Abstract
Background
Maternal uniparental disomy for chromosome 6 (upd(Cajaiba MM, Witchel S, Madan-Khetarpal S, Hoover J, Hoffner L, Macpherson T, et al. Prenatal diagnosis of trisomy 6 rescue resulting in paternal UPD6 with novel placental findings. Am J Med Genet Part A. 2011;155 A(8):1996–2002.)mat) has been previously reported to cause intrauterine growth restriction (IUGR), but the specific clinical phenotype has not been defined. Based on clinical data from two new cases and patients from the literature, specific phenotypes and mechanisms will be discussed further.
Case presentation
: In case 1, a maternal isodisomy mixed with a heterodisomy was found on chromosome 6, including a regional absence of heterozygosity between 6q23.3 and 6q27. In case 2, a homozygous SCUBE3 mutation and upd(Cajaiba MM, Witchel S, Madan-Khetarpal S, Hoover J, Hoffner L, Macpherson T, et al. Prenatal diagnosis of trisomy 6 rescue resulting in paternal UPD6 with novel placental findings. Am J Med Genet Part A. 2011;155 A(8):1996–2002.)mat, involving the 6p21.1-25.1 region were found. Clinical data related to upd(Cajaiba MM, Witchel S, Madan-Khetarpal S, Hoover J, Hoffner L, Macpherson T, et al. Prenatal diagnosis of trisomy 6 rescue resulting in paternal UPD6 with novel placental findings. Am J Med Genet Part A. 2011;155 A(8):1996–2002.)mat were also reviewed. Of all the 21 reported cases with upd(Cajaiba MM, Witchel S, Madan-Khetarpal S, Hoover J, Hoffner L, Macpherson T, et al. Prenatal diagnosis of trisomy 6 rescue resulting in paternal UPD6 with novel placental findings. Am J Med Genet Part A. 2011;155 A(8):1996–2002.)mat (including our 2 cases), 18 (85.7%) presented IUGR.
Conclusions
The phenotypes of the two newly identified patients with upd(Cajaiba MM, Witchel S, Madan-Khetarpal S, Hoover J, Hoffner L, Macpherson T, et al. Prenatal diagnosis of trisomy 6 rescue resulting in paternal UPD6 with novel placental findings. Am J Med Genet Part A. 2011;155 A(8):1996–2002.)mat further suggest that IUGR is associated with upd(Cajaiba MM, Witchel S, Madan-Khetarpal S, Hoover J, Hoffner L, Macpherson T, et al. Prenatal diagnosis of trisomy 6 rescue resulting in paternal UPD6 with novel placental findings. Am J Med Genet Part A. 2011;155 A(8):1996–2002.)mat and case 2 is the first reported upd(Cajaiba MM, Witchel S, Madan-Khetarpal S, Hoover J, Hoffner L, Macpherson T, et al. Prenatal diagnosis of trisomy 6 rescue resulting in paternal UPD6 with novel placental findings. Am J Med Genet Part A. 2011;155 A(8):1996–2002.)mat patient with a homozygous SCUBE3 gene mutation. However, the specific phenotypes involved in upd(Cajaiba MM, Witchel S, Madan-Khetarpal S, Hoover J, Hoffner L, Macpherson T, et al. Prenatal diagnosis of trisomy 6 rescue resulting in paternal UPD6 with novel placental findings. Am J Med Genet Part A. 2011;155 A(8):1996–2002.)mat and the related mechanisms need to be further studied.
Similar content being viewed by others
Background
Uniparental disomy (UPD), first reported by Engel in 1980 [1], is defined as the inheritance of both copies of genetic material from one parent and can be classified into isodisomy and heterodisomy based on the underlying mechanism. In uniparental heterodisomy, a child inherits both alleles from a single parent while a single parental allele is duplicated in uniparental isodisomy [2]. Heterodisomy and isodisomy can occur on the same chromosome, making it difficult to distinguish them. UPD usually arises through meiotic non-disjunction with mitotic correction or gametic complementation [3].
