERT gene variants can contribute to an elevated risk of CSVD, and that shorter LTL may represent a causal factor for CSVD. Owing to the limited sample size in this study, however, additional MR studies utilizing GWAS or individual data will be essential to fully clarify the nature of this potential causal association.
Data availability
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
Abbreviations
- TERT:
-
Telomerase reverse transcriptase gene
- LTL:
-
Leukocyte telomere length
- CSVD:
-
Cerebral small vessel disease
- SNPs:
-
Single nucleotide polymorphisms
- MR analysis:
-
Mendelian randomization analysis
- PRS:
-
Polygenic risk score
- IVs:
-
Instrumental variables
- SBP:
-
Systolic blood pressure
- LDL-C:
-
Low-density lipoprotein cholesterol
- Hcy:
-
Homocysteine
- 95% CI:
-
95% Confidence interval
- BMI:
-
Body mass index
- 2SLS:
-
Two-stage least square regression model
References
Litak J, Mazurek M, Kulesza B, Szmygin P, Litak J, Kamieniak P, Grochowski C. Cerebral small Vessel Disease. Int J Mol Sci. 2020;21(24):9729.
Cannistraro R, Badi M, Eidelman B, Dickson D, Middlebrooks E, Meschia J. CNS small vessel disease: a clinical review. Neurology. 2019;92:1146–56.
Søndergaard C, Nielsen J, Hansen C, Christensen H. Hereditary cerebral small vessel disease and stroke. Clin Neurol Neurosurg. 2017;155:45–57.
Shay J, Wright W. Telomeres and telomerase: three decades of progress. Nat Rev Genet. 2019;20:299–309.
Saretzki G, Telomeres. Telomerase and ageing. Subcell Biochem. 2018;90:221–308.
Zhang S, Ji G, Liang Y, et al. Polymorphisms in Telomere Length Associated TERC and TERT predispose for ischemic stroke in a Chinese Han population. Sci Rep. 2017;7:40151.
Tian Y, Wang S, Jiao F, Kong Q, Liu C, Wu Y. Telomere length: a potential biomarker for the risk and prognosis of stroke. Front Neurol. 2019;10:624.
Heidenreich B, Kumar R. TERT promoter mutations in telomere biology. Mutat Res. 2017;771:15–31.
Barthel F, Wei W, Tang M, et al. Systematic analysis of telomere length and somatic alterations in 31 cancer types. Nat Genet. 2017;49:349–57.
Bowden J, Holmes M. Meta-analysis and mendelian randomization: a review. Res Synthesis Methods. 2019;10:486–96.
Zheng J, Baird D, Borges M, et al. Recent developments in mendelian randomization studies. Curr Epidemiol Rep. 2017;4:330–45.
Wardlaw J, Smith C, Dichgans M. Small vessel disease: mechanisms and clinical implications. Lancet Neurol. 2019;18:684–96.
Low A, Mak E, Rowe J, Markus H, O’Brien J. Inflammation and cerebral small vessel disease: a systematic review. Ageing Res Rev. 2019;53:100916.
Colebatch A, Dobrovic A, Cooper W. TERT gene: its function and dysregulation in cancer. J Clin Pathol. 2019;72:281–4.
Bressler J, Franceschini N, Demerath E, Mosley T, Folsom A, Boerwinkle E. Sequence variation in telomerase reverse transcriptase (TERT) as a determinant of risk of cardiovascular disease: the atherosclerosis risk in communities (ARIC) study. BMC Med Genet. 2015;16:52.
Wei R, DeVilbiss F, Liu W. Genetic polymorphism, Telomere Biology and Non-small Lung Cancer Risk. J Genet Genomics = Yi Chuan Xue bao. 2015;42:549–61.
Gao D, Zhang R, Ji G. Relative telomere length and stroke risk in a Chinese Han Population. J Mol Neuroscience: MN. 2018;66:475–81.
Han XD, Liang ZG, Yan ZH, Zhang HL, Zhang ZL, Qu Y. Correlation between Helicobacter pylori infection,TERT gene polymorphism and carotid atherosclerosis in patients with cerebral infarction. Chin J Nosocomiology. 2022;22:3391–6.
Jin X, Pan B, Dang X, Wu H, Xu D. Relationship between short telomere length and stroke: a meta-analysis. Medicine. 2018;97:e12489.
Ding H, Chen C, Shaffer J, et al. Telomere length and risk of stroke in Chinese. Stroke. 2012;43:658–63.