If the UPD affects a chromosome harboring imprinted genes, it can result in an imprinting disorder. Imprinted genes tend to cluster, and the imprinting control is often not restricted to a single gene at an imprinted locus but affects the expression of several factors. The clinical outcome in the case of microduplications or microdeletions is influenced by the size, the breakpoint positions, and the parental inheritance of the imbalance as well as by the imprinting status of the affected genes [4]. Furthermore, there is the potential risk of homozygosity of an autosomal-recessive mutation in the case of uniparental isodisomy. In this case, homozygous mutations can be detected in the patient. And one parent is heterozygous for the mutant vector, while the other parent is homozygous for the wild-type allele. A third pathobiological mechanism can be delineated from UPD formation mechanisms: uniparental heterodisomy may be the result of a trisomic rescue [5].
The phenotype of paternal UPD6 (upd [6]pat) results from the biallelic expression of the maternally imprinted, paternally expressed PLAGL1 and HYMAI genes and includes transient neonatal diabetes mellitus, intrauterine growth restriction (IUGR), macroglossia, and minor anomalies [6].
The first reported maternal uniparental disomy for chromosome 6 (upd [6]mat) was found in kidney transplant patients in 1996 [7]. However, upd [6]mat is extremely rare, with only about 20 cases reported so far. Its exact phenotype and associated mechanisms are still unknown, with IUGR being the most common phenotype in the patients reported. Herein, we report 2 upd [6]mat pediatric patients presented with IUGR to highlight the specific phenotype and mechanism of upd [6]mat.
Case presentation
Clinical report
Case 1 is a 6 years and 8 months boy admitted to our hospital as growth retardation. He was the second child of his non-consanguineous marriage parents. He was born by cesarean section at 32 weeks gestation with a birth weight of 1.3 kg. After birth, he had feeding difficulties and had a gastrostomy at the age of 1 year. He started walking and talking when he was one year old, and neither his intellectual nor physical ability significantly regressed. Additionally, he had allergic rhinitis. When he was six and a half years old, his bone age was about nine years. The insulin-like growth factor 1 (IGF-1) and dehydroepiandrosterone were 250 ng/ml and 2.92 µmol/L, respectively. The adrenal routine scan showed no obvious abnormalities in local hospital. His 8-year-old brother was 129 cm tall. His mother is 158 cm tall, while his father is 160 cm. The heights of the paternal grandmother and grandfather are 156 cm and 167 cm, respectively. The maternal grandmother is 156 cm tall and the maternal grandfather is 168 cm tall.
Physical examination revealed a weight of 24 kg and a height of 117 cm (-2SD–1SD). He was found to have strange body hair, penetrating hands, and a high palatal arch despite having a uniform figure and appearance. His cardiopulmonary auscultation revealed no abnormalities. The bilateral testicular stage was G1 and the pubic hair stage was Ph1.
The basic luteinizing hormone was 0.12 IU/l, follicle-stimulating hormone was 1.14 IU/l, prolactin was 153.4 mIU/l, testosterone was lower than 0.45 nmol/l and human chorionic gonadotropin was lower than 1.2 IU/l. Adrenocorticotropic hormone (ACTH) stimulation test showed the cortisol levels of 13.6, 27.6, 28.2, and 32.4 µg/dl, respectively (basic normal range, 5–25 µg/dl), dehydroepiandrosterone sulfate levels of 224, 208, 234 and 241 ng/ml (basic normal range for prepubertal children, < 80.1 ng/ml), the 17α-hydroxyprogesterone levels of 1.1, 2, 1.8 and 1.2 ng/ml, respectively (basic normal range, < 11.58 ng/ml), and testosterone levels of 0.47, 0.57. 0.62 and 0.58 nmol/l at 0, 30, 60 and 90 min. The fasting blood glucose was 5.59 mmol/L and the insulin was 95.6 pmol/L. Testicular echo was found on the left scrotum scan (1.7 cm × 1.0 cm × 0.8 cm), and on the right scrotum scan (1.8 cm × 1.1 cm × 0.8 cm). Blood gases, thyroid function, magnetic resonance imaging (MRI) of the pituitary, electrocardiogram, and abdominal ultrasound were unremarkable.