Luo D, Hou Q, Yu J, Yu D. Telomere length associated with the risks of high-risk and ischemic stroke in southern Chinese Han population. Oncotarget. 2017;8:105915–22.
Ellehoj H, Bendix L, Osler M. Leucocyte telomere length and risk of Cardiovascular Disease in a cohort of 1,397 Danish men and women. Cardiology. 2016;133:173–7.
Fitzpatrick A, Kronmal R, Gardner J, et al. Leukocyte telomere length and cardiovascular disease in the cardiovascular health study. Am J Epidemiol. 2007;165:14–21.
Cao W, Li X, Zhang X, Zhang J, Sun Q, Xu X, Sun M, Tian Q, Li Q, Wang H, Liu J, Meng X, Wu L, Song M, Hou H, Wang Y, Wang W. No Causal Effect of Telomere length on ischemic stroke and its subtypes: a mendelian randomization study. Cells. 2019;8(2):159. https://doi.org/10.3390/cells8020159.
Cao W, Zheng D, Zhang J. Association between telomere length in peripheral blood leukocytes and risk of ischemic stroke in a Han Chinese population: a linear and non-linear mendelian randomization analysis. J Translational Med. 2020;18:385.
Pulit SL, Weng LC, McArdle PF, Trinquart L, Choi SH, Mitchell BD, Rosand J, de Bakker PIW, Benjamin EJ, Ellinor PT, Kittner SJ, Lubitz SA, Anderson CD. Atrial fibrillation genetic risk differentiates cardioembolic stroke from other stroke subtypes. Neurol Genet. 2018;4(6):e293. https://doi.org/10.1212/NXG.0000000000000293.
Abraham G, Malik R, Yonova-Doing E, Salim A, Wang T, Danesh J, Butterworth AS, Howson JMM, Inouye M, Dichgans M. Genomic risk score offers predictive performance comparable to clinical risk factors for ischaemic stroke. Nat Commun. 2019;10(1):5819. https://doi.org/10.1038/s41467-019-13848-1.
Bakker MK, Kanning JP, Abraham G, Martinsen AE, Winsvold BS, Zwart JA, Bourcier R, Sawada T, Koido M, Kamatani Y, Morel S, Amouyel P, Debette S, Bijlenga P, Berrandou T, Ganesh SK, Bouatia-Naji N, Jones G, Bown M, Rinkel GJE, Veldink JH, Ruigrok YM. HUNT All-In stroke, CADISP group, International Consortium for Blood Pressure, International Headache Genetics Consortium, International Stroke Genetics Consortium (ISGC) Intracranial Aneurysm Working Group. Genetic risk score for intracranial aneurysms: prediction of subarachnoid hemorrhage and role in clinical heterogeneity. Stroke. 2023;54(3):810–8. https://doi.org/10.1161/STROKEAHA.122.040715.
Ruan Y, Lin YF, Feng YA, Chen CY, Lam M, Guo Z, Stanley Global Asia Initiatives, He L, Sawa A, Martin AR, Qin S, Huang H, Ge T. Improving polygenic prediction in ancestrally diverse populations. Nat Genet. 2022;54(5):573–80. https://doi.org/10.1038/s41588-022-01054-7.
Li J, Chaudhary DP, Khan A, Griessenauer C, Carey DJ, Zand R, Abedi V. Polygenic risk scores augment stroke subtyping. Neurol Genet. 2021;7(2):e560. https://doi.org/10.1212/NXG.0000000000000560.
Acknowledgements
The authors acknowledge all the patients and healthy subjects for their participation in this study.
Funding
This study was financially supported by Shenyang Science and Technology Bureau(No.19-1124-038),Natural Science Foundation of Liaoning Province(No.2022-MS-217),and Science and Technology Joint Project, Liaoning Province(No.2023JH2/101700098)
Author information
Authors and Affiliations
Contributions
YS contributed to data analysis and was a major contributor to writing the manuscript. JX, WG, and LY contributed to the data collection and analysis. JL and JZ conceived, designed the study, and reviewed critically the article. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study involves human participants and was approved by the Ethics Committee of Liaoning Provincial People’s Hospital (No. (2021)HS007). Participants gave informed consent to participate in the study before taking part.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Song, Y., Xu, J., Geng, W. et al. Association and causal impact of TERT genetic variants on peripheral blood leukocyte telomere length and cerebral small vessel disease risk in a Chinese Han population: a mendelian randomization analysis. Orphanet J Rare Dis 19, 309 (2024). https://doi.org/10.1186/s13023-024-03316-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13023-024-03316-5