Case, a 9-year-old girl, presented to our unit because of growth retardation and poor response to recombinant human growth hormone (rhGH) treatment. She was the first child of her non-consanguineous marriage parents. She was born by cesarean section at 36 weeks gestation with a birth weight of 1.2 kg. she had normal development milestones without significant abnormal intelligence. However, growth retardation was noted with a height of 118.6 cm (-2SD–1SD) at the age of 8. Bone age showed 8 carpal osteogenesis, ulnar shaft protrusion, and sesamoid bone present, which implied about 10.5 years old. Growth hormone (GH) stimulation test showed a peak GH of 18.39 ng/ml and an IGF-1 of 266 ng/ml in the local hospital. The basic luteinizing hormone, follicle-stimulating hormone, testosterone, human chorionic gonadotropin, and 17α-hydroxyprogesterone levels were within the normal range for prepubertal children. Liver or kidney function, thyroid function, MRI of the pituitary, and abdominal ultrasound were unremarkable. Small for gestational age (SGA) was regarded and rhGH was administered. The dose of rhGH was gradually increased from the initial 2.5U to 4U (about 0.19 U/kg). However, her height was poor increased with about 2 cm in 6 months. The mother’s second fetus was aborted because of the deformity (without detail data). Her father is 168 cm tall and her mother is 155 cm tall. The maternal grandmother’s height is 140 cm.
Physical examination revealed a height of 124.5 cm (-2SD–1SD) and a weight of 21.1 kg (-2SD–1SD). She has a well-proportioned figure and no distinctive features were noted. Her cardiopulmonary auscultation revealed no abnormalities. The breast stage was B1 and the pubic hair stage was Ph1.
Genetic testing
In case 1, genetic testing is done because parents want to know why their children lag behind their peers. chromosomal microarray analysis (CMA) and whole exome sequencing (WES) were performed, and CYP21A2 gene rearrangement was detected to further exclude adrenocortical hyperplasia as well. WES was performed for case 2 genetic testing was carried out as growth retardation and poor response of rhGH. The sequencing results were analyzed by bioinformatics and interpreted by pedigree genetics.
Results of genetic testing
In case 1, no copy number changes were identified by CMA analysis. However, the single nucleotide polymorphism (SNP) component of this assay identified 2 large regions of the absence of heterozygosity (AOH) on chromosome 6, including a 55 Mb in 6p21.2q15 (37 496 966 − 92 651 403) region and a 34 Mb 6q23.3q27 (136 295 353 − 170 903 114) region. At least 199 genes were enrolled in this region, which includes the imprinted region. The presence of a large region of AOH on an imprinted chromosome may be indicative of UPD6. The trio-WES data showed a UPD6, which originated from his mother. This suggested a uniparental isodisomy mixed with a uniparental heterodisomy. No rearrangements or hot spot mutations were detected in the CYP21A2 gene.
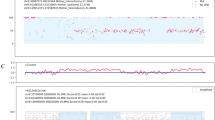
A homozygous missense variant c.2330T > C (p. Phe777Ser) in the exon 18 of the SCUBE3 gene was found in case 2. It was noted that a similar heterozygous variant was found in her mother but not in her father (Fig. 1). Deep data mining analysis showed that the SNPs in the 6 318 921 − 42 236 498 of the 6p21.1-25.1 region (about 36 Mb) were homozygous and inherited from the mother with normal signal intensity, which suggested the mUPD in this region and the homozygous variant detected in this patient was associated with upd [6]mat.
Following-up
Case 1 has been taking 3.5 U (about 0.19 U/kg) of rhGH powder daily for about 4 months and has gained about 3 cm in height. Case 2 discontinued rhGH treatment because of poor response to the rhGH treatment.
Literature review
In PubMed and Wangfang Date, articles related to upd [6]mat are retrieved by searching for keywords “maternal uniparental disomy chromosome 6” or “mat UPD6” or “upd [6]mat” till Jule 30, 2022.
Only 21 cases (including our 2 cases) have been reported. Although phenotype was different in different cases, IUGR was present in 18 of 21 cases (85.7%) and postnatal short stature was present in 11 cases (52.4%), as showed Table 1 [4, 7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22].
Discussion and conclusions
UPD is a rare event that can lead to disease phenotypes through different mechanisms: genomic imprinting, mosaics, or uncovering autosomal recessive genetic variants [5]. Due to the rarity of upd [6]mat, its mechanism and phenotype are not well understood.
One of the possible mechanisms by which upd [6]mat contributes to the phenotype is the disturbance of imprinted genes. Disturbances of imprinting genes are known to cause abnormalities in fetal growth and placental function [23, 24]. Of the 21 reported upd [6]mat patients, 18 had IUGR. IUGR may be the specific phenotype of upd [6]mat and the occurrence of IUGR in upd [6]mat patients is most likely caused by the disorder of the imprinted gene. Genetic detection of case 1 revealed the presence of upd [6]mat, mainly involving 6q23.3q27, which contains the imprinted genes HYMAI and PLAGL1 (at 6q24). The patient presents with IUGR and short stature. In upd [6]pat, the overexpression of imprinted genes PLAGL1 and HYMAI lead to IUGR and other specific clinical phenotypes, while in case 1, the absence of imprinted genes also indicates IUGR. We hypothesized that not imprinted genes HYMAI and PLAGL1, but other imprinted genes on chromosome 6 are responsible for IUGR in case 1. The effect of IGF2R (at 6q25.3) methylation on intrauterine growth and upd [6]mat has been reported [14]. PRIM2, PXDC1, and other imprinted genes on chromosome 6 can be further investigated.
Upd [6]mat can also lead to phenotypes by uncovering homozygous mutations in autosomal recessive genes. Case 2 has an autosomal recessive disorder caused by upd [6]mat, which is the first reported case of upd [6]mat with SCUBE3 mutation. The SCUBE3 gene is highly expressed in primary osteoblasts and long bones and is localized on human chromosome 6p21.3 [25]. SCUBE3 loss-of-function causes a recognizable recessive developmental disorder. The common clinical manifestations of homozygous SCUBE3 mutations are short stature, facial deformities, and skeletal abnormalities with or without cardiac abnormalities [26]. A homozygous missense variant c.2330T > C (p.Phe777Ser) in exon18 of the SCUBE3 gene was found in case 2. It was noted that a similar heterozygous variant was found in her mother but not in her father. The patient presented with IUGR, further suggesting that upd [6]mat is associated with IUGR and may be due to an autosomal recessive disorder caused by upd [6]mat. Case 2 showed short stature, but no facial deformity or skeletal abnormality was found on physical examination, and the presence of cardiac abnormality requires further examination.
Upd [6]mat can be found in the mechanism exploration of some rare diseases, such as Silver-Russell syndrome [5]. There are also some patients with upd [6]mat whose phenotype does not appear abnormal and are ignored [20]. Due to the limitation of the number of upd [6]mat cases, the mechanism by which it leads to the phenotype is unclear. At present, more related cases need to be found, and the specific phenotype and mechanism that lead to them of upd [6]mat should be actively explored.
In conclusion, our patients further provided evidence that upd [6]mat is associated with IUGR and we report the first upd [6]mat patient with SCUBE3 mutation. Further understanding of the specific phenotype of upd [6]mat and exploring its pathogenesis will not only facilitate the detection of upd [6]mat patients and early treatment but also help to expand the mutation spectrum and pathogenesis of various rare diseases, which will help to carry out genetic counseling and reduce the incidence of the disease.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- UPD:
-
Uniparental disomy
- UPD6:
-
Uniparental disomy for chromosome 6
- upd(6)mat:
-
Maternal uniparental disomy for chromosome 6
- upd(6)pat:
-
Paternal UPD6 uniparental disomy for chromosome 6
- IUGR:
-
Intrauterine growth restriction
- CMA:
-
Chromosomal microarray analysis
- WES:
-
Whole exome sequencing
- SNP:
-
Single nucleotide polymorphism
- IGF-1:
-
Insulin-like growth factor 1
- MRI:
-
Magnetic resonance imaging
- GH:
-
Growth hormone
- rhGH:
-
Recombinant human growth hormone
- AOH:
-
Absence of heterozygosity
- ACTH:
-
Adrenocorticotropic hormone
References
Engel E. A new genetic concept: uniparental disomy and its potential effect, isodisomy. Am J Med Genet. 1980;6(2):137–43.
Milenkovic T, Martic J, Robinson DO, Mackay DJ, Petrovic K, Zdravkovic D. Transient neonatal diabetes mellitus in an infant with paternal uniparental disomy of chromosome 6 including heterodisomy for 6q24. J Pediatr Endocrinol Metabolism: JPEM. 2006;19(11):1353–7.
Benn P. Uniparental disomy: origin, frequency, and clinical significance. Prenat Diagn. 2021;41(5):564–72.
Begemann M, Spengler S, Gogiel M, Grasshoff U, Bonin M, Betz RC, et al. Clinical significance of copy number variations in the 11p15.5 imprinting control regions: new cases and review of the literature. J Med Genet. 2012;49(9):547–53.
Sachwitz J, Strobl-Wildemann G, Fekete G, Ambrozaitytė L, Kučinskas V, Soellner L, et al. Examinations of maternal uniparental disomy and epimutations for chromosomes 6, 14, 16 and 20 in Silver-Russell syndrome-like phenotypes. BMC Med Genet. 2016;17:20.
Cajaiba MM, Witchel S, Madan-Khetarpal S, Hoover J, Hoffner L, Macpherson T, et al. Prenatal diagnosis of trisomy 6 rescue resulting in paternal UPD6 with novel placental findings. Am J Med Genet Part A. 2011;155A(8):1996–2002.
van den Berg-Loonen EM, Savelkoul P, van Hooff H, van Eede P, Riesewijk A, Geraedts J. Uniparental maternal disomy 6 in a renal transplant patient. Hum Immunol. 1996;45(1):46–51.
Spiro RP, Christian SL, Ledbetter DH, New MI, Wilson RC, Roizen N, et al. Intrauterine growth retardation associated with maternal uniparental disomy for chromosome 6 unmasked by congenital adrenal hyperplasia. Pediatr Res. 1999;46(5):510–3.
Cockwell AE, Baker SJ, Connarty M, Moore IE, Crolla JA. Mosaic trisomy 6 and maternal uniparental disomy 6 in a 23-week gestation fetus with atrioventricular septal defect. Am J Med Genet Part A. 2006;140(6):624–7.
Parker EA, Hovanes K, Germak J, Porter F, Merke DP. Maternal 21-hydroxylase deficiency and uniparental isodisomy of chromosome 6 and X results in a child with 21-hydroxylase deficiency and Klinefelter syndrome. Am J Med Genet Part A. 2006;140(20):2236–40.
Gümüş H, Ghesquiere S, Per H, Kondolot M, Ichida K, Poyrazoğlu G, et al. Maternal uniparental isodisomy is responsible for serious molybdenum cofactor deficiency. Dev Med Child Neurol. 2010;52(9):868–72.
Salahshourifar I, Halim AS, Sulaiman WA, Zilfalil BA. Maternal uniparental heterodisomy of chromosome 6 in a boy with an isolated cleft lip and palate. Am J Med Genet Part A. 2010;152A(7):1818–21.
Sasaki K, Okamoto N, Kosaki K, Yorifuji T, Shimokawa O, Mishima H, et al. Maternal uniparental isodisomy and heterodisomy on chromosome 6 encompassing a CUL7 gene mutation causing 3 M syndrome. Clin Genet. 2011;80(5):478–83.
Poke G, Doody M, Prado J, Gattas M. Segmental maternal UPD6 with prenatal growth restriction. Mol Syndromol. 2013;3(6):270–3.
Roosing S, van den Born LI, Hoyng CB, Thiadens AA, de Baere E, Collin RW, et al. Maternal uniparental isodisomy of chromosome 6 reveals a TULP1 mutation as a novel cause of cone dysfunction. Ophthalmology. 2013;120(6):1239–46.
Takimoto T, Takada H, Ishimura M, Kirino M, Hata K, Ohara O, et al. Wiskott-Aldrich syndrome in a girl caused by heterozygous WASP mutation and extremely skewed X-chromosome inactivation: a novel association with maternal uniparental isodisomy 6. Neonatology. 2015;107(3):185–90.
Lazier J, Martin N, Stavropoulos JD, Chitayat D. Maternal uniparental disomy for chromosome 6 in a patient with IUGR, ambiguous genitalia, and persistent mullerian structures. Am J Med Genet Part A. 2016;170(12):3227–30.
Eggermann T, Oehl-Jaschkowitz B, Dicks S, Thomas W, Kanber D, Albrecht B, et al. The maternal uniparental disomy of chromosome 6 (upd(6)mat) phenotype: result of placental trisomy 6 mosaicism? Genomic Med. 2017;5(6):668–77. Molecular genetics.
Leung WC, Lau WL, Lo TK, Lau TK, Lam YY, Kan A, et al. Two IUGR foetuses with maternal uniparental disomy of chromosome 6 or UPD(6)mat. J Obstet Gynaecology: J Inst Obstet Gynecol. 2017;37(1):113–5.
Kerr ER, Stuhlmiller GM, Maha GC, Ladd MA, Mikhail FM, Koester RP, et al. Maternal uniparental isodisomy for chromosome 6 discovered by paternity testing: a case report. Mol Cytogenet. 2018;11:60.
Souzeau E, Thompson JA, McLaren TL, De Roach JN, Barnett CP, Lamey TM, et al. Maternal uniparental isodisomy of chromosome 6 unmasks a novel variant in TULP1 in a patient with early onset retinal dystrophy. Mol Vis. 2018;24:478–84.
Zhang P, Ying W, Wu B, Liu R, Wang H, Wang X, et al. Complete IFN-γR1 Deficiency in a boy due to UPD(6)mat with IFNGR1 novel splicing variant. J Clin Immunol. 2021;41(4):834–6.
Butler MG. Imprinting disorders in humans: a review. Curr Opin Pediatr. 2020;32(6):719–29.
Thamban T, Agarwaal V, Khosla S. Role of genomic imprinting in mammalian development. J Biosci. 2020;45.
Wu BT, Su YH, Tsai MT, Wasserman SM, Topper JN, Yang RB. A novel secreted, cell-surface glycoprotein containing multiple epidermal growth factor-like repeats and one CUB domain is highly expressed in primary osteoblasts and bones. J Biol Chem. 2004;279(36):37485–90.
Lin YC, Niceta M, Muto V, Vona B. SCUBE3 loss-of-function causes a recognizable recessive developmental disorder due to defective bone morphogenetic protein signaling. Am J Hum Genet. 2021;108(1):115–33.
Acknowledgements
Not applicable.
Funding
Our study was funded by the National Natural Science Foundation of China (81371215 & 81670786) and Key R & D Projects of Zhejiang Provincial Department of Science and Technology (2021 C03094).
Author information
Authors and Affiliations
Contributions
Chao-Chun Zou conceptualized the study. Jing-Wen Li and Yan-Jie Qian drafted the initial manuscript. Shao-Jia Mao, Yun-Qi Chao, Yi-Fang Qin, Chen-Xi Hu and Zheng-Lan Li polished and revised the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Our cases have been approved for research by the Medical Ethics Committee of the Children’s Hospital of Zhejiang University School of Medicine, under review number 2022-IRB-255.
Consent for publication
The consent of their parents or legal guardians has been obtained.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it.The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Li, JW., Qian, YJ., Mao, SJ. et al. Clinical features associated with maternal uniparental disomy for chromosome 6. Mol Cytogenet 17, 18 (2024). https://doi.org/10.1186/s13039-024-00688-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13039-024-00688-